Abstract
Background:
Lumbar decompressive surgery is a standard surgical technique for lumbar spinal stenosis. Many new surgical techniques have been introduced, ranging from open surgery to minimally invasive procedures. Minimally invasive surgical techniques are preferred because patients experience less postoperative pain and shorter hospital stays. However, the success rate of minimally invasive techniques have been controversial. The object of this study was to assess the feasibility of spinal decompression using biportal technique/endoscopic surgery compared with microscopic surgery.
Methods:
Seventy lumbar spinal stenosis patients undergoing laminectomy were included in this study. A number table was used to randomize the patients into two groups: a biportal technique/endoscopic surgery group (BG-36) and a microscopic surgery group (OG-34). One surgeon performed either biportal technique/endoscopic decompression or microscopic decompression using a tubular retractor, depending on the group to which the patient was randomized. Perioperative data and clinical outcomes at postoperative 6 months were collected and analyzed.
Results:
The demographic data and level of surgery were comparable between the two groups. A shorter operation time (36 ± 11 vs 54 ± 9 min), less hemovac drain output (25.5 ± 15.8 vs 53.2 ± 32.1 ml), less opioid usage (2.3 ± 0.6 vs 6.5 ± 2.5 T) and shorter hospital stay (1.2 ± 0.3 vs 3.5 ± 0.8 days) were shown in BG. The BG experienced no significant differences in clinical outcomes compared with OG. Favorable clinical outcomes were shown at 6 months after surgery in both groups.
Conclusion:
Lumbar decompressive surgery using biportal technique/endoscopy showed favorable clinical outcomes, less pain and a shorter hospital stay compared to microscopic surgery in patients with lumbar spinal stenosis.
Keywords: biportal technique/endoscopic spinal surgery, decompression, lumbar spinal stenosis, microscopic surgery
1. Introduction
Lumbar spinal stenosis is caused by pathologic spinal canal narrowing and compression of the thecal sac and nerve roots.[1] Degenerative lumbar spinal stenosis is caused by mechanical and biochemical alterations within the intervertebral disc that lead to disc space collapse, facet joint hypertrophy, soft-tissue infolding, and osteophyte formation, leading to the narrowing of the space available for the thecal sac and nerve roots.[2,3] Lumbar spinal stenosis patients present with claudication, back and leg pain, and decreased walking ability.[1] Eventually, lumbar spinal stenosis can lead to a significant decrease in the quality of life and even debilitating results.
In most cases, treatment for lumbar spinal stenosis begins with non-operative methods, such as physical therapy, corticosteroid injections, and oral medications.[4] Operative treatment is indicated for patients with intractable pain, decreased quality of life, progressive neurologic deficit, and failed non-operative treatment.[5] Though some patients might benefit from non-operative methods, past studies, such as the Spine Patient Outcomes Research Trial (SPORT), have shown that patients with symptomatic spinal stenosis showed greater improvement in both pain and function after being treated surgically.[6] Operative treatment lead to improvement in 60%–70% of patients with worsened symptoms despite proper non-operative treatment.[4,7]
As the elderly population increases, the number of operative treatments performed for lumbar spinal stenosis has increased over the past decades.[8] The primary goal of operative treatment is to decompress the neural structures that are being encroached, thus relieving symptoms and improving function. Decompressive surgery is the standard treatment for lumbar spinal stenosis, and open laminectomy, often combined with medial facetectomy and foraminotomy, is the conventional operation.[3] Traditionally, the surgery was carried out by making large incisions over the affected area with dissection of the paraspinal muscles from the spinous processes and prolonged retraction of the paraspinal muscles to expose the lamina.[9] Several studies have expressed concerns about the extensive invasiveness of such conventional operations, and less invasive procedures have emerged.[10]
Various minimally invasive spinal surgery techniques using microscopes, endoscopes, and arthroscopes have been introduced to be as least invasive as possible; these techniques are related to minimal disturbance of the normal anatomy with smaller incisions and less soft tissue dissection.[9,11] Such minimally invasive spinal surgery techniques were able to reduce iatrogenic complications and postoperative pain, promote faster recovery, shorten the hospital stay, and reduce the need for analgesics.[12] The aim of minimally invasive decompression is to achieve adequate neural decompression while decreasing iatrogenic tissue trauma and postoperative spinal instability.[10] Several studies have revealed that the effectiveness of minimally invasive decompression was equivalent to conventional laminectomy in the surgical treatment for lumbar spinal stenosis.[13]
Among various minimally invasive spinal surgery techniques, bipotal technique/endoscopic surgery is an emerging technique for the treatment of disc herniation and lumbar spinal stenosis. In this study, we performed both biportal technique/endoscopic decompression and microscopic decompression using a tubular retractor for lumbar spinal stenosis. Biportal technique/endoscopic decompression surgery provides several advantages with fewer limitations, and sufficient and safe decompression can be performed utilizing the magnified clear view and free handling of instruments. Several studies have shown favorable results by biportal technique/endoscopic decompression surgery in lumbar spinal stenosis.[8,14,15]
Despite the increase in the number of minimally invasive spinal surgeries performed, there are only a few studies in which one surgical procedure is superior to others. The current evidence does not allow strong conclusions to be drawn about the comparative effectiveness of these surgeries. The objective of this study was to compare the effectiveness and safety of biportal technique/endoscopic surgery with microscopic surgery in lumbar spinal stenosis patients.
