Abstract
Background/Objective:
Evidence from previous research has shown that the incidence of aphasia following a stroke is high in Nigeria and other countries, and there is a call for intervention programs. The objective of the current study was to investigate the efficacy of cognitive behavior language therapy (CBLT) on aphasia following a stroke.
Methods:
The study was designed as a group randomized trial, which involved treatment and no-treatment control procedures. The participants of the study were 86 patients who had experienced aphasia following a stroke. The Porch Index of Communicative Ability (PICA) and Speech-Language Unhelpful Thoughts and Beliefs Scale (SLUTBS) were the measures used in the study. The repeated measures analysis of variance procedure, with Partial eta squared  , adjusted R2, mean, standard deviation, and upper/lower limit was followed in analyzing the data collected in the study.
, adjusted R2, mean, standard deviation, and upper/lower limit was followed in analyzing the data collected in the study.
Results:
The CBLT intervention significantly reduced aphasia following a stroke and significantly reduced speech-language and unhelpful thought and beliefs among aphasic stroke patients exposed to the treatment intervention when compared with the no-treatment control group.
Conclusion:
Based on the findings of the study, language educators, speech and language pathologists and therapists in education institutions, hospitals, and rehabilitation centers should adopt the principles of CBLT used in the current study to help them improve communication ability among aphasia stroke patients.
Keywords: aphasia, cognitive behavior language therapy, language education, stroke
1. Introduction
The phrase “aphasia following stroke” suggests that a stroke is one of the major causes of aphasia.[1] Though other factors like head trauma, brain tumors, or serious infections can cause aphasia, it appears that aphasia always occurs as a result of injury to the brain after a stroke, especially among older individuals.[1,2] Generally, the term “aphasia” is defined as linguistic impairment or impairment of language associated with a brain lesion in middle-aged or older individuals and sometimes young children.[3] It usually affects the production or comprehension of speech, as well as the ability to read or write.[1] As described further by the National Aphasia Association, aphasia may be severe to the point that communication with the patient becomes nearly impossible. It can also be mild such that communication with the patient is possible. Further, aphasia may affect a single aspect of language use like the ability to retrieve the names of objects; the ability to construct sentences; or the ability to read.[1,2] It is noted that numerous aspects of communication are impaired whenever aphasia is diagnosed. Therefore, aphasia can lead to a range of communication deficits, including language comprehension, language expression, reading, writing, attention, memory, and other cognitive domains.[4]
Previous research findings suggest high incidence of aphasia. For instance, there are 180,000 cases of aphasia per year in the United States.[5] Another study noted that approximately 100,000 stroke survivors are diagnosed with aphasia each year.[4] According to the National Aphasia Association,[1] the incidence of aphasia is expected to reach 180,000 in the year 2020. Another study indicated that 15% of individuals under the age of 65 experience aphasia after their first ischemic stroke.[4] Evidence also shows that the percentage increases to 43% for individuals 85 years of age and older.[6] In a study with Nigerian population,[7] 96% of stroke patients experienced aphasia. Ekeh et al,[8] reported four cases of crossed aphasia seen in their practice within 1 week. Other studies conducted in Nigeria prove that the case of aphasia following stroke is high in Nigeria.[9,10] The present study is inspired by the high level of aphasia cases found in previous studies.
Studies have also established that aphasia following a stroke is associated with increased risk of death,[11] reduced probability of returning to work,[12] and decreased rates of functional recovery,[13] especially when compared with non-aphasic stroke patients.[6] Many aphasic patients experience social isolation and limitations in social participation due to their persisting communication difficulties.[14,15] Also, there is a notable high financial problem among aphasic patient. The cost of treating aphasia following stroke is significantly higher due to the frequent long-term need for rehabilitative services to improve communication abilities.[16] The social impact of aphasia following stroke is persistent and pervasive lasting impact significantly on daily life, causing social isolation, loneliness, a loss of autonomy, restricted activities, role changes, and stigmatization.[15] In Nigeria and other developing countries, the quality of life of individuals suffering from aphasia following stroke is poor.[10,17,18] There is thus a need for intervention programs to be carried out among the aphasia patients in these countries in order to help them improve their communication and social skills.
Meanwhile, evidence from research shows that efficacious speech treatment for aphasia following stroke is available.[2,3,5,6,15] It is unfortunate that the available speech treatment methods for aphasia following stroke are not placing an emphasis on the cognitive and behavioral aspects of the patients. Meanwhile, it may be possible that the aphasic patients’ inability to communicate effectively is related to their cognition and behaviors.[1,5] However, aphasia following stroke in adults is much less responsive to the speech therapies that are available. Cognitive behavioral language program, involving speech restructuring appears to be evidence-based treatment for aphasia following stroke in adulthood.[19] Since aphasia following is stroke is mostly caused by damage on one or more of the language areas of the brain, intervention programs should involve improving cognitive abilities that support the processing of language, such as short-term memory and attention.[1,5] Many aphasic patients are prone to unhelpful thoughts and beliefs that sometimes prolong their recovery even after being subjected to treatment program.[20–22] Through cognitive behavior language therapy (CBLT), the aphasic patients can be helped to change their unhelpful beliefs and judgments, predominantly about the evaluations of others. Therefore, CBLT may cause a significant improvement on the ability of the patients with aphasia following stroke to communicate more effectively. Cognitive behavior language therapy aims to improve aphasia patients’ ability to communicate by helping them to use remaining language abilities, restore language abilities as much as possible, and learn other ways of communicating, including gestures, pictures, or use of electronic devices. This form of therapy involves individual sessions that focus on the specific needs of the patient. There are also group sessions that offer opportunities for aphasic patients to use new communication skills in a small-group setting.
