Abstract
Background:
Children with isolated cleft of the lip and/or palate (iCL/P) are at increased risk for reading impairment. The purpose of this study was to evaluate the impact of early risk factors (hearing, speech, and early literacy) on reading performance compared to unaffected participants with average (uAR) and impaired (uIR) reading.
Methods:
Reading achievement and early literacy skills were evaluated across three groups (27 iCL/P, 32 uAR, and 33 uIR). All participants were males, ages 8 – 11 years old. Those with history of head trauma/injury or major medical/mental health conditions were excluded. Group differences in achievement and early literacy skills were evaluated with ANCOVAs. Participants with impaired reading achievement (at or below 25th Percentile) were identified. Medical record reviews for participates with iCL/P were conducted and audiology and speech ratings recorded. Correlations were calculated between achievement, early literacy, hearing, and speech.
Results:
Participants with iCL/P had significantly elevated risk for reading impairment (37%); this risk differed by cleft type (0% iCL, 55% iCLP, and 60% iCP). Achievement for participants with iCP similar to the uIR group. Early literacy risk resulted in lower achievement scores for both iCL/P and unaffected participants. History of inadequate hearing and speech did not significantly impact early literacy or achievement measures.
Conclusions:
There is a high risk of reading impairment for children with iCL/P – highest for those with iCLP and iCP. Early literacy predictors of reading outcome are similar for iCL/P and idiopathic dyslexia. Current screening and intervention methods are supported.
Keywords: Dyslexia, Cleft, Hearing, Speech
Decades of research have documented deficits in language-based skills among children with isolated cleft lip and/or palate (iCL/P). Case/control (Collett, Stott-Miller, Kapp-Simon, Cunningham, & Speltz, 2010; Conrad, DeVolder, McCoy, Richman, & Nopoulos, 2014; Conrad, Richman, & P., 2015) and population-based studies (Clausen et al., 2016; Collett et al., 2014; Gallagher et al., 2017; Persson, Becker, Conrad, & Svensson, 2018; Persson, Becker, & Svensson, 2012; Wehby et al., 2014; Wehby, Collett, Barron, Romitti, & Ansley, 2015) have reported increased risk for language and reading disabilities. Evaluation of risk factors for these deficits has understandably focused on the potential influence of hearing loss and speech disruption. However, results are mixed (Conrad et al., 2014; Jocelyn, Penko, & Rode, 1996; Lamb, Wilson, & Leeper, 1972; Schonweiler et al., 1999; Shriver, Canady, Richman, Andreasen, & Nopoulos, 2006; Thanawirattananit & Prathanee, 2013). Additionally, research between early otitis media with effusion and later academic language skills in the general population has not produced a strong connection (Fougner et al., 2017; Nylund et al., 2018; Zumach, Gerrits, Chenault, & Anteunis, 2010). This leaves uncertainty on the degree that insults to these sensory domains impact later language and reading achievement. However, across this work, strong patterns of cleft-type differences have emerged (Clausen et al., 2016; Conrad et al., 2015; Persson et al., 2018; Persson et al., 2012; Wehby et al., 2015). Specifically, males with cleft palate only (iCP) are found to be at the highest risk, cleft lip and palate (iCLP) are at some risk, and cleft lip only (iCL) are at minimal risk. This suggests that biological factors may have a stronger contribution to language and reading outcomes for this population.
Idiopathic dyslexia (occurring in the general population, without co-occurring medical conditions) has been extensively researched. Dyslexia is a breakdown of communication between language, visual, and attention neural pathways (Beitchman & Young, 1997; Mather & Wendling, 2012; Shaywitz & Shaywitz, 2005). The two strongest, early predictors of dyslexia are deficits in phonological awareness (ability to recognize and manipulate individual sounds within words) and automaticity (rapid naming of highly learned objects or symbols) (Shaywitz & Shaywitz, 2008). Other studied predictors of reading impairment include auditory rote memory (immediate recall) (Daigneault & Braun, 2002), working memory (recall after manipulation) (Nicolielo-Carrilho, Crenitte, Lopes-Herrera, & Hage, 2018), visual memory (Mather & Wendling, 2012), and attention (Menghini et al., 2010).
Past research on reading in children with iCL/P has also evaluated the roles of traditional early literacy skills (phonological awareness and rapid automatized naming) and other related neuropsychological skills (i.e., auditory memory, visual memory, and attention) (Chapman, 2011; Collett, Leroux, & Speltz, 2010; Collett, Stott-Miller, et al., 2010; Conrad et al., 2014; Conrad et al., 2015; Richman, Eliason, & Lindgren, 1988; Richman & Ryan, 2003). However, in these studies, children with iCL/P are compared to normative data, an unaffected sibling, or a “healthy control” population. No study to date has compared patterns of reading impairment to idiopathic dyslexia. The benefit of such a comparison is the ability to determine if predictors of reading impairment among children with iCL/P are the same as those without iCL/P.
Biologically, this asks the question “Are the phenotypic similarities of reading impairment in children with iCL/P and idiopathic dyslexia caused by breakdowns in similar early literacy skills?” Or, from a clinical viewpoint, “Are the screening measures and interventions we are currently using appropriate for children with iCL/P?”
Methods
Participants
Three groups of males (ages 8 – 11 years) were recruited: unaffected boys with average reading (uAR), unaffected boys with impaired reading (uIR), and boys with iCL/P (regardless of reading ability). Eligibility criteria for all groups included: no history of head trauma/injury and no major medical/mental health conditions (aside from cleft in the iCL/P group).
