Abstract
Background:
The prevalence of mental health problems in medical students has continuously increased and is higher than the prevalence of mental health problems in students with other majors, which could lead to undesirable consequences for the students and their future patients. In China, the current states of medical education and healthcare workplaces differ in certain areas from those in Western or other Asian countries. However, the mental health status of Chinese medical students has not been systematically analyzed.
Objectives:
The purpose of this meta-analysis was to summarize the prevalence of mental health problems in Chinese medical students.
Methods:
All cross-sectional studies that investigated the prevalence of any mental health problem among Chinese medical students were retrieved from the following databases: EMBASE, PubMed, PsycINFO, OVID, the Cochrane Database of Systematic Reviews, and the Cochrane Central Register of Controlled Trials. We accepted each individual trial's inclusion and exclusion criteria for participants. The National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was adopted to appraise the methodological quality of each study. RevMan (version 5.3) was used to analyze the data.
Results:
Ten cross-sectional studies involving a total of 30,817 Chinese medical students were included. The prevalence of depression, anxiety, suicidal ideation, and eating disorders were 29%, 21%, 11%, and 2%, respectively. Subgroup analysis revealed no significant differences in the prevalence of depression and suicidal ideation between genders and no significant difference in the prevalence of depression between individuals of different ages (20 years and older or younger than 20 years).
Conclusions and implications of key findings:
Chinese medical students have relatively high prevalence of depression, anxiety, and suicidal ideation but a low prevalence of eating disorders. Mental health problems in Chinese medical students should be taken seriously, and timely screening of and proper intervention in these mental health problems are highly recommended.
Keywords: China, medical student, mental health, meta-analysis, prevalence
1. Introduction
One of the main aims of medical schools is to train students to meet the healthcare needs of current and future national populations.[1,2] This is usually achieved through an arduous training curriculum and long-term clinical practice, for which high levels of motivation, intelligence, and stamina are expected. Generally, the total time required to acquire the necessary professional knowledge and skills is greater for medical students than those with other majors,[3,4] and the study of medicine is believed to be associated with significantly higher mental and physical pressure than is experienced in other subject areas.[5,6] In addition, individuals between 18 to 24 years of age are at particularly high risk for mental disorders such as major depressive disorder, anxiety, and psychiatric comorbidities.[7–9] As a consequence, mental health problems among medical students have been reported to be continuously increasing[10,11] and to be much more prevalent in medical students than in students with other majors.[12–17]
Mental health problems may persist into adulthood if they remain undetected or are not treated appropriately.[18] For students majoring in health-related subjects, these problems can result in numerous undesirable personal and professional consequences (e.g., they can impair their quality of life and increase the risk of suicidal ideation and decrease academic performance, professionalism, and empathy toward their patients).[12,19,20]
The current state of the medical education system and healthcare working environment in China differs in some areas compared to those in Western or other Asian countries. A high patient population with a relatively small number of doctors has resulted in a need for a large, strong labor force. Unstable relationships between patients and doctors frequently lead to workplace violence (WPV), with the patients as the perpetrators. Despite these discrepancies, there are few existing systematic reviews or meta-analyses on psychological issues in medical students from China. Thus far, mental health problems in the Chinese medical educational setting remain unclear.
This meta-analysis aimed to provide a comprehensive insight into the prevalent mental health experienced by Chinese medical students and an evidence-based basis for intervening in these problems.
2. Methods
All analyses were based on previously published studies; thus, ethical approval and patient consent were not necessary.
2.1. Inclusion and exclusion criteria
All the studies were screened and selected by 2 independent authors (W.Z. and R.C.). The prespecified eligibility criteria were as follows: types of studies—the included studies were cross-sectional studies that analyzed the prevalence of mental health problems among medical students in China or provided sufficient data for percentages to be calculated; types of participants—the included studies only involved medical students as participants, who were enrolled in medical schools or universities in China. We accepted each individual trial's criteria for the diagnosis of mental health problems and the exclusion of participants; types of outcomes—the included studies reported the prevalence of one of more mental health problems; types of screening methods and/or screening tools—the included studies utilized standardized validated instruments to assess the prevalence; type of journal—the included studies were published in peer-reviewed journals; and publication language—the included studies were written in English. In this review, we defined a mental health problem as any diagnosable mental disorder or symptom of a mental disorder (e.g., depression, anxiety, and suicidal ideation).
Studies were excluded if mental health problems were not the main focus of the questionnaire/diagnostic instrument (e.g., the focus was quality of life) or the adopted instruments had not been validated in the Chinese population.
2.2. Search method
We developed and conducted a comprehensive search of published and unpublished studies using EMBASE (1980–June 2018), PubMed (1966–June 2016), PsycINFO (1806–June 2016), OVID (1966–June 2018), the Cochrane Database of Systematic Reviews (CDSR, 2018), and the Cochrane Central Register of Controlled Trials (CENTRAL, 2018). The search terms consisted of medical subject headings and keywords, including terms related to medical schools, medical students, mental health, mental disorders, psychological distress, psychological health, and China. We also searched the reference lists of original reports, case reports, guidelines, letters to the editor, reviews, and meta-analyses retrieved through these electronic searches for additional articles.
2.3. Study selection and data extraction
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart was used to illustrate the study selection process (Fig. 1).[21] The titles and/or abstracts of the studies retrieved using the search strategy and those from additional sources were screened independently by 2 authors (W.Z. and Q.Z.) to identify studies that potentially met the inclusion and exclusion criteria outlined above. For studies that potentially fulfilled the inclusion and exclusion criteria, we retrieved the full texts, which were assessed independently by the same 2 authors. The same 2 authors also used a predesigned data collection form (Microsoft Office Excel 2013) to extract all the data independently. The following information was collected: study characteristics [first author name, year of publication, study design, sampling methods, study time, study site (province, city, and area of China), medical school], participant characteristics (age, sex, grade, and type of students), and outcome-related data [sample size (case and total size), outcomes, screening methods, and prevalence of mental health problems].
Figure 1.
