Abstract
Background:
When landing from a jump, the production of increased intersegmental knee abduction moments and coupled valgus motions has been associated with an increased risk of suffering a noncontact anterior cruciate ligament (ACL) injury in one study. This research has led to the development of a clinic-based algorithm that utilizes measures of knee valgus motion, knee flexion range of motion, body mass, tibial length, and quadriceps-to-hamstring strength ratio data to predict the probability of a high knee abduction moment (pKAM) when landing from a jump in female athletes. The ability of this algorithm to identify athletes at increased risk of suffering ACL injury has not been assessed.
Hypothesis:
The pKAM is associated with ACL injury in female athletes.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
This study was based on secondary analysis of data obtained from a previous investigation that focused on the use of the drop vertical jump (DVJ) test to assess the risk of ACL injury in female athletes. The DVJ screenings were performed on 1855 female high school and college athletes over 3 years. Knee valgus motion, knee flexion range of motion, and tibial length were measured from videos of the DVJ obtained during preseason screenings. Mass was measured using a physician’s scale, and quadriceps-to-hamstring strength ratio was included using a surrogate value. These data were entered into the clinic-based algorithm that determined the pKAM. The association of pKAM with ACL injury was assessed using conditional logistic regression.
Results:
A total of 20 athletes sustained ACL injury and were matched with 45 uninjured control athletes who were recruited from the same teams. There was no relationship between the risk of suffering ACL injury and pKAM, as determined by the clinic-based algorithm.
Conclusion:
The pKAM was not associated with noncontact ACL injury in our group of injured athletes and matched controls.
Keywords: anterior cruciate ligament, injury risk, jump landing, knee kinematics
Anterior cruciate ligament (ACL) injuries of the knee are immediately disabling and are associated with premature onset of osteoarthritis regardless of whether surgical or nonsurgical treatment is administered.1,5,6,8,15,17 These debilitating injuries in otherwise young, healthy people have caused researchers to focus on identifying the risk factors for ACL injury so that those at increased risk can be identified and interventions may be applied.
The use of video-based measurements during gameplay as well as the administration of dynamic tests such as the drop vertical jump (DVJ) have determined that increased intersegmental knee abduction moment2 and valgus angle at the knee,2–4,13 increased foot-floor reaction force,2 and decreased stance time when landing2 are associated with an increased risk of suffering a noncontact ACL injury.2,4,13,18 Evaluation of these biomechanical parameters requires the use of complex, laboratory-based measurement systems to characterize the 3-dimensional (3-D) biomechanics of the lower extremities and ground-reaction forces that occur during activities that challenge the knee. These approaches are time consuming and consequently not practical to use as screening tools in the large population of active athletes at risk for suffering a severe knee ligament injury. Therefore, there is a need for valid screening tools that can assess lower extremity biomechanics in a time-efficient manner to specifically identify those at an increased risk for ACL injury.
Recently, Myer et al9–12 and Hewett et al2 have expanded on their original laboratory-based, 3-D biome-chanics research of 15- to 16-year-old female soccer and basketball players, identifying increased intersegmental abduction moments about the knee when landing from a DVJ was associated with an increased risk of suffering an ACL injury. They recently published a series of 4 works describing the development of a clinic-based algorithm to predict the probability of a high knee abduction moment (pKAM) based on analysis of 2-dimensional (2-D) video data obtained with standard video cameras, to provide a measurement tool that has the capacity to be applied to larger populations for mass screening of injury risk.9–12 First, laboratory-based measures of intersegmental knee abduction moments were obtained, and then clinic-based surrogate variables for the laboratory-based measurements were identified. Correlations between the clinic-and laboratory-based measures ranged from .87 to .98 (P < .001).12 The clinic-based surrogate variables included knee valgus and flexion range of motion during the landing phase of the DVJ, tibial length, body mass, and a surrogate measure for quadriceps-to-hamstring strength ratio (quad:ham).9,11,12 A clinic-based algorithm was then developed using the surrogate variables to assess the pKAM when landing from the DVJ.9–12 The clinic-based algorithm predicted pKAM values on a scale that ranged between 0 and 1 with 84% sensitivity, 67% specificity, and a C statistic of .85.12 The primary outcome of the current study was pKAM, as defined by the clinic-based algorithm, rather than the intersegmental knee abduction moment.