Recruitment for the uAR group occurred through local advertisements. Average reading achievement at school was required (i.e., no services for reading assistance and no accelerated or talented/gifted programing). Seventy-two potential participants responded. Nineteen (26%) did not respond to follow-up for screening, 20 (28%) did not meet eligibility criteria, 5 (7%) could not be scheduled due to conflicts, and 28 (39%) were scheduled and completed participation. Recruitment for the uIR group occurred through advertisements posted on webpages and Facebook pages of state-wide dyslexia associations (Decoding Dyslexia – [STATE] and the [STATE] Chapter of the International Dyslexia Association). Eligible participants required either a documented diagnosis of dyslexia or participation in Tier 3 (special education) services for reading. Records for all children who participated without a formal diagnosis were reviewed to ensure they had significant deficits in early literacy measures (phonological awareness and/or rapid naming) and reading achievement (decoding and/or fluency). A total of 49 potential participants responded. Ten (20%) did not meet eligibility criteria, 6 (12%) could not be scheduled due to conflicts, and 33 (67%) were scheduled and completed participation.
Recruitment for the iCL/P group occurred through the patient registry of the Cleft Clinic at the [HOSPITAL]. Potential participants were sent letters outlining the details of the project. Those with an identified syndrome were excluded. Fifty-nine potential participants responded. Nine (15%) did not respond to follow-up for screening, 22 (37%) did not meet eligibility criteria, 2 (3%) could not be scheduled due to conflicts, and 26 (44%) were scheduled and completed participation. Three participants were excluded after participation; one had Van der Woude syndrome, one spoke English as a second language, and the other had aged-out.
A subset of 8 participants [4 uAR and 4 iCL/P] from the pilot phase of this study (Conrad et al., 2015) were included in analyses. The final sample included 32 uAR, 33 uIR, and 27 iCL/P (6 iCL, 11 iCLP, and 10 iCP). There were no group differences in age (F 2, 89) = 0.054, p = .948). Despite ruling out TAG and ELP students and all groups having an average or higher mean IQ, the uAR group had significantly higher intelligence than the uIR and iCL/P groups (Welch Statistic (2, 52.63) = 8.319, p = .001). Finally, participants with iCL/P had a significantly higher socioeconomic status score (SES; based on a modified Hollingshed rating scale; reflecting lower parental socioeconomic status) compared to uAR (Welch Statistic (2, 53.68) = 4.515, p = .015). Age (F (2, 24) = 0.850, p = .440), intelligence (F (2, 23) = 0.524, p = .599), and SES (Welch Statistic (2, 14.63) = 1.613, p = .233) were not significantly different between cleft types. (See Table 1).
Table 1.
Mean Demographics (95% Confidence Interval) by Participant Group and Cleft Type.
| Total Sample | iCL/P | |||||
|---|---|---|---|---|---|---|
| uAR | ulR | iCL/P | iCL | iCLP | iCP | |
| Age | 9.94 | 10.01 | 10.03 | 10.21 | 10.30 | 9.63 |
| 9.54–10.34 | 9.61–10.40 | 9.60–10.47 | 9.17–11.24 | 9.54–11.07 | 8.83–10.44 | |
| GAI^ | 112.14 | 104.97‡ | 103.35‡ | 107.50 | 102.80 | 101.40 |
| 109.47–114.80 | 101.29–108.65 | 98.70–108.00 | 97.59–117.41 | 95.12–110.48 | 93.72–109.08 | |
| SES^ | 2.06 | 2.15 | 2.48‡ | 2.17 | 2.45 | 2.70 |
| 1.94–2.19 | 1.99–2.31 | 2.11–2.32 | 1.74–2.60 | 2.10–2.81 | 2.11–3.29 |
Notes. GAI = Global Ability Index. SES = Socioeconomic Status.
Welch statistic and Games-Howell pairwise comparisons due to heterogeneity of variances. ^Significantly different than uAR.
Significantly different than uAR.
All parents were asked to self-report if their child had any learning, attention, or psychosocial diagnoses as well as if they were receiving any services through the school or private tutoring. As expected by design, no participants in the uAR group had a pre-existing diagnosis and only one received a school service (speech therapy). Similarly, the majority of participants in the uIR group had pre-existing diagnoses (82%) and received school services (91%). Among participants with iCL/P, only 4 had a pre-existing diagnosis (15%) and 6 received services through the school (22%). (See Table 2). Exploratory analyses of iCL/P participants with either a pre-existing diagnosis or school services (total n = 8) compared to those without (n = 19) did not yield any significant differences in demographic, achievement, or early literacy measures.
Table 2.
Rates of Pre-Existing Diagnoses and School Services by Particinant Tyne.
| uAR n=32 | iCL n=6 | iCLP n=11 | iCP n=10 | uIR n=33 | |
|---|---|---|---|---|---|
| Diagnoses | 0 | 1 | 1 | 2 | 27 |
| Dyslexia | 0 | 0 | 0 | 1 | 20 |
| ADHD | 0 | 1 | 1 | 0 | 1 |
| ADHD + LD | 0 | 0 | 0 | 0 | 3 |
| Sneech | 0 | 0 | 0 | 1 | 0 |
| Mixed | 0 | 0 | 0 | 0 | 3 |
| Services | 1 | 2 | 1 | 3 | 30 |
| Title 1 Reading | 0 | 0 | 1 | 0 | 2 |
| 504 Plan | 0 | 0 | 0 | 0 | 8 |
| IEP | 1 | 1 | 0 | 2 | 17 |
| Unspecified | 0 | 1 | 0 | 1 | 3 |
Notes. ADHD = Attention Deficit/Hyperactivity Disorder. LD = Learning Disorder. IEP = Individual Education Plan.
Protocol
All procedures were approved by the local Institutional Review Board. Prior to participation, the Research Assistant met with families to discuss the details of the study and review the consent form. Legal guardians provided written consent and participants provided verbal and written assent. Guardians were reimbursed for travel expenses and participants were monetarily compensated. Participation took place in 1 day during a visit to the [HOSPITAL]. All groups completed the same 4 hour protocol of neuropsychological and achievement assessment.