Cognitive behavior language therapy involves the application of the principles of cognitive behavior therapy (CBT) to language defect treatment such as aphasia following stroke. Beck et al[23] and Beck[24] discovered that people often make errors in their thinking that fuel their mental health problems. They hypothesize that people's emotions and behaviors are influenced by their perception of events. In their studies patients are subjected to examine the way thoughts, behaviors, and emotions influence each other. Automatic thoughts are based on core beliefs about self and intermediate beliefs (rules, attitudes, and assumptions). Menzies et al,[19] provided an overview of cognitive-behavior therapy (CBT) strategies that can be applied by speech-language pathologists to treat language deficit disorder. Studies also support the argument that CBT can effectively decrease anxiety and social avoidance and increase engagement in everyday speaking situations for individuals suffering from language impairment.[25] However, the principles of CBT that are used in the current CBLT are drawn from CBT models widely used in clinical psychology, psychiatry, mental counseling, and rehabilitation counseling. Its components include cognitive restructuring, behavioral experiments, and attentional training.[21,25]
In a previous study using a group CBT intervention for 13 adults who stuttered, the authors concluded that CBT was effective for treating individuals with this issue.[22] In another study using CBT with language therapy, Menzies et al,[26] observed that the participants who were exposed to the treatment experienced a significant improvement in their chronic stuttering compared with those who did not partake in the experiment. Though many previous studies with language-related CBT have not focused on aphasia but rather on the treatment of stuttering and other language deficits,[19,21,25] the current researchers argued that CBLT might have a significant, positive effect of aphasia following stroke. Therefore, we, the researchers of the current study hypothesized that CBLT will lead to significant reduction in aphasia following stroke, and significant reduction in speech-language unhelpful thought and beliefs among aphasic stroke patients exposed to the treatment intervention when compared with no-treatment control group.
2. Method
2.1. Ethical consideration
The researchers complied with the ethical standards for conducting human research set by Human Research and Ethics committee of the faculty of Education, University of Nigeria, Nsukka; the American Psychological Association; the National Aphasia Association; the World Health Organisation; the American Medical Association; and the Medical Association of Nigeria. The researchers also complied with the research ethic of the federal university medical center, where the study was conducted. Patients’ rights were maintained throughout the duration of the study, and their informed consent was obtained before inclusion in the study.
2.2. Design
The study was designed as a group randomized trial, which involved a treatment and no-treatment control procedure. This design has become standard for assessing the efficacy of an intervention program.[27] Therefore, the design was suitable for the current study.
2.3. Participants
The participants of the study were 86 aphasia stroke patients (see Table 1 for specific demographic variables). All types of aphasia were considered, including receptive aphasia, expressive aphasia, mixed aphasia, dysphasia, global aphasia, and non-specific. The inclusion criteria maintained by the researchers were: over 50 years old; no known history of severe cognitive decline or mental health problems; no associated disabilities like deafness, blindness, or confusion so severe that the operation is required for assessment and treatment was not possible; speaking and understanding the English language prior to experiencing a stroke; severed aphasia following stroke; high instance of unhelpful speech-language thoughts and beliefs; not participating in any other psychotherapeutic program, psycho-education, language therapy, or speech-language intervention program or therapy; willing to sign an informed consent form; having a caregiver who is willing to be around during the period of treatment; not currently on any aphasia treatment; and able to be present throughout the intervention.
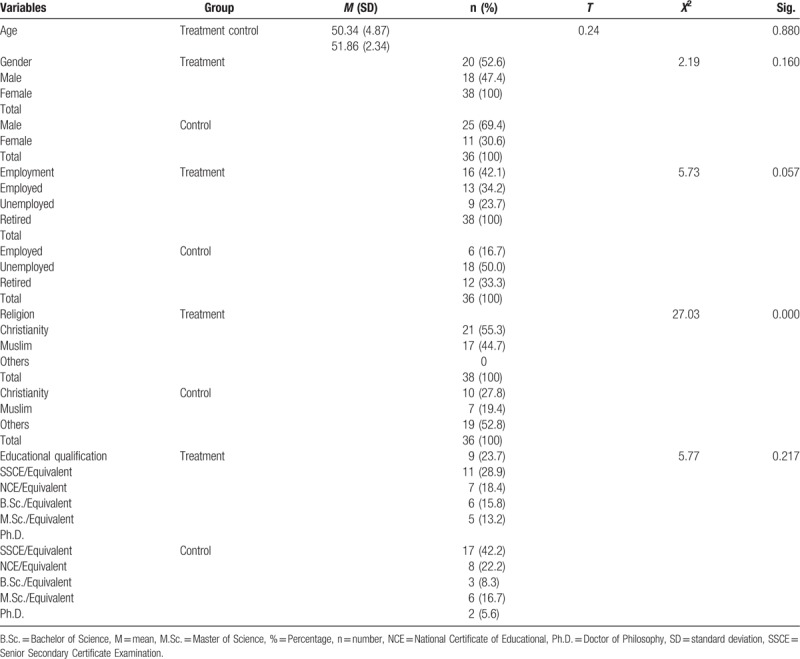
Table 1.
Demographic variables.