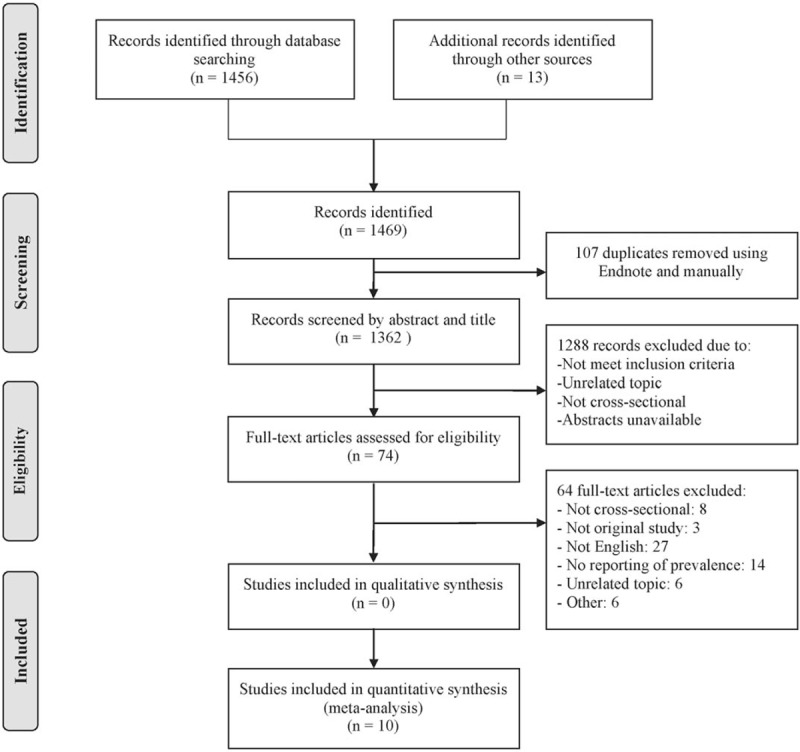
Study flow diagram using the PRISMA flow chart.
The information used to appraise the methodological quality of each study with the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (NIH-QAT, National Institutes of Health, 2014)[22] was also collected, including the clarity of the research objectives, the adequacy of the study population description, the appropriateness of the sample selection, the presence of a justification of the sample size, the exposure and outcome measurements, the sufficiency of study timeframe, the presence of follow-ups, and the adequacy of the statistical analyses.
The data were entered twice into Review Manager (RevMan, version 5.3, The Cochrane Collaboration). We defined depression[23–27] as our primary outcome (for any measure used), and anxiety, suicidal ideation, and eating disorders were combined as secondary outcomes. After extraction, all data were checked by another author (W.D.), and discrepancies were resolved via discussion. We sent letters to the authors of the studies as needed to clarify important missing or unclear data.
2.4. Data synthesis and statistical analysis
Two review authors entered the data separately (X.W. and Q.Z.), and we conducted the meta-analysis using RevMan. The extracted data were utilized to compute the standard error (SE) of the prevalence of mental health problems for each included study using the equation below[28] [because all included studies met the requirement of n × p > 5 and n × (1−p) > 5], using the number of medical students (n) and the prevalence of each mental health problem in medical students (p). This was calculated for the overall prevalence and for the prevalences among the identified subgroups.
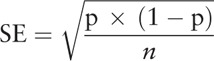 |
The prevalence was computed for each study in this review to derive a pooled effect estimate with the inverse variance method, which involved calculating the weighted average using SEs,[29] as mentioned above. Except for the aggregate prevalence, the corresponding P-value and 95% confidence interval (95% CI) were also reported.
Heterogeneity was analyzed by the I2 test, which describes the proportion of variation across the studies that is due not to chance but rather to the heterogeneity.[30,31] The higher the percentage, the higher the level of heterogeneity was.[31] If P > .10 and I2 < 50%, we considered the heterogeneity to be relatively low, and a fixed effects model was used to pool data; if P < .10 and I2 > 50%, we considered the heterogeneity to be substantial, so we used a random effects model to summarize the results. If heterogeneity was still high after adopting the random effects model, the reasons for the heterogeneity were investigated. P < .05 was used to determine statistical significance. In addition, a sensitivity analysis was performed to test the robustness of the pooled prevalence of depression by excluding each study and rerunning the meta-analysis.
Subgroup analyses were conducted to explore the source of heterogeneity among subgroups—stratified by gender and age—for the prevalence of mental health problems among medical students. The gender groups were divided into male and female groups for analysis. The age groups were determined by using the mean age of the participants of 20 years old as the cut-off value (≤20 years and >20 years).
We used forest plots and funnel plots. The funnel plots indicate possible publication bias, evidence of asymmetry, and other small study effects.[32] Finally, we followed PRISMA guidelines to report our findings.[33]
3. Results
3.1. Results of the search
We identified 1469 records from the literature research and finally kept 10 studies (Fig. 1). All 10 studies were cross-sectional in design, involving a total of 30,817 Chinese medical students for the quantitative synthesis.
3.2. Study characteristics
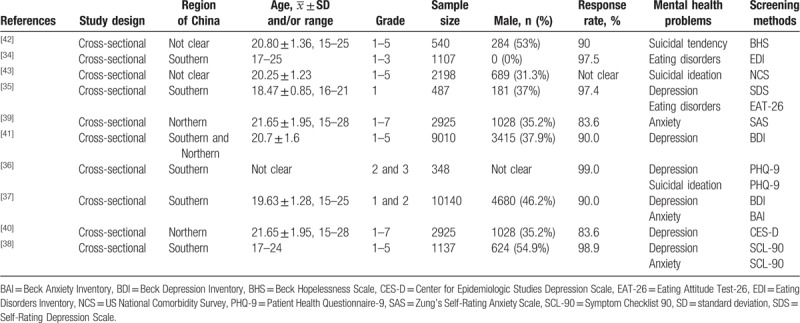
The participants in the 10 studies were all medical students from mainland China. Among the studies, 5 were conducted in South China,[34–38] 2 were conducted in North China,[39,40] 1 was conducted in 23 provinces covering both South and North China,[41] and the other 2 studies[42,43] did not describe the geographic region in their article. The mean age of students was above 20 years old in 5 studies,[39–43] below 20 years old in 2 studies,[35,37] and unknown in the other 3 studies.[34,36,38] All the included studies adopted validated self-report questionnaires to measure the outcomes. Various instruments were utilized. For depression, the most commonly used tool was the Beck Depression Inventory,[37,41] while the Self-Rating Depression Scale,[35] the Center for Epidemiologic Studies Depression Scale,[40] the Patient Health Questionnaire-9 (PHQ-9),[36] and the Symptom Checklist (SCL-90)[38] were also adopted. For anxiety, Zung's Self-Rating Anxiety Scale,[39] the Beck Anxiety Inventory[37] and the SCL-90[38] were used in 3 studies. For suicidal ideation, 3 different tools, namely, the Beck Hopelessness Scale,[42] the PHQ-9,[36] and the US National Comorbidity Survey,[43] were also used in 3 studies. In addition, for eating disorders, 1 study used the Eating Disorders Inventory,[34] while another study adopted the Eating Attitude Test.[35] The characteristics of the included studies are presented in Table 1.
