Abstract
Rationale:
Real-time three-dimensional navigation systems can provide useful information for operators during surgery. The authors report a case of synovial chondromatosis of the temporomandibular joint treated by open surgery under the guidance of a real-time 3-dimensional navigation system with a 3-point rigid cranial fixation device.
Patient concerns:
A 73-year-old woman presented with swelling in the left preauricular region and left temporomandibular joint pain.
Diagnoses:
The patient was diagnosed with synovial chondromatosis of the temporomandibular joint by imaging examinations.
Interventions:
The patient was treated by open surgery under the guidance of a real-time 3-dimensional navigation system with a 3-point rigid cranial fixation device.
Outcomes:
The patient was diagnosed with synovial chondromatosis by histopathological examination. There were no complications. The real-time 3-dimensional navigation system with a 3-point rigid cranial fixation device provided an accurate and useful navigation image and clear surgical field during the surgical procedure. Thirty months have passed since the operation without clinical findings associated with recurrence.
Lessons:
The guidance provided by a real-time 3-dimensional navigation system with a 3-point rigid cranial fixation device is useful in open surgery for the treatment of synovial chondromatosis of the temporomandibular joint.
Keywords: real-time 3-dimensional navigation systems, synovial chondromatosis, temporomandibular joint, 3-point rigid cranial fixation device
1. Introduction
Real-time 3-dimensional navigation systems can provide objective anatomical information for operators during surgery.[1] In neurosurgery, intraoperative navigation systems have been particularly used in order to confirm the position of instrumentation in real time because intracranial tumors may be clinically indistinct from the surrounding normal tissue.[2] In recent years, the usefulness of real-time 3-dimensional navigation systems in oral and maxillofacial surgery has been reported, and there exist some studies on open surgery of the temporomandibular joint (TMJ) under the guidance of a navigation image.[1–3]
Synovial chondromatosis (SC) is a benign condition characterized by the formation of cartilaginous nodules that may become pedunculated and detached from the synovial membrane, becoming loose bodies within the joint space.[4,5] SC was histologically classified into 3 phases by Milgram as follows: an active intrasynovial disease alone, with no loose bodies, transitional lesions with both active intrasynovial proliferation and free loose bodies, and multiple free osteochondral bodies with no demonstrable intrasynovial disease.[6] Although the etiology of SC is still not entirely clear, cases of SC are divided into primary SC and secondary SC depending on the presence or absence of obvious initiating factors such as trauma or joint disease.[7] Primary SC is considered to be more aggressive and to have a higher incidence of recurrence than secondary SC.[7] Common symptoms of SC of the TMJ are pain, tenderness, swelling, limitation of jaw movement, and joint sound.[5] Imaging examinations such as conventional x-rays, computed tomography (CT), and magnetic resonance imaging (MRI) are helpful in the diagnosis of SC and confirmation of the extent of the lesion.[5] Usually, arthroscopic surgery or open surgery is chosen for the treatment of SC of the TMJ.[5]
Firm fixation of a real-time 3-dimensional navigation system reference point is important to obtain accurate images because shifting of the reference point from the initial fixed position leads to a loss of accuracy of the navigation image. Additionally, the reference point fixed to a patient's body or head may interfere with the surgical field. The reference point should not be fixed directly to the patient's body or head to solve the problems described above. In this paper, the authors report a case of SC of the TMJ treated by open surgery under the guidance of a real-time 3-dimensional navigation system with a 3-point rigid cranial fixation device.
2. Consent
Written informed consent was obtained from the patient for publication of the case and any accompanying images.
3. Case report
A 73-year-old woman presented to the authors’ department complaining of swelling in the left preauricular region and left TMJ pain. She had experienced left TMJ pain during chewing for 25 years. She had no history of maxillofacial trauma. A physical examination revealed swelling in the left preauricular region. The interincisal opening was 45 mm, and the deviation of the jaw toward the left side during mouth opening was 3 mm. A panoramic radiograph, lateral oblique transcranial projection, and CT revealed multiple radiopaque bodies surrounding the left condyle. A T2-weighted MRI revealed a mass containing hypointense loose bodies. A CT and MRI showed that the lesion was separated from the intracranial fossa by the thin temporal bone. The results of the imaging examination suggested a diagnosis of SC.
