Abstract
Patients with persistent or recurrent trigeminal neuralgia (TN) after microvascular decompression (MVD) are frequently difficult to manage. This study aimed to analyze the safety and efficiency of repeat MVD, with the main focus on prognostic factors and long-term outcomes.
We performed a retrospective study of 41 TN patients (19 men, 22 women) who underwent repeat MVD due to persistent or recurrent pain from January 2008 to January 2016. These patients were followed up from 12 to 96 months (mean, 42 ± 17.3 months). Univariate analysis by Spearman's rank correlation coefficient was used for analysis of prognostic factors.
During the repeat MVD, compression of the trigeminal nerve was noted by an artery in 15 patients (36.6%), vein in 6 patients (14.6%), Teflon in 8 patients (19.5%), and no compression in 12 patients (29.3%). Twenty-one patients (51.2%) had already undergone 1 or more previous ablative procedures, either before the first MVD or between the surgeries. The complete pain relief rates of repeat MVD were 87.8% immediately after surgery and 75% at last follow-up. Thirteen patients (31.7%) had new or increased facial numbness after repeat surgery. Univariate analysis revealed 2 prognostic factors, negative finding during reoperation (P = .021) and no pain relief after the initial surgery (P = .038), that showed a negative influence on success rates after repeat MVD.
Repeat MVD can still achieve an excellent outcome in patients with persistent or recurrent pain. However, the risk of facial numbness is increased. Surgeons should be selective in performing repeat MVD, priority should be given to patients who have a pain-free interval after initial MVD or show demonstrable compression on imaging studies.
Keywords: microvascular decompression, outcome, recurrent, trigeminal neuralgia
1. Introduction
Trigeminal neuralgia (TN) is reputed to be one of the most painful conditions characterized by short, unilateral paroxysms of unbearable electric shock-like pain in the distribution of fifth cranial nerve, resulting in significant impairment of the quality of life, and is even known historically as the “suicide disease”. Drug therapy is the first line of treatment and can offer adequate pain relief in most patients.[1] However, if patients who do not respond to medical therapy or have intolerable adverse effects, surgical options should be considered.
Since its first introduction by Dandy[2] and popularization by Jannetta[3], microvascular decompression (MVD) has become a widely accepted treatment for TN and is regarded as the only etiological therapy with the best outcome in terms of long-term pain-free rate.[4] Although the initial success rate is typically high, there are still about 5% of patients experience little or no pain relief after MVD. In addition, 10 to 30% of patients may suffer recurrent neuralgia in the follow-up, with a yearly recurrence risk of 1% to 4%.[5,6] Patients with persistent or recurrent symptoms after MVD may require additional treatment if the neuralgia is medically intractable. However, controversy still exists regarding the optimal surgical option for these patients.
A number of procedures with differing benefits and risks are available for treating TN, including radiofrequency rhizotomy, radiosurgery, and MVD.[1,7] However, patients with persistent or recurrent pain after MVD pose a dilemma: whether to choose the less invasive procedures or the repeat MVD is still a matter of debate. Because of the presumed increased surgery-related risks in repeat MVD, some less invasive procedures have been proposed as safer and more efficient alternatives. However, although these ablative procedures often provide successful short-term relief, the long-term results can be disappointing, with reported success rates of 40% to 50%.[8] Additionally, they are more likely to cause facial numbness, especially the bothersome kind.[9,10]
Repeat MVD has been established as a feasible option for patients with persistent or recurrent TN. However, little is known about the prognostic factors, as well as the long-term outcome. In the present study, we analyzed the clinical features, operative findings, surgical outcomes and complications of 41 patients who underwent repeat MVD due to persistent or recurrent pain, with the main focus on prognostic factors.