Table 1.
Characteristics of the included studies.
3.3. Quality appraisal
All included studies received quality rating scores of 50% or higher according to the NIH-QAT quality appraisal tool.
3.4. Prevalence of mental health problems
3.4.1. Depression
Six studies[35–38,40,41] reported that the pooled prevalence of depression among medical students in China was 29% (95% CI: 15–44%, P < .0001; I2 = 100%, P < .00001), with a range from 3.2% to 66.8% (Fig. 2).
Figure 2.
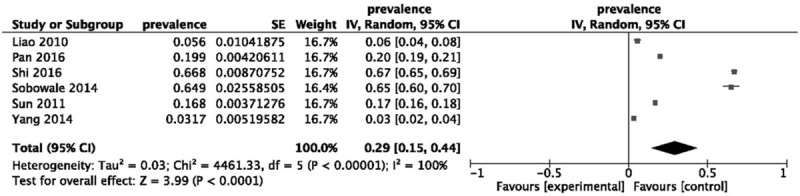
Forest plot assessing the prevalence of depression among medical students in China. CI = confidence interval, SE = standard error.
The difference in the prevalence of depression in male[35,37,41] (15%, 95% CI: 5– 25%, P = .003) and female[35,37,41] (14%, 95% CI: 10–18%, P < .00001) medical students were not statistically significant (χ2 = 0.04, P = .85, I2 = 0%) (Fig. 3). When stratified by age into younger[35,37] (≤20 years old) and older group (>20 years old)[40,41] (Fig. 4), older medical students (43%, 95% CI: −3–89%, P = .06) had a higher prevalence of depression than younger medical students (11%, 95% CI: 0–22%, P = .04), but the difference was not significant (χ2 = 1.77, P = .18, I2 = 43.6%).
Figure 3.
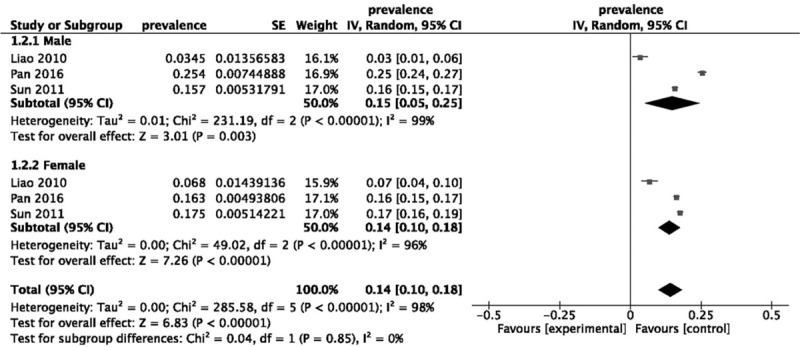
Forest plot assessing the prevalence of depression among medical students in China, stratified by the gender of the participants. CI = confidence interval, SE = standard error.
Figure 4.
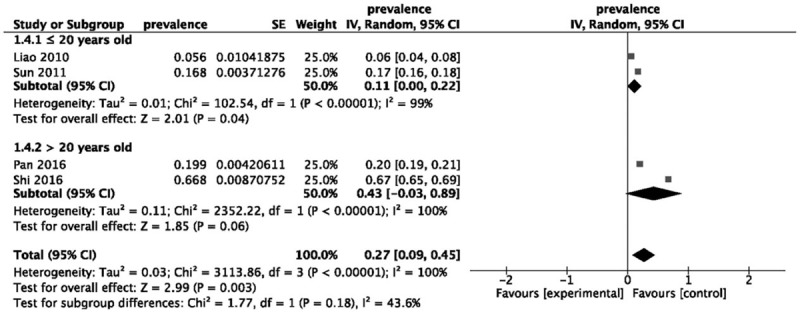
Forest plot assessing the prevalence of depression among medical students in China, stratified by the mean age of the participants. CI = confidence interval, SE = standard error.
3.4.2. Anxiety
The summarized prevalence of anxiety among Chinese medical students was 21% (95% CI: 3–39%, P = .02; I2 = 100%, P < .00001, Fig. 5) based on the analysis of 3 studies,[37–39] ranging from 2.0% to 47.3%.
Figure 5.
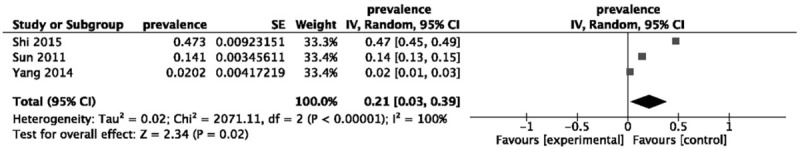
Forest plot assessing the prevalence of anxiety among medical students in China. CI = confidence interval, SE = standard error.
3.4.3. Suicidal ideation
As shown in Figure 6, suicidal ideation was prevalent in 11% of the Chinese medical students (95% CI: 4–19%, P = .001; I2 = 97%, P < .00001, Fig. 7) in the 3 included studies,[36,42,43] ranging between 7.5% and 17.9%.
