Abstract
This paper presents a brief, focused physical examination (PE, the Buffalo Concussion Physical Examination [BCPE]) for sport-related concussion (SRC) to be considered for use in the outpatient setting by sports medicine physicians, pediatricians, and primary-care physicians. This companion paper describes how to perform the PE, which was derived in a separate study presented in this journal. It is envisioned for use at the initial and follow-up outpatient visits both for acute concussions and in patients with prolonged symptoms. A pertinent PE, combined with other assessments, can help identify specific treatment targets in those with persistent symptoms after SRC. The BCPE includes orthostatic vital signs and examinations of the cranial nerves, oculomotor/ophthalmologic, cervical, and vestibular systems. Supplementary tests, including testing for exercise tolerance and neurocognitive function, may be performed if indicated. It is recommended that a PE be performed at the initial visit and every 1–2 weeks after SRC. Upon return of symptoms, cognition, and the PE to baseline, as well as normalization of any supplementary tests, patients can begin a return to play program.
Keywords: concussion, management, Buffalo Concussion Physical Exam, Buffalo Concussion Treadmill Test
Introduction
Sport-related concussion (SRC), a sub-type of mild traumatic brain injury (mTBI), typically results in reversible neurological dysfunction caused by either by a direct blow to the head, neck, or elsewhere on the body with an impulsive force transmitted to the head.1 SRC is common in sports medicine, pediatric, and primary-care clinics.2 The first step in establishing the diagnosis in the outpatient setting is a detailed account of the injury and a comprehensive medical history, including a validated concussion symptom questionnaire. Information about symptoms is essential but relying solely on subjective symptom reports is problematic because athletes often under-report symptoms and concussion-related symptoms are non-specific since they are reported often in patients without concussion.3–5 It is important to document pre-existing medical conditions that may impact recovery such as a history of previous concussions, migraine headaches, learning disorders, psychiatric conditions such as depression or anxiety, and pre-existing neuro-ophthalmological conditions such as strabismus or convergence insufficiency because they have been associated with prolonged recovery.6 Cognitive function should be assessed using a standardized assessment tool, the most common of which is the Standardized Assessment of Concussion (SAC) of the Sport Concussion Assessment Tool 5 (SCAT5).7 It measures orientation, memory, and concentration.
Following the history and cognitive assessment, physicians should perform a focused physical examination (PE) at the initial outpatient visit because physical signs may develop in the 24 hours after injury that were not present at the sideline assessment.1 Recent studies have shown that some physicians who see concussed patients are not current with the latest international recommendations.8 In prior work,9 we presented a comprehensive “toolbox” that contained PE elements that may be useful for the evaluation of concussed patients. In this paper we present directions on how to perform a brief, focused PE to help clinicians efficiently identify physical impairments and track recovery after SRC. Derivation of the Buffalo Concussion Physical Exam (BCPE) is presented in an associated paper in this journal. Objective signs, when combined with symptoms, cognitive evaluation and, where indicated, supplementary tests, may help the clinician diagnose concussion and understand the cause of symptoms in order to prescribe specific treatment for those with prolonged recovery. Acutely concussed patients should in general be seen every 1 to 2 weeks to monitor recovery. If they develop Persistent Post-Concussive Symptoms (PPCS), defined as symptoms persisting more than 2weeks in adults or more than 1 month in children and adolescents,1 the frequency may be subsequently reduced. Primary care physicians might also consider referring those with PPCS to a multidisciplinary concussion clinic or expert.