2. Material and methods
2.1. Patient population
This is a retrospective study; patients with TN who underwent MVD in our department from January 2008 to January 2016 were retrospectively reviewed and analyzed. Idiopathic TN was diagnosed according to the criteria of the second edition of the International Classification of Headache Disorders.[11] Forty-one patients who underwent repeat MVD due to persistent or recurrent pain after initial surgery were included in this study. Among them, 6 patients were initially treated at other institutions and underwent repeat MVD at our center. The basic characteristics of these patients were analyzed from chart review, including clinical symptoms, demographic data, initial treatment modality; time elapsed to recurrence, retreatment modalities, time between first and repeat MVD, operative findings, surgical outcomes, and complications. Before the second operation, magnetic resonance imaging (MRI) with emphasis on the trigeminal nerve was performed in each patient. This study was approved by the West China Hospital Ethics Committee.
2.2. Operative procedure
As in the initial surgery, the repeat MVD was performed via a standard suboccipital retromastoid craniotomy in the lateral position.[12] The main aim of surgery was to decompress the trigeminal nerve from an offending vessel or the Teflon felt effect. In case of renewed vascular compression, a piece of Teflon felt was inserted between the offending vessel and the trigeminal nerve for decompression. However, if fibrotic adhesion was induced by Teflon felt, microsurgical sharp dissection and complete excision of the Teflon granuloma were performed, and no more Teflon was inserted in case new fibrotic adhesion was induced by foreign material. After the trigeminal nerve was completely freed, the stitched sling retraction procedure was carried out to hold the surrounding artery away from the nerve to prevent further recurrence of symptoms. Furthermore, if no compressing lesions were noted at the time of surgery, we performed the trigeminal root compression procedure to cause minimal trauma (neuropraxia) of the nerve after meticulous dissection and lysis of the surrounding arachnoid.[13]
2.3. Follow-up and outcome assessment
Surgical outcomes were evaluated based on the Barrow Neurological Institute (BNI) Pain Intensity Scale[14] by an independent neurosurgeon who was blinded to the patient management. Then all these patients were followed-up at the outpatient department or by telephone. Surgical outcomes of TN were categorized as complete pain relief (BNI pain score I), partial pain relief (BNI pain score II–III) and failure (BNI pain score IV–V). The surgical outcomes and complications were evaluated at discharge and during follow-up visits.
2.4. Statistical analysis
The mean was expressed ± SD throughout. Descriptive statistics were used to summarize clinical features and patient characteristics. Univariate analysis by Spearman's rank correlation coefficient was used for analysis of prognostic factors. A Kaplan–Meier survival analysis was performed by using the time interval between the date of repeat surgery and the date of failure.
All statistical analyses were performed using SPSS software (version 24.0). Associations were considered statistically significant when P <.05.
3. Results
3.1. Patient characteristics
The 41 patients who underwent repeat MVD surgery for persistent or recurrent TN included 22 females (53.7%) and 19 males (46.3%) with a mean age of 56.7 ± 8.1 years (range, 36–74 years) at the time of repeat surgery. The left side was affected in 18 patients (43.9%) and right in 23 patients (56.1%). The total duration of TN pain since onset was 6.5 ± 4.1 years (range, 2–30 years). The mean interval between the 2 MVD surgeries was 4.6 ± 2.3 years (range, 1.5–12 years). Single division pain was present in 17 patients (41.5%), whereas 24 patients (58.5%) had pain involving multiple divisions. The clinical features of the 41 TN patients are presented in Table 1.
Table 1.
Demographic data and clinical characteristics of the patients with TN who underwent repeat MVD.

In 32 of 41 patients (78%), a pain-free interval after the first MVD was observed, with a mean duration of 26.4 ± 15.7 months (range, 6–72 months). Among them, 18 patients (56.3%) had early recurrences within 2 years. Nine of 41 patients (22%) had no postoperative pain relief. The distribution of pain changed after initial MVD was observed in 22 patients (53.7%). Twenty-three MRI scans showed a vessel in conflict with the trigeminal nerve before repeat MVD, but only 16 of these patients were found to have a vessel in contact at the time of surgery. Fifteen patients had no obvious abnormality on the MRI scan before repeat MVD. Three patients showed suspicious lesion at the site of first surgery. Twenty-one patients (51.2%) had already undergone 1 or more previous ablative procedures, either before the first MVD or between the surgeries, including gamma knife radiosurgery (GKS) in 12 patients, percutaneous glycerol rhizotomy (PGR) in 5 patients, radiofrequency thermorhizotomy (RFT) in 8 patients and peripheral nerve procedures in 6 patients.