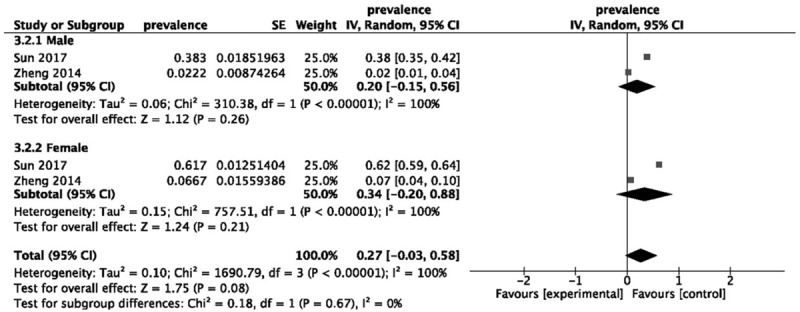
Figure 6.
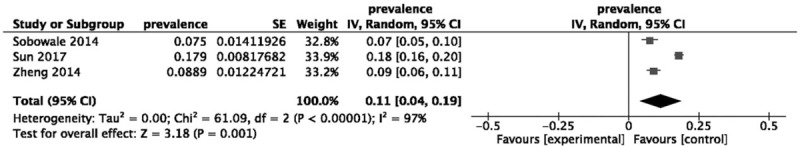
Forest plot assessing the prevalence of suicidal ideation among medical students in China, stratified by the gender of the participants. CI = confidence interval, SE = standard error.
Figure 7.
Forest plot assessing the prevalence of suicidal ideation among medical students in China. CI = confidence interval, SE = standard error.
As shown in Figure 6, female[42,43] medical students (34%, 95% CI: 20–88%, P = .21) had a relatively higher prevalence of suicidal ideation than male[42,43] medical students (20%, 95% CI: 15–56%, P = .26), but the difference between these 2 groups was not statistically significant (χ2 = 1.75, P = .08; I2 = 0%, P = .67).
3.4.4. Eating disorders
In the analysis of 2 studies,[34,35] medical students in China showed an overall eating disorder prevalence of 2% (95% CI: 2–3%, P < .00001, Fig. 8), ranging from 2.17% to 2.5%, and there was a low level of heterogeneity between the studies (I2 = 0%, P = .70).
Figure 8.
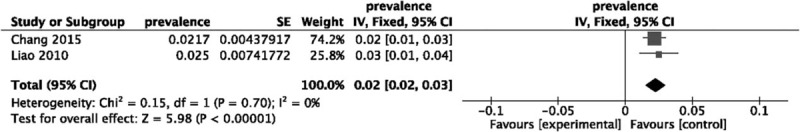
Forest plot assessing the prevalence of eating disorders among medical students in China. CI = confidence interval, SE = standard error.
3.5. Publication bias
The funnel plot for the primary outcome, depression (Fig. 9), appeared somewhat asymmetrical. However, because the number of trials included was insufficient, the assessment of publication bias may be inaccurate for this outcome.
Figure 9.
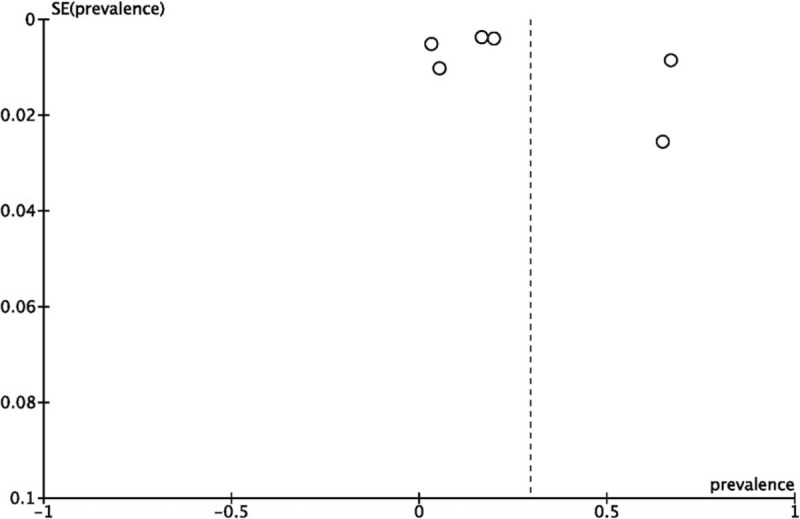
Funnel plot assessing the prevalence of depression among medical students in China. SE = standard error.
3.6. Sensitivity analysis
Each study was sequentially excluded to examine the stability of the pooled prevalence of our primary outcome, depression. As shown in Figure 10, the results were not altered by the exclusion of any specific study, which suggests that the results are reliable and that the prevalence of depression among Chinese medical students is exceedingly high.
Figure 10.
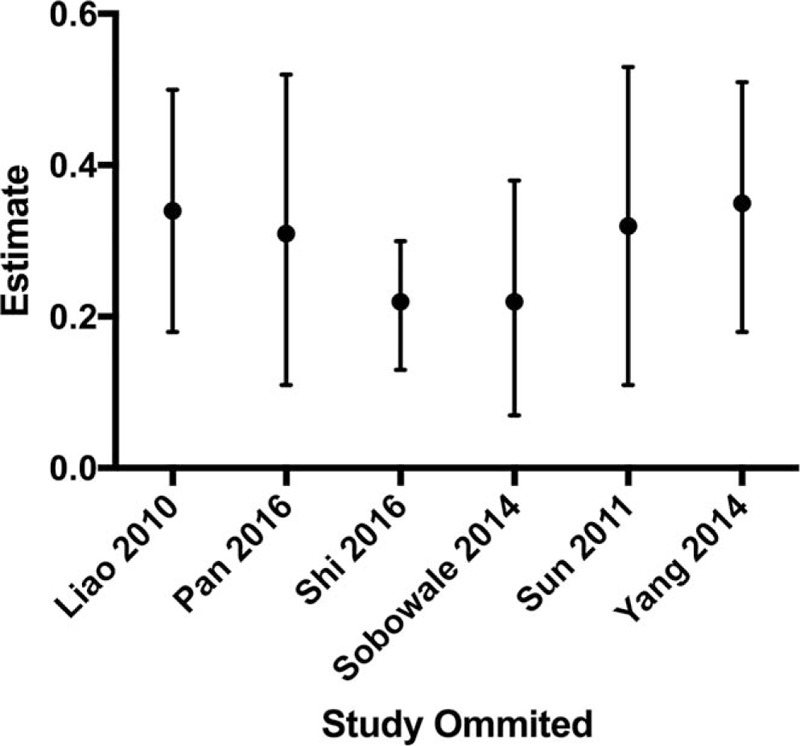
Plot of the sensitivity analysis, which was conducted by excluding 1 study each time and pooling the estimate for the rest of the studies.