Intelligence
Select subtests from the Wechsler Intelligence Test for Children, 5th Edition (WISC-V) (Wechsler, 2014) were administered to obtain an overall Global Ability Index (GAI). This widely-used cognitive battery included subtests assessing verbal skills (Similarities [verbally describing abstract relationships between two given words] and Vocabulary [defining a given word]), visual skills (Block Design [2-dimensional figure construction]), and fluid reasoning (Matrix Reasoning [identifying patterns in matrices with different designs and finding the missing piece], and Figure Weights [using learned relationships between given figures to determine a missing piece]). Participants in the pilot study were administered 4 overlapping subtests (Similarities, Vocabulary, Block Design, and Matrix Reasoning) from the Wechsler Abbreviated Scale of Intelligence, 2nd Edition (WASI-II) (Wechsler, 2011) to obtain a 4-subtest Full Scale IQ score (FSIQ). These composite scores were used interchangeably for demographic purposes.
Achievement Battery
Select subtests from the Woodcock Reading Mastery Test, 3rd Edition (WRMT-III) (Woodcock, 2011) were administered to assess achievement. Word Identification (WI) provided a measure of single word reading accuracy. In Word Attack, participants read aloud a list of nonwords (words that are not actual words, but which can be pronounced using rules of the English language [e.g., RIX], this assessed nonword decoding (NWD). Oral Reading Fluency (ORF) measured rate and accuracy while reading paragraphs aloud. In Paragraph Comprehension, participants were given sentences/paragraphs and had to fill in a missing word. This provided a measure of reading comprehension (RComp). Finally, on Listening Comprehension (LComp), participants listened to short passages and responded to questions about them. This evaluated the ability to pull meaning from information heard aloud.
Early Literacy
Phonological Awareness:
Two subtests from the Comprehensive Test of Phonological Processing (CTOPP) (Wagner, Torgesen, & Rashotte, 1999) were administered: Sound Blending (participants listen to a word, one phoneme at a time and need to blend the sounds together to find the word) and Elision (participants are given a word and are asked to say what word remains when a part of that word is removed). Scores on these subtests were averaged to create a Phonological Awareness composite score (PhAw).
Rapid Automatized Naming:
Two subtests from the CTOPP were administered: Digit Naming and Letter Naming. Participants were shown separate grids of numbers and letters and asked to read them aloud as quickly as possible. Scores on these subtests were averaged to create a Rapid Automatized Naming composite score (RAN).
Auditory Rote Memory:
The Digits Forward trial on the Digit Span subtest from the WISC-V was used as one test of auditory rote memory. (For the pilot study, the comparable Memory for Digits subtest from the CTOPP was used). In both tasks, participants listen to a series of numbers and have to repeat them back in the same order. Additionally, the Nonword Repetition subtest from the CTOPP was used as a secondary measure. Here, participants are given a nonword and have to repeat it. Scores on these subtests were averaged to create an Auditory Rote Memory composite score (RoteMem).
Auditory Working Memory:
The Digits Backward and Digits Sequencing trials on the Digit Span subtest from the WISC-V were averaged to create an Auditory Working Memory composite score (AudWM). For these subtests, participants listen to a series of numbers and then either say them back in reverse order (Backwards trial) or in sequential order (Sequencing trial). (These subtests were not administered to participants in the pilot study.)
Visual Memory:
The Picture Sequences subtest from the WISC-V was used as a test of visual memory (VisMem). Participants are shown a series of pictures and then asked to recall them in order. (This subtest was not administered to participants in the pilot study.)
Attention:
Participants were administered the Connors Continuous Performance Test, 3rd Edition (CPT-III) (Conners, 2014) to measure sustained attention. In this test, participants watch a screen and are asked to hit the spacebar as quickly as they can after seeing a letter. However, they are told to not hit the spacebar if the letter is an “x”. Number of omission errors (reversed so that higher scores indicated better performance) was used as a measure of Attention (Attn). (This test was not administered to participants in the pilot study.)
Medical Chart Review
For participants with iCL/P, medical charts were systematically reviewed for information on hearing and speech history. Audiology and speech records were available for 25 and 26 participants (respectively).
Hearing:
Values for all Speech Detection Threshold (lowest level of sound intensity at which a sound can be heard) and Speech Reception Threshold (lowest level of sound intensity at which the spoken word is identified 50% of the time) were recorded with lower threshold scores indicating better hearing. Number of assessments per participant ranged from 1 to 18; participants with iCLP had significantly more evaluations than participants with iCL or iCP. Participants with iCLP and iCL had earlier age of first evaluation compared to participants with iCP. To best capture the potential impact of hearing impairment on early literacy and reading outcomes, worst audiology score was used as the measure of interest. Values ranged from 0 to 100 dB, where 0 was best and values above 15 – 20 dB can be indicative of a hearing issue depending upon the age of subject at testing (“First Years,” 2004). There was no cleft type difference in worst audiology score. (See Table 3).
Table 3.
Hearing and Speech Measures; Mean Values (95% Confidence Interval) by Cleft Type.
| iCL | iCLP | iCP | F | p-value | |
|---|---|---|---|---|---|
| Audiology | |||||
| Number of Evaluations | 6.33|| | 10.80 | 3.33|| | 10.929 | .001 |
| 3.62–9.05 | 8.70–12.91 | 0.62–6.05 | |||
| Age at Youngest Evaluation | 1.47ƪ | 1.62ƪ | 3.89 | 6.516 | .007 |
| 0.32–2.63 | 0.72–2.51 | 2.74–5.04 | |||
| Worst Audiology Score | 25.00 | 26.00 | 28.33 | 0.122 | .886 |
| 13.39–36.61 | 17.00–35.00 | 18.85–37.82 | |||
| Speech | |||||
| Number of Evaluations | 4.50|| | 9.09 | 5.70|| | 3.579 | .044 |
| 1.33–7.67 | 6.75–11.44 | 3.24–8.16 | |||
| Age at Youngest Evaluation | 2.13 | 2.06 | 3.05 | 1.342 | .281 |
| 0.89–3.36 | 1.10–3.01 | 2.09–4.00 |
Notes.