3.2. Operative findings
Marked to severe adhesions were observed in all of the 41 patients during the second MVD. Compression of the trigeminal nerve was noted by an artery in 15 patients (36.6%), vein in 6 patients (14.6%), or Teflon in 8 patients (19.5%). Furthermore, no vascular compression was encountered in 12 patients (29.3%) (Table 2). Among the 21 patients with vascular compression, a piece of Teflon felt was inserted between the offending vessel and the trigeminal nerve for decompression. In 8 patients of these patients, a careful and complete excision of the Teflon felt was carried out. In 12 patients, trigeminal root compression was performed due to the negative exploration during the repeat operation.
Table 2.
Operative findings to be responsible for TN in these patients who underwent repeat MVD.

3.3. Surgical outcomes and complications
Thirty-six patients (87.8%) achieved complete pain relief without medication immediately after the surgery, 3 patients (7.3%) achieved partial pain relief, and only 2 patients (4.9%) failed to obtain pain relief immediately after the operation. The patients in this cohort were followed up from 12 to 96 months (mean, 42 ± 17.3 months). One patient was lost to follow-up and was not included in any statistical analyses. At the last follow-up, 30 patients (75%) were pain-free without medication, 7 patients (17.5%) suffered from partial pain relief in different degrees and 3 patients (7.5%) failed to obtain pain relief (Table 3). The Kaplan–Meier curve of pain relief patients is presented in Figure 1.
Table 3.
Surgical outcomes and complications of the 41 TN patients who underwent repeat MVD.

Figure 1.
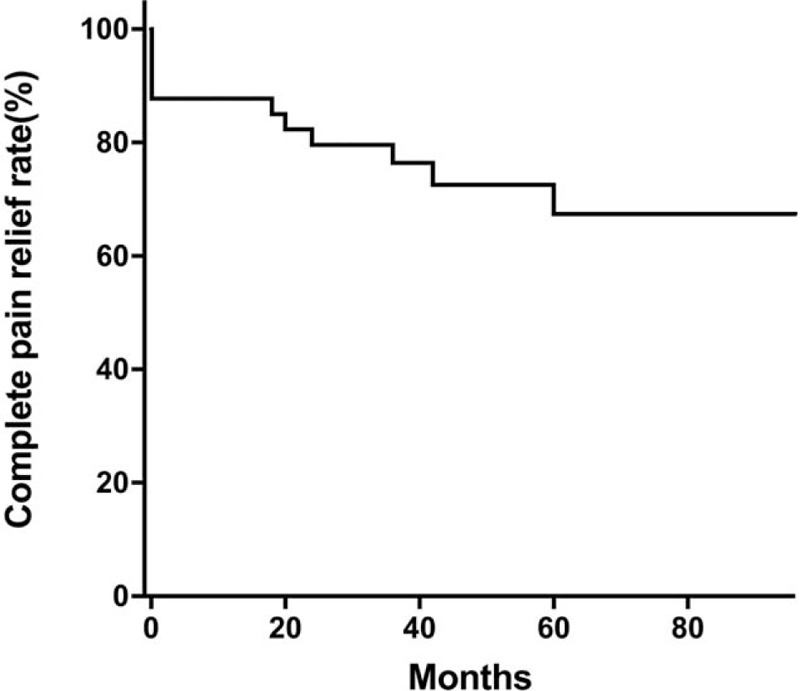
Kaplan–Meier survival graph showing the probability of complete pain relief after repeat MVD in patients with persistent or recurrent pain. MVD = microvascular decompression.