4. Discussion
4.1. Summary of results
The present study is the first meta-analysis to investigate the prevalence of some common mental health problems among Chinese medical students based on a pooled population of 30,817 participants from 10 cross-sectional studies that were all published after 2010. Based on our study, the prevalence of depression, anxiety, suicidal ideation, and eating disorders was 29%, 21%, 11%, and 2%, respectively. The recent publication of these studies and the high prevalence values for depression, anxiety, and suicidal ideation draws attention to the fact that although these mental health issues have long been reported worldwide, especially in some advanced countries, more attention should be paid to medical students in developing countries such as China; these mental health problems have recently been emphasized and have continued to become more common according to assessments in recent years.[44,45]
4.2. Depression
It has been well documented that depression can lead to many negative consequences for young people, such as poor academic performance, high rates of substance use, and even suicidal ideation.[36,46–49] As the first meta-analysis investigating the nationwide prevalence of depression among Chinese medical students, our study reported a pooled prevalence of 29% based on 6 cross-sectional studies. The result is much higher compared with the prevalence of depression in Chinese students with other majors[50] as well as in medical students from other countries.[51] Several reasons may account for this result. First, the undergraduate medical education system in China applies much heavier academic pressure on medical students than on students studying other professions, since the content of their courses is rarely related to what they have learned before and is, therefore, harder to understand. In addition, as a profession related to the safety of human life, medical education is particularly strict and is more demanding than with other majors. Additionally, the doctor–patient relationship in China has become increasingly tense in recent years, with frequent violent attacks against healthcare workers, a lack of respect from society and relatively low remuneration, all of which decrease the enthusiasm of young medical students for pursuing their future careers.[52–54] These abovementioned reasons could be the cause of substantial psychological stress and hopelessness in medical students. Notably, there was no significant difference in the prevalence of depression based on gender or age according to the subgroup analyses, indicating that all medical students have a high risk of depression. As the most commonly reported psychological problem in Chinese medical students, it is suggested that more attention should be paid to those with signs and symptoms of depression, and timely screening and proper interventions are highly necessary. In addition, more efforts should be made by medical educators to improve the sense of professional identity and the professional expectations for Chinese medical students.
4.3. Anxiety
Anxiety is the second most common mental health problem found in Chinese medical students. The pooled prevalence was 21%, which is higher than that reported among Asian medical students.[51] The long-term heavy academic burden, high-intensity internships, frequent WPV, complex multipersonal relationships, and uncertainty regarding their future careers might be the cause of the high incidence of anxiety in Chinese medical students. Similar to depression, anxiety may also lead to many undesirable consequences, such as poor academic performance and dropping out of school due to impaired cognitive function or even suicidal ideation and attempts.[55–57] Based on the results of our study, anxiety disorders in medical students should also be taken seriously, promptly diagnosed, and supported by medical school educators.
4.4. Suicidal ideation
The combined result of our meta-analysis revealed that the prevalence of suicidal ideation among medical students in China was 11%, which is higher than in medical students in Brazil[58] and similar to the result reported in other Chinese college students[59] and in medical students from the United States.[60] We believe that excessive academic pressure is a major cause of suicidal ideation. Additionally, suicidal ideation is reported to be closely related to other mental health disorders, such as depression and anxiety. According to our meta-analysis, the incidence of depression combined with anxiety among Chinese medical students is generally higher than those in other places and populations, which could be another cause of their high prevalence of suicidal ideation. Moreover, it is worth noting that suicidal ideation is highly likely to transfer to suicidal attempts and suicidal actions,[61] leading to fatal and irreversible consequences. Therefore, more attention should be paid to early screening of Chinese medical students for suicidal ideation. Meanwhile, more mental health counseling and suicide-related psychological education should be provided to Chinese medical students to avoid those serious consequences. Previous studies[62,63] reported a higher incidence of suicidal ideation in female university students than in males. However, according to the subgroup analysis, the prevalence of suicidal ideation did not differ statistically between genders in Chinese medical students, indicating that equal attention should be paid to both male and female medical students.
4.5. Eating disorders
Eating disorders frequently occur in young females,[64,65] which can be a cause of overeating or insufficient ingestion.[66,67] The combined results showed that the prevalence of eating disorders in Chinese medical students was 2%. This result is lower than the rates in several Western countries, such as Spain (5.34%),[68] Turkey (12%),[69] and the United States (15% of females and 4% of males).[70] The results indicate that Chinese medical students are at relatively lower risk of suffering eating disorders regardless of other mental health problems, including depression and anxiety. Some studies have reported that body weight is positively correlated with eating disorders,[71,72] and the average body mass index of Chinese people is generally lower than those of the populations in Western countries.[73–75] This might explain why Chinese medical students have a relatively lower prevalence of eating disorders. However, due to the severe consequences of eating disorders,[66,67] careful screening and proper intervention are still important for Chinese medical students.
4.6. Comparison with other published reviews
Previous meta-analyses and systematic reviews investigated the prevalence of mental health problems among medical students in Asia,[51] Brazil,[76] and some English-speaking countries.[77] In China, several pooled studies reported the prevalence of mental health problems among college students,[50,78] but none of them focused on medical students, and the majority of them focus on only depression as their outcome. To the best of our knowledge, this meta-analysis is the first study to summarize the prevalence of mental health problems among medical students in China. In addition to depression, we also identified anxiety, suicidal ideation, and eating disorders as outcomes.