Classification6
While we are not able to classify all concussed patients into specific categories or subtypes because concussion is a unique injury to each individual patient with several associated conditions, it is useful for the clinician to try to identify the predominant physical signs and symptoms to direct specific treatments for those with PPCS (Figure 1). These classifications may overlap as it is possible to have one or more associated conditions after a head injury. Physiological Post-Concussion Syndrome (PCS) is believed to be characterized by persistent autonomic dysfunction and altered control of cerebral blood flow from the global cerebral metabolic disturbance after concussion. These patients typically present with minimal PE abnormalities but can have signs of oculomotor and/or vestibular dysfunction. They often complain of cognitive fatigue and report symptoms with orthostatic vital signs and have early exercise intolerance on graded treadmill testing (i.e., symptom-limited exercise at <70% of age-predicted maximum heart rate, HR). Other sub-classifications (or associated conditions) include vestibulo-ocular post-traumatic disorder (PTD) and cervicogenic PTD, which present with predominantly vestibulo-ocular and cervical signs and symptoms, respectively. These disorders are not labelled PCS because they are not considered to represent the global metabolic disturbance of brain function after concussion but rather persistent injuries to the central oculomotor and vestibular systems and/or to the upper cervical spine. These patients may demonstrate exercise intolerance during graded treadmill testing but symptom exacerbation typically occurs at a significantly greater workload (beyond 70% of age-predicted maximum HR) than in autonomic/physiological PCS. Some patients with PPCS primarily have affective and/or cognitive symptoms, the management of which is challenging because of the extensive overlap between their symptoms and primary mood disorders. In the authors’ experience, PPCS patients whose symptoms are primarily affective and/or cognitive evolve to having minimal PE signs and are capable of exercising to exhaustion during graded treadmill tests without symptom exacerbation. They require a multidisciplinary team approach to treatment that may involve a psychiatrist, a psychologist and/or a neuropsychologist.
Figure 1.
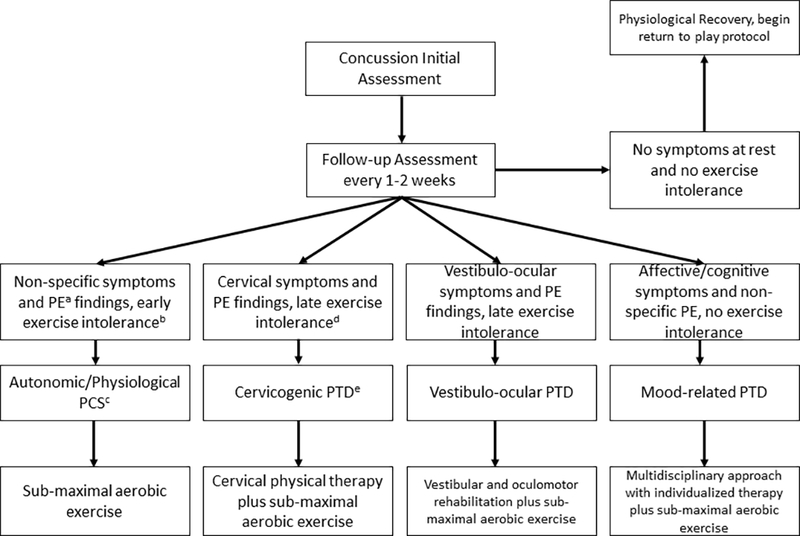
Overview of classification and management.
a: physical examination.
b: Heart rate achieved is below 70% of age-appropriate maximum
c: Post-concussion syndrome
d: Heart rate achieved is 70% or more of age-appropriate maximum at initial assessment
e: Post-traumatic disorder
Physical Examination
A concussion-specific PE should include evaluation of orthostatic vital signs, cranial nerves, and the oculomotor/ophthalmologic, cervical, and vestibular systems. A sample assessment form of the brief BCPE with directions on how to perform it is presented in Table 1. After orthostatic vital signs have been measured, the BCPE takes about 5 minutes to perform, is recommended for clinicians in the outpatient setting, and is convenient enough to perform at every visit.