2. Materials and methods
2.1. Study design and participants
We hypothesized that biportal technique/endoscopic decompression is an effective and safe procedure compared to microscopic decompression in spinal stenosis patients. This prospective, randomized, controlled trial was performed under the Consort guideline. A total of 70 patients who were clinically and radiologically diagnosed with central spinal stenosis in the lumbar spine were included. The patients were recruited from January 2015 to December 2016 at the Korea University, Anam Hospital. The inclusion criteria were neurogenic claudication, unresponsive to conservative treatment, and single-level central canal stenosis without evidence of instability. Exclusion criteria included previous spine surgery, infection, trauma, and tumors. All patients had undergone nonoperative treatment for at least 3 months before surgery. Patients were recommended for surgery if they had failed nonoperative treatment and continued to have significant pain and daily activity restrictions due to neurogenic claudication or radicular pain.
This study was approved by our Institutional Review Board, and informed consent was obtained from each patient (ED14309/K181301). Prior to surgery, 70 patients were randomly divided into 2 groups using computerized randomization: 36 patients received biportal technique/endoscopic surgery and 34 patients received microscopic surgery. One orthopedic spine surgeon from our institute preformed all the operations, and the 2 groups were closely followed for 6 months after surgery. Four patients from each group were lost during the post-operative follow-up period, making the final number of patients from the biportal technique/endoscopic group and the microscopic group 32 and 30 patients, respectively (Fig. 1).
Figure 1.
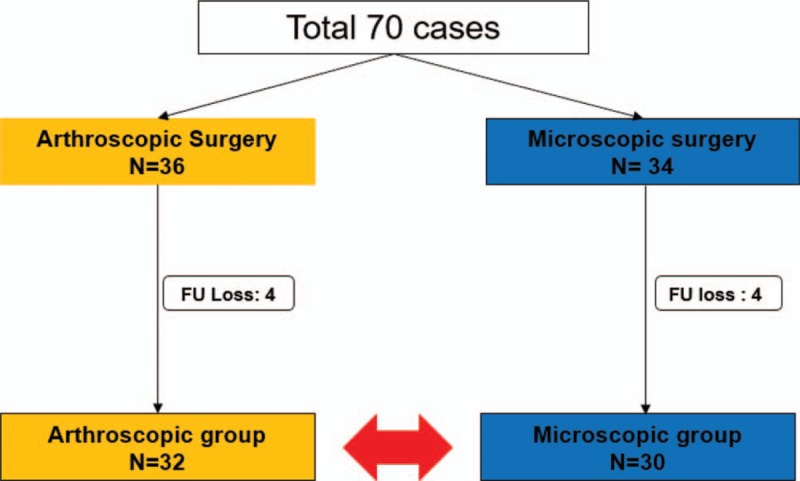
Trial profile.
2.2. Surgical procedures
Both biportal technique/endoscopic and microscopic surgeries were performed with the patient under general anesthesia in the prone position. We have performed unilateral laminotomy with bilateral decompression in both groups.
2.2.1. Biportal technique/endoscopic surgery
Two separate 1 cm-sized skin incisions were made 1 cm above and below the disc space obliquely and 1 cm laterally from the midline (KU; Korea University; portal) (Fig. 2). The first cranial portal was made as a viewing and continuous irrigation portal, and the second caudal portal was made in a more distal direction to be used as a working portal (Fig. 3). A 0° arthroscope was inserted through the viewing portal, and a saline irrigation pump was connected and set to a pressure of 30 mmHg during the procedure. A continuous flow of saline irrigation by irrigation pump was essential to prevent excessive elevation of the epidural pressure. Using the working portal, conventional spinal surgical instruments (Kerrison rongeur, pituitary forcep, and curette) and arthroscopic instruments were freely used in various angles. Ipsilateral decompression was executed by performing partial hemilaminectomy with a burr and the Kerrison rongeur until the superior edge of the deep part of the ligamentum flavum was exposed. The contralateral sublaminar space can be easily viewed by shifting the arthroscope and contralateral decompression was done by undercutting lamina with a burr and the Kerrison rongeur. The ligamentum flavum was carefully dissected from the dura and completely excised (Fig. 4).