Significantly lower than iCLP.
Significantly lower than iCP.
Speech:
The number of speech evaluations per participant from 1 to 18. Participants with iCLP had more speech evaluations than those with iCL or iCP (See Table 4). Youngest age of evaluation ranged from 1 to 6 years old and did not differ between the three cleft types.
Velopharyngeal insufficiency (VPI) is when the soft palate does not fully close off the airway between the nasal cavity and the mouth when producing specific sounds. Among participants with iCL/P, This structural abnormality was marginal to inadequate in 69% of the iCL/P sample. Deficits were most common in those with iCP (90%) and iCLP (80%), while minimal in iCL (17%).
Ranked severity scores (None, One, Some/Mild, and Multiple) for 4 common speech errors were obtained. Distortion errors (producing a sound in an unfamiliar manner) were most common in those with iCLP (100% at mild or multiple), and moderate for iCL (60% and iCP (68%), Developmental errors (common errors found in typically developing children),were evenly distributed for iCL participants (50% at mild or multiple), but elevated for iCP (62%) and iCLP (67%). Compensatory errors (learned articulation errors) were only present for those with iCP (20% multiple) and iCLP (39%). Finally, obligatory errors (errors due to structural abnormalities) were only noted in participants with iCLP (63% mild).
Table 4.
Mean (95% Confidence Interval) Percentile Rank on Reading Achievement and Early Literacy Measures Across Groups.
| uAR | iCL | iCLP | iCP | uIR | F Statistic | p-value | |
|---|---|---|---|---|---|---|---|
| Achievement | |||||||
| WI | 61.20# | 66.76# | 44.76 | 35.3 | 17.12 | 21.404 | <.001 |
| 53.85–68.56 | 50.09–83.43 | 32.26-57.26 | 21.74-49.04 | 9.99-24.25 | |||
| NWD^ | 59.53# | 49.83 | 44.82 | 40.60 | 21.1’ | 20.189 | <.001 |
| 51.22–67.85 | 21.11–78.56 | 21.29-68.35 | 21.14-60.06 | 15.25-27.09 | |||
| ORF^ | 55.12# | 54.83# | 39.36 | 27.2 | 14.63 | 21.564 | <.001 |
| 47.34–62.90 | 33.22–76.45 | 22.72-56.00 | 11.41–43 | 9.77-19.48 | |||
| RComp | 60.42# | 78.27# | 66.60 | 53.6 | 34.18 | 6.509 | <.001 |
| 50.81–70.03 | 56.52-100.03 | 49.43-83.77 | 35.81-71.41 | 24.73-43.63 | |||
| LComp | 81.20 | 77.97 | 89.31 | 66.77 | 75.82 | 1.444 | .228 |
| 73.32–89.08 | 61.31–94.63 | 76.03-102.59 | 49.42-84.12 | 68.71-82.94 | |||
| Early Literacy | |||||||
| PhAw | 68.32# | 69.59 | 63.39 | 61.9 | 53.36 | 2.550 | .045 |
| 61.14–75.50 | 53.32–85.87 | 51.19-75.59 | 48.60-75.25 | 46.40-60.32 | |||
| RAN^ | 55.00# | 44.67 | 46.77 | 35.95 | 27.18 | 6.070 | <.001 |
| 45.01–64.99 | 29.23–60.10 | 29.19-64.36 | 22.90-49.00 | 20.08-34.27 | |||
| RoteMem^ | 48.11# | 39.92 | 43.59 | 28.70 | 31.35 | 6.828 | .001 |
| 42.52–53.70 | 10.46–69.38 | 24.30-62.88 | 22.96-34.44 | 23.19-39.50 | |||
| AudWM | 61.81# | 52.06 | 51.80 | 51.90 | 38.39 | 4.420 | .003 |
| 53.44–70.17 | 34.35–69.78 | 38.41-65.18 | 33.45-70.34 | 30.83-45.96 | |||
| VisWM | 63.92 | 82.27 | 70.75 | 53.12 | 52.26 | 2.186 | .078 |
| 53.03–74.82 | 59.63-104.91 | 52.71-88.79 | 29.55-76.69 | 42.58-61.93 | |||
| Attn | 38.15 | 43.52 | 39.61 | 41.4 | 41.2 | 0.074 | .990 |
| 27.75–48.55 | 19.21–67.83 | 21.19-58.03 | 20.27-62.63 | 31.68-50.81 |
Notes.
Welch statistic due to heterogeneity of variance. WI = Word Identification. NWD = Nonword Decoding. ORF = Oral Reading Fluency. RComp = Reading Comprehension. LComp = Listening Comprehension. PhAw = Phonological Awareness. RAN = Rapid Automatized Naming, RoteMem = Auditory Rote Memory. AudWM = Auditory Working Memory. VisMem = Visual Memory. Attn = Attention.
Significantly higher than uIR. %Significantly higher than iCP.
Similar to audiology measures, worst speech score for each variable of interest was used in analyses. Cleft type differences in speech ratings could not be calculated due to low cell sizes.