The objective of the current study was to apply the clinic-based algorithm developed by Myer et al9–12 to a population of female athletes who competed in varsity-level high school and college sports and determine if pKAM was associated with ACL injury risk. We also sought to evaluate the intrarater reliability of measurements of knee valgus motion and knee flexion range of motion obtained with 2-D video. Our hypothesis was that the clinic-based algorithm would predict athletes at increased risk of suffering an ACL injury.
MATERIALS AND METHODS
Participants
The University Committee on Human Research in the Medical Sciences review board approved this study, and all participants and/or their legal guardians provided informed consent before participation. This investigation was a secondary analysis of data obtained from an ongoing prospective study,16 which was designed to evaluate multiple risk factors for ACL injury by screening at-risk athletes before participation in their athletic season using the DVJ and then monitoring this population for ACL injury. Once an injury occurred, injured athletes and controls visited our laboratories for further evaluation of other potential risk factors as well as analysis of the DVJ videos. The clinic-based algorithm reported by Myer et al9–12 was developed for female patients, and consequently, this secondary analysis included the 1855 female athletes who were screened before participation in their competitive athletic season using the DVJ testing procedure.14 Screenings took place over a 3-year interval that began in the fall of 2008 and ran through the spring of 2011. Athletes participated in soccer, field hockey, basketball, gymnastics, lacrosse, rugby, ultimate Frisbee, and volleyball. Participants were followed during their sport seasons, and those who subsequently suffered a grade III noncontact injury to their ACL (defined as an event where no direct contact to the knee was reported at the time of injury) were included in the analysis. Participants who had experienced a previous ACL tear were excluded. This study used a nested case-control analysis to assess the relationship between the pKAM and ACL injury risk. Each participant was matched with between 1 and 3 control athletes who were selected from the same team, were the same sex, were the same age (within 1 year), and had been screened with the DVJ at the same time. Multiple controls were selected whenever available to increase statistical power. An ACL rupture was verified with evaluation by an orthopaedic surgeon, magnetic resonance imaging, and subsequent arthroscopic visualization. A detailed description of the participants has been presented.16
Testing and Data Processing Procedures
Before participation in their at-risk sport, participants underwent a screening following the procedures previously described.16 Each participant performed 3 DVJ trials according to the protocol previously described by Padua et al.14 Frontal and sagittal view video data were acquired using standard Canon high-definition video camcorders (Tokyo, Japan) that were positioned according to the protocol.14 The Video Supplements are available in the online version of this article at http://ajs.sagepub.com/supplemental/. There are 2 reference videos, taken simultaneously of the same jump from the sagittal and frontal views.
Video Measurements
The DVJ video data were analyzed using Dartfish ProSuite 4.5.2.0 software (Dartfish Ltd, Fribourg, Switzerland). Videos of each ACL-injured athlete and their matched controls were viewed by 1 investigator (J.G.), and measurements of tibial length, knee valgus motion, and knee flexion range of motion were made for the landing phase of all 3 DVJ trials. For each trial, all measurements were made 3 times and then averaged. Displacement measurements were calibrated using a box of known dimensions that was located at the point of landing from the DVJ and filmed from each camera just before each screening session. Descriptions of how each measurement was made follow.
Knee Valgus Motion.
Knee valgus motion produced during the landing phase of the DVJ was characterized. This was measured as the medially directed movement of the knee joint center between the video frame just before initial contact of the foot with the ground and the frame that captured the maximum medial position of the knee that was produced during the landing phase of the DVJ.9 The center of the knee joint was identified on the frontal plane video by digitizing the midpoint of the horizontal distance between the most medial and lateral aspects of the knee at the level of the tibiofemoral joint line. This was done at initial contact of the foot with the ground (Figure 1) and the maximum medial position (Figure 2) video frames, and then the distance between these 2 points was measured (parallel to the plane of the floor) and used to characterize the valgus motion of the knee during the landing phase of the DVJ (Figure 3).
Figure 1.