| Orthostatic Vital Signs | ||
|---|---|---|
| Supine | Standing (after 1 minute) | |
| Blood Pressure (mmHg) | ||
| Heart Rate (bpm) | ||
| Symptoms1 | □ No □ Yes If yes: Description? |
□ No □ Yes If yes: Description? |
| Results | □ Normal □ Abnormal | |
| Test results are deemed clinically significant if they include at least one of the following AND symptomatic: (1) systolic BP drop of ≥ 20mmHg or (2) diastolic BP drop of ≥ 10mmHg. | ||
| Cranial Nerve Exam | ||
|---|---|---|
| □ Performed □ Not performed | ||
| Nerve | Test | Results |
| I – Olfactory | With eyes closed, have the patient plug one nostril and smell distinctive scent (e.g. coffee grounds), repeat on other side. | □ Normal □ Abnormal |
| V – Trigeminal | With eyes closed, touch the patient on the forehead, cheek and jaw while asking if the sensation is the same bilaterally. | □ Normal □ Abnormal |
| VII – Facial | Ask the patient to smile, puff out the cheeks, wrinkle the forehead, and close the eyes tightly. | □ Normal □ Abnormal |
| IX – Glossopharyngeal | Ask the patient to open the mouth and say “ahhh.” | □ Normal □ Abnormal |
| X – Vagus | Ask the patient to swallow. | □ Normal □ Abnormal |
| XI – Accessory | Push down lightly on the patient’s shoulders while the patient shrugs. | □ Normal □ Abnormal |
| XII - Hypoglossal | Ask the patient to stick out the tongue. | □ Normal □ Abnormal |
| Oculomotor/Ophthalmologic Evaluation | ||
|---|---|---|
| Test | Results | Symptoms |
| Fundoscopy | □ Performed □ Not performed |
□ Normal Other: |
| Pupil Reactivity (CN II) | □ Normal □ Abnormal | |
| Visual Tracking (CN III, IV, VI) | □ Normal □ Abnormal | |
| Smooth Pursuits (10 repetitions and then stop, horizontal and vertical) |
□ Normal □ Abnormal Horizontal □ Abnormal Vertical |
□ Nystagmus2 (sign) □ Saccadic movement (sign) □ Dizziness/nausea (symptom) □ Worse headache (symptom) □ Other: |
| Repetitive Saccades3 (30 repetitions horizontal, 30 repetitions vertical) |
□ Normal □ Abnormal Horizontal □ Abnormal Vertical |
□ Nystagmus2 (sign) □ Saccadic movement (sign) □ Dizziness/nausea (symptom) □ Worse headache (symptom) □ Other: |
| VOR (CN VIII) 3 (10 repetitions horizontal, 10 repetitions vertical) |
□ Normal □ Abnormal Horizontal □ Abnormal Vertical |
□ Does not maintain fixation (sign) □ Dizziness/nausea (symptom) □ Worse headache (symptom) □ Other: |
| Near-Point Convergence and Accommodation4 | ||||
|---|---|---|---|---|
| Trial | Convergence (diplopia) |
Convergence Recovery (single image) | Accommodation – Right (blurry) | Accommodation – Left (blurry) |
| 1 | cm | cm | cm | cm |
| 2 | cm | cm | cm | cm |
| Best | cm | cm | cm | cm |
| Neck and Sub-Occipital Region Exam | ||
|---|---|---|
| Palpitation6 | Signs and Symptoms | Location |
| Spasm | □ Normal □ Abnormal | |
| Tenderness | □ Normal □ Abnormal | |
| Cervical Range of Motion | Result | |
| Flexion (50°) | □ Normal □ Abnormal | |
| Extension (60°) | □ Normal □ Abnormal | |
| Right Lateral Flexion (40–45°) | □ Normal □ Abnormal | |
| Left Lateral Flexion (40–45°) | □ Normal □ Abnormal | |
| Right Rotation (80°) | □ Normal □ Abnormal | |
| Left Rotation (80°) | □ Normal □ Abnormal | |
| Postural Control and Motor Coordination | |||
|---|---|---|---|
| Test | Description | Result | Signs/Symptoms |
| Tandem Gait Eyes Open (forward and backward) | Patient walks 5 steps forward and backward heel to toe while looking straight ahead. | □ Normal □ Abnormal |
□ Fall/unstable (sign) □ Over step (sign) □ Dizziness/nausea (symptom) □ Other: |
| Tandem Gait Eyes Closed (forward and backward) | Patient walks 5 steps forward and backward heel to toe with eyes closed. | □ Normal □ Abnormal |
□ Fall/unstable (sign) □ Over step (sign) □ Dizziness/nausea (symptom) □ Other: |
| Tandem Stance | Patient stops walking and stands for 20 seconds in a heel to toe stance with hands on the hips and eyes closed. | □ Normal □ Abnormal |
□ Fall/unstable (sign) □ Dizziness/nausea (symptom) □ Other: |
Total Abnormal Signs
Typical symptoms include dizziness and lightheadedness.