4.7. Implications for practice
Compared with Chinese students with different majors and medical students from other countries, Chinese medical students have a higher prevalence of depression, anxiety, and suicidal ideation but a relatively lower incidence of eating disorders. These results indicate that the current status of mental health problems among Chinese medical students is still very serious. Based on our study, depression and anxiety are the 2 most prevalent mental health disorders, and suicidal ideation is the risk factor with the most fatal consequence. Thus, careful screening of and proper intervention in these mental health problems are necessary and should be supported by educators and counselors in a timely and consistent manner.
4.8. Implications for future research
Through the literature search, we found that previous studies about mental health problems among medical students in China were mostly cross-sectional studies, which focused only on the current status at a certain point of time. Therefore, future longitudinal investigations with dynamic study designs are highly recommended. In addition, current studies on mental health problems among Chinese medical students mainly focus on depression, anxiety, and suicidal ideation. Additional studies are needed to investigate a variety of other mental health problems, such as burnout, stress, and obsessive-compulsive disorder and the combination of different mental health problems such as bipolar disorder or combination of depression and eating disorder. In addition, more stratified and subgroup analyses are suggested in future research to investigate mental health problems in a clearer and more comprehensive manner.
4.9. Strengths and limitations
To the best of our knowledge, this meta-analysis is the first evidence-based study to investigate the prevalence of mental health problems among medical students in China. The instruments measuring the mental health problems used in the included studies are all currently widely used scales, with good reliability and validity. Instead of evaluating only depression, which was the most common outcome in previous meta-analyses, we also reported the prevalence of some other mental health problems, including anxiety, suicidal ideation, and eating disorders, making this meta-analysis more comprehensive and accurate than previous studies. The results of our study will be highly relevant to the medical education and could be a very important warning and reminder regarding the current status of several mental health problems among Chinese medical students.
Nevertheless, several potential limitations should also be addressed. Because all the included studies were cross-sectional in design, this meta-analysis lacks a dynamic analysis of mental health problems among Chinese medical students; high heterogeneity across studies, and some bias might exist. Besides, the included studies were all conducted using self-rating scales and lack of further investigation to the screened population with positive mental health problems, which may influence the accuracy of the results. Meanwhile, due to the limited mental health problems covered in current original studies, there are many factors other than depression, anxiety, suicidal ideation, and eating disorders that are not synthesized in this present meta-analysis.
5. Conclusions
Chinese medical students have a relatively higher prevalence of depression, anxiety, and suicidal ideation but a lower prevalence of eating disorders compared with Chinese students with different majors and medical students from other countries. The findings highlight the necessity and urgency of providing timely screening of and proper intervention in these mental health problems among Chinese medical students. However, high heterogeneity across the studies and some bias might exist due to the flaws in the cross-sectional designs of the included studies. Thus, we should interpret these results with caution.
Author contributions
Conceptualization: Qin Zhang, Wei Deng.
Data curation: Wen Zeng, Ruiqi Chen, Wei Deng.
Formal analysis: Wen Zeng, Xingyue Wang, Wei Deng.
Funding acquisition: Wei Deng, Wen Zeng, Ruiqi Chen.
Methodology: Wen Zeng, Xingyue Wang, Qin Zhang.
Project administration: Wei Deng.
Software: Ruiqi Chen, Xingyue Wang, Qin Zhang, Wei Deng.
Supervision: Wei Deng.
Writing – original draft: Wen Zeng, Ruiqi Chen, Xingyue Wang.
Writing – review & editing: Qin Zhang.
Footnotes
Abbreviation: BAI = Beck Anxiety Inventory, BDI = Beck Depression Inventory, BHS = Beck Hopelessness Scale, CDSR = Cochrane Database of Systematic Reviews, CES-D = Center for Epidemiologic Studies Depression Scale, CI = confidence interval, EAT-26 = Eating Attitude Test, EDI = Eating Disorders Inventory, NCS = National Comorbidity Survey, PHQ-9 = Patient Health Questionnaire-9, SAS = Self-Rating Anxiety Scale, SCL-90 = Symptom Checklist 90, SDS = Self-Rating Depression Scale, SE = standard error, WPV = workplace violence.
WZ and RC contributed equally to the manuscript.
This research was supported by National Key Research & Development Program of China (2016YFC1201700); Sichuan Provincial Health and Family Planning Commission research projects (18PJ312); Fundamental Research Funds for the Central Universities (2012017yjsy200).
The authors have no conflicts of interest to disclose.