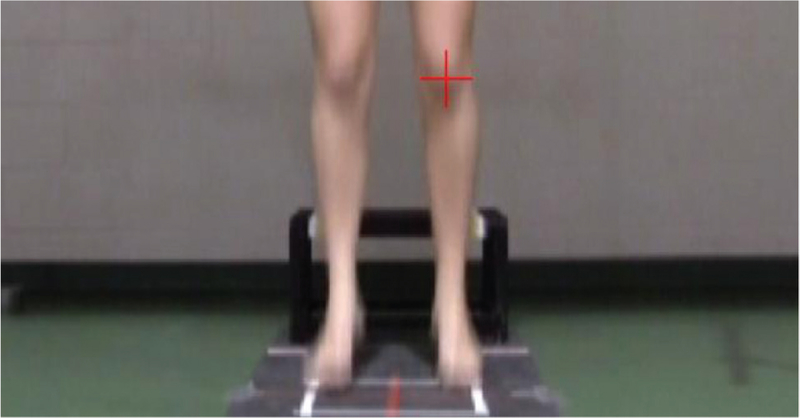
Knee joint center at initial contact with the ground during the landing phase of the drop vertical jump. The + represents the location of the knee joint center at initial contact of the foot with the ground.
Figure 2.
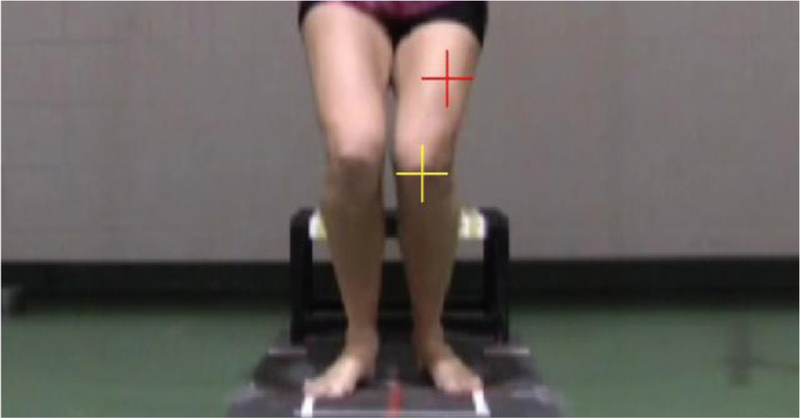
Knee joint center at maximum medial position during the landing phase of the drop vertical jump. The top + represents the location of the knee joint center at initial contact with the ground, and the bottom + is the knee joint center at its maximum medial position during landing.
Figure 3.
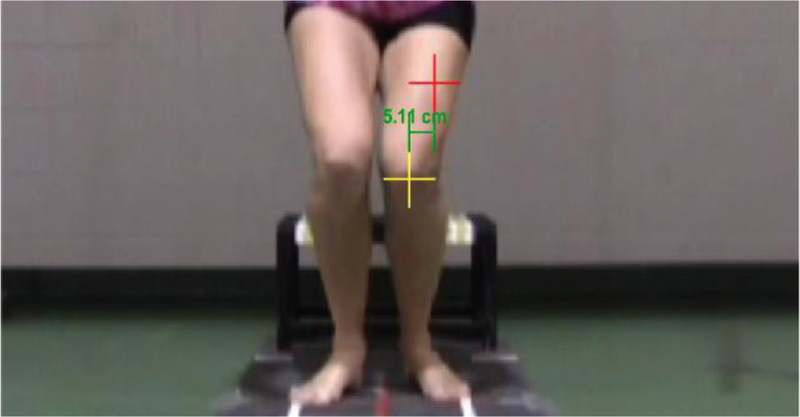
Knee valgus motion during the landing phase of the drop vertical jump (DVJ). The line between the top and bottom + is a measurement of knee motion from initial contact with the ground to the maximum medial position of the knee during the landing portion of the DVJ.
Knee Flexion Range of Motion.
Knee flexion range of motion was also characterized during the landing phase of the DVJ. This was determined by measuring the angle between lines constructed along the anterior aspects of the thigh and lower leg in the sagittal plane video. Knee flexion range of motion was defined as the change between the knee flexion angle measured from the video frame just before initial contact of the foot with the floor (Figure 4) and the flexion angle measured at the frame with maximum knee flexion (Figure 5).9
Figure 4.