Figure 2.
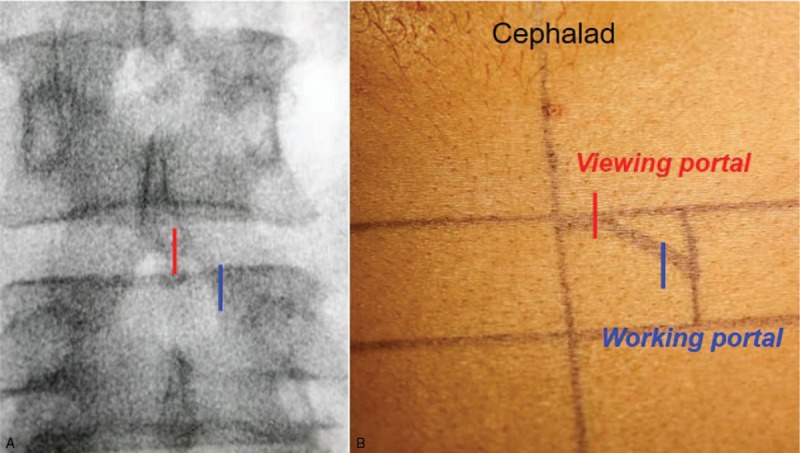
Portal placement in the biportal technique/endoscopic approach. Two separate 1 cm vertical incisions were made obliquely. (A) Portal locations on anteroposterior view of fluoroscopy, (B) Skin entry points.
Figure 3.
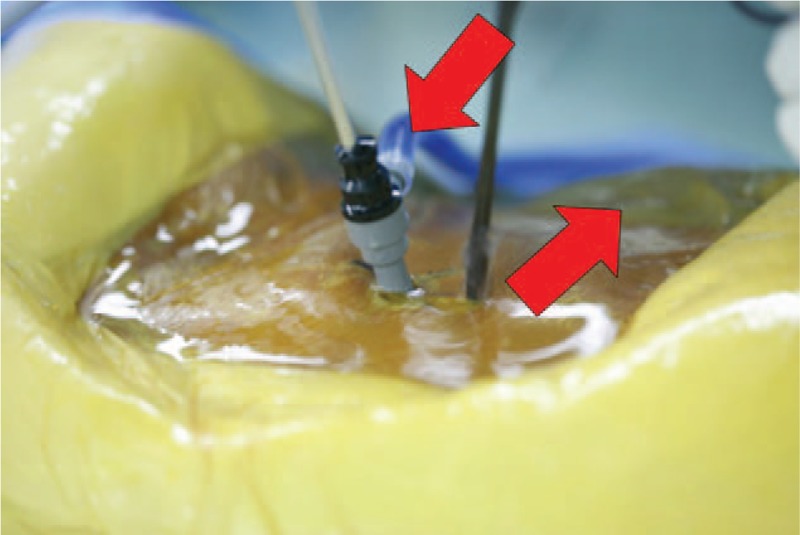
One portal was used for endoscopic viewing and continuous irrigation, and the other portal was used for the insertion and manipulation of instruments. Saline inflow through the cranial viewing portal and outflow through the caudal working portal provides continuous irrigation.
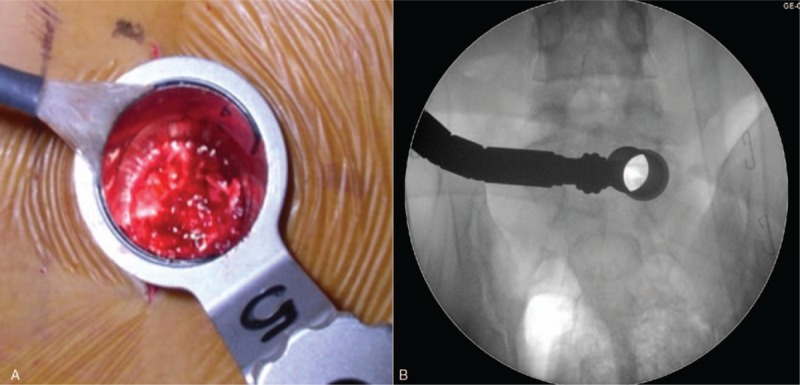
Figure 4.