References
- [1].Schofield JR. New and expanded medical schools, mid-century to the 1980s: an analysis of changes and recommendations for improving the education of physicians. San Francisco: Jossey-Bass; 1984. [Google Scholar]
- [2].Mullan F, Chen C, Petterson S, et al. The social mission of medical education: ranking the schools. Ann Intern Med 2010;153:804–11. [DOI] [PubMed] [Google Scholar]
- [3].Bond AR, Mason HF, Lemaster CM, et al. Embodied health: the effects of a mind–body course for medical students. Med Educ Online 2013;18:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].O’Rourke M, Hammond S, O’Flynn S, Boylan G. The medical student stress profile: a tool for stress audit in medical training. Med Educ 2010;44:1027–37. [DOI] [PubMed] [Google Scholar]
- [5].Adams J. Straining to describe and tackle stress in medical students. Med Educ 2004;38:463–4. [DOI] [PubMed] [Google Scholar]
- [6].Association BM. BMA medical students’ finance survey academic year 2010/2011. London: BMA; 2011. [Google Scholar]
- [7].Patten SB. Major depression prevalence in Calgary. Can J Psychiatry 2000;45:923–6. [DOI] [PubMed] [Google Scholar]
- [8].Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med 1998;28:109–26. [DOI] [PubMed] [Google Scholar]
- [9].Alonso JA, Bernert S, Angermeyer MC, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 2004;420:21–7. [DOI] [PubMed] [Google Scholar]
- [10].Benton SA, Robertson JM, Tseng WC, et al. Changes in counseling center client problems across 13 years. Prof Psychol Res Pract 2003;34:66–72. [Google Scholar]
- [11].Gallagher RP, Weaver W, Assistant GR, et al. National survey of counseling center directors. International Association of Counseling Service 2012. [Google Scholar]
- [12].Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med 2006;81:354–73. [DOI] [PubMed] [Google Scholar]
- [13].Tyssen R, Vaglum P, Grøvold NT, Ekeberg O. Suicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictors. J Affect Disord 2001;64:69–79. [DOI] [PubMed] [Google Scholar]
- [14].Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ 2010;39:594–604. [DOI] [PubMed] [Google Scholar]
- [15].Bayram N, Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol 2008;43:667–72. [DOI] [PubMed] [Google Scholar]
- [16].Tomoda A, Mori K, Kimura M, et al. One-year prevalence and incidence of depression among first-year university students in Japan: a preliminary study. Psychiatry Clin Neurosci 2000;54:583–8. [DOI] [PubMed] [Google Scholar]
- [17].Stewartbrown S, Evans J, Patterson J, et al. The health of students in institutes of higher education: an important and neglected public health problem? J Public Health Med 2000;22:492–9. [DOI] [PubMed] [Google Scholar]
- [18].Pine DS, Cohen P, Gurley D, et al. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry 1998;55:56–64. [DOI] [PubMed] [Google Scholar]
- [19].Liliane L, Carvalho FM, Menezes MS, et al. Health-related quality of life of students from a private medical school in Brazil. Int J Med Educ 2015;6:149–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Dyrbye LN, Harper W, Moutier C, et al. A multi-institutional study exploring the impact of positive mental health on medical students’ professionalism in an era of high burnout. Acad Med 2012;87:1024–31. [DOI] [PubMed] [Google Scholar]
- [21].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J 2009;339:332–6. [PMC free article] [PubMed] [Google Scholar]
- [22].2014. Health NIo. Quality Assessment Tool for Observational Cohort and Cross-sectional Studies. Retrieved January 24, 2016 from. [Google Scholar]
- [23].Cukor D, Ver Halen N, Asher DR, et al. Psychosocial intervention improves depression, quality of life, and fluid adherence in hemodialysis. J Am Soc Nephrol 2014;25:196–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Chen HY, Cheng IC, Pan YJ, et al. Cognitive-behavioral therapy for sleep disturbance decreases inflammatory cytokines and oxidative stress in hemodialysis patients. Kidney Int 2011;80:415–22. [DOI] [PubMed] [Google Scholar]
- [25].Duarte PS, Miyazaki MC, Blay SL, et al. Cognitive–behavioral group therapy is an effective treatment for major depression in hemodialysis patients. Kidney Int 2009;76:414–21. [DOI] [PubMed] [Google Scholar]
- [26].Lii YC, Tsay SL, Wang TJ. Group intervention to improve quality of life in haemodialysis patients. J Clin Nurs 2007;16(11C):268–75. [DOI] [PubMed] [Google Scholar]
- [27].Tsay SL, Lee YC, Lee YC. Effects of an adaptation training programme for patients with end-stage renal disease. J Adv Nurs 2005;50:39–46. [DOI] [PubMed] [Google Scholar]
- [28].Collett D. Modelling binary data, 2nd ed. Boca Raton, FL: Chapman & Hall; 2003. [Google Scholar]
- [29].Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. 8th edPhiladelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014. [Google Scholar]
- [30].Cochran WG. The combination of estimates from different experiments. Biometrics 1954;10:101–29. [Google Scholar]
- [31].Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Guyatt GH, Oxman AD, Montori V, et al. GRADE guidelines: 5. Rating the quality of evidence: publication bias. J Clin Epidemiol 2011;64:1277–82. [DOI] [PubMed] [Google Scholar]
- [33].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2009;151:264–9. [DOI] [PubMed] [Google Scholar]
- [34].Chang WW, Nie M, Kang YW, et al. Subclinical eating disorders in female medical students in Anhui, China: a cross-sectional study. Nutr Hosp 2015;31:1771–7. [DOI] [PubMed] [Google Scholar]
- [35].Liao YH, Knoesen NP, Castle DJ, et al. Symptoms of disordered eating, body shape, and mood concerns in male and female Chinese medical students. Compr Psychiatry 2010;51:516–23. [DOI] [PubMed] [Google Scholar]
- [36].Sobowale K, Zhou N, Fan J, et al. Depression and suicidal ideation in medical students in China: a call for wellness curricula. Int J Med Educ 2014;5:31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Sun L, Sun LN, Sun YH, et al. Correlations between psychological symptoms and social relationships among medical undergraduates in Anhui Province of China. Int J Psychiatry Med 2011;42:29–47. [DOI] [PubMed] [Google Scholar]
- [38].Yang F, Meng H, Chen H, et al. Influencing factors of mental health of medical students in China. J Huazhong Univ Sci Technolog Med Sci 2014;34:443–9. [DOI] [PubMed] [Google Scholar]
- [39].Shi M, Liu L, Wang ZY, et al. The mediating role of resilience in the relationship between big five personality and anxiety among Chinese medical students: a cross-sectional study. PloS One 2015;10:e0119916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Shi M, Liu L, Wang ZY, et al. Prevalence of depressive symptoms and its correlations with positive psychological variables among Chinese medical students: an exploratory cross-sectional study. BMC Psychiatry 2016;16:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Pan XF, Wen Y, Zhao Y, et al. Prevalence of depressive symptoms and its correlates among medical students in China: a national survey in 33 universities. Psychol Health Med 2016;21:882–9. [DOI] [PubMed] [Google Scholar]