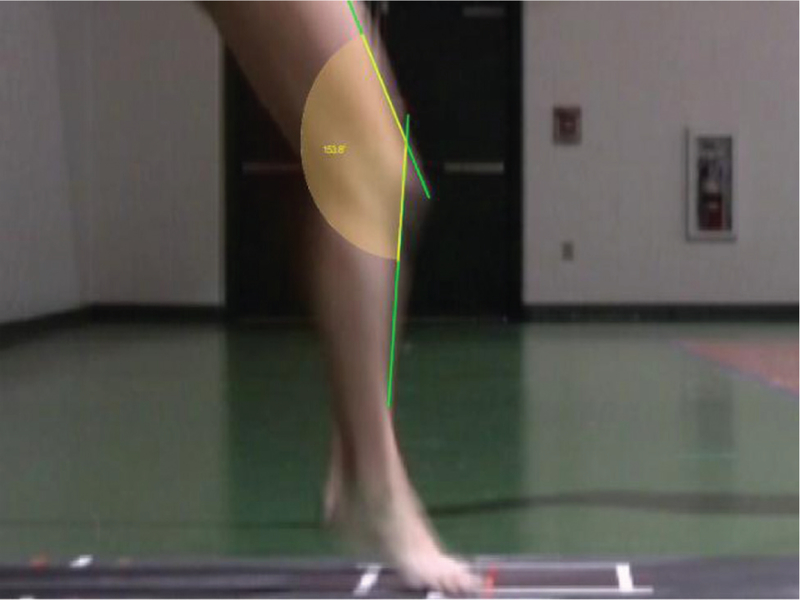
Knee flexion angle at initial contact with the ground produced during the landing phase of the drop vertical jump.
Figure 5.

Knee flexion angle at maximum flexion during the landing phase of the drop vertical jump.
Tibial Length.
Not all injured athletes and controls chose to participate in the follow-up laboratory visit to obtain a measurement of tibial length with a handheld caliper as part of the overall study of ACL injury risk factors. Therefore, these data were obtained using the sagittal view of the DVJ video using the Dartfish video analysis program. To accomplish this, measurement calibrations were performed for both the horizontal and vertical dimensions using the known width and height of the calibration box. Then, the regions overlaying the distal aspect of the lateral malleolus and the proximal aspect of the fibular head were identified on the same video frame of the flexed knee, and the distance between these points was measured and used to represent the length of the fibula. To confirm the accuracy of this approach, the video-based measure was correlated with the length of the tibia that was measured with a handheld caliper on the subgroup of participants that underwent both measurements. This correlation was very good, with r = .85.
Body Mass and Quad:Ham Strength Ratio.
The athletes who participated in a laboratory visit underwent measurements of body mass and height using a calibrated physician’s scale, while those who did not provided their height and weight. The clinical algorithm utilizes a quad:ham strength ratio obtained from isokinetic strength measurements performed at 300 deg/s. These measurements require expensive equipment, are labor intensive, and are not practical for screening evaluations. This was recognized by Myer et al,9 who developed a surrogate measure of quad:ham strength ratio that was defined using a linear regression analysis based on body mass. This measure was obtained by multiplying the female athlete’s mass by 0.01 and adding the resultant value to 1.10.9
Statistical Methods (Reliability and Case-Control Analyses)
Intrarater reliability of knee valgus motion and knee flexion range of motion were evaluated on a subset of 10 participants not included in this study. Intrarater reliability was evaluated using duplicate measurements of knee valgus and knee flexion range of motion from the same video, which were obtained by 1 investigator at 2 time points separated by 1 week.
The clinic-based algorithm was applied, as it was developed to compute the pKAM for all participants and controls. The primary outcome of the current study was pKAM rather than the intersegmental knee abduction moment. Conditional logistic regression, which directly compares participants to their respective matched controls, was used to assess the association between pKAM and risk of ACL injury, independent of potential differences in DVJ landing techniques because of type of sport, sex, and age (the study was designed to match participants on these variables). A detailed description for the rationale associated with the use of the statistical methods has been previously described.16 Briefly, a nested case-control analysis using conditional logistic regression provides results that are comparable to those from Cox regression analysis of the entire cohort, with only a small reduction in statistical power. The odds ratio (OR) associated with a 0.10 increase in pKAM and its corresponding 95% confidence intervals (CIs) are reported for both continuous and quartile measures. Statistical significance was set at P < .05.
RESULTS
Participants
Of the 1855 female athletes who were screened with the DVJ protocol and followed over the duration of their sport seasons, 20 suffered a complete ACL tear and underwent reconstruction. Each participant was matched with between 1 and 3 female control athletes who were the same age within 1 year, were on the same athletic team at the time of injury, and had been previously screened with the DVJ at the same time as the case participant. Five of these had 1 matched control, 7 had 2 controls, and 8 had 3 controls, for a total of 65 participants (20 athletes and 45 controls). Characteristics of the injured athletes and controls are summarized in Table 1.