After repeat MVD, no patient suffered severe complications such as death, stroke, or paralysis. Thirteen patients (31.7%) had new or increased facial numbness after surgery; only 5 patients (12.2%) reported that this increased sensory loss was bothersome. Other postoperative complications included hearing loss in 2 patients (4.8%), cerebrospinal fluid leak in 1 patient (2.4%) and wound infection in 1 patient (2.4%) (Table 3). Most of these postoperative complications were reversible and only 9.7% of patients experienced varying degrees of complications at the last follow-up visit.
3.4. Prognostic factors
Univariate analysis showed that negative finding at exploration was a significant determining factor for long-term failure of repeat MVD (P = .021). Furthermore, the analysis also showed that patients who experienced no postoperative pain relief after the initial surgery tended to have a worse surgical outcome after repeat MVD (P = .038). Other factors, such as age, sex, pain duration, or previous ablative procedures, did not influence success rates.
4. Discussion
4.1. Reoperation for TN after failed MVD
Based on the hypothesis that vascular compression of the trigeminal nerve plays a major role in the etiology of TN, MVD has become widely accepted as the gold standard surgical procedure for treating this disease.[1,15] Previous studies have shown that immediate pain relief after MVD occurs in about 90 to 95% of patients,[4,15] hence, nearly one-tenth of TN patients will experience little or no pain relief at all. Furthermore, although the initial pain relief rate is high, some patients may develop recurrent symptoms in the follow-up.[6] Barker et al[4] described the long-term results of MVD in 1185 TN patients, the results showed that 30% of the patients had recurrences of pain during the study period of 6.2 years. Sindou et al[15] reported 17% of TN patients experienced recurrence of neuralgia after 15 years of follow-up. The recurrence of TN symptoms after MVD often develops within the first 2 years. There are several factors that may associate with poor outcomes after MVD, including female sex, younger age, longer pain duration, atypical features, venous compression, and occurrence of intraoperative trigeminocardiac reflex (TCR).[4,6,16,17]
Controversy still exists regarding the use of repeat MVD for persistent or recurrent neuralgia after failed MVD. One criticism of repeat MVD is the possibility that posterior fossa surgery may be more difficult and hazardous due to the development of adhesive arachnoidal bands and scar tissue. Meanwhile, some studies have suggested that repeat surgery is associated with less favorable outcomes, and the postoperative complications are more frequent than the previous MVD.[18,19] Therefore, most neurosurgeons recommend less invasive procedures to achieve pain relief in patients with failed MVD. However, some authors strongly believe that MVD is the procedure with the highest likelihood of providing a permanent cure, the surgical complications are rare and mortality is negligible in experienced hands, hence, they conclude that repeat MVD is a feasible therapeutic option in patients with persistent or recurrent pain.[20–22]
4.2. Operative findings during repeat MVD
Our intraoperative findings in 41 patients during repeat surgery are quite different from those reported in the first MVD. Marked to severe adhesions were observed in all of the patients. In addition, a high percentage of venous compression was present during the repeat MVD. Besides, 29.3% of patients showed negative explorations in the repeat surgery. Compression by veins or no compression is also common in repeat MVD among other similar studies. Lee et al conducted a research to demonstrate the cause of recurrent TN in 32 patients caused by veins during the initial MVD; they found that development of new veins around the nerve root was observed in 28 cases (87.5%) in the repeat surgery. Hence, they concluded that the development and regrowth of new veins was the most common cause of recurrence.[23] Furthermore, Cho et al performed the repeat MVD in 31 TN patients, among the repeat operations, they found that there was negative exploration in 16 patients (52%) and venous compression in 4 patients (13%).[24] The negative explorations during the repeat surgery suggested that there may be an intrinsic factor causing the recurrence of symptom in some patients with TN.