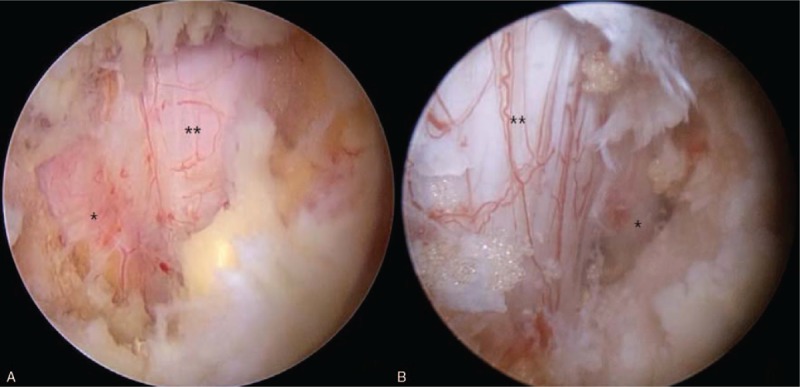
Hemilaminectomy and ligamentum flavum resection was performed. Decompression was confirmed with the freely moving nerve root. A) Ipsilateral decompression, B) Contralateral decompression. (asterisk: exiting root, double asterisk: thecal sac).
2.2.2. Microscopic surgery
A 3 cm skin incision was made with a paramedian approach, slightly lateral (1 cm) to the midline. A muscle splitting technique using the microendoscopic tubular-retractor system left the midline structures, which support muscles and ligaments, intact (Fig. 5). A tubular retractor was placed to create a surgical corridor and expose the lamina at the affected level. Muscle and other soft tissues covering the lamina and medial facet were resected. Unilateral laminectomy was performed with a high-speed burr, exposing the ligamentum flavum. Hypertrophied ligamentum flavum was excised with the Kerrison rongeur and curette.
Figure 5.
A tubular retractor was placed with the muscle splitting technique at the affected level (A) and confirmed with C-arm imaging (B).
2.3. Outcome measures and statistical analysis
All patients completed self-assessment questionnaires and provided demographic and clinical information, including age, sex, diagnosis, and levels of surgery. Clinical outcomes were evaluated with the Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) for back pain. Serial evaluation measures were obtained at baseline and in the postoperative period at the following intervals: immediately postoperative, and 1, 3, and 6 months after surgery. Postoperative data were collected by a different investigator who was blinded to the details of the randomization. Operation time (min), intraoperative blood loss (ml), total hemovac drain output (ml), postoperative opioid consumption (IRcodon 5 mg, T), hospital stay (days), and perioperative complications were compared between the 2 groups.
The endpoints were analyzed by a per-protocol analysis that included all data available from patients in the follow-up period. Differences in mean ODI and VAS scores between the baseline and each postoperative period were assessed with the paired t test. Repeated analysis of covariance was performed to compare the ODI and VAS scores between the 2 groups in each of the follow-up periods. Demographic data, predetermined clinical data, and the incidence of adverse events were compared with the Mann–Whitney U test and Fisher exact test. The level of significance was set at P < .05. All statistical analyses were performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL).
3. Results
3.1. Demographic data
Neither age, gender, level of surgery, nor severity of stenosis showed a significant difference between the 2 groups. The mean age of the biportal technique/endoscopic surgery group patients was 65.1 years and that of the microscopic surgery group was 67.2 years. The 32 patients in the biportal technique/endoscopic surgery group were composed of 18 males and 14 females, and the 30 patients in the microscopic surgery group were composed of 14 males and 16 females. Among the biportal technique/endoscopic surgery group, 4 patients had spinal stenosis at the L3/4 level, 16 at the L4/5 level, and 12 at the L5/S1 spinal level. Among the microscopic surgery group, 5 patients had spinal stenosis at the L3/4 level, 15 at the L4/5 level, and 10 at the L5/S1 spinal level. Severity of stenosis according to Schizas criteria in the biportal technique/endoscopic surgery group showed 3 moderate, 19 severe, and 10 extreme degree, and in the microscopic surgery group showed 1 moderate, 20 severe, and 9 extreme degree (Table 1).
Table 1.
Demographic data.