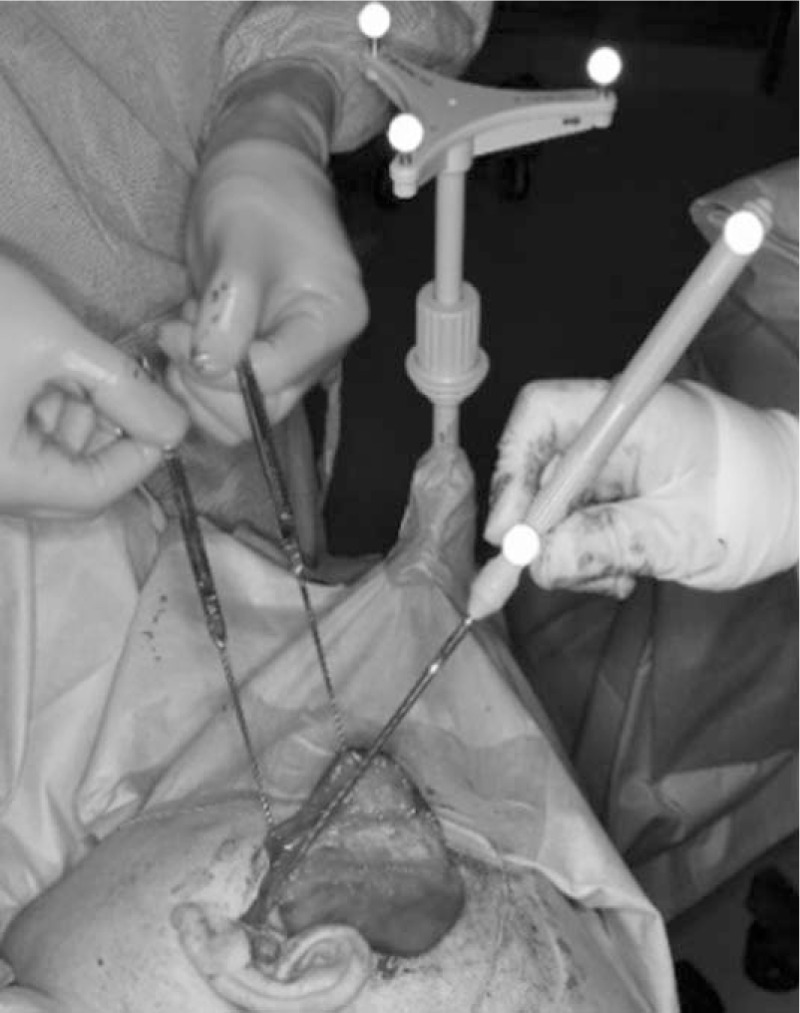
The authors performed open surgery on the patient under general anesthesia to treat SC with the guidance of a real-time 3-dimensional navigation system. The posture of the patient was changed from a supine position to an operative position (i.e., the right lateral decubitus position). The patient's head was fixed with a radiotranslucent 3-point rigid cranial fixation device by experienced neurosurgeons in order to prevent changes in the head's position during surgery. To obtain the surgical field, the authors chose the forehead and the occipital region as the areas of insertion of the 3 pins of a 3-point rigid cranial fixation device (DORO Skull Clump Radiolucent, pro med instruments Inc., Freiburg, Germany). A reference point was fixed to the 3-point rigid cranial fixation device using a radiotranslucent adapter kit (Headholder Adapter for Doro and Mayfield and Reference Array Intraop Imaging Cranial, BrainLAB Inc., Heimstetten, Germany) in order to prevent displacement from an initial fixed position during surgery and interference with the surgical visual field when the authors performed open surgery using a modified preauricular temporal approach (Fig. 1).[8] Then, preoperative thin-cut (1.0 mm) CT scan data were obtained, which were imported to a real-time 3-dimensional navigation system (iPLAN, BrainLAB Inc., Heimstetten, Germany). The authors performed open surgery using a modified preauricular temporal approach after confirming a match between the navigation image and the patient's anatomical landmarks (the tragus, infraorbital edge, etc.). Loose bodies in the upper joint space were confirmed when the authors opened the TMJ capsule. The authors confirmed the surgical field through the navigation image after all of the visible loose bodies were removed, revealing the remaining loose bodies in the area where the authors’ instruments had not reached (Figs. 2 and 3). Then, the authors tried to remove the remaining loose bodies under the guidance of the navigation image while the mandible was moved in order to make space for removing them. Consequently, the authors were able to remove 44 