- [42].Zheng A, Wang Z. Social and psychological factors of the suicidal tendencies of Chinese medical students. Biopsychosoc Med 2014;8:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Sun L, Zhou C, Xu L, et al. Suicidal ideation, plans and attempts among medical college students in china: the effect of their parental characteristics. Psychiatry Res 2017;247:139–43. [DOI] [PubMed] [Google Scholar]
- [44].Glatt MM. Characteristics and prognosis of alcoholic doctors. Br Med J 1977;1:507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Murray RM. Psychiatric illness in male doctors and controls: an analysis of Scottish hospitals in-patient data. Br J Psychiatry 1977;131:1–0. [DOI] [PubMed] [Google Scholar]
- [46].Andrews B, Wilding JM. The relation of depression and anxiety to life-stress and achievement in students. Br J Psychol 2004;95:509–21. [DOI] [PubMed] [Google Scholar]
- [47].Deas D, Brown ES. Adolescent substance abuse and psychiatric comorbidities. J Clin Psychiatry 2006;67Suppl 7:18–23. [PubMed] [Google Scholar]
- [48].Kessler RC, Foster CL, Saunders WB, et al. Social consequences of psychiatric disorders, I: educational attainment. Am J Psychiatry 1995;152:1026–32. [DOI] [PubMed] [Google Scholar]
- [49].Garlow SJ, Rosenberg J, Moore JD, et al. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress Anxiety 2008;25:482–8. [DOI] [PubMed] [Google Scholar]
- [50].Lei XY, Xiao LM, Liu YN, et al. Prevalence of depression among Chinese university students: a meta-analysis. PLoS One 2016;11:e0153454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Cuttilan AN, Sayampanathan AA, Ho RC. Mental health issues amongst medical students in Asia: a systematic review [2000-2015]. Ann Transl Med 2016;4:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Zeng J, Zeng XX, Tu Q. A gloomy future for medical students in China. Lancet 2013;382:1878. [DOI] [PubMed] [Google Scholar]
- [53].Jingang A. Which future for doctors in China? Lancet 2013;382:936–7. [DOI] [PubMed] [Google Scholar]
- [54].Xu D, Sun B, Wan X, et al. Reformation of medical education in China. Lancet 2010;375:1502–4. [DOI] [PubMed] [Google Scholar]
- [55].Singh I, Jha A. Anxiety, optimism and academic achievement among students of private medical and engineering colleges: a comparative study. J Educ Dev Psychol 2013;3:222. [Google Scholar]
- [56].Saravanan C, Wilks R. Medical students’ experience of and reaction to stress: the role of depression and anxiety. Sci World J 2014;2014:737382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Sareen J, Cox BJ, Afifi TO, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry 2005;62:1249–57. [DOI] [PubMed] [Google Scholar]
- [58].Torres AR, Campos LM, Lima MC, et al. Suicidal ideation among medical students: prevalence and predictors. J Nerv Ment Dis 2018;206:160–8. [DOI] [PubMed] [Google Scholar]
- [59].Li ZZ, Li YM, Lei XY, et al. Prevalence of suicidal ideation in Chinese college students: a meta-analysis. PLoS One 2014;9:e104368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Zisook S, Young I, Doran N, et al. Suicidal ideation among students and physicians at a US medical school: a healer education, assessment and referral (HEAR) program report. OMEGA 2016;74:35–61. [Google Scholar]
- [61].Klonsky ED, May AM. The three-step theory (3ST): a new theory of suicide rooted in the “ideation-to-action” framework. Int J Cogn Ther 2015;8:114–29. [Google Scholar]
- [62].Zhai H, Bai B, Chen L, et al. Correlation between family environment and suicidal ideation in university students in China. Int J Environ Res Public Health 2015;12:1412–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Yousaf M, Daud S, M Shafique M. Gender Difference in Depression and Suicidal Ideation of medical students. Vol 102016 [Google Scholar]
- [64].Kovacs T. Prevalence of eating disorders in the cultural context of the Romanian majority and the Hungarian minority in Romania. Psychiatr Hung 2007;22:390–6. [PubMed] [Google Scholar]
- [65].Szabo P, Tury F. Prevalence of clinical and subclinical forms of anorexia and bulimia nervosa among working females and males. Orv Hetil 1995;136:1829–35. [PubMed] [Google Scholar]
- [66].Herpertz-Dahlmann B. Adolescent eating disorders: definitions, symptomatology, epidemiology and comorbidity. Child Adolesc Psychiatr Clin N Am 2009;18:31–47. [DOI] [PubMed] [Google Scholar]
- [67].Klump KL, Bulik CM, Kaye WH, et al. Academy for eating disorders position paper: eating disorders are serious mental illnesses. Int J Eat Disord 2009;42:97–103. [DOI] [PubMed] [Google Scholar]
- [68].Fernádez MA, Labrador FJ, Raich RM. Prevalence of eating disorders among adolescent and young adult scholastic population in the region of Madrid (Spain). J Psychosom Res 2007;62:681–90. [DOI] [PubMed] [Google Scholar]
- [69].Celikel FC, Cumurcu BE, Koc M, et al. Psychologic correlates of eating attitudes in Turkish female college students. Compr Psychiatry 2008;49:188–94. [DOI] [PubMed] [Google Scholar]
- [70].Forman S, Prokop L, Keliher A, et al. Screening high school students for eating disorders: results of a national initiative. Prev Chronic Dis 2008;5:A114. [PMC free article] [PubMed] [Google Scholar]
- [71].Von LA, Abraham S. Personality factors and eating disorders: self-uncertainty. Eat Behav 2014;15:106–9. [DOI] [PubMed] [Google Scholar]
- [72].Celik S, Yoldascan E, Okyay R, et al. Prevalence of eating disorders in female university students and affecting factors. Anadolu Psikiyatr De 2016;17:42–51. [Google Scholar]
- [73].Brunt A, Zhong L, Rhee Y. Comparison of dietary variety between US and Chinese college students. J Am Diet Assoc 2009;109:A25–125. [Google Scholar]
- [74].Yang F, Yang C, Liu Y, et al. Associations between body mass index and visual impairment of school students in Central China. Int J Environ Res Public Health 2016;13:1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Wyon MA, Hutchings KM, Wells A, et al. Body mass index, nutritional knowledge, and eating behaviors in elite student and professional ballet dancers. Clin J Sport Med 2014;24:390–6. [DOI] [PubMed] [Google Scholar]
- [76].Pacheco JP, Giacomin HT, Tam WW, et al. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz J Psychiatry 2017;39:369–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ 2014;48:963–79. [DOI] [PubMed] [Google Scholar]
- [78].Jiang CX, Li ZZ, Chen P, et al. Prevalence of depression among college-goers in mainland China: a methodical evaluation and meta-analysis. Medicine 2015;94:e2071. [DOI] [PMC free article] [PubMed] [Google Scholar]