A few beats of fatigable nystagmus at end gaze is normal. Sustained is abnormal.
Abnormality is abnormal response OR symptom provocation.
Prescription glasses are allowed. Measure with an Accommodation Rule.
Directions of Physical Exam
Vital signs: A manual or automated blood pressure cuff is used to measure heart rate (HR) and blood pressure (BP). The first measurement is taken with the patient lying supine on the examination table for at least 2 minutes. The patient is then asked to stand up without support and with both feet firmly on the ground and a second measurement is taken after standing for 1 minute. The patient is asked if any dizziness or lightheadedness is experienced upon standing or by one minute. The test is considered to be clinically significant if symptoms are present plus any of the following: systolic BP drop of ≥ 20 mmHg or diastolic BP drop of ≥ 10 mmHg.
Cranial Nerve tests: CN I-XII are tested using standard cranial nerve testing procedures. This should be done at the initial visit but can be omitted on the subsequent visits if no abnormality is seen.
Fundoscopy: Performed using a standard ophthalmoscope.
Pupil reactivity: In a dimmed room, using a penlight or similar light source, shine light on one of the patient’s pupils and observe the changes in the ipsilateral pupil. Remove the light source and wait until the pupil returns to dilated position. Now shine the light on pupil while observing the contralateral pupil. Normal response is for the ipsilateral and contralateral pupil to constrict. Repeat on other eye.
Visual Tracking: Stand at an arm’s length from the patient. Ask the patient to follow your finger with his/her eyes while keeping the head steady. Using your finger, trace an imaginary “H” or rhomboid shape, making sure that your finger moves far enough out and up/down so that you’re able to see all appropriate eye movements. In the end, slowly bring your finger up to the patient’s nose to check convergence/accommodation response. Patient should be able to track easily and smoothly.
Smooth Pursuits: The patient is asked to visually track an object moving slowly in the horizontal direction with the head stationary. Target movement should be limited to 30 degrees from neutral to avoid eliciting end-gaze nystagmus. Abnormal is sustained beats of nystagmus, staccatic (or jerking) eye motion, loss of conjugate vision, corrective (catch-up or back-up) saccades, loss of visual fixation OR symptom provocation (dizziness, nausea or headache). Repeat in vertical visual plane.
Repetitive saccades: The examiner holds both index fingers three feet apart from each other at half an arm length’s distance from the patient. The patient is instructed to move the eyes side to side in rapid succession in the horizontal visual plane, rapidly switching focus between the examiner’s two index fingers. This is repeated in the vertical plane by having the patient move the eyes vertically in rapid succession between the examiner’s two index fingers, three feet apart, located in the midline of the vertical field. Abnormal responses include delayed initiation of eye movement, slow velocity, or inaccurate movements such as over/undershooting with greater than 1 re-fixation saccade. These eye movements in the healthy population can sometimes elicit eye strain but do not provoke symptoms of increased headache or dizziness. Abnormal movements OR abnormal symptom provocation of increased headache or dizziness is considered to be an abnormal response. Patients are considered to have healthy function when they can do 30 side-to-side motions with normal velocity and accuracy without eliciting symptoms of headache, dizziness or nausea.
Vestibulo-ocular reflex (VOR) or Gaze Stability Test: The patient is asked to focus on the examiner’s thumb located directly in the frontal-central field of vison, approximately 30 cm from the forehead. The patient then rotates the head as rapidly as possible for at least 10 complete turns while maintaining visual fixation on the finger. The eye movements are observed. Any staccatic eye movements, inability to maintain visual fixation (i.e., beating back to the center) OR symptom provocation of headache, dizziness, or lightheadedness is abnormal.