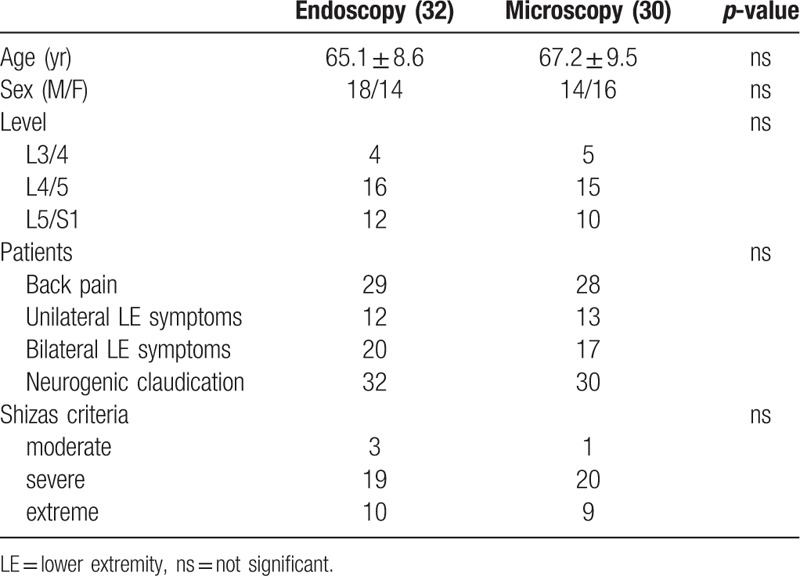
3.2. Clinical data
Most patients (92%) complained of back pain, and all patients had significant unilateral or bilateral buttock and leg pain before the surgery. The most common leg complaints were due to neurogenic claudication. Patients complained of pain, numbness, tingling, or weakness, beginning in the low back and buttocks and radiating into legs after walking (Table 1).
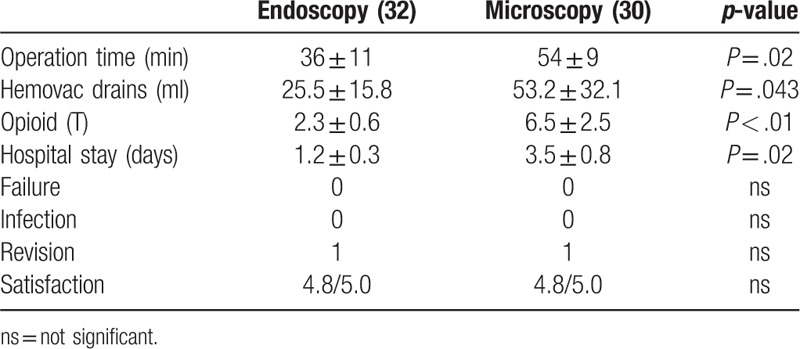
The mean operation time for the biportal technique/endoscopic surgery group was significantly shorter than the microscopic surgery group (36 ± 11 vs 54 ± 9 minutes, P = .02). The hemovac drain output amount of the biportal technique/endoscopic surgery group was significantly less than the microscopic surgery group (25.5 ± 15.8 vs 53.2 ± 32.1 ml, P = .043). The mean amount of postoperative opioid used to manage pain was significantly less for the biportal technique/endoscopic surgery group (2.3 ± 0.6 vs 6.5 ± 2.5 T, P < .01). The duration of the hospital stay after surgery was significantly shorter for the biportal technique/endoscopic surgery group (1.2 ± 0.3 vs 3.5 ± 0.8 days, P = .02). Neither group had any failures or postoperative infection cases, and each group had 1 revision operation case due to postoperative hematoma formation (Table 2).
Table 2.
Clinical data.
The VAS score in the biportal technique/endoscopic surgery group showed 6.3 immediately postoperative and 2.6, 2.2, and 1.6 at 1, 3, and 6 months after surgery, respectively. In the microscopic surgery group, the VAS score was 6.2 immediately postoperative and 3.5, 2.3, and 1.5 at 1, 3, and 6 months after surgery, respectively (Fig. 6). The ODI score in the biportal technique/endoscopic surgery group showed 55 preoperative, 32 immediately postoperative, and 17, 12, and 5 at 1, 3, and 6 months after surgery, respectively. In the microscopic surgery group, the ODI score was 53 preoperative, 31 immediately postoperative, and 21, 11, and 4 at 1, 3, and 6 months after surgery, respectively (Fig. 7). Clinical outcomes using the VAS and ODI scores showed good results in both groups, but the biportal technique/endoscopic surgery group showed lower VAS and ODI scores at 1 month postoperative. Both groups showed similar VAS and ODI scores 6 months after surgery.
Figure 6.
