Abstract
Rationale:
Chronic intestinal pseudo-obstruction (CIPO) and pneumatosis cystoides intestinalis (PCI) are rare abdominal diseases and the pathological mechanisms have not been fully elucidated. Systemic sclerosis (SSc), which is characterized by the progressive sclerotic changes of skin and internal organs, is a refractory collagen disease and is frequently associated with digestive disorders including CIPO.
Patient concerns:
A 68-year-old woman who has been well managed for SSc over the long term, who presented with abdominal fullness for the first time.
Diagnoses:
Abdominal X-ray and computed tomography (CT) images showed PCI with pneumoperitoneum findings. Based on the diagnosis of CIPO, we evaluated the intestinal peristalsis of the patient by using cine magnetic resonance imaging (MRI).
Interventions:
Oral medications of 15 g/d of Daikenchuto, 750 mg/d of Metronidazole and Sodium Picosulfate were started for improving the bowel peristaltic movement and decreasing intestinal gas production.
Outcomes:
A great improvement of CIPO and PCI by multidrug therapy without any surgical treatments for such an unusual case.
Lessons:
This case indicates that SSc can be accompanied with not only CIPO but also PCI as digestive disorders and that cine MRI, which is a definitely beneficial imaging modality, can intelligibly visualize the peristalsis of the intestines and lead to successful medical control by noninvasive treatment.
Keywords: chronic intestinal pseudo-obstruction, pneumatosis cystoides intestinalis, systemic sclerosis
1. Introduction
Chronic intestinal pseudo-obstruction (CIPO) is a rare abdominal disease that causes recurrent symptoms such as abdominal distension, abdominal pain, and vomiting due to an intestinal motility disorder without mechanical obstructions.[1–3] However, the pathological mechanisms of CIPO have not been fully elucidated, and therapeutic guidelines for CIPO have not been established. Systemic sclerosis (SSc), which is characterized by the progressive sclerotic changes of the skin and internal organs, is a refractory collagen disease and the aetiology is still unknown.[4] SSc can cause systemic sclerosis-related symptoms, such as Raynaud phenomenon, scleroderma, pulmonary fibrosis, and scleroderma renal crisis and is frequently associated with digestive disorders including gastroesophageal reflux disease and CIPO.[1] Pneumatosis cystoides intestinalis (PCI) is also a comparatively unusual disease and is divided into 2 groups: primary PCI and secondary PCI, from chronic obstructive pulmonary disease, asthma, some digestive diseases, etc. Some collagen diseases can also be one of the major origins of secondary PCI.[5]
2. Case report
A 68-year-old woman, who has been well managed for her SSc condition using 5 mg/d of prednisone as a maintenance dosage for the past 6 years, was admitted to our hospital with mild abdominal fullness for 3 months for the first time. On admission, physical examination showed only mild abdominal fullness without tenderness and rebound tenderness in her entire abdomen. Abdominal X-ray and contrast-enhanced computed tomography (CT) images showed PCI and pneumoperitoneum findings without mechanical obstructions (Figs. 1 and 2). In spite of the significant imaging findings, there was no critical complaint from the patient, and there were no abnormalities in any of the laboratory results or blood and faecal culture examinations.
Figure 1.

Abdominal computed tomography (CT) examinations on admission: (A) abdominal CT image showed gas in the wall of the small bowel indicative of pneumatosis cystoides intestinalis (arrows). Intestinal dilatation of the small bowel was noticeably observed. B, Abdominal CT image showed exacerbation of intraperitoneal free gas indicative of pneumoperitoneum (arrow heads).
Figure 2.
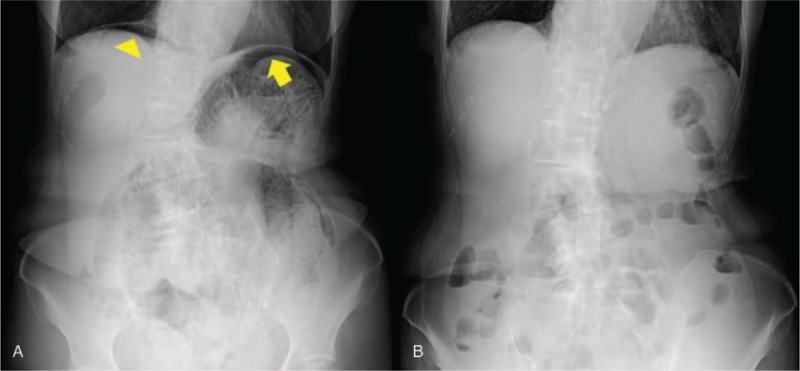
Abdominal X-ray images on admission (A) and posttreatment (B): (A) abdominal X-ray image showed gas in the wall of the small bowel indicative of pneumatosis cystoides intestinalis (arrows). Intestinal dilatation of the small bowel was noticeably observed and showed exacerbation of intraperitoneal free gas indicative of pneumoperitoneum (arrow heads). B, Pneumatosis cystoides intestinalis and intraperitoneal free gas had disappeared.