Near Point of Convergence (NPC) and Accommodation: Convergence (binocular) is measured using an Astron ACR/21 Accommodation ruler (Gulden Ophthalmics, Elkins Park, PA, see Figure 2) with a standard single 20/30 card as the visual target. Two measurements are taken by placing the ruler at the forehead just above the subject’s nose. Starting at the furthest distance away from the nose, the target is slowly moved toward the patient’s nose. The distance to convergence (measured to the nearest half centimeter) is recorded when either the patient reports image doubling (not blurring of vision) on the card or when the clinician notices binocular loss of convergence. It is best to have the patient blink at the first report of diplopia and then identify when diplopia occurs as the target is moved forward after the blink. An optional test is to assess Convergence Recovery as the target is moved back away from the subject when vision is reported to be single again. For some patients, NPC is normal but recovery is prolonged. The best of the two measurements is considered and ≥ 10 cm is considered to be abnormal for both NPC and recovery. Accommodation (monocular) is also measured to the nearest half centimeter using the same rule and standard card and is acquired over two trials for each eye. The patient is instructed to cover one eye. Starting at the furthest distance away from the nose, the target is moved slowly toward the patient’s nose. As with NPC, it is best to have the patient blink at the first report of blurred vision and then identify when blurring occurs as the target is moved forward after the blink. Accommodation testing is discontinued when the patient reports blurring (not doubling) of the image. ≥ 12 cm is considered to be abnormal.
Neck and Sub-occipital Region Exam: The patient is asked to demonstrate range of motion of the neck. Flexion, hyper-extension, lateral flexion, and rotation of the neck are tested and recorded as normal if they demonstrate full range of motion in the tested plane. While the patient is lying in the supine position, palpate the musculature of the neck. Begin from the base of the neck starting at the trapezius muscles, up the para-cervical muscles to the nuchal ridges, and then along the occipital ridges. Then palpate the cervical spine itself from the occipital protuberance to the prominence of the T1 vertebra. Tenderness is documented according to the subjective reporting of pain by the patient and spasm according to objective palpation by the examiner.
Tandem Gait with Eyes Open and Closed, and Tandem Stance: The patient is asked to walk in a straight line for 5 steps, heel to toe, with hands at the side, while looking straight ahead on a fixed point on the wall. The patient then walks backwards, toe to heel, along the same line while looking straight ahead. The patient then performs the tandem gait again but with their eyes closed. The patient then performs a tandem stance with hands on their hips and one foot planted directly in front of the other and attempts to hold it for 20 seconds with eyes closed. Inability to walk the line, stumbling, or stepping out of line while walking forward, backward or during tandem stance is abnormal.
Orthostatic Vital Signs:
Autonomic dysregulation is common after a head injury and may present with symptoms of orthostatic hypotension, dizziness or vestibular dysfunction, postural orthostatic tachycardia syndrome (POTS), or altered HR and blood pressure (BP) responses at rest and during exercise.9 According to the American Autonomic Society, orthostatic hypotension (OH) is defined as a 20 mmHg or greater reduction in systolic BP or a >10 mmHg reduction in diastolic BP after 1 and 3 minutes of standing from the supine position.10 Since the prevalence of OH is between 5–30% in the non-concussed population, this change in BP is clinically significant only when it is accompanied by symptoms of dizziness or lightheadedness.11 Patients with symptoms upon standing may have orthostasis and/or a central vestibular injury. HR response is useful since a rise in HR (> 40 beats per minute standing vs. supine) with a drop in BP usually indicates hypovolemia whereas lack of HR response is more consistent with a central neurogenic cause. Patients with symptoms of dizziness or vertigo while supine are more likely to have a peripheral vestibular injury and testing including the Dix-Halpike maneuver or otoscopic examination may be indicated. Orthostatic vital signs are measured only supine to standing since two-thirds of cases can be missed seated to standing.12 Common sources of error for measuring BP include not maintaining the arm at the level of the heart, using an improperly sized cuff, and rapid cuff deflation in those with a slow HR. To save time in clinical practice, orthostatic vital signs can be measured by an allied health professional prior to seeing the physician. See Table 1 for directions.
Cranial Nerve Examination:
Isolated abnormalities may suggest a brainstem lesion and should prompt further investigation. This part of the PE contains those nerves not assessed during the oculomotor portion of the examination and should always be performed in the first clinical visit. It can be omitted in subsequent visits if no abnormality is found. See Table 1 for directions.