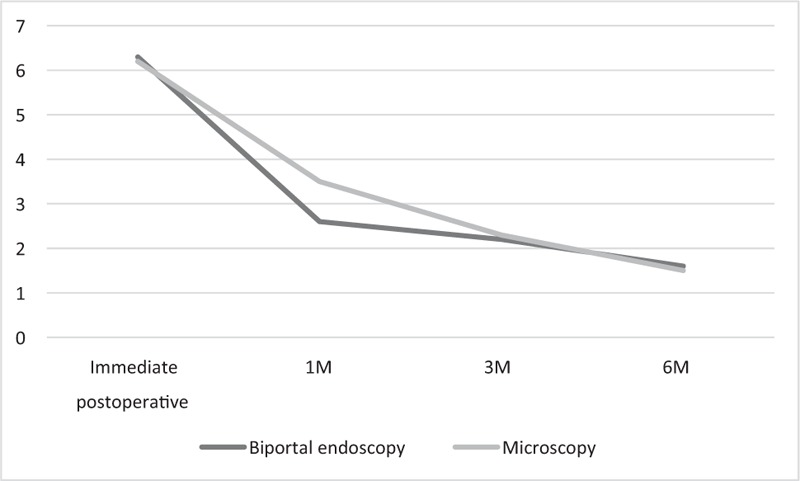
Clinical outcomes compared with the visual analog scale (VAS) (P > .05).
Figure 7.
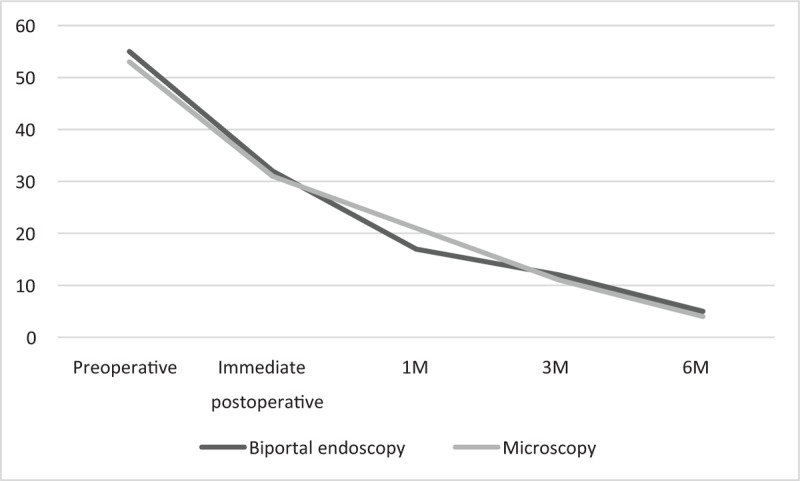
Clinical outcomes compared with the Oswestry disability index (ODI) (P > .05).
4. Discussion
Various techniques of minimally invasive spinal decompression surgery using microscopy, uniportal endoscopy, and biportal technique/endoscopy have shown effective and comparable clinical results compared to conventional open decompression in lumbar spinal stenosis patients. However, which procedures are superior among the minimally invasive spinal surgeries has not been studied. In this prospective, randomized, controlled study, we compared lumbar spinal stenosis patients undergoing unilateral laminotomy with bilateral decompression surgery using biportal technique/endoscopy and microscopy. Biportal technique/endoscopy group showed less pain at the immediate postoperative period, less need for opioids, significantly less pain 1 month after surgery, and the same clinical results and satisfaction at 6 months after surgery compared to microscopic surgery group.
Traditionally, lumbar spinal stenosis was treated with an open decompressive laminectomy and foraminotomy.[3] The overall success rate of such conventional decompression surgery ranges from 62% to 70%.[7] However, the resection of the structures which provide lumbar stability may induce surgery-related secondary postoperative spinal instability.[16] This spinal instability after decompression surgery can cause pain, and additional fusion surgery may be needed. The conventional lumbar spinal stenosis operation involves dissection and retraction of the multifidus muscle, from the spinous processes to expose the lamina, and also damages the delicate posterior dorsal rami.[17] The long duration of multifidus retraction may lead to muscle atrophy and disturbed arteriolar blood supply, resulting in postoperative chronic low back pain. Other possible adverse effects include destruction and denervation of the dorsal branches of the spinal nerve, which may be harmful to stabilization and coordination.[18]
Recently, minimally invasive spinal surgery has been widely performed to reduce the risk of the adverse effects of conventional open surgery.[9] Foley and Smith introduced microendoscopic surgery using the tubular-retractor system and endoscope, which allowed better visualization, maximized muscle sparing, and minimized soft tissue damage.[19] Microscopic unilateral laminotomy with bilateral decompression via a unilateral approach (ULBD) has been used in degenerative lumbar stenosis, with good postoperative outcomes. Mobbs et al[20] compared microscopic ULBD and open laminectomy, and ULBD was equally effective in improving function and more effective for decreasing pain. Nerland et al[13] compared the clinical outcomes of minimally invasive decompression using microscopic and open laminectomy in central lumbar spinal stenosis, and their results showed equivalent effectiveness and favorable outcomes.