The exclusion criterion was non-compliance with any of the inclusion criterion. The researchers excluded participants after the onset of the trial in cases where they were found to be unsuitable for the study. Reasons such as death, further morbidity, patients moving away from the area, patients refusing treatment, and problems with transport were suggested as reasons for patients dropping out. Participants with pre-existing aphasia caused by a non-stroke etiology were excluded from the study, as were all patients who had aphasia resulting from ischemic stroke but for whom this event was a recurrent, rather than the first ischemic stroke, as in previous studies.[6]
2.3.1. Study setting
The study was conducted in a federal university medical center in Akwa Ibom State, Nigeria.
2.4. Measures
2.4.1. Porch index of communicative ability (PICA)
The authors’ modified version of PICA was used to determine the presence and severity of aphasia, using a 3-scale rating of mild; moderate; and severe. The PICA has 20 items that indicate a patient's level of communicative ability.[28–30] Individual mean scores of 2.50 to 3.00 indicate severe aphasia following stroke. This measure was used in previous randomized trials.[28,29,31,32] The internal consistency of the measure was 0.89, using Cronbach α.
2.4.2. Speech-language unhelpful thoughts and beliefs scale (SLUBS)
The design of SLUBS was inspired by the unhelpful thoughts and beliefs scale for stuttering by Menzies et al.[26] The researchers also followed the principles of CBT[24] in writing the contents of the scale. The SLUBS was comprised of 26 items with a response format scaled on a 4 points rating system of: 1 = strongly disagree; 2 = disagree; 3 = agree; and 4 = strongly agree. Individual mean scores of 3.50 to 4.00 indicated a high level of speech-language unhelpful thoughts and beliefs. The validity of the SLUBS was checked by 3 CBT experts, 2 experts in educational measurement and evaluation, and 2 experts in language education. The overall reliability of the SLUBS was a = 0.79.
2.5. Procedures
Recruitment in the study involved contacting 15 speech-language therapists and 5 cognitive-behavioral therapists, working in rehabilitation centers, hospitals, and universities. The therapists visited rehabilitation centers and hospitals to recruit 86 individuals who experienced aphasia following stroke. During the first meeting, we used a clearly concealed randomization procedure to place the participants who met the study's inclusion criteria into treatment and no-treatment groups (n = 43). A random allocation software was used for the allocation to provide unique identifiers in the study.[33] Also, sealed envelopes were used, and the person allocating patients was not aware of the identity of the patient whose name was in the envelope. The person allocating the patients did not have direct patient contact. Patients whose sealed envelopes were inscribed with “T” formed the treatment group while those with “No-T” inscribed envelop formed the no-treatment group. The participants in the treatment group received 4 hours a week of direct therapist contact in a group of 5 patients and also on an individual basis. The meeting was held 2 times per week and each meeting lasted for 2 hours. The participants in the no-treatment group did not receive therapeutic treatment of any kind within the study period.
The 2 measures described in the current study were administered by speech pathologists and cognitive behavior therapists who had no previous interaction with the patients in either the treatment or no-treatment control group. Again, the speech pathologists and cognitive behavior therapist who administered the 2 measures, respectively, were not informed of the type of therapy being provided. The measures were administered 3 times: first as a baseline assessment before the treatment program; second as a post-treatment assessment; and third as a follow-up assessment. In all the measures, the examiners did not review any previous tests for an individual patient until the patient completed the entire protocol. All data were collected at the baseline assessment (Time 1); post-treatment assessment (Time 2); and follow-up assessment (Time 3). Data were analyzed by a professional data analyst who did not take part in the measures administration or the therapy implementation. In order to comply with previous studies, the researchers ensured the CBLT therapists were not involved in the assessment and analysis of data in the study.[34]
2.6. Intervention
2.6.1. Cognitive behavior language therapy (CBLT)
The goal of CBLT is to reduce aphasia following stroke by helping aphasic stroke patients to use their remaining language abilities; restore language abilities as much as possible; and learn other ways of communicating, including using gestures, pictures, or electronic devices. The CBLT for this study was designed for treatment to be 20 sessions over 10 weeks with 4-weeks of follow-up sessions 2 months after completion of initial treatment. There were 2 sessions each week that lasted for 2 hours each. The therapy component consisted of individual sessions that focused on the specific needs of the patient; sessions were also offered opportunity for aphasic patients to use new communication skills in a small-group setting.
The aim of the intervention was achieved by increasing participants’ capacity to attend to alternative cognitive and behavioral targets regarding language use. Through CBLT, the aphasic patients in the current study were encouraged to challenge their language-related negative beliefs. Also, the patients were trained to identify and systematically modify any irrational thoughts related to speech making, language, and communication. Using CBT principles, the intervention program included activities in which the therapies directly targeted specific listening, speaking, reading, or writing skills. The participants learned to identify and dispute their unhelpful thoughts and beliefs, regarding specific language activities such as listening, speaking, reading, and writing skills.
The participants identified and countered unhelpful thoughts and beliefs such as, “people will doubt my ability because I’m having difficulty communicating with them; it's impossible to be really successful in life if you cannot speak clearly; I won’t be able to keep a job if I’m having aphasia; It's all my fault-I should be able to control my speech; I’m a weak person because I have aphasia’; No one will like me if I cannot speak correctly; People focus on every word I say; I am incompetent, among others.” The patients were also helped to indicate the items that they most frequently experienced in consciousness in difficult speaking situations.