Oculomotor/Ophthalmologic Examination:
Fundoscopy should be performed at the first visit using a standard ophthalmoscope to assess abnormalities in the retina. Abnormal results should prompt further imaging. Abnormal smooth pursuits, repetitive saccades, vestibulo-ocular reflex (VOR), near point convergence (NPC, binocular vision), and abnormal accommodation (monocular vision) are present in up to 69% of adolescents after mTBI.13 Persistent dysfunction may warrant examination by a neuro-ophthalmologist and/or imaging (if not previously done) since it may represent lesions in cranial nerves, their nuclei, or the brain stem.14 Abnormal and/or symptomatic repetitive saccades and smooth pursuits (complaints of blurred vision, headache, dizziness) are commonly observed after concussion and may be associated with prolonged recovery.15 Performance of these tests accurately requires experience as they involve observing subtle changes. Quantitative tests such as NPC and accommodation should be performed using a standard accommodation rule (Figure 2). The patient is instructed specifically to report diplopia for NPC and blurred vision for accommodation testing. Due to age-related changes in the eye, normal NPC values are lower in children (diplopia reported > 6 cm from the forehead) than in adults (diplopia reported > 10 cm from the forehead).16 See Table 1 for directions.
Figure 2.
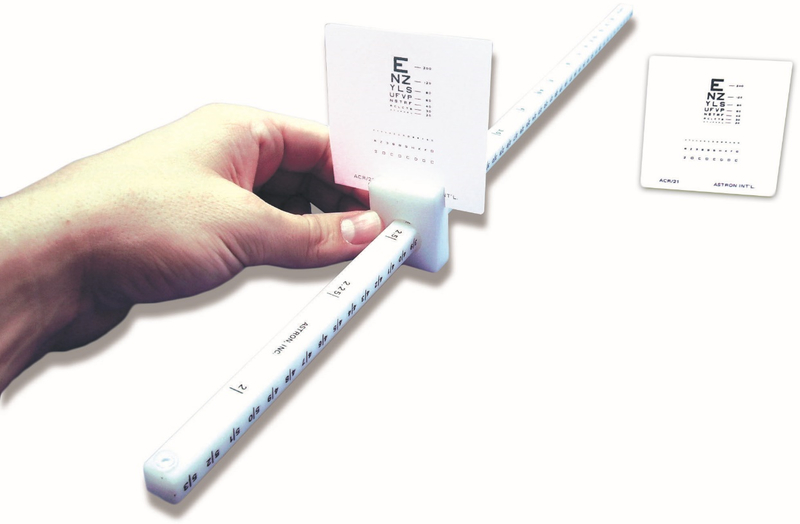
Astron ACR/21 Accommodation Rule by Bernell Corporation, image used with permission from Gulden Ophthalmics, Elkins Park, PA
Cervical Examination:
The neck and sub-occipital regions are frequently involved in head injuries and can cause headaches, persistent dizziness, and balance difficulties.17 Immediately after the injury, the cervical spine should be assessed and managed if needed. In the outpatient setting, typically a few days after the injury, sub-acute neck injuries can closely mimic the symptoms of concussion.17 There may be transient mild symptom exacerbation late in systematic exertion testing but the patient can typically exercise to near maximum for age and fitness level. This pattern distinguishes cervical injury from the early and significant symptom exacerbation that causes patients with physiological PCS to terminate exercise early during systematic exercise assessment. See Table 1 for directions.
Vestibular Examination:
Postural control and motor coordination problems are common after concussion and could lead to further injuries during sport or work.18 Objective signs of vestibular pathology may not be detectable at rest but only upon provocation, potentially pointing to subtle vestibular pathology.15 The Balance Error Scoring System (BESS) test and the modified BESS are validated tests that are typically used to assess balance on the sideline. For clinicians in a busy clinic, tandem gait and tandem stance are more useful tests because of their convenience and high inter-rater reliability.19 Dual task tandem gait tests (for example, reciting the months of the year in reverse during tandem gait) may be more sensitive for unmasking subtle vestibular problems after concussion. See Table 1 for directions.