Notably, almost 20% of patients had significant compression secondary to Teflon felt in this series. Many surgeons have confirmed that adhesion of the interposed foreign material was a significant cause of TN recurrence after MVD.[21,25,26] Lots of materials have been used to separate the offending vessels from the trigeminal nerve, such as muscle, cotton, Ivalon sponge and Teflon felt. Teflon felt has been thought to be an ideal material because of its tissue acceptance, little dislocation and the lack of resorption.[27] However, it also has some complications, the major one is inflammatory foreign body reaction, which may cause severe adhesion, fibrotic change, or even granulomatous formation around the trigeminal nerve and lead to the recurrence of TN. The reported incidence of Teflon granuloma after MVD is about 5%.[25,28] However, this might have been underestimated because Teflon-induced granulomas might be present in patients who have not undergone a repeat operation. For those recurrent patients caused by Teflon felt related fibrotic adhesion, we suggest that the Teflon felt-fibrotic tissue should be completely removed without inserting a new Teflon felt between the offending vessel and the trigeminal nerve. Because the Teflon felt showed potential fibrotic reaction in some patients, additional foreign material may induce new foreign body reaction. In addition, we also suggest that the stitched sling retraction procedure may be a good choice to hold the surrounding artery away from the trigeminal nerve to prevent further recurrence of symptoms in the repeat MVD.
4.3. Long-term outcome and prognostic factors of repeat MVD
Our results showed that the complete pain relief rates of repeat MVD were 87.8% immediately after surgery and 75% at last follow-up, which were similar to that reported in patients who underwent initial MVD.[4,15] The results of the present study demonstrated that repeat surgery can still achieve an excellent outcome in patients with persistent or recurrent pain after MVD. However, we found there was a high incidence of transitory or permanent trigeminal sensory impairment in the present series. The results showed that 31.7% of patients had new or increased facial numbness after surgery. However, in our previous study, only 5% of patients developed facial numbness after first time MVD. Hence, the risk of facial numbness seems greater after repeat MVD when compared with our previous results. However, there is same problem in other similar studies. Amador et al reported 52% of patients had facial numbness after repeat posterior fossa exploration.[26] Bakker et al found that 27% of patients suffered from facial numbness after repeat MVD.[19] Several possible reasons have been proposed to explain this phenomenon. First, repeat surgery is often complicated by severe adhesions and abnormal anatomical relationships, and even careful dissection may cause damage to neurovascular structures. Second, surgeons frequently perform a partial nerve section if there is no compelling compressive lesion at the time of repeat surgery. Hence, the chance of trigeminal nerve injury in this situation is comparable with destructive procedures. We, therefore, advocate performing a limited neurolysis. In this series, if no compressing lesions were noted at the time of surgery, trigeminal root compression was performed to cause minimal trauma of the nerve after meticulous dissection and lysis of the surrounding arachnoid.[13] Third, most patients have already undergone 1 or more previous ablative procedures at the time of repeat MVD, which may increase the susceptibility to damage of trigeminal nerve. Given the potential risk and high complication rate of repeat MVD, we used to hold the concept of initially attempting less invasive surgeries after a failed MVD. Nonetheless, repeat MVD remains an appropriate and effective rescue therapy, especially if less invasive operations do not provide successful pain relief.
The present study revealed 2 prognostic factors, negative finding during reoperation and no pain relief after the initial surgery that showed a negative influence on success rates after repeat MVD. This means patients who show no compressing lesions at repeat surgery are significantly related to poorer long-term results. In addition, patients who experience no postoperative pain relief after the initial surgery tend to have a worse surgical outcome after repeat MVD. These results suggest that surgeons should be selective in performing repeat MVD. Therefore, it is important to recognize that not all failed cases would be able to benefit from repeat MVD, but only patients who have a pain-free interval after initial MVD or show demonstrable compression on imaging studies.
This study has some limitations. First, all of the study subjects were from a single treatment center, which might have introduced bias. Second, this study is a retrospective research with limitations inherent to the study design. In addition, the sample size is not large enough, and there is no control group. However, we can still infer that conclusions based on the analysis of results in 41 patients with persistent or recurrent TN, although the conclusions are not firm enough. Future large sample-size multi-center prospective case-control studies are further needed to confirm the results demonstrated in the present analysis.