Following the improvement of surgical instruments (optics, high-resolution cameras, light sources, high-speed burr, and irrigation pumps), minimally invasive spine surgery can be performed, and endoscopic operations have been performed in many fields. The biportal technique/endoscopic surgery combines the advantages of conventional open surgery and uniportal endoscopic surgery.[21] It allows for a good field of vision of the contralateral, sublaminar, and foraminal areas with high magnification.[14] It uses conventional open spine surgery instruments and ordinary arthroscopic instruments without the need for special endoscopic instruments. This allows free movement and handling as well as angulation of the surgical instruments and the arthroscope, independent of each other, as they are not restricted in a single portal. It also reduces irritation to the nerve roots, and technical flexibility by both sufficient bony and soft tissue work is as possible as much as in conventional open surgery.[22] Finally, continuous saline irrigation can control epidural and bone bleeding, as well as infection.[8]
We achieved a clear visual field with continuous saline irrigation in the working space.[23] A potential space needs to be created because the spine is not a hollow space like the knee or shoulder, and endoscopic visualization of the working instrument and target tissues may not be easy, even with saline pumping and irrigation.[8] An increased risk of dural tears is one of the disadvantages of microscopic tubular decompression surgery.[9] Continuous saline irrigation at 30 mmHg maintains a clear surgical view and causes a slight compression of dura mater, thus widening the epidural space during the procedure and preserving the epidural fat and vessels from damage.[23] Dural tear is uncommon since the ligamentum flavum serves as a protective barrier for the dura mater.[8] Bleeding is more effectively controlled by the radiofrequency bipolar system under continuous irrigation, which also prevents thermal injury.[23]
Mean operation time for biportal technique/endoscopic decompression was 36 minutes, which was shorter than microscopic decompression. It is thought that because fluoroscopy was not used during the operation after preoperative level check. And clear, wide, and excellent arthroscopic visualization and freely moving instruments would also affect the operation time.
Our study's limitations are its small sample size and short length of follow-up. However, it has strength in that it is a prospective, randomized, comparative study.
5. Conclusion
Our study has strength in that it is a prospective, randomized, comparative study. Surgical decompression with biportal technique/endoscopic surgery showed favorable clinical outcomes, less pain and a shorter hospital stay compared to microscopic surgery in patients with lumbar spinal stenosis. Biportal technique/endoscopic surgery could be an alternative treatment for not only lumbar spinal stenosis but also other spinal surgeries.
Author contributions
Conceptualization: Si Young Park, Jong Hoon Park, Seung Woo Suh.
Data curation: Taewook Kang, Si Young Park, Seung Woo Suh.
Formal analysis: Taewook Kang, Si Young Park.
Funding acquisition: Taewook Kang, Si Young Park.
Investigation: Taewook Kang, Si Young Park, Jong Hoon Park.
Methodology: Taewook Kang, Si Young Park, Jong Hoon Park.
Project administration: Taewook Kang, Si Young Park, Chun Hyung Kang.
Resources: Si Young Park, Chun Hyung Kang.
Software: Chun Hyung Kang.
Validation: Soon Hyuck Lee.
Writing – original draft: Taewook Kang.
Writing – review & editing: Si Young Park, Soon Hyuck Lee.
Footnotes
Abbreviations: KU = Korea University, LE = lower extremity, ns = not significant, ODI = Oswestry disability index, ULBD = unilateral laminotomy with bilateral decompression via a unilateral approach, VAS = visual analogue scale.
The authors thank Korea University Research Fund (K1132311).
The authors have no conflicts of interests to disclose.