TABLE 1.
Demographicsa
| Injured Athletes | Controls | |
|---|---|---|
| Age, y | 17.8 ± 1.8 (15–21) | 18.1 ± 1.7 (16–22) |
| Height, cm | 167.0 ± 4.8 (160.0–175.3) | 165.2 ± 6.7 (152.4–177.8) |
| Weight, kg | 64.2 ± 8.1 (52.6–83.0) | 63.2 ± 8.7 (50.3–85.3) |
Values are shown as mean ± standard deviation (range).
Reliability
The intrarater reliability of repeated measures of knee valgus and knee flexion range of motion were excellent, with intraclass correlation coefficient (ICC) values of .997 and .952, respectively.
Case-Control Analysis of the Association Between pKAM and Risk of ACL Injury
The clinic-based algorithm values of pKAM ranged from 0.18 to 0.98, and the mean ± standard deviation was 0.54 ± 0.19 for the injured athletes and 0.52 ± 0.21 for the controls. Conditional logistic regression analyses did not reveal a statistically significant relationship between pKAM as a continuous variable and the risk of suffering an ACL injury (P = .61), with an OR of 1.09 (95% CI, 0.78–1.52) for each 0.10 increase in pKAM. When pKAM values were grouped into quartiles, the ORs compared with the lowest quartile ranged from 1.24 to 2.00, with an overall P value of .88 (Table 2).
TABLE 2.
Odds Ratios for Quartiles of the pKAM Distribution Determined With the Clinic-Based Algorithma
| pKAM Quartile | Injured Athletes, n (%) | Controls, n (%) | Odds Ratio (95% CI) |
|---|---|---|---|
| 1: 0.00–0.36 | 4 (20) | 12 (27) | 1.00 (reference) |
| 2: 0.37–0.47 | 5 (25) | 12 (27) | 1.24 (0.30–5.10) |
| 3: 0.48–0.69 | 5 (25) | 11 (24) | 1.34 (0.27–6.74) |
| 4: 0.70–0.98 | 6 (30) | 10 (22) | 2.00 (0.36–11.02) |
pKAM, probability of a high knee abduction moment; CI, confidence interval.
DISCUSSION
We did not find a significant relationship between the pKAM, as calculated with the clinic-based algorithm developed by Myer et al,9–12 and an increased risk of suffering a noncontact ACL injury in female athletes. It is important for us to point out that we screened 1855 female athletes over a 3-year interval, and 20 of these athletes subsequently suffered a first-time, noncontact ACL injury. With 20 athletes and 45 matched controls, our study had 80% power to detect an OR of 1.65 for each 0.10 increase in pKAM. Our observed OR of 1.06 indicates that any association existing between pKAM and the risk of ACL injury in female athletes may be too small to warrant its use as a screening tool.
As in the prior work, time between screening and injury was an average of 224 days, ranging between 1 and 434 days. If DVJ landing biomechanics and/or pKAM changed as a function of time because of conditioning and/or maturation between the testing and the injury time points, we would assume that the change was the same for the athletes and the controls, as they were screened on the same date. While we did not collect exposure data on all screened participants, we matched injured athletes with controls on the same team who participated in the game or practice during which the athlete was injured and thus had the same exposure. This nested case-control design using conditional logistic regression, as previously decribed,16 produces results that are comparable with those that would be obtained from Cox regression, using exposure data from the entire cohort to model time to injury. The conditional logistic regression has nearly as much statistical power as the Cox regression but does not permit the variables used for matching injured athletes with controls (age, sex, and sport) to be assessed as risk factors for ACL injury.