The therapists used techniques such as psycho-education about the nature of aphasia following stroke, exposure, behavioral; and cognitive restructuring, and they attempted to help the patients avoid being conscious of their unhelpful thoughts in their speaking situations. These techniques proved successful in a previous study.[22] Using exposure techniques, the patients who participated in the study were exposed to a situation that would normally induce considerable language-specific fear. At that point, the patients were asked to confront the situation without using any avoidance or escape strategies and to remain in the situation until the level of fear begins to diminish. The goal of the technique in the current CBLT program was to help the aphasic patients practice fluency skills in increasingly difficult and feared speaking situations. Exposure in the current CBLT was specifically aimed at providing evidence to counter threat-related expectancies such as “everyone will laugh at me; no one will like me if I cannot speak correctly,” among others. Following previous examples,[19] early exposure sessions began with low-level fear situations while later sessions involved more difficult tasks. The exposure program was repeated until the patient was able to complete it with relative ease.
A behavioral experiment was used to reduce the probability estimates associated with the patients’ fears that they would be evaluated negatively in speaking or writing situations. The experiment was conducted frequently in social situations in which the participants were asked to voluntarily produce speech-language errors and mistakes, ideally in a more severe form than most typically experienced. This technique has been a used as treatment component in several speech-language treatment programs.[6,19,26] Following instructions by the previous authors, the behavioral experiment was presented in a hierarchical manner, moving from relatively non-feared situations through to more feared ones. The participants were asked to record predicted outcomes of the voluntary speech-language errors and mistakes (e.g., “the listener will laugh at me”) prior to engaging in the experiment. The outcomes of the experiments were reviewed, and new predictions were made for further experiments. The participants were encouraged to create experiments to test any of their negative or unhelpful predictions. A worksheet was used for recording observations made during behavioral experiments.
Finally, cognitive restructuring was used to challenge the participants’ identified speech-language related negative and unhelpful thought, beliefs, and judgments. The participants were trained to identify and systematically modify any irrational thoughts related to speech-language, and to use these “reframes” in everyday situations. The participants were made to focus on evidence, in the legal sense of the word, rather than on their personal reasons for believing the negative and unhelpful thoughts. The participants answered questions such as: evidence for their thoughts; evidence they have against their thoughts; what they could tell a friend if they were to have the same thoughts; how their thoughts made them feel; the good things they would gain if they gave up the thoughts among others. Furthermore, the participants were encouraged to consider the severity of possible negative outcomes of feared speech-language situations. Each therapist used several techniques to improve the communication competence of the participants: humor; appropriate tone of voice; verbal and non-verbal support; and recognition that the person with aphasia knew what they wanted to say.
In addition, the CBLT intervention program also involved the direct training of caregivers. The training of caregivers was based on previous evidence that when the aphasia was more severe, treatment programs should involve direct training of caregivers.[5,35] The caregivers were considered as direct communication partners with the responsibility of facilitating and encouraging communicative interactions with their aphasiac patients. The communication partners also led to increased skill practice and generalization to real life situations, in line with previous recommendations.[36]
The caregivers’ training was focused on education about aphasia and its impact on communication, counseling of one or both parties, and strategies for developing communicative success. Emphasis was placed on communication between caregivers and patients. The caregivers also give feedback to the therapist about their patients. Therefore, they were required to attend all of the therapy sessions and to video record interactions during the therapy sessions. They also participated in role-play to practice facilitation strategies. After the sessions, the caregivers were required to help their patients to watch the videos as often as possible before the next meeting. Caregivers were expected to help their patients practice what they learned from the previous sessions. Again, participants’ comprehension was ensured through the use of gestures, key words, or drawings, which simplified the learning process. Caregivers asked fixed-choice questions and gave ample time for response. Responses were verified by using writing to expand upon or summarize what the patients had said.
2.7. Data analysis
Before the analysis, screening for missing values and violation of assumptions was completed, using IBM SPSS, version 22 statistical software (IBM Corp., Armonk, NY). The repeated measures analysis of variance procedure was followed, with Partial eta squared  , adjusted R2, mean, standard deviation, and upper/lower limit. All decisions regarding the significance value were taken at P ≤ .05. Analysis of the demographic variables was done using mean, standard deviation, t test, and chi-square.
, adjusted R2, mean, standard deviation, and upper/lower limit. All decisions regarding the significance value were taken at P ≤ .05. Analysis of the demographic variables was done using mean, standard deviation, t test, and chi-square.
3. Results
The demographic variables in this study are presented in Table 1, where, it can be observed that the mean age of participants in the treatment group was 50.34 ± 4.87 years, while that of those in the control group was 51.86 ± 2.34 years, with no significant difference, t (74) = 0.24, P = .880. In terms of sex, there were 20 (52.6%) male and 18 (47.4%) female participants in the treatment group, while there were 25 (69.4%) males and 11 (30.6%) female participants in the control group, with no significant difference, X2 (1) = 2.19, P = .160. It was also revealed that 16 (42.1%) of the participants in the treatment group and 6 (16.7%) in the control group were employed, while 13 (34.2%) participants in the treatment group and 18 (50.0%) in the control group were unemployed. Nine (23.7%) of the participants in the treatment group and 12 (33.3%) in the control group were retired, with significant difference, X2 = 5.73, P = .05. In terms of religion, 21 (55.3%) in the treatment group and 10 (27.8%) in the control group were Christian, while 17 (44.7%) in the treatment group and 7 (19.4%) in the control group were Muslim, with significant difference, X2 = 27.03, P = .000. In addition, in terms of educational qualifications, 9 (23.7%) of the participants in the treatment group and 17 (42.2%) in the control group had Senior Secondary Certificate Examination (SSCE) or its equivalent; 11 (28.9%) in the treatment group and 8 (22.2%) in the control group had National Certificate in Education (NCE) or its equivalent; 7 (18.4%) in the treatment group and 3 (8.3%) had earned a Bachelor of Science (B.Sc.) or its equivalent; 6 (15.8%) in the treatment group and 6 (16.7%) in the control group had Masters of Science (M.Sc.); 5 (13.2%) in the treatment group and 2 (5.6%) in the control group had earned a Doctor of Philosophy (Ph.D.), with no significant difference, X2 = 5.77, P = .217.