loose bodies (Fig. 4). The authors did not perform discectomy and synovectomy on the basis of intraoperative findings that the disc was in a normal position without perforation and there was no abnormal synovial tissue. The calcification of these loose bodies was confirmed by histological examination. The authors diagnosed the patient with phase 3 SC according to Milgram classification using intraoperative findings and postoperative histopathological examination. After surgery, swelling in the left preauricular region and left TMJ pain disappeared. Further, there have been no findings suspected of damaging vital structures, such as postoperative bleeding, neurologic symptoms, ear symptoms, and so on. In addition, there have been no complications related to a 3-point rigid cranial fixation device. Depressed skin on the forehead and the occipital region caused by the pin headrest healed soon, and no visible scars were observed. Thirty months have passed since the operation without clinical findings associated with recurrence.
Figure 1.

Under general anesthesia, the patient's head was fixed at points of the forehead and the occipital region with a 3-point rigid cranial fixation device. A navigation system reference point was fixed to the device.
Figure 2.
In open surgery of the TMJ using a modified preauricular temporal approach, the reference point separated from the patient provided us a surgical field without interference. TMJ = temporomandibular joint.
Figure 3.
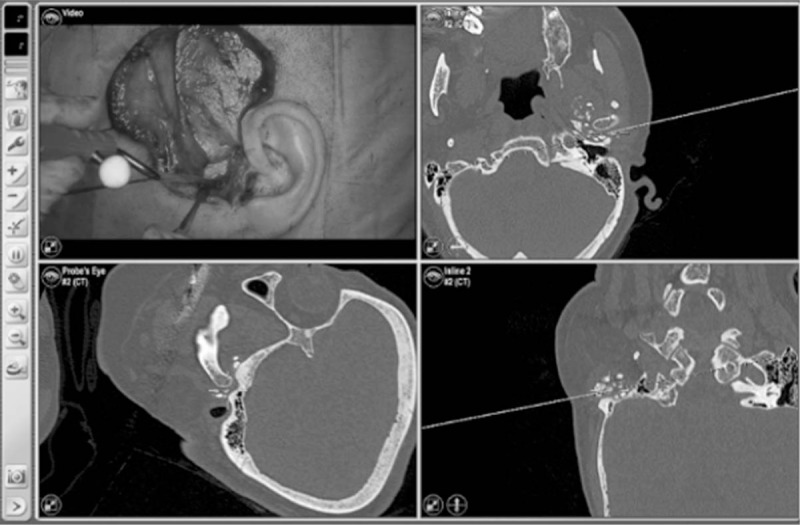
Calcified loose bodies around the condyle could be confirmed during surgery using an accurate real-time 3-dimensional navigation image. The upper left image shows the intraoperative image of the surgical approach with the periarticular flap reflected. The lower left image shows a perpendicular view of the instrument axis that contains the instrument tip. The upper right image shows a reconstruction plane spanned by the instrument axis in a vertical direction. The lower right image shows a perpendicular view of the upper right image, namely the reconstruction plane is spanned by the instrument axis in a horizontal direction.
Figure 4.