Supplementary Testing
Sometimes the clinician is not sure if the symptoms are due to concussion, or there may be a particularly prominent symptom (for example, a significant memory problem) that warrants additional testing. Exercise tolerance after concussion may be assessed using a graded aerobic treadmill test such as the Buffalo Concussion Treadmill Test (BCTT). The BCTT is particularly useful for assessing the exercise capacity of patients with PPCS but has been shown to be safe even when performed within the first week after SRC in adolescents.20 Early exercise intolerance (test stopped because of symptom exacerbation of headache or dizziness below 70% of age-appropriate maximum HR) at the initial exam is very sensitive for diagnosing physiological concussion whereas exercise intolerance later in the test (test stopped because of symptom exacerbation or fatigue above 70% of age-appropriate HR maximum) is suggestive of other cause of the symptoms such as cervical injury and/or vestibulo-ocular sub-system dysfunction.21 The HR at symptom exacerbation will improve as the patient recovers so classification is based on the initial test. The ability to exercise to maximum without symptom exacerbation and patient report of a baseline level of symptoms at rest correlates with cardiovascular and cerebrovascular physiological recovery from concussion.20 In those patients with significant vestibular complaints or other injuries that prevent them from walking on a treadmill, an equivalent graded aerobic test can also be performed on a stationary bike with adjustable resistance.22 Exercise that rapidly raises HR, for example weight lifting or sprinting, is not recommended for assessing the symptom exacerbation threshold in concussed patients because they cause a rapid increase in cerebral blood flow. Formal neurocognitive tests are a frequently used and convenient method to assess cognitive difficulties after concussion.23 The use of formal neurocognitive testing (computerized or paper/pencil) for monitoring recovery is not always recommended but should be considered if the patient complains of persistent concentration deficits or a significant deficit was documented during the SAC.7 These patients should be monitored longitudinally until return to baseline (or age-appropriate norm if baseline is not available).
Limitations
This brief concussion PE combines elements of the SCAT5 and the Vestibular/Ocular Motor Screening (VOMS)15 test while adding greater emphasis to assessing autonomic function, dynamic balance and the cervical spine. It is recommended for the outpatient setting and not for sideline use. The BCPE was designed to be used in adolescents and young adults and may therefore not be useful for younger children or older adults. A PE is dependent on physician skill so this examination requires practice. Subtle signs such as abnormal saccadic eye movements, for example, may be missed and have poor inter-rater reliability.24 OH guidelines recommend measuring BP after 1 and 3 minutes of standing whereas we measured it only after 1 minute of standing. The baroreceptor reflex requires only a few seconds to stabilize BP in a healthy state so we assumed that the majority of healthy participants would normalize at the 1-minute time point. Furthermore, performing a 3-minute measurement does not have much clinical utility because it is not routinely performed in the outpatient setting. Finally, this focused PE should not be used in isolation but in combination with a comprehensive history, a cognitive evaluation, and supplementary tests when indicated.
Conclusion
This paper presents a brief, pertinent and practical physical examination for concussed patients, the BCPE, that includes orthostatic vital signs and examinations of the cranial nerves, oculomotor/ophthalmologic, cervical, and vestibular systems. It is recommended that a PE be performed at the initial visit and every 1–2 weeks after SRC. It is important for clinicians to perform a pertinent PE in patients after concussion to help to establish the diagnosis, define recovery, and to identify potential treatment targets in patients with persistent symptoms.