The researchers reported the results of a 3-time assessment of aphasia following stroke, using the PICA and speech-language unhelpful thoughts and beliefs using SLUTBS, respectively in Table 2. As observed in Table 2, there was no significant difference between the treatment and no-treatment control groups in baseline assessment of aphasia following stroke using PICA, F (1,73) = 1.52, P = .220,  , R2 = 0.007. After the CBLT intervention program, the measure indicated a significant reduction in aphasia following stroke among aphasic stroke patients in the treatment group when compared with their counterparts in the no-treatment control group, F (1,73) = 1394, P = .000,
, R2 = 0.007. After the CBLT intervention program, the measure indicated a significant reduction in aphasia following stroke among aphasic stroke patients in the treatment group when compared with their counterparts in the no-treatment control group, F (1,73) = 1394, P = .000,  , R2 = 0.900. Likewise, at the follow-up measure, there was a significant decrease in aphasia following stroke among aphasic stroke patients in the treatment group when compared with their counterparts in the no-treatment control group, F (1,73) = 1712.51, P = .000,
, R2 = 0.900. Likewise, at the follow-up measure, there was a significant decrease in aphasia following stroke among aphasic stroke patients in the treatment group when compared with their counterparts in the no-treatment control group, F (1,73) = 1712.51, P = .000,  , R2 = 0.950. Based on these findings, we concluded that the CBLT intervention program was effective in reducing aphasia following stroke among aphasic stroke patients.
, R2 = 0.950. Based on these findings, we concluded that the CBLT intervention program was effective in reducing aphasia following stroke among aphasic stroke patients.
Table 2.
Repeated-measures ANOVA showing the effect of CBLT intervention program on aphasia following stroke.
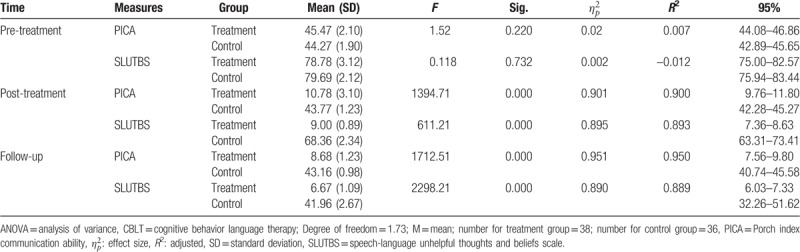
Table 2 indicated that there was no significant difference between the treatment and no-treatment control groups in speech-language and unhelpful thoughts and beliefs before the treatment, F (1,73) = 0.118, P = .732,  , R2 = –0.012. After the CBLT intervention program, the measure indicated a significant reduction in speech-language and unhelpful thoughts and beliefs among aphasic stroke patients in the treatment group when compared with their counterparts in the no-treatment control group, F (1,73) = 611.21, P = .000,
, R2 = –0.012. After the CBLT intervention program, the measure indicated a significant reduction in speech-language and unhelpful thoughts and beliefs among aphasic stroke patients in the treatment group when compared with their counterparts in the no-treatment control group, F (1,73) = 611.21, P = .000,  , R2 = 0.893. In addition, at the follow-up measure, the reduction in speech-language and unhelpful thoughts and beliefs among aphasic stroke patients in the treatment group was maintained when compared with their counterparts in the no-treatment control, F (1,73) = 2298.21, P = .000,
, R2 = 0.893. In addition, at the follow-up measure, the reduction in speech-language and unhelpful thoughts and beliefs among aphasic stroke patients in the treatment group was maintained when compared with their counterparts in the no-treatment control, F (1,73) = 2298.21, P = .000,  , R2 = 0.889. On the whole, the CBLT intervention significantly reduced aphasia following stroke and significantly reduced speech-language and unhelpful thoughts and beliefs among aphasic stroke patients who were exposed to the treatment intervention when compared with no-treatment control group. The authors further presented the results in time by group graphs (see Figs. 1 and 2).
, R2 = 0.889. On the whole, the CBLT intervention significantly reduced aphasia following stroke and significantly reduced speech-language and unhelpful thoughts and beliefs among aphasic stroke patients who were exposed to the treatment intervention when compared with no-treatment control group. The authors further presented the results in time by group graphs (see Figs. 1 and 2).
Figure 1.