Analyses
Differences in Achievement
Separate univariate analyses of covariance (ANCOVA) were run to assess group differences in reading achievement. Because the purpose of this design was to evaluate differences in relation to unaffected average and impaired readers, as well as the previously established pattern of cleft type differences, the independent variable was group membership across 5 separate groups: uAR, iCL, iCLP, iCP, and uIR. Socioeconomic status (SES) was included as a covariate. Dependent variables included the 5 achievement measures (WI, NWD, ORF, RComp, and LComp). Welch statistics were used if homogeneity of variance was violated.
To evaluate clinical levels of concern, “impaired reading” was operationally defined as a score at or below the 25th Percentile on any reading accuracy or fluency subtest (WI, NWD, or ORF). Low expected cell sizes did not permit evaluation across the cleft type level, so Chi-Square analyses were run for uAR, iCL/P, and uIR to evaluate impairment across the different participant groups. Observed counts were compared with expected rates of 75% no risk and 25% at risk. Descriptive rates were also calculated for cleft type iCL, iCLP, and iCP.
Differences in Early Literacy
Univariate ANCOVAs were run to calculate group differences on measures of early literacy (PhAw, RAN, RoteMem, AudWM, VisMem, and Attn as dependent variables). Analyses were again run with 5 group membership as the independent factor and co-varying for SES.
Predictors of Reading Achievement
Early Literacy:
Due to restriction of range among the uAR and uIR participant groups, they were combined to create an “unaffected” (no cleft) group. Pearson correlations were run separately for “unaffected” and “affected” participants. Relationships between early literacy and achievement measures were calculated.
Hearing and Speech:
Spearman-Rho correlations were calculated between hearing, speech, early literacy, and achievement measures.
Results
Achievement
See Table 4 for mean percentile rank by participant group across the different achievement measures. Significant differences were found for WI, NWD, ORF, and RComp. Pairwise comparisons (with Bonferroni correction for ANCOVAs and Games-Howell for Welch) demonstrated a consistent pattern of participants in the uIR group performing significantly lower than those in the uAR group. Those in the uIR group were also significantly lower than those with iCL and iCLP on WI, ORF, and RComp. There were no significant differences between uIR and iCP. Participants with iCP were significantly lower than uAR and iCL on WI as well as lower than uAR on ORF.
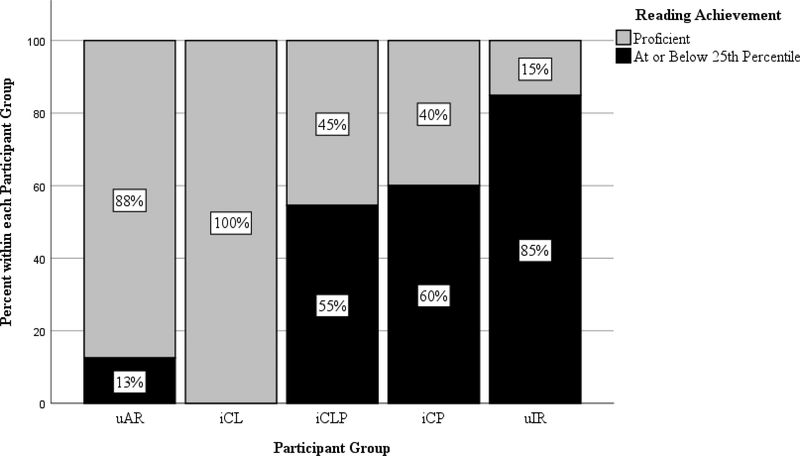
As expected, a very small percentage of participants in the uAR group met clinical criteria for impaired reading (13%; Chi-Square = 2.667, p = .102) while this rate was significantly elevated for the uIR group (85%; Chi-Square = 63.040, p < .001). There was a significant proportion of children with iCL/P who met criteria for impaired reading (44%; Chi-Square = 5.444, p = .020). When looking across cleft types, there was no risk for iCL (0%) and elevated risk for both iCLP (55%) and iCP (60%). (See Figure 1).
Figure 1.
Rates of Clinical Risk for Reading Impairment by Participant Group.
Early Literacy
See Table 4 for mean percentile rank by participant group across early literacy domains. Results of the ANCOVAs evaluating overall group differences indicated significant differences in PhAw, RAN, RoteMem, and AudWM; uIR had significantly lower scores than uAR and participants with iCP had significantly lower RoteMem than uAR.
Predictors of Reading Achievement
Early Literacy:
Results from the Pearson Correlations evaluating the relationship of early literacy on reading achievement for both “affected” and “unaffected” participants indicated similar patterns. For “unaffected” participants, early literacy measures of PhAw, RAN, RoteMem, and AudWM had strong positive correlations to reading achievement measures. While PhAw and RAN were also positively correlated for “affected” participants, RoteMEM and AudWM were only associated to decoding skills and Attn was an additional predictor of decoding, but this relationship was not significant after Bonferroni correction. (See Table 5).
Table 5.
Pearson Correlations for Unaffected and iCL/P Participants between Early Literacy and Achievement Measures.
| Word Identification | Nonword Decoding | Achievement Oral Reading Fluency | Reading Comp. | Listening Comp. | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unaff | iCL/P | Unaff | iCL/P | Unaff | iCL/P | Unaff | iCL/P | Unaff | iCL/P | |
| Early Literacy | ||||||||||
| PhAw | .496* | .672** | .532** | .761** | .382** | .606** | .365** | .443* | .277* | .188 |
| RAN | .448* | .394* | .626** | .435* | .700** | .630** | .404** | .355 | .254* | .521* |
| RoteMem | .396* | .390* | .366** | .494** | .464** | .297 | .480** | .164 | .130 | .096 |
| AudWM | .462* | .270 | .476** | .595** | .436** | .068 | .394** | .311 | .206 | .208 |
| VisMem | .227 | .384 | .213 | .307 | .299* | .482* | .248 | .451* | .149 | .486* |
| Attn | .012 | .451* | .077 | .470* | −.142 | .349 | .057 | .360 | .107 | .015 |
Notes. PhAw = Phonological Awareness. RAN = Rapid Automatized Naming, RoteMem = Auditory Rote Memory. AudWM = Auditory Working Memory. VisMem = Visual Memory. Attn = Attention.