5. Conclusions
Our study demonstrated that repeat MVD can still achieve an excellent outcome in patients with persistent or recurrent pain. However, the risk of facial numbness seems greater than that in initial MVD. Furthermore, we found 2 prognostic factors, negative finding during reoperation and no pain relief after the initial surgery, that showed a negative influence on success rates after repeat MVD. The results of the present study are useful in counseling patients regarding treatment after failed MVD. We suggest that surgeons should be selective in performing repeat MVD; priority should be given to patients who have a pain-free interval after initial MVD or show demonstrable compression on imaging studies, especially if less invasive surgeries have not relieved their pain.
Author contributions
Conceptualization: Jian Cheng, Xuhui Hui.
Data curation: Jian Cheng, Ding Lei.
Formal analysis: Jian Cheng, Jinli Meng, Ding Lei, Xuhui Hui.
Investigation: Jian Cheng.
Methodology: Jian Cheng, Ding Lei, Xuhui Hui.
Project administration: Jian Cheng.
Resources: Ding Lei, Xuhui Hui.
Software: Jian Cheng.
Supervision: Ding Lei.
Validation: Jian Cheng, Jinli Meng.
Visualization: Jinli Meng, Xuhui Hui.
Writing – original draft: Jian Cheng, Jinli Meng, Ding Lei, Xuhui Hui.
Writing – review & editing: Jian Cheng, Jinli Meng, Ding Lei, Xuhui Hui.
Footnotes
Abbreviations: MRI = magnetic resonance imaging, MVD = microvascular decompression, TN = trigeminal neuralgia.
The authors have no conflicts of interest to disclose.
References
- [1].Bennetto L, Patel NK, Fuller G. Trigeminal neuralgia and its management. BMJ 2007;334:201–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Dandy W. Concerning the cause of trigeminal neuralgia. Am J Surg 1934;24:447–55. [Google Scholar]
- [3].Jannetta PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg 1967;26suppl 1:159–62. [DOI] [PubMed] [Google Scholar]
- [4].Barker FG, 2nd, Jannetta PJ, Bissonette DJ, et al. The long-term outcome of microvascular decompression for trigeminal neuralgia. New Engl J Med 1996;334:1077–83. [DOI] [PubMed] [Google Scholar]
- [5].Sanchez-Mejia RO, Limbo M, Cheng JS, et al. Recurrent or refractory trigeminal neuralgia after microvascular decompression, radiofrequency ablation, or radiosurgery. Neurosurg Focus 2005;18:1–6. [DOI] [PubMed] [Google Scholar]
- [6].Theodosopoulos PV, Marco E, Applebury C, et al. Predictive model for pain recurrence after posterior fossa surgery for trigeminal neuralgia. Arch Neurol 2002;59:1297–302. [DOI] [PubMed] [Google Scholar]
- [7].Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ 2014;348:g474. [DOI] [PubMed] [Google Scholar]
- [8].Huang CF, Chiou SY, Wu MF, et al. Gamma Knife surgery for recurrent or residual trigeminal neuralgia after a failed initial procedure. J Neurosurg 2010;113:172–7. [DOI] [PubMed] [Google Scholar]
- [9].Kanpolat Y, Savas A, Bekar A, et al. Percutaneous controlled radiofrequency trigeminal rhizotomy for the treatment of idiopathic trigeminal neuralgia: 25-year experience with 1,600 patients. Neurosurgery 2001;48:532–4. [DOI] [PubMed] [Google Scholar]
- [10].Kondziolka D, Zorro O, Lobato-Polo J, et al. Gamma Knife stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg 2010;112:758–65. [DOI] [PubMed] [Google Scholar]
- [11].Society HCCotIH. The International Classification of Headache Disorders: 2nd edition. Cephalalgia: An International Journal of Headache. 2004; 24 suppl 1:9–160. [DOI] [PubMed] [Google Scholar]