Orthostatic Vital Signs
Supplementary Material
Acknowledgments
Funding:
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under award number 1R01NS094444. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–847. [DOI] [PubMed] [Google Scholar]
- 2.Arbogast KB, Curry AE, Pfeiffer MR, et al. Point of health care entry for youth with concussion within a large pediatric care network. JAMA pediatrics. 2016;170(7):e160294–e160294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kroshus E, Garnett B, Hawrilenko M, Baugh CM, Calzo JP. Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Social Science & Medicine. 2015;134:66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunt AW, Paniccia M, Reed N, Keightley M. Concussion-Like Symptoms in Child and Youth Athletes at Baseline: What Is “Typical”? Journal of athletic training. 2016;51(10):749–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alla S, Sullivan SJ, McCrory P. Defining asymptomatic status following sports concussion: fact or fallacy? British journal of sports medicine. 2012;46(8):562–569. [DOI] [PubMed] [Google Scholar]
- 6.Ellis MJ, Leddy JJ, Willer B. Physiological, vestibulo-ocular and cervicogenic post-concussion disorders: an evidence-based classification system with directions for treatment. Brain injury. 2015;29(2):238–248. [DOI] [PubMed] [Google Scholar]
- 7.Echemendia RJ, Meeuwisse W, McCrory P, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5). Br J Sports Med. 2017:bjsports-2017–097506. [DOI] [PubMed] [Google Scholar]
- 8.Haider MN, Leddy JJ, Baker JG, et al. Concussion management knowledge among residents and students and how to improve it. Concussion. 2017;2(3):CNC40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matuszak JM, McVige J, McPherson J, Willer B, Leddy J. A Practical Concussion Physical Examination Toolbox Evidence-Based Physical Examination for Concussion. Sports Health: A Multidisciplinary Approach. 2016;8(3):260–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clinical Autonomic Research. 2011;21(2):69–72. [DOI] [PubMed] [Google Scholar]
- 11.Low PA. Prevalence of orthostatic hypotension. Clinical Autonomic Research. 2008;18(1):8–13. [DOI] [PubMed] [Google Scholar]
- 12.Cooke J, Carew S, O’connor M, Costelloe A, Sheehy T, Lyons D. Sitting and standing blood pressure measurements are not accurate for the diagnosis of orthostatic hypotension. QJM: An International Journal of Medicine. 2009;102(5):335–339. [DOI] [PubMed] [Google Scholar]
- 13.Master CL, Scheiman M, Gallaway M, et al. Vision Diagnoses Are Common After Concussion in Adolescents. Clinical Pediatrics. 2016;55(3):260–267. [DOI] [PubMed] [Google Scholar]
- 14.Shawkat FS, Kriss A, Thompson D, Russell-Eggitt I, Taylor D, Harris C. Vertical or asymmetric nystagmus need not imply neurological disease. British journal of ophthalmology. 2000;84(2):175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anzalone AJ, Blueitt D, Case T, et al. A Positive Vestibular/Ocular Motor Screening (VOMS) Is Associated With Increased Recovery Time After Sports-Related Concussion in Youth and Adolescent Athletes. The American journal of sports medicine. 2017;45(2):474–479. [DOI] [PubMed] [Google Scholar]
- 16.Ostadimoghaddam H, Hashemi H, Nabovati P, Yekta A, Khabazkhoob M. The distribution of near point of convergence and its association with age, gender and refractive error: a population‐based study. Clinical and Experimental Optometry. 2017;100(3):255–259. [DOI] [PubMed] [Google Scholar]
- 17.Marshall CM, Vernon H, Leddy JJ, Baldwin BA. The role of the cervical spine in post-concussion syndrome. The Physician and sportsmedicine. 2015;43(3):274–284. [DOI] [PubMed] [Google Scholar]
- 18.Kontos AP, Elbin R, Schatz P, et al. A revised factor structure for the post-concussion symptom scale: baseline and postconcussion factors. The American journal of sports medicine. 2012;40(10):2375–2384. [DOI] [PubMed] [Google Scholar]
- 19.Schneiders AG, Sullivan SJ, Gray AR, Hammond-Tooke GD, McCrory PR. Normative values for three clinical measures of motor performance used in the neurological assessment of sports concussion. Journal of Science and medicine in Sport. 2010;13(2):196–201. [DOI] [PubMed] [Google Scholar]
- 20.Leddy JJ, Hinds AL, Miecznikowski J, et al. Safety and prognostic utility of provocative exercise testing in acutely concussed adolescents: a randomized trial. Clinical Journal of Sport Medicine. 2018;28(1):13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leddy JJ, Kozlowski K, Donnelly JP, Pendergast DR, Epstein LH, Willer B. A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clinical Journal of Sport Medicine. 2010;20(1):21–27. [DOI] [PubMed] [Google Scholar]
- 22.Leddy JJ, Haider MN, Ellis M, Willer BS. Exercise is medicine for concussion. Current Sports Medicine Reports. 2018;17(8):262–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haider MN, Leddy JJ, Pavlesen S, et al. A systematic review of criteria used to define recovery from sport-related concussion in youth athletes. British Journal of Sports Medicine. 2017:bjsports-2016–096551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maples W, Ficklin T. Interrater and test-retest reliability of pursuits and saccades. Journal of the American Optometric Association. 1988;59(7):549–552. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