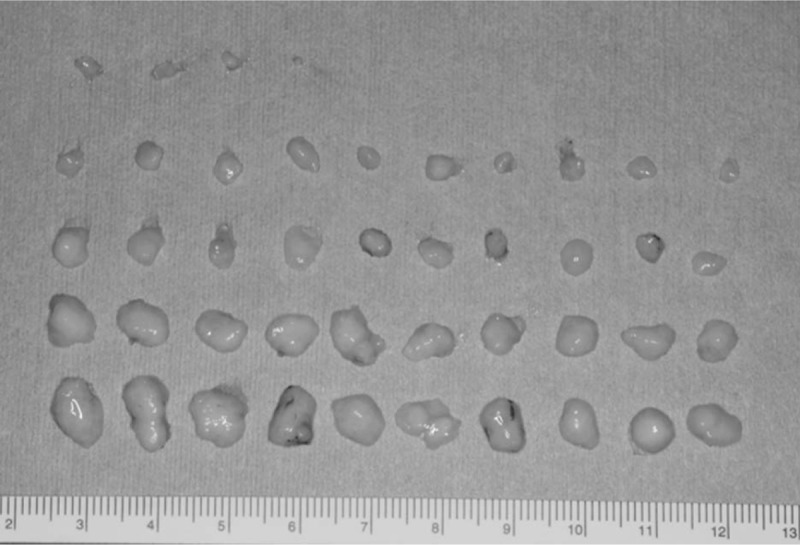
Loose bodies.
4. Discussion
The use of the navigation system during surgical procedures may be helpful when applied to patients with complicated disease conditions.[9] There are some vital structures around the TMJ such as the middle ear, middle cranial fossa, vessels, and nerves.[10] There is a high risk of damaging these vital structures under subjective visual assessment in open surgery of TMJ. Furthermore, delicate surgical procedures are needed in a small visual field in the TMJ capsule. Therefore, the guidance of the real-time 3-dimensional navigation system is useful to perform accurate and safe open TMJ surgery. Additionally, the authors suggested that it can be helpful to construct a navigation image using the results of intraoperative or immediate presurgical imaging examinations because the mandibular fossa and intracranial fossa are separated by a thin temporal bone.[10] In addition, SC is likely to progress to the intracranium, and mandibular fossa is occasionally absorbed regardless of the presence or absence of the lesion.[11] If time passes after the image examination is carried out, there is a possibility that the absorption of a temporal bone will occur regardless of the presence or absence of the lesion and the mandibular fossa communicate with the intracranium.
Collyer noted that the unpredictable movement of an anesthetized patient affects the accuracy of the navigation image.[2] In neurosurgery, a 3-point rigid cranial fixation device is usually used to firmly fix the patient's head, and a navigation system reference point is fixed to the device with an adapter kit.[2] In this case, a real-time 3-dimensional navigation system with a 3-point rigid cranial fixation device provided us accurate and useful navigation images during the surgical procedure. Additionally, the authors obtained a clear surgical field without interference by reference point because it was not directly fixed to the patient's head. This allowed us to perform open surgery of the TMJ without complications.
There have been few reports on pin headrest complications.[12] However, the fixation of the patient's head with a 3-point rigid cranial fixation device must be carried out in a proper procedure before the initiation of surgery in order to prevent pin headrest complications, such as skull fracture, epidural hematoma, and so on.[12]
Milgram suggested that synovectomy may not be necessary in phase 3 of SC of Milgram classification.[6] The recommended treatment for SC consists of removal of the loose bodies and resection of the abnormal synovial tissue.[13] Sato et al[14] reported a case of SC in which they removed loose bodies without discectomy and synovectomy on the basis of intraoperative findings in order to maintain the structure and function of the TMJ, with no recurrence found over 30 months after surgery. In a similar fashion, the authors only removed loose bodies on the basis of intraoperative findings in this case. The symptoms disappeared after surgery, and there have been no clinical findings associated with recurrence.
Several limitations of this method based on CT scan data should be noted. First, it may be difficult to use in phase 1 SC according to Milgram classification because calcified loose bodies are often not revealed in radiographic examinations at that stage.[15] Second, this method requires a longer operation time and a higher cost of equipment and technology than routine surgical procedures.[9] Also, this technology may be available only in the university setting at the present time. Third, surgeons have to consider radiation exposure to patients associated with imaging examinations.
In conclusion, the guidance provided by a real-time 3-dimesional navigation system with a 3-point rigid cranial fixation device was useful in open surgery for the treatment of SC of the TMJ in this patient.