The evidence supporting knee intersegmental abduction moments produced when landing from a jump as a risk factor for ACL injury is derived from the study conducted by Hewett et al.2 That study was based on 9 injured young female athletes, aged 15.8 6 1.0 years (injured athletes) versus 16.1 ± 1.7 years (controls), who participated in basketball, volleyball, and soccer and underwent a 3-D laboratory-based assessment. Our study focused on older participants who were skeletally mature, competed at high school and college levels, participated in a wider range of sports, and applied the 2-D clinic-based algorithm developed by Myer et al.9–12 The potential differences in study participants, levels of play, the types of sports the athletes participated in, and measurement approaches that were used may explain why we did not demonstrate a relationship between pKAM and ACL injury. For example, our athletes participated in different sports that ranged from high school to the National Collegiate Athletic Association (NCAA) Division I level. This wide range of fitness and skill inherent to different sports that are played at different levels of competition could affect the capacity of pKAM to predict ACL injury if DVJ biomechanics varies with the type and level of competition. In that case, a single algorithm to predict high knee abduction moments may not be universally applicable or predictive of injury risk for athletes who participate in different sports and different levels of competition. We screened 1855 female athletes between 2008 and 2011, and only 20 suffered noncontact ACL injuries in the follow-up time period. To have adequate power for sport-specific assessments of pKAM, a comparable number of injuries would be needed in each sport. Determining whether potential biomechanical differences between athletes in different sports contribute to sport-related differences in risk would be an interesting research question; however, our study was not designed to address this question. Instead, our goal was to assess the ability of pKAM to identify those at an increased risk of ACL injury among athletes participating in the same sport. We therefore controlled for differences in risk because of sport and level of play by matching controls and injured athletes from the same team and using conditional logistic regression to analyze the data.
In addition, it may be that a complete 3-D analysis of landing biomechanics is necessary to identify those at increased risk of suffering knee injury. While the correlations between the 3-D kinematic motion analysis and the 2-D camcorder screenings are considered robust, as previously described by the developers,9–12 it is possible that differences between the 2 screening techniques exist. This may have contributed to the clinic-based algorithm’s inability to predict ACL injury in our group of female participants. Specifically, the 2-D medial translation of the knee when landing from a jump may not be a comprehensive representation of the complex 3-D kinematics associated with ‘‘valgus,’’ or ‘‘valgus collapse,’’ which may only be characterized with the use of 3-D laboratory-based measurement systems. Myer et al12 reported good correlation between 3-D and 2-D knee valgus measures used in the algorithm. Previous work from the same group has shown that frontal plane 2-D knee angle and 3-D knee valgus measures correlate well (r2 = .64) during a side-jump task.7 Although 3-D and 2-D comparisons for knee valgus and the frontal plane projection of this angle have not been completed for a DVJ landing task outside of the development of the pKAM algorithm, we would expect frontal plane biomechanics to be similar. This work also showed larger movement ranges for the 2-D measurements compared with 3-D measurements.7 This finding suggests that 2-D motion analysis may not accurately capture the complete motion that occurs about the knee in comparison with 3-D motion analysis and would be less likely to show relationships between knee motion and ACL injury risk.
In an effort to include all 20 injured athletes in the analysis, the video-based method of measuring tibial length was developed and used to calculate pKAM. Twelve of the 20 case-control groups in this study (39 participants) also underwent direct measurement of tibial length using a handheld caliper (Pit Bull Tools, China), and the 2 measures correlated well (r = .85). Although our video-based measurement of tibial length correlated well with direct handheld caliper measurements, the values were, on average, 0.78 cm longer and significantly different between the 2 approaches (P < .01). Conditional logistic regression analysis performed on the 12 participants and 27 controls with direct handheld caliper measurements of tibial length yielded an OR of 1.01 (95% CI, 0.76–1.56) for each 0.10 increase in pKAM (P = .96). This finding indicates that the lack of an association between pKAM and risk of ACL injury in our analysis of the full complement of injured participants that was based on the video method of determining tibial length was not associated with the approach of using the video-based technique to measure tibial length.
Along with the clinic-based algorithm, Myer et al9 developed a nomogram to allow the evaluation of pKAM with a ‘‘clinician-friendly’’ approach. The nomogram is based on the same measurements as the clinic-based algorithm but utilizes a diagram to evaluate pKAM values. The use of the nomogram requires the evaluator to estimate specific values along a linear scale. We also compared the pKAM value calculated by the clinical algorithm with the pKAM value calculated by the mathematical algorithm in 10 participants because we wanted to determine if there were errors inherent with constructing lines on the nomogram. Reliability was estimated by calculating ICCs, and Pearson correlation was used to assess the relationship between the pKAM values based on the clinic-based algorithm and nomogram. The ICC for intrarater reliability of pKAM values based on the nomogram was .993, and the correlation between values from the nomogram and the clinic-based algorithm was .983 for the right leg and .990 for the left leg (Table 3). The clinic-based algorithm calculations of pKAM were highly correlated with the values predicted by the nomogram, and consequently, if we used the nomogram to determine pKAM, we would expect to obtain the same results.