Uncorrected p < .05 (Not significant after Bonferroni correction.)
Uncorrected p < .01 (Remains significant after Bonferroni correction.)
Uncorrected p < .001 (Remains significant after Bonferroni correction.)
Hearing and Speech:
Among participates with iCL/P, Spearman Rho correlations between ratings of audiology/speech and measures of achievement/early literacy yielded very few significant correlations. Worse VPI was associated with worse WI, ORF, and VisMem, but this did not remain significant after Bonferroni correction. (See Table 6).
Table 6.
Spearman Rho for iCL/P Participants between Hearing/Speech Ratings and Early Literacy and Achievement Measures.
| Hearing/Speech | ||||||
|---|---|---|---|---|---|---|
| Audiology | Dist. | Dev. | Comp. | Oblig. | VPI | |
| Achievement | ||||||
| WI | − | −0.358 | −0.190 | −0.237 | −0.337 | −0.455* |
| 0.010 | ||||||
| NWD | 0.120 | 0.102 | −0.148 | −0.315 | −0.291 | −0.272 |
| ORF | 0.209 | −0.024 | −0.188 | −0.138 | −0.166 | −0.407* |
| RComp | 0.008 | −0.046 | −0.164 | 0.097 | −0.028 | −0.240 |
| LComp | 0.051 | 0.159 | 0.211 | 0.207 | 0.099 | −0.158 |
| Early Literacy | ||||||
| PhAw | 0.014 | −0.101 | −0.139 | −0.251 | −0.419 | −0.276 |
| RAN | 0.159 | 0.211 | −0.011 | −0.044 | −0.148 | −0.286 |
| RoteMem | −0.059 | −0.267 | −0.043 | −0.165 | −0.425 | 0.006 |
| AudWM | 0.088 | 0.063 | 0.254 | 0.072 | −0.159 | 0.127 |
| VisMem | 0.176 | −0.034 | −0.107 | −0.078 | −0.413 | −0.525* |
| Attn | 0.063 | 0.092 | −0.174 | −0.295 | −0.343 | −0.322 |
Notes. Dist. = Distortion Errors. Dev. = Developmental Errors. Comp. = Compensatory Errors. Oblig. = Obligatory Errors. VPI = Velopharyngeal Insufficiency. WI = Word Identification. NWD = Nonword Decoding. ORF = Oral Reading Fluency. RComp = Reading Comprehension. LComp = Listening Comprehension. PhAw = Phonological Awareness. RAN = Rapid Automatized Naming, RoteMem = Auditory Rote Memory. AudWM = Auditory Working Memory. VisMem = Visual Memory. Attn = Attention.
Uncorrected p < .05 (Not significant after Bonferroni correction.)
Discussion
Evaluation of reading outcomes replicated previous cleft type differences: those with iCP had the lowest scores, iCLP were in the middle, and iCL had minimal risk. While both iCL and iCLP were higher than uIR on decoding, fluency, and comprehension measures, iCP was never significantly different from uIR. Areas of deficit for those with iCP were single word reading and reading fluency. The most surprising finding was that despite only 1 of 27 participants with iCL/P entering the study with a diagnosis of dyslexia (4%), the rate of reading impairment was 37% (as high as 60% among iCP). This is significantly greater than the expected risk and indicates that there is a substantial amount of reading issues going unnoticed among children with iCL/P.
Participants with uIR had expected deficits in nearly all early literacy measures. While participants with iCL/P were somewhat lower across these measures, differences only reached significance for participants with iCP on rote auditory memory. This finding is in contrast to previous work identifying deficits in phonological awareness and rapid automatized naming (Chapman, 2011; Collett, Stott-Miller, et al., 2010; Richman et al., 1988; Richman & Ryan, 2003). Low auditory memory has been identified among iCL/P, and it has been associated with deficits in single word decoding (Conrad et al., 2015).
Even though traditional early literacy measures were not statistically deficient for participants with iCL/P, lower scores on PhAw and RAN were associated with deficits in reading accuracy and fluency. Deficits in RoteMem and AudWM were only associated with issues in NWD. This is consistent with the global pattern among unaffected participants, where poor performance on PhAw, RAN, RoteMem, and AudWM predicted poor performance on all the reading achievement measures. The relationship between early literacy and reading achievement appears to be similar for unaffected and affected participants.
History of hearing and speech impairment impact early literacy or achievement measures. There were non-significant trends for VPI to be related to lower reading accuracy and fluency. However, effect sizes were small and inconsistent across measures (VPI was also associated with worse visual memory; a relationship that would not be expected). While speech deficits likely do have a role in the development of phonological awareness and decoding skills, there are stronger factors impacting this development. Work in this area needs to continue to elucidate these relationships. Findings in hearing and speech measures should be interpreted with caution as they were obtained through medical chart reviews; a method that is limited in what data is available, quality of the data, and the retrospective manner of collection.