Acknowledgments
The authors wish to thank Professor Kenichirou Kikuta and Drs Yoshifumi Higashino, Hiroshi Arai, and Ayumi Akazawa, Department of Neurosurgery, Faculty of Medical Science, University of Fukui, for their support in the operation.
Author contributions
Conceptualization: Shinpei Matsuda.
Data curation: Shinpei Matsuda.
Writing – original draft: Shinpei Matsuda.
Writing – review & editing: Shinpei Matsuda, Hitoshi Yoshimura, Kazuo Sano.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging, SC = synovial chondromatosis, TMJ = temporomandibular joint.
Ethics approval: Not applicable. This is a case report.
Written informed consent was obtained from the patient for publication of the case and any accompanying images.
The authors declare no conflicts of interest.
References
- [1].Matsuda S, Yoshimura H, Yoshida H, et al. Application of a real-time three-dimensional navigation system to dental implant removal: a five-year single-institution experience. J Hard Tissue Biol 2018;27:359–62. [Google Scholar]
- [2].Collyer J. Stereotactic navigation in oral and maxillofacial surgery. Br J Oral Maxillofac Surg 2010;48:79–83. [DOI] [PubMed] [Google Scholar]
- [3].Hohlweg-Majert B, Metzger MC, Böhm J, et al. Advanced imaging findings and computer-assisted surgery of suspected synovial chondromatosis in the temporomandibular joint. J Magn Reson Imaging 2008;28:1251–7. [DOI] [PubMed] [Google Scholar]
- [4].Milgram JW. The classification of loose bodies in human joints. Clin Orthop Relat Res 1977;124:282–91. [PubMed] [Google Scholar]
- [5].Guarda-Nardini L, Piccotti F, Ferronato G, et al. Synovial chondromatosis of the temporomandibular joint: a case description with systematic literature review. Int J Oral Maxillofac Surg 2010;39:745–55. [DOI] [PubMed] [Google Scholar]
- [6].Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases. J Bone Joint Surg Am 1977;59:792–801. [PubMed] [Google Scholar]
- [7].Villacin AB, Brigham LN, Bullough PG. Primary and secondary synovial chondrometaplasia: histopathologic and clinicoradiologic differences. Hum Pathol 1979;10:439–51. [DOI] [PubMed] [Google Scholar]
- [8].Al-Kayat A, Bramley P. A modified pre-auricular approach to the temporomandibular joint and malar arch. Br J Oral Maxillofac Surg 1979;17:91–103. [DOI] [PubMed] [Google Scholar]
- [9].Dai J, Wu J, Wang X, et al. An excellent navigation system and experience in craniomaxillofacial navigation surgery: a double-center study. Sci Rep 2016;16:28242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sugisaki M, Ikai A, Tanabe H. Dangerous angles and depths for middle ear and middle cranial fossa injury during arthroscopy of the temporomandibular joint. J Oral Maxillofac Surg 1995;53:803–10. [DOI] [PubMed] [Google Scholar]
- [11].Chen MJ, Yang C, Qiu YT, et al. Synovial chondromatosis of the tempromandibular joint: relationship between MRI information and potential aggressive behavior. J Craniomaxillofac Surg 2015;43:349–54. [DOI] [PubMed] [Google Scholar]
- [12].Sade B, Mohr G. Depressed skull fracture and epidural haematoma: an unusual post-operative complication of pin headrest in an adult. Acta Neurochir (Wien) 2005;147:101–3. [DOI] [PubMed] [Google Scholar]
- [13].Stuart CW, Michael JP. Oral Radiology: Principles and Interpretation. 6th ed.St. Louis, MO: Mosby Elsevier; 2009. [Google Scholar]
- [14].Sato J, Notani KI, Goto J, et al. Synovial chondromatosis of the temporomandibular joint accompanied by loose bodies in both the superior and inferior joint compartments: case report. Int J Oral Maxillofac Surg 2010;39:86–8. [DOI] [PubMed] [Google Scholar]
- [15].Testaverde L, Perrone A, Caporali L, et al. CT and MR findings in synovial chondromatosis of the temporo-mandibular joint: our experience and review of literature. Eur J Radiol 2011;78:414–8. [DOI] [PubMed] [Google Scholar]