According to the image findings, we diagnosed as initial onset of CIPO from SSc accompanied with PCI and pneumoperitoneum and planned further investigations for her bowel peristaltic activity by using cine MRI with observation under fasting state.
This patient underwent cine MRI before initiation of treatment (Fig. 3). All images were acquired on a 3.0-Tesla (3T) Siemens MAGNETOM trio. To make clear visualization of the distended small intestine, the patient drank 500 mL of water before the examination of cine MRI. The each successive scan of cine MRI was gotten within about 1 second. The cine MRI images showed manifest peristaltic malfunction in the right lower small bowel, whereas sufficient intestinal movement with PCI findings could be observed in the left upper small bowel (Fig. 3). Intestinal dilatation of the small bowel was noticeably seen in the entire small intestine.
Figure 3.

Cine MRI findings before initiation of treatment. A, Cine MRI images showed that sufficient intestinal movement could be observed in the upper left small bowel (arrows). B, Cine MRI images showed manifest peristaltic malfunction with pneumatosis cystoides intestinalis in the right lower small bowel (arrow heads). Intestinal dilatation of the small bowel was noticeably observed. MRI = magnetic resonance imaging.
Based on the results of cine MRI, we started multidrug therapy including 15 g/d of Daikenchuto, 750 mg/d of Metronidazole and Sodium Picosulfate for improving the bowel peristaltic movement and decreasing intestinal gas production. After confirming the improvement of abdominal fullness, we re-evaluated her bowel peristaltic activity by using 3T cine MRI and could find the crucial amelioration of peristaltic movement, especially in the right lower small bowel, which had mainly shown the peristaltic malfunction, and the marked reduction of intestinal gas volume (Fig. 4). The observation suggests that the peristaltic malfunction of a part of the small intestine might be the origin of her digestive disorder, which occurred from SSc. Finally, the patient was discharged from our hospital and has been able to keep in satisfactory intestinal condition with stable medical status by continual multidrug therapy in our outpatient clinic without any surgical interventions for around 1 year.
Figure 4.

Cine MRI findings after initiation of multidrug treatment: Cine MRI images demonstrated obvious improvement of pneumatosis cystoides intestinalis and intestinal dilatation of the small bowel (arrow heads). Moreover, peristaltic malfunction in the right lower small bowel was definitely improved. MRI = magnetic resonance imaging.
3. Discussion
Intestinal pseudo-obstruction, which has high morbidity and mortality, is a rare abdominal disease first reported by Dudley et al in 1958. The cause may be primary or secondary from various diseases. The patient presents abdominal symptoms without mechanical obstructions in the intestinal tract. The clinical course is characterized by chronic symptoms of intestinal obstruction such as abdominal pain, fullness, vomiting, etc. CIPO usually lacks specific laboratory findings, biological markers and symptoms, and the symptoms are similar to those of the other peristaltic dysfunctional diseases. In addition, it often takes a lot of time to get an accurate CIPO diagnosis because of the nonspecificity.[1–3] Therefore, CIPO patients have sometimes undergone unnecessary surgery.
The annual morbidity rate of CIPO was reported as 0.212/100,000 in men and 0.237/100,000 in women, and there was no significant difference in morbidity rate by sex.[2] The clinical course of CIPO is mostly severe due to the progressive deterioration of intestinal function. Oral nutrition is gradually difficult for most CIPO patients and finally parenteral nutrition would be needed. The main causes of death are septic shock and complications related to total parenteral nutrition and surgery.[1] Although CIPO is included in benign functional diseases, the prognosis is poor, and the 10-year survival rate is only 60% to 80%.[3]
Currently, conventional modalities, such as radiation opaque markers, hydrogen breath test, and small intestine manometry, to approach whole small bowel for evaluating the peristaltic malfunction, were insufficient.[6] With an array of high-resolution MRI imaging now available, the utility of MRI for functional assessing of CIPO was actually reported.[7] In addition, cine MRI, which has been used for cardiac functional assessment with a high-temporal resolution, was gradually applied for the evaluation for bowel motility without radiation exposure.[8] Accordingly, we conducted the evaluation by using cine MRI for the patient and could precisely assess the patient's entire intestinal peristalsis, and the efficacy of multidrug therapy by using 3T cine MRI result in the patient can be managed conservatively without any surgical interventions.