TABLE 3.
Assessment of Nomogram Versus Clinic-Based Algorithm Modela
| Algorithm pKAM | Nomogram pKAM | Correlation Coefficient | |
|---|---|---|---|
| Right leg | .469 ± .223 | .456 ± .222 | r = .983 |
| Left leg | .422 ± .217 | .408 ± .211 | r = .990 |
Values are shown as mean ± standard deviation unless otherwise indicated. pKAM, probability of a high knee abduction moment.
This study is the second analysis of the same data set that applied a 2-D clinic-based approach to predict the risk of ACL injury in a large population. In the prior work, it was found that the Landing Error Scoring System (LESS) was not predictive of ACL injury risk,16 and the same was found with the clinic-based algorithm prediction of pKAM that was used in the current study. In contrast, the intersegmental knee abduction moment has been shown to be predicitve of injury risk in one prospective study.2 In that study, female athletes were evaluated during a DVJ landing task for intersegmental knee joint loading using 3-D kinematics and force plate data, and ACL-injured athletes (n = 9) exhibited increased knee abduction and intersegmental abduction moment as well as a greater ground-reaction force and shorter stance time in comparison to those who were not injured.2 It may be that 3-D measurement approaches are necessary to establish a relationship between the intersegmental moment generated at the knee during the landing phase of the DVJ and the risk of suffering an ACL injury rather than the 2-D clinic-based approaches.
CONCLUSION
We did not find the clinic-based algorithm of pKAM to be useful for identifying female athletes at increased risk of suffering a noncontact ACL injury. Without the use of predictive screening tools to provide an effective and efficient method for determining those at an increased risk for injury, intervention programs will need to be applied to populations as a whole rather than focusing on just those at increased risk. Therefore, additional research is needed to develop alternative clinic-based algorithms for the prediction of ACL injury risk that can be applied in an efficient manner to large groups of participants involved in activities that are associated with an increased risk of suffering an ACL injury.
Acknowledgments
source of funding: Funding provided by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01-AR050421).
Footnotes
One or more of the authors has declared the following potential conflict of interest
REFERENCES
- 1.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting. Am J Sports Med 2006;34(9):1512–1532. [DOI] [PubMed] [Google Scholar]
- 2.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 3.Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med 2010;38(11):2218–2225. [DOI] [PubMed] [Google Scholar]
- 4.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med 2007;35:359–367. [DOI] [PubMed] [Google Scholar]
- 5.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long term consequence of anterior cruciate ligament and meniscus injuries: osteo-arthritis. Am J Sports Med 2007;35(10):1756–1769. [DOI] [PubMed] [Google Scholar]
- 6.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 2004;50:3145–3152. [DOI] [PubMed] [Google Scholar]
- 7.McLean SG, Walker K, Ford KR, Myer GD, Hewett TE, van den Bogert AJ. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med 2005;39:355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mihata LCS, Beutler AI, Boden BP. Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players: implications for anterior cruciate ligament mechanism and prevention. Am J Sports Med 2006;34:899–904. [DOI] [PubMed] [Google Scholar]
- 9.Myer GD, Ford KR, Hewett TE. New method to identify athletes at high risk of ACL injury using clinic-based measurements and free-ware computer analysis. Br J Sports Med 2011;45(4):238–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med 2011;45(4):245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Clinical correlates to laboratory measures for use in non-contact anterior cruciate ligament injury risk prediction algorithm. Clin Biomech 2010;25(7):693–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med 2010;38(10):2025–2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med 2004;32:1002–1012. [DOI] [PubMed] [Google Scholar]
- 14.Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE Jr, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med 2009;37:1996–2002. [DOI] [PubMed] [Google Scholar]
- 15.Renstrom P, Ljungqvist A, Arendt E, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med 2008;42(6):394–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med 2012;40(3):521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient-relevant outcomes. Ann Rheum Dis 2004;63:269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu B, Garrett WE. Mechanisms of non-contact ACL injuries. Br J Sport Med 2007;41(Suppl I):i47–i51. [DOI] [PMC free article] [PubMed] [Google Scholar]