- [12].Zhang H, Lei D, You C, et al. The long-term outcome predictors of pure microvascular decompression for primary trigeminal neuralgia. World Neurosurg 2013;79:756–62. [DOI] [PubMed] [Google Scholar]
- [13].Cheng J, Lei D, Zhang H, et al. Trigeminal root compression for trigeminal neuralgia in patients with no vascular compression. Acta Neurochir 2015;157:323–7. [DOI] [PubMed] [Google Scholar]
- [14].Rogers CL, Shetter AG, Fiedler JA, et al. Gamma knife radiosurgery for trigeminal neuralgia: the initial experience of The Barrow Neurological Institute. Int J Radiat Oncol Biol Phys 2000;47:1013–9. [DOI] [PubMed] [Google Scholar]
- [15].Sindou M, Leston J, Decullier E, et al. Microvascular decompression for primary trigeminal neuralgia: long-term effectiveness and prognostic factors in a series of 362 consecutive patients with clear-cut neurovascular conflicts who underwent pure decompression. J Neurosurg 2007;107:1144–53. [DOI] [PubMed] [Google Scholar]
- [16].Tyler-Kabara EC, Kassam AB, Horowitz MH, et al. Predictors of outcome in surgically managed patients with typical and atypical trigeminal neuralgia: comparison of results following microvascular decompression. J Neurosurg 2002;96:527–31. [DOI] [PubMed] [Google Scholar]
- [17].Spiriev T, Sandu N, Kondoff S, et al. Tic and autonomic symptoms. J Neurosurg 2012;116:1397–8. [DOI] [PubMed] [Google Scholar]
- [18].Rath SA, Klein HJ, Richter HP. Findings and long-term results of subsequent operations after failed microvascular decompression for trigeminal neuralgia. Neurosurgery 1996;39:933–8. [DOI] [PubMed] [Google Scholar]
- [19].Bakker NA, Van Dijk JM, Immenga S, et al. Repeat microvascular decompression for recurrent idiopathic trigeminal neuralgia. J Neurosurg 2014;121:936–9. [DOI] [PubMed] [Google Scholar]
- [20].Yang DB, Jiang DY, Chen HC, et al. Second microvascular decompression for trigeminal neuralgia in recurrent cases after microvascular decompression. J Craniofac Surg 2015;26:491–4. [DOI] [PubMed] [Google Scholar]
- [21].Schmieder K, Scholz M, Hardenack M, et al. Surgical treatment of recurrent trigeminal neuralgia. Minim Invasive Neurosurg 1999;42:47–50. [DOI] [PubMed] [Google Scholar]
- [22].Pollock BE, Stein KJ. Surgical management of trigeminal neuralgia patients with recurrent or persistent pain despite three or more prior operations. World Neurosurg 2010;73:523–8. [DOI] [PubMed] [Google Scholar]
- [23].Lee SH, Levy EI, Scarrow AM, et al. Recurrent trigeminal neuralgia attributable to veins after microvascular decompression. Neurosurgery 2000;46:356–61. [DOI] [PubMed] [Google Scholar]
- [24].Cho DY, Chang CG, Wang YC, et al. Repeat operations in failed microvascular decompression for trigeminal neuralgia. Neurosurgery 1994;35:665–9. [DOI] [PubMed] [Google Scholar]
- [25].Gu W, Zhao W. Microvascular decompression for recurrent trigeminal neuralgia. J Clin Neurosci Off J Neurosurg Soc Australasia 2014;21:1549–53. [DOI] [PubMed] [Google Scholar]
- [26].Amador N, Pollock BE. Repeat posterior fossa exploration for patients with persistent or recurrent idiopathic trigeminal neuralgia. J Neurosurg 2008;108:916–20. [DOI] [PubMed] [Google Scholar]
- [27].Capelle HH, Brandis A, Tschan CA, et al. Treatment of recurrent trigeminal neuralgia due to Teflon granuloma. J Headache Pain 2010;11:339–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Chen J, Lee S, Lui T, et al. Teflon granuloma after microvascular decompression for trigeminal neuralgia. Surg Neurol 2000;53:281–7. [DOI] [PubMed] [Google Scholar]