The purposes of treatment for CIPO are the improvement of bowel peristalsis, the suppression of intestinal bacteria overgrowth, and the decompression inside the small intestine. In general, both the mechanical obstruction of the small intestine and peristaltic malfunctional diseases including CIPO can cause the bacterial overgrowth in the small intestine, which results in overproduction of gas inside the small bowel.[9] According to the previous study, we could control gas volume in the small intestine by using Metronidasole.[10,11] Interestingly, we confirmed by 3T cine MRI that the peristaltic malfunction of the patient was locally occurred in the lower part of the small bowel. It suggests that the local occurrence of peristaltic malfunction can be the origin of CIPO and lead to secondary PCI in the patient with SSc. When medical treatment cannot control the CIPO state, percutaneous endoscopic gastro-jejunostomy (PEG-J) tube should be considered an available therapeutic tool. Previous studies showed that PEG-J could reduce the intestinal pressure of the patient with poor oral intake, which results in the amelioration of oral intake.[9,12]
4. Conclusion
The case presented here demonstrates that SSc can be accompanied with CIPO with PCI as digestive disorders, and 3T cine MRI, which is definitely a beneficial imaging modality, can intelligibly visualize peristalsis of the intestines, which can lead to successful medical control by noninvasive treatment.
Author contributions
Data curation: Takashi Kobayashi, Nanako Ogawa.
Investigation: Yuki Mitsuyoshi, Kazuki Takakura.
Methodology: Toshiyuki Sakurai, Masanori Nakano.
Resources: Taro Ukichi, Yozo Ishiuji.
Supervision: Yuichi Torisu, Masayuki Saruta.
Writing – original draft: Yuki Mitsuyoshi.
Writing – review & editing: Kazuki Takakura.
Footnotes
Abbreviations: CIPO = chronic intestinal pseudo-obstruction, CT = computed tomography, MRI = magnetic resonance imaging, PCI = pneumatosis cystoides intestinalis, SSc = systemic sclerosis.
Informed written consent was obtained from the patient for publication of this case report and accompanying images.
The authors have no conflicts of interest to disclose.
References
- [1].Antonucci A, Fronzoni L, Cogliandro L, et al. Chronic intestinal pseudo-obstruction. World J Gastroenterol 2008;14:2953–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Iida H, Ohkubo H, Inamori M, et al. Epidemiology and clinical experience of chronic intestinal pseudo-obstruction in Japan: a nationwide epidemiologic survey. J Epidemiol 2013;23:288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Fuyuki A, Ohkubo H, Higurashi T, et al. Clinical importance of cine-MRI assessment of small bowel motility in patients with chronic intestinal pseudo-obstruction: a retrospective study of 33 patients. J Gastroenterol 2017;52:577–84. [DOI] [PubMed] [Google Scholar]
- [4].Adler BL, Russell JW, Hummers LK, et al. Symptoms of autonomic dysfunction in systemic sclerosis assessed by the COMPASS-31 questionnaire. J Rheumatol 2018;45:1145–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lee YS, Han JJ, Kim SY, et al. Pneumatosis cystoides intestinalis associated with sunitinib and a literature review. BMC Cancer 2017;17:732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Grønlund D, Poulsen JL, Sandberg TH, et al. Established and emerging methods for assessment of small and large intestinal motility. Neurogastroenterol Motil 2017;29:e13008. [DOI] [PubMed] [Google Scholar]
- [7].Menys A, Butt S, Emmanuel A, et al. Comparative quantitative assessment of global small bowel motility using magnetic resonance imaging in chronic intestinal pseudo-obstruction and healthy controls. Neurogastroenterol Motil 2016;28:376–83. [DOI] [PubMed] [Google Scholar]
- [8].Khalaf A, Nowak A, Menys A, et al. Cine MRI assessment of motility in the unprepared small bowel in the fasting and fed state: beyond the breath-hold. Neurogastroenterol Motil 2019;31:e13466. [DOI] [PubMed] [Google Scholar]
- [9].Di Nardo G, Karunaratne TB, Frediani S, et al. Chronic intestinal pseudo-obstruction: progress in management? Neurogastroenterol Motil 2017;29:e13231. [DOI] [PubMed] [Google Scholar]
- [10].Stanghellini A, Cogliandro RF, De Giorgio R, et al. Chronic intestinal pseudo-obstruction: manifestations, natural history and management. Neurogastroenterol Motil 2007;19:440–52. [DOI] [PubMed] [Google Scholar]
- [11].Dull JS, Raufman JP, Zakai MD, et al. Successful treatment of gastroparesis with erythromycin in a patient with progressive systemic sclerosis. Am J Med 1990;89:528–30. [DOI] [PubMed] [Google Scholar]
- [12].Ohkubo H, Fuyuki A, Arimoto J, et al. Efficacy of percutaneous endoscopic gastro-jejunostomy (PEG-J) decompression therapy for patients with chronic intestinal pseudo- obstruction (CIPO). Neurogastroenterol Motil 2017;29:e13127. [DOI] [PubMed] [Google Scholar]