Conclusion
The next steps in evaluating reading outcomes among children with iCL/P will involve assessing the impact of language as well as the relationship to brain structure and connectivity (both planned within this lab). This will help further identify the interplay of biological factors (i.e., cleft type) and neuropsychological patterns. Females also need to be included to clarify sex differences. Past work has identified different cleft type patterns for females (Persson et al., 2018) and this needs to be re-evaluated with larger samples. Finally, studies utilizing neuroimaging have suggested that the academic deficits found among children with iCL/P may be related to abnormal neural migration (Conrad et al., 2015; Goldsberry, O’Leary, Hichwa, & Nopoulos, 2006; Nopoulos et al., 2000; Nopoulos, Langbehn, Canady, Magnotta, & Richman, 2007). This theory has also been proposed in idiopathic dyslexia (Galaburda, Fitch, LoTurco, & Rosen, 2011). Genetic studies between children with iCL/P and idiopathic dyslexia may shed more light on this hypothesis and the potential overlap of deficits between these two populations. Clinically, practitioners need to be aware of the heightened risk for reading deficits among children with iCL/P. Regular screening should be conducted; results from this study continue to support the evaluation of phonological awareness and rapid automatized naming. Parents should be educated on early “red flags” for dyslexia and how to appropriately advocate for their children’s needs within the school system.
Acknowledgements:
The author would like to acknowledge the contributions of Ian DeVolder, PhD and Emily Kuhlmann, BA in data collection as well as Scott Dailey, PhD in guidance with speech data collection and analysis. Thank-you to the chapter leaders at Decoding Dyslexia and the International Dyslexia Association who made recruitment so successful. Finally, thank-you to the families who participated in this study; their time and effort is greatly appreciated.
Funding Source: Research reported in this publication was supported by the National Institute of Dental and Craniofacial Research (award number DE024511) and the National Center for Advancing Translational Sciences of the National Institutes of Health (award number UL1TR002537).
References
- Beitchman JH, & Young AR (1997). Learning disorders with a special emphasis on reading disorders: a review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 36(8), 1020–1032. doi: 10.1097/00004583-199708000-00009 [DOI] [PubMed] [Google Scholar]
- Chapman KL (2011). The relationship between early reading skills and speech and language performance in young children with cleft lip and palate. Cleft Palate Craniofac J, 48(3), 301–311. doi: 10.1597/08-213 [DOI] [PubMed] [Google Scholar]
- Clausen NG, Pedersen DA, Pedersen JK, Moller SE, Grosen D, Wehby GL, . . . Hansen TG (2016). Oral Clefts and Academic Performance in Adolescence: The Impact of Anesthesia-Related Neurotoxicity, Timing of Surgery, and Type of Oral Clefts. Cleft Palate Craniofac J. doi: 10.1597/15-185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collett BR, Leroux B, & Speltz ML (2010). Language and early reading among children with orofacial clefts. The Cleft Palate-Craniofacial Journal, 47(3), 284–292. doi: 10.1597/08-172.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collett BR, Stott-Miller M, Kapp-Simon KA, Cunningham ML, & Speltz ML (2010). Reading in children with orofacial clefts versus controls. Journal of pediatric psychology, 35(2), 199–208. doi: 10.1093/jpepsy/jsp047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collett BR, Wehby GL, Barron S, Romitti PA, Ansley TN, & Speltz ML (2014). Academic achievement in children with oral clefts versus unaffected siblings. J Pediatr Psychol, 39(7), 743–751. doi: 10.1093/jpepsy/jsu049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conners CK (2014). Conners Continuous Performance Test, 3rd Edition: Technical Manual. North Tonawanda, NY: Multi-Health Systems Inc. [Google Scholar]
- Conrad AL, DeVolder I, McCoy T, Richman L, & Nopoulos P (2014). Reading in Subjects with an Oral Cleft: Speech, Hearing and Neuropsychological Skills. Neuropsychology, 28(3), 415–422. doi: 10.1037/neu0000024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad AL, Richman LC, & P., N. (2015). Reading Achievement in Boys With NonSyndromic Cleft Palate Only: Relationship to Neuropsychological Skill and Neurocircuitry. Developmental Neuropsychology, 40(7–8), 395–406. doi: 10.1080/87565641.2016.1142991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daigneault S, & Braun CM (2002). Pure severe dyslexia after a perinatal focal lesion: evidence of a specific module for acquisition of reading. J Dev Behav Pediatr, 23(4), 256–265. [DOI] [PubMed] [Google Scholar]
- First Years. (2004, September 2011). Retrieved from http://www.firstyears.org/lib/howtoread.htm
- Fougner V, Korvel-Hanquist A, Koch A, Dammeyer J, Niclasen J, Lous J, & Homoe P (2017). Early childhood otitis media and later school performance - A prospective cohort study of associations. Int J Pediatr Otorhinolaryngol, 94, 87–94. doi: 10.1016/j.ijporl.2017.01.016 [DOI] [PubMed] [Google Scholar]
- Galaburda AM, Fitch RH, LoTurco JL, & Rosen G (2011). Neurogenetic Contribution to Developmental Reading Disorders In McCardle P, Miller B, Lee J. Ren, & Tzeng OJL (Eds.), Dyslexia Across Languages: Orthography and teh Brain-Gene-Behavior Link (pp. 226–238). Baltimore, Maryland: Paul Brookes Publishing Co. [Google Scholar]