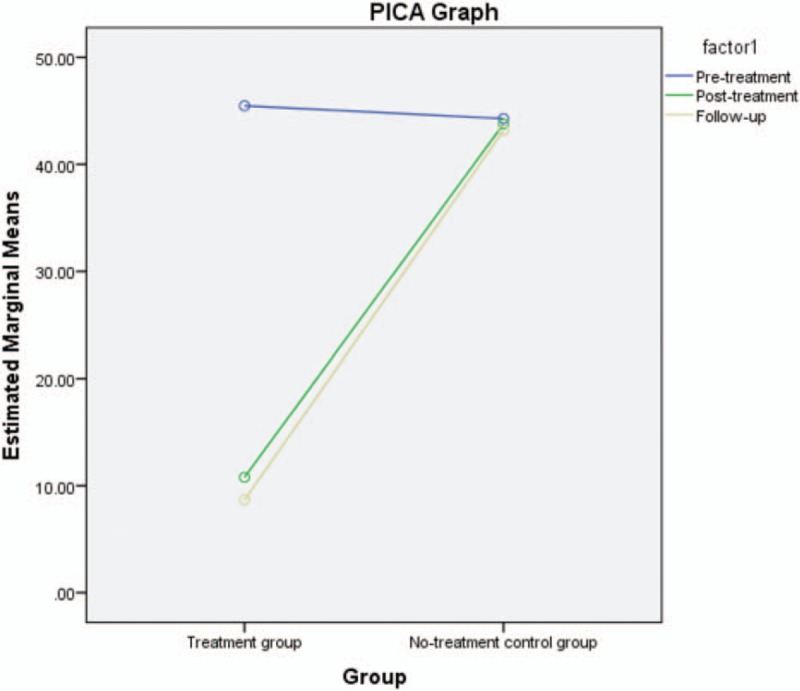
PICA graph. PICA = Porch index of communicative ability.
Figure 2.

SLUTBS graph. SLUTBS = speech-language unhelpful thoughts and beliefs scale.
4. Discussion
The objective of the current study was to investigate the efficacy of CBLT on individuals who experienced aphasia following stroke. Before the CBLT intervention, the researchers confirmed that all of the participants who were approved for the study had severe aphasia following stroke. This supported previous studies, which found the incidence of aphasia is high.[4–6] The finding supports evidence that aphasia following is expected to reach 180,000 in the year 2020.[1] The finding also supported previous studies conducted in Nigerian, which showed evidence of high rate of aphasia following stroke.[7–10] The findings from post-treatment and follow-up sessions revealed a significant reduction in aphasia following stroke among aphasic stroke patients exposed to the CBLT intervention when compared with the no-treatment control group. In other words, the CBLT intervention was efficacious in helping the aphasia stroke patients improve upon their communication abilities. Their degree of aphasia was significantly reduced, and that was why they were able to improve their communication ability. This finding affirmed findings from a previous study, which argued that the most effective, evidence-based treatment for aphasia following stroke in adulthood was a cognitive behavioral language program involving speech restructuring.[19] The findings also supported the previous assertion that intervention program for aphasia following stroke should involve improving cognitive abilities such as short-term memory and attention that support the processing of language.[1,5] The CBLT intervention was effective in improving the cognitive abilities of the participants, and this resulted in improvement in their communication abilities (Fig. 3).
Figure 3.
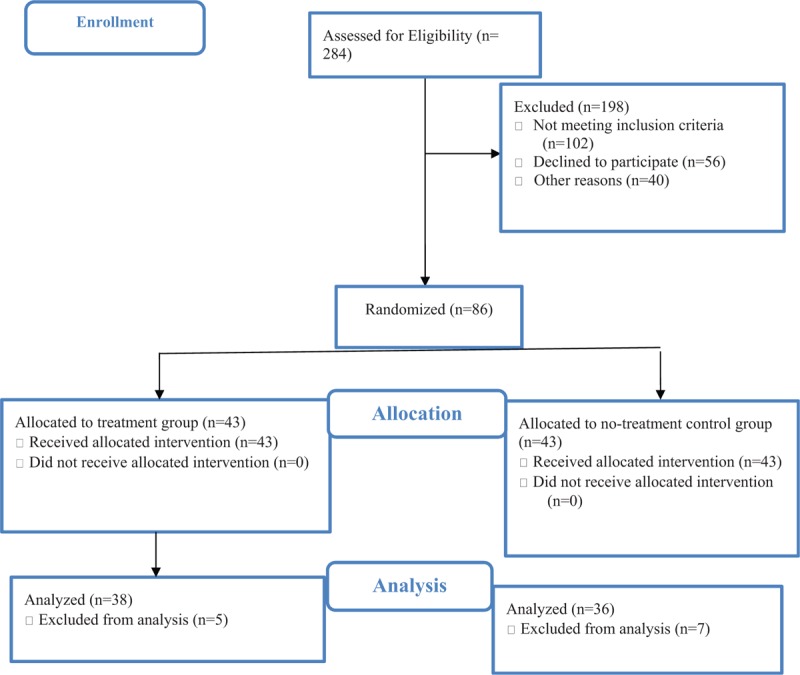
Flow chart.
The study also revealed a significant reduction in speech-language and unhelpful thoughts and beliefs among aphasic stroke patients exposed to the CBLT intervention when compared with the no-treatment control group. Before the intervention, the baseline measure showed that the aphasic stroke patients had high speech-language and unhelpful thoughts and beliefs. This finding supported previous studies, which showed that many aphasic patients were prone to unhelpful thoughts and beliefs that sometimes prolonged their recovery even after participating in a treatment program.[20–22] After being exposed to the CBLT intervention, the patients experienced reductions in their speech-language unhelpful thoughts and beliefs. This showed that CBLT was significant in reducing unhelpful thoughts and beliefs. The finding is in line with Menzies et al,[26] who noted that CBT intervention was effective in improving communication ability among patients with language impairment, and other studies, which noted that speech-language unhelpful thoughts and beliefs were reduced through CBT intervention.[20–22] From our findings, we determined that CBLT intervention can be used to help aphasia stroke patients improve their communication abilities.
5. Limitations
There were limitations for the study, which future studies will need to address. The sample size was small, which may limit generalizability of the results. Based on this limitation, we recommend that future researchers intending to determine the efficacy of CBLT for aphasia following stroke should use larger samples in their investigation. We used only quantitative data for this study. It is important that future studies also use qualitative assessment of aphasia following stroke to further justify the effectiveness of CBLT on aphasia following stroke. Another limitation was that the current study did not consider the interaction effect demographic variables could have had on the findings. It would be helpful for future researchers to analyze how demographic variables such as sex, age, among others, may interact with CBLT intervention for aphasia following stroke.