References
- [1].Hall S, Bartleson JD, Onofrio BM, et al. Lumbar spinal stenosis. Clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med 1985;103:271–5. [DOI] [PubMed] [Google Scholar]
- [2].Issack PS, Cunningham ME, Pumberger M, et al. Degenerative lumbar spinal stenosis: evaluation and management. J Am Acad Orthop Surg 2012;20:527–35. [DOI] [PubMed] [Google Scholar]
- [3].Costa F, Sassi M, Cardia A, et al. Degenerative lumbar spinal stenosis: analysis of results in a series of 374 patients treated with unilateral laminotomy for bilateral microdecompression. J Neurosurg Spine 2007;7:579–86. [DOI] [PubMed] [Google Scholar]
- [4].Djurasovic M, Glassman SD, Carreon LY, et al. Contemporary management of symptomatic lumbar spinal stenosis. Orthop Clin North Am 2010;41:183–91. [DOI] [PubMed] [Google Scholar]
- [5].Parker SL, Godil SS, Mendenhall SK, et al. Two-year comprehensive medical management of degenerative lumbar spine disease (lumbar spondylolisthesis, stenosis, or disc herniation): a value analysis of cost, pain, disability, and quality of life: clinical article. J Neurosurg Spine 2014;21:143–9. [DOI] [PubMed] [Google Scholar]
- [6].Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 2008;33:2789–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Turner JA, Ersek M, Herron L, et al. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine (Phila Pa 1976) 1992;17:1–8. [DOI] [PubMed] [Google Scholar]
- [8].Torudom Y, Dilokhuttakarn T. Two portal percutaneous endoscopic decompression for lumbar spinal stenosis: preliminary study. Asian Spine J 2016;10:335–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ikuta K, Tono O, Tanaka T, et al. Surgical complications of microendoscopic procedures for lumbar spinal stenosis. Minim Invasive Neurosurg 2007;50:145–9. [DOI] [PubMed] [Google Scholar]
- [10].Armin SS, Holly LT, Khoo LT. Minimally invasive decompression for lumbar stenosis and disc herniation. Neurosurg Focus 2008;25:E11. [DOI] [PubMed] [Google Scholar]
- [11].Yagi M, Okada E, Ninomiya K, et al. Postoperative outcome after modified unilateral-approach microendoscopic midline decompression for degenerative spinal stenosis. J Neurosurg Spine 2009;10:293–9. [DOI] [PubMed] [Google Scholar]
- [12].Rahman M, Summers LE, Richter B, et al. Comparison of techniques for decompressive lumbar laminectomy: the minimally invasive versus the “classic” open approach. Minim Invasive Neurosurg 2008;51:100–5. [DOI] [PubMed] [Google Scholar]
- [13].Nerland US, Jakola AS, Solheim O, et al. Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ 2015;350:h1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Eun SS, Eum JH, Lee SH, et al. Biportal endoscopic lumbar decompression for lumbar disk herniation and spinal canal stenosis: a technical note. J Neurol Surg A Cent Eur Neurosurg 2017;78:390–6. [DOI] [PubMed] [Google Scholar]
- [15].Lee JH, Choi K-C, Shim HK, et al. Percutaneous biportal endoscopic surgery for lumbar degenerative diseases. J Minim Invasive Spine Surg Tech 2017;2:15–9. [Google Scholar]
- [16].Abumi K, Panjabi MM, Kramer KM, et al. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine (Phila Pa 1976) 1990;15:1142–7. [DOI] [PubMed] [Google Scholar]
- [17].Johnsson KE, Willner S, Johnsson K. Postoperative instability after decompression for lumbar spinal stenosis. Spine (Phila Pa 1976) 1986;11:107–10. [DOI] [PubMed] [Google Scholar]
- [18].Cooper RG, Mitchell WS, Illingworth KJ, et al. The role of epidural fibrosis and defective fibrinolysis in the persistence of postlaminectomy back pain. Spine (Phila Pa 1976) 1991;16:1044–8. [DOI] [PubMed] [Google Scholar]
- [19].Perez-Cruet MJ, Foley KT, Isaacs RE, et al. Microendoscopic lumbar discectomy: technical note. Neurosurgery 2002;515 Suppl:S129–136. [PubMed] [Google Scholar]
- [20].Mobbs RJ, Li J, Sivabalan P, et al. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine 2014;21:179–86. [DOI] [PubMed] [Google Scholar]
- [21].Heo DH, Son SK, Eum JH, et al. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus 2017;43:E8. [DOI] [PubMed] [Google Scholar]
- [22].Choi DJ, Jung JT, Lee SJ, et al. Biportal endoscopic spinal surgery for recurrent lumbar disc herniations. Clin Orthop Surg 2016;8:325–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Choi CM, Chung JT, Lee SJ, et al. How I do it? Biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir (Wien) 2016;158:459–63. [DOI] [PMC free article] [PubMed] [Google Scholar]