- Gallagher ER, Collett BR, Barron S, Romitti P, Ansley T, & Wehby GL (2017). Laterality of Oral Clefts and Academic Achievement. Pediatrics, 139(2). doi: 10.1542/peds.2016-2662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsberry G, O’Leary D, Hichwa R, & Nopoulos P (2006). Functional abnormalities in the neural circuitry of reading in men with nonsyndromic clefts of the lip or palate. Cleft Palate Craniofacial Journal, 43(6), 683–690. [DOI] [PubMed] [Google Scholar]
- Jocelyn LJ, Penko MA, & Rode HL (1996). Cognition, communication, and hearing in young children with cleft lip and palate and in control children: a longitudinal study. Pediatrics, 97(4), 529–534. [PubMed] [Google Scholar]
- Lamb MM, Wilson FB, & Leeper HA Jr. (1972). A comparison of selected cleft palate children and their siblings on the variables of intelligence, hearing loss, and visualperceptual-motor abilities. Cleft Palate Journal, 9, 218–228. [PubMed] [Google Scholar]
- Mather N, & Wendling BJ (2012). Essentials of Dyslexia Assessment and Intervention. Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Menghini D, Finzi A, Benassi M, Bolzani R, Facoetti A, Giovagnoli S, . . . Vicari S (2010). Different underlying neurocognitive deficits in developmental dyslexia: a comparative study. Neuropsychologia, 48(4), 863–872. doi: 10.1016/j.neuropsychologia.2009.11.003 [DOI] [PubMed] [Google Scholar]
- Nicolielo-Carrilho AP, Crenitte PAP, Lopes-Herrera SA, & Hage SRV (2018). Relationship between phonological working memory, metacognitive skills and reading comprehension in children with learning disabilities. J Appl Oral Sci, 26, e20170414. doi: 10.1590/1678-7757-2017-0414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nopoulos P, Berg S, Canady J, Richman L, Van Demark D, & Andreasen NC (2000). Abnormal brain morphology in patients with isolated cleft lip, cleft palate, or both: a preliminary analysis. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association, 37(5), 441–446. doi:;2 [DOI] [PubMed] [Google Scholar]
- Nopoulos P, Langbehn DR, Canady J, Magnotta V, & Richman L (2007). Abnormal brain structure in children with isolated clefts of the lip or palate. Archives of pediatrics & adolescent medicine, 161(8), 753–758.17679656 [Google Scholar]
- Nylund A, Toivonen L, Korpilahti P, Kaljonen A, Peltola V, & Rautakoski P (2018). Recurrent respiratory tract infections or acute otitis media were not a risk factor for vocabulary development in children at 13 and 24 months of age. Acta paediatrica (Oslo, Norway : 1992). doi: 10.1111/apa.14546 [DOI] [PubMed] [Google Scholar]
- Persson M, Becker M, Conrad AL, & Svensson H (2018). Female and Male Differences in Academic Achievement in Individuals With Cleft: A Population-Based Register Study. Cleft Palate Craniofac J, 55(2), 196–203. doi: 10.1177/1055665617726990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson M, Becker M, & Svensson H (2012). Academic achievement in individuals with cleft: a population-based register study. Cleft Palate Craniofac J, 49(2), 153–159. doi: 10.1597/09-047 [DOI] [PubMed] [Google Scholar]
- Richman LC, Eliason MJ, & Lindgren SD (1988). Reading disability in children with clefts. Cleft Palate J, 25(1), 21–25. [PubMed] [Google Scholar]
- Richman LC, & Ryan SM (2003). Do the reading disabilities of children with cleft fit into current models of developmental dyslexia? Cleft Palate Craniofac J, 40(2), 154–157. [DOI] [PubMed] [Google Scholar]
- Schonweiler R, Lisson JA, Schonweiler B, Eckardt A, Ptok M, Trankmann J, & Hausamen JE (1999). A retrospective study of hearing, speech and language function in children with clefts following palatoplasty and veloplasty procedures at 18–24 months of age. Int J Pediatr Otorhinolaryngol, 50(3), 205–217. [DOI] [PubMed] [Google Scholar]
- Shaywitz SE, & Shaywitz BA (2005). Dyslexia (specific reading disability). Biological psychiatry, 57(11), 1301–1309. doi: 10.1016/j.biopsych.2005.01.043 [DOI] [PubMed] [Google Scholar]
- Shaywitz SE, & Shaywitz BA (2008). Paying attention to reading: the neurobiology of reading and dyslexia. Development and psychopathology, 20(4), 1329–1349. doi: 10.1017/S0954579408000631 [DOI] [PubMed] [Google Scholar]
- Shriver AS, Canady J, Richman L, Andreasen NC, & Nopoulos P (2006). Structure and function of the superior temporal plane in adult males with cleft lip and palate: pathologic enlargement with no relationship to childhood hearing deficits. Journal of Child Psychology and Psychiatry, 47(10), 994–1002. [DOI] [PubMed] [Google Scholar]
- Thanawirattananit P, & Prathanee B (2013). Relationship of language development and hearing status in children with cleft lip and palate. J Med Assoc Thai, 96 Suppl 4, S49–54. [PubMed] [Google Scholar]
- Wagner RK, Torgesen JK, & Rashotte CA (1999). Comprehensive Test of Phonological Processing. Austin, TX: PRO-ED. [Google Scholar]
- Wechsler. (2011). Wechsler Abbreviated Scale of Intelligence - Second Edition Manual. Bloomington, MN: Pearson. [Google Scholar]
- Wechsler. (2014). Wechsler Intelligence Scale for Children, Fifth Edition. United States of America: PsychCorp. [Google Scholar]
- Wehby GL, Collet B, Barron S, Romitti PA, Ansley TN, & Speltz M (2014). Academic achievement of children and adolescents with oral clefts. Pediatrics, 133(5), 785–792. doi: 10.1542/peds.2013-3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehby GL, Collett BR, Barron S, Romitti P, & Ansley T (2015). Children with oral clefts are at greater risk for persistent low achievement in school than classmates. Arch Dis Child, 100(12), 1148–1154. doi: 10.1136/archdischild-2015-308358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodcock RW (2011). Woodcock Reading Mastery Tests, Third Edition Manual. Bloomington, MN: Pearson. [Google Scholar]
- Zumach A, Gerrits E, Chenault M, & Anteunis L (2010). Long-term effects of early-life otitis media on language development. J Speech Lang Hear Res, 53(1), 34–43. doi: 10.1044/1092-4388(2009/08-0250) [DOI] [PubMed] [Google Scholar]