5.1. Implications for language education research
We recommend that large scale, randomized, controlled trials of CBLT for patients who have aphasia following stroke be conducted in other regions of Nigeria, as well as in other developing countries. These trials should also be conducted by language educators in order to expand the scope of research in language education disciple. If possible, CBLT treatment should be compared with no-treatment in order to confirm the current findings. However, for this research choice to be considered ethical, the patients in the no-treatment control group should be those who would currently not routinely receiving treatment. If the results from such trials confirm that patients experienced reduced symptoms of aphasia after receiving CBLT treatment, it would then be practical to adopt CBLT treatment as part of speech and language intervention plans in language education disciplines.
Another limitation of the study was that the CBLT treatment did not address the satisfaction levels of the patients who received the treatment. Satisfaction on the part of family and caregivers was not surveyed. Therefore, it is recommended that future studies should develop outcome measures, which take these viewpoints into justification. Furthermore, there is need for future research to focus on the level of functional communication on a day-to-day basis in the patients’ own contexts. This will help to further justify the efficacy of CBLT on aphasia following stroke. Again, future researchers may consider the possibility of using social media platforms to deliver CBLT so as to reach long-distant patients. Another implication is that CBLT can be applied to treat other speech and language impairment like stuttering and autism.
6. Conclusion
The findings of the current study demonstrated that CBLT caused significant reduction in aphasia following stroke and significant reduction in speech-language unhelpful thoughts and beliefs among aphasic stroke patients exposed to the treatment intervention, when compared with no-treatment control group. Therefore, it is recommended that language educators in higher education institutions incorporate the principles of CBLT into their curriculum so as to help produce speech and language experts who will be able to apply CBLT intervention to treat aphasia cases among stroke patients. Language educators, speech and language pathologists, and therapists in education institutions, hospitals, and rehabilitation centers should adopt the principles of CBLT used in the current study to help reduce aphasia following stroke among aphasia stroke patients. To ensure this paradigm shift, future studies are urgently needed to further ascertain the efficacy of CBLT in reducing aphasia in another sample of Nigerian stroke patients.
Acknowledgment
The authors thank all the study's participants and assistants. They also thank the therapists, pathologists, and data analysts who participated in the study. They specially acknowledge staff and management of Otusum Consult, Training, and Services for providing technical assistance in the study.
Author contributions
Conceptualization: Amuche Nnamani Nnamani, Mkpoikanke Sunday Otu.
Data curation: Amuche Nnamani Nnamani, Mkpoikanke Sunday Otu.
Formal analysis: Evelyn Ukoha, Olayinka M. Iyekekpolor.
Funding acquisition: Josephine Akabogu, Evelyn Ukoha, Olayinka M. Iyekekpolor.
Investigation: Josephine Akabogu, Evelyn Ukoha, Jacinta Chinwe Omile.
Methodology: Josephine Akabogu, Amuche Nnamani Nnamani, Mkpoikanke Sunday Otu, Anastasia E. Dike.
Project administration: Josephine Akabogu, Amuche Nnamani Nnamani.
Resources: Mkpoikanke Sunday Otu, Annah C. Uloh-Bethels, Maureen Nnenna Obiezu.
Software: Josephine Akabogu.
Supervision: Josephine Akabogu, Annah C. Uloh-Bethels, Maureen Nnenna Obiezu, Anastasia E. Dike.
Validation: Josephine Akabogu, Mkpoikanke Sunday Otu, Annah C. Uloh-Bethels, Maureen Nnenna Obiezu, Anastasia E. Dike.
Visualization: Josephine Akabogu, Chioma Vivian Ike.
Writing – original draft: Mkpoikanke Sunday Otu, Chioma Vivian Ike.
Writing – review & editing: Mkpoikanke Sunday Otu, Jacinta Chinwe Omile.
Mkpoikanke Sunday Otu orcid: 0000-0002-7251-2561.
Footnotes
Abbreviations: PICA = Porch index of communicative ability, SLUTBS = speech-language unhelpful thoughts and beliefs scale.
The authors have no conflicts of interest to disclose.
References
- [1].National Aphasia Association, Association NA. Aphasia Definitions. 2013. [Google Scholar]
- [2].Simmons-Mackie N, Code C, Armstrong E, et al. What is aphasia? Results of an international survey. Aphasiology 2002;16:837–48. [Google Scholar]
- [3].Greener J, Enderby P, Whurr R. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev 2000. CD000425. [DOI] [PubMed] [Google Scholar]
- [4].Ellis C, Urban S. Age and aphasia: a review of presence, type, recovery and clinical outcomes. Top Stroke Rehabil 2016;23:430–9. [DOI] [PubMed] [Google Scholar]
- [5].McLean SC. A Communication Partner Training Program for Individuals With Aphasia Secondary to a Traumatic Brain Injury: A Case Study. USA: Southern Connecticut State University; 2017. [Google Scholar]
- [6].Engelter ST, Gostynski M, Papa S, et al. Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke 2006;37:1379–84. [DOI] [PubMed] [Google Scholar]
- [7].Komolafe MA, Komolafe EO, Fatoye F, et al. Profile of stroke in Nigerians: a prospective clinical study. Afr J Neurol Sci 2007;26:5–13. [Google Scholar]
- [8].Ekeh B, Dike F, Paul W, et al. Acquired crossed aphasia: a report of four cases in Uyo, Southern Nigeria. J Neurol Sci 2015;357:e373. [Google Scholar]
- [9].Owolabi MO. Determinants of health-related quality of life in Nigerian stroke survivors. Trans R Soc Trop Med Hyg 2008;102:1219–25. [DOI] [PubMed] [Google Scholar]
- [10].Owolabi M, Ogunniyi A. Profile of health-related quality of life in Nigerian stroke survivors. Eur J Neurol 2009;16:54–62. [DOI] [PubMed] [Google Scholar]
- [11].Laska A, Hellblom A, Murray V, et al. Aphasia in acute stroke and relation to outcome. J Intern Med 2001;249:413–22. [DOI] [PubMed] [Google Scholar]
- [12].Black-Schaffer R, Osberg J. Return to work after stroke: development of a predictive model. Arch Phys Med Rehabil 1990;71:285–90. [PubMed] [Google Scholar]
- [13].Ellis A. Routledge, The Revised ABCs of Rational-Emotive: Therapy (RET). The Evolution of Psychotherapy: The Second Conference. United Kingdom: 2014. [Google Scholar]
- [14].Mazaux JM, Lagadec T, Panchoa De Sèze M, et al. Communication activity in stroke patients with aphasia. J Rehabil Med 2013;45:341–6. [DOI] [PubMed] [Google Scholar]
- [15].Dalemans RJ, De Witte LP, Beurskens AJ, et al. An investigation into the social participation of stroke survivors with aphasia. Disabil Rehabil 2010;32:1678–85. [DOI] [PubMed] [Google Scholar]
- [16].Ellis C, Simpson AN, Bonilha H, et al. The one-year attributable cost of poststroke aphasia. Stroke 2012;43:1429–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gbiri CA, Akinpelu AO. Quality of life of Nigerian stroke survivors during first 12 months post-stroke. Hong Kong Physiother J 2012;30:18–24. [Google Scholar]
- [18].Vincent-Onabajo G, Adamu A. Impact of poststroke fatigue on health-related quality of life of Nigerian stroke survivors. J Stroke 2014;16:195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Menzies RG, Onslow M, Packman A, et al. Cognitive behavior therapy for adults who stutter: a tutorial for speech-language pathologists. J Fluency Disord 2009;34:187–200. [DOI] [PubMed] [Google Scholar]
- [20].Craig A, Blumgart E, Tran Y. The impact of stuttering on the quality of life in adults who stutter. J Fluency Disord 2009;34:61–71. [DOI] [PubMed] [Google Scholar]
- [21].Craig A, Tran Y. Fear of speaking: chronic anxiety and stammering. Adv Psychiatric Treat 2006;12:63–8. [Google Scholar]
- [22].Ezrati-Vinacour R, Gilboa-Schechtman E, Anholt G, Weizman A, Hermesh H. Association of Behavioral and cognitive therapies, Effectiveness of Cognitive Behaviour Group Therapy (CBGT) for Social Phobia (SP) in People Who Stutter (PWS) With Social Phobia (SP). 5th World Congress of Behavioural and Cognitive Therapies. New York: 2007. [Google Scholar]
- [23].Beck AT, Steer RA, Brown GK. Beck depression inventory-II. San Antonio 1996;78:490–8. [Google Scholar]
- [24].Beck JS. Cognitive Behavior Therapy: Basics and Beyond. New York City: Guilford press; 2011. [Google Scholar]
- [25].Cream A, Onslow M, Packman A, et al. Protection from harm: the experience of adults after therapy with prolonged-speech. Int J Lang Commun Disord 2003;38:379–95. [DOI] [PubMed] [Google Scholar]
- [26].Menzies RG, O’Brian S, Onslow M, et al. An experimental clinical trial of a cognitive-behavior therapy package for chronic stuttering. J Speech Lang Hear Res 2008;51:1451–64. [DOI] [PubMed] [Google Scholar]
- [27].Lee JH, Schell MJ, Roetzheim R. Analysis of group randomized trials with multiple binary endpoints and small number of groups. PLoS One 2009;4:e7265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Porch BE. Porch Index of Communicative Ability: Theory and Development. USA: Consulting Psychologists Press; 1971. [Google Scholar]
- [29].PoRc B. Porch Index of Communicative Ability. Palo Alto, CA: Consulting Psychological Press; 1981. [Google Scholar]
- [30].Martin AD. Aphasia testing: a second look at the Porch Index of Communicative Ability. J Speech Hear Disord 1977;42:547–62. [DOI] [PubMed] [Google Scholar]
- [31].Hartman J, Landau WM. Comparison of formal language therapy with supportive counseling for aphasia due to acute vascular accident. Arch Neurol 1987;44:646–9. [DOI] [PubMed] [Google Scholar]
- [32].Lincoln N, McGuirk E, Berman A, et al. Speech therapy for the stroke patient. Lancet 1984;324:104. [Google Scholar]
- [33].Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol 2004;4:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].David R, Enderby P, Bainton D. Treatment of acquired aphasia: speech therapists and volunteers compared. J Neurol Neurosurg Psychiatry 1982;45:957–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Simmons-Mackie N, Worrall L, Frattali C. Social approaches to the management of aphasia. Neurogenic Commun Disord 2000;2:162–87. [Google Scholar]
- [36].Cunningham R, Ward C. Evaluation of a training programme to facilitate conversation between people with aphasia and their partners. Aphasiology 2003;17:687–707. [Google Scholar]


