Abstract
Objectives
We sought to develop and implement a Maternity Dashboard to improve the quality of health care at the ground level.
Methods
We conducted a prospective, descriptive cross-sectional study, involving patients with high-risk pregnancies who had been referred to Nizwa Hospital, Oman. The selection of quality indicators was based on the prototype of clinical outcomes from the Royal College of Obstetricians and Gynecologists. The Maternity Dashboard team adapted local parameters and used preselected general parameters, based on clinical observations, to develop the dashboard.
Results
The issues posing a threat to Nizwa Hospital in becoming a world-class healthcare facility were: overbooked outpatient department, insufficient staff, and more junior doctors compared to senior doctors and consultants. Additionally, being pioneers, naturally, the dashboard development team faced difficulties while handling adverse situations. More time, guidance, and standardization of quality indicators are desirable.
Conclusions
Following the approval for a Maternity Dashboard in Nizwa Hospital, the data compiled in an Excel sheet are transmitted manually every month for display on the dashboard in the delivery suite. It is intended to make data collected and dissemination completely automated in the future with the help of the Al-Shifa Healthcare Information System. Expansion of the idea of a Maternity Dashboard to other hospitals and specialties at the regional and tertiary level of the health care system in Oman and a comparison of the standard of health care provided between hospitals based on similar quality indicators would be the next milestone.
Keywords: Patient Safety; Quality Indicators, Health Care; Obstetrics; Gynecology
Introduction
The quality of clinical care and patient safety is crucial for the health care system, and the responsibility for building a culture of safety lies with the health care organizations. The maintenance of high standards demands well-advised monitoring of clinical care, which assures adherence to guidelines or protocols and clinical outcome as part of a standardized set of quality indicators (QIs),1-3 and analysis of the patient feedback to ensure excellent patient-centered healthcare, and safety. For a continuous improvement in the quality of healthcare, the implementation of effective care and the desired outcomes require continuous monitoring by setting certain standards against which the performance is monitored.4 The concept of health is in itself complex; therefore, monitoring it using health indicators involves equal complexity due to which potential opportunities for improvement in quality care at ground level could be overlooked and would create obstruction in patient safety. Altogether, such indicators should display the health status of a specific population and help in the surveillance of health conditions.5
A wide range of quality improvement tools and methods are being employed by healthcare authorities and professionals globally that involves the collection, monitoring, evaluation, and reviewing of data by local, national, and even international bodies to put healthcare in the right perspective. The Oman healthcare system, which offers free primary health care to Omani nationals, and subsidized care for the foreign population, follows the same objectives.6 The commitment towards the development and implementation of QIs has been largely stimulated by the introduction of computerized administrative and clinical databases, and the need to publish performance data.7
‘Clinical dashboards,’ a new promising tool, have transformed the way healthcare professionals and senior leaders monitor organizational performance and prioritize improvement by timely interventions. The principle was adapted from the dashboard of a car and cockpit display of an airplane. It provides the updated rates or frequencies of key/selected QIs at a glance and provides information for quality assurance and exception reporting. Multiple hospitals have successfully employed dashboards in different medical specialties, with positive results.8-11 Looking at the growing interest in the dashboard as an adjunct, ‘Maternity Dashboard,’ a clinical performance and governance scorecard that enables monitoring of various preselected parameters on a monthly basis, has been recommended by the Royal College of Obstetricians and Gynecologists (RCOG) for use in all maternity units. The Maternity Dashboard is designed to compare the current performance against expected standards and ensure that the principles of clinical governance are safeguarded in daily clinical practice (good practice).12 The visual representation of data acts as an early warning system, with each QI used to identify suboptimal performance that might otherwise pass undetected.
Our study sought to evaluate the potential of a visual display of clinical performance and outcome in improving the quality of health care at the ground level by developing and implementing a Maternity Dashboard.
Methods
This prospective, descriptive cross-sectional study was conducted between January and December 2017, in patients with high-risk pregnancies who had been referred to Nizwa Hospital. Nizwa Hospital is a senior consultant-led hospital, and the only regional referral hospital in the large A'Dakhliya governorate catering to a population of 326 521 people, and at present handles between 6000 to 7000 deliveries per year. All high-risk pregnancies within the governorate are referred to this hospital.
A situation where either the mother or her fetus, or both, are at risk is known as a high-risk pregnancy. Two types of medical conditions put a pregnancy at risk. The medical conditions that exist before pregnancy include high blood pressure, polycystic ovary syndrome, lung, kidney, or heart problems, obesity, diabetes, autoimmune diseases, chronic infections like HIV, and sexually transmitted diseases. Other factors include conditions that develop during pregnancy such as preeclampsia, gestational diabetes, premature labor, multiple births, hemorrhage during pregnancy, grand multiparity, and teenage pregnancy.
The implementation of a dashboard requires a core set of QIs with clear definition and predetermined gold standards/benchmark/threshold. QIs are measurable elements that help in understanding a performance and its outcome so that they can be compared with the gold standard and improved if necessary. The RCOG has recently produced a prototype set of intrapartum clinical outcomes, which are measurable and can be improved by practicing it in line with the ‘Good Practice Series’ on the Maternity Dashboard.13,14 The key to an effective dashboard is to use a limited number of meaningful measurements, in accordance to local need. In addition to the preselected general parameter, local parameters were adapted by the Maternity Dashboard team, based on clinical observations that required improvement.15 Box 1 shows the selected parameters which are broadly categorized into clinical activity, maternal outcome, and neonatal outcome measures.
Box 1: Indicators used in the Maternity Dashboard.
| Indicators |
|---|
| Clinical activities |
| Deliveries |
| Admission to the antenatal ward (excluding direct admission to the delivery suite) |
| Outpatient department appointment |
| Instrumental deliveries |
| Cesarean section rate |
| Maternal measures |
| Induction of labor |
| Workforce |
| Midwife/patient ratio |
| Supervisor/midwife ratio |
| Eclampsia |
| Intensive care unit admission |
| Severe postpartum hemorrhage |
| Third-degree perineal tear |
| Shoulder dystocia |
| Hematomas |
| Postpartum hysterectomy |
| Others (e.g., near miss/mortality) |
| Neonatal outcomes |
| Low five-minute Apgar score (< 7) |
| Perinatal asphyxia |
| Meconium aspiration syndrome |
| Stillbirth |
| Stillbirth with diabetes |
| Early neonatal death |
| Patient complaints |
Data were collected manually from the labor ward register and through electronic records (i.e., Al-Shifa, a comprehensive healthcare information system used in Oman designed to manage the operations of a hospital or a network of healthcare units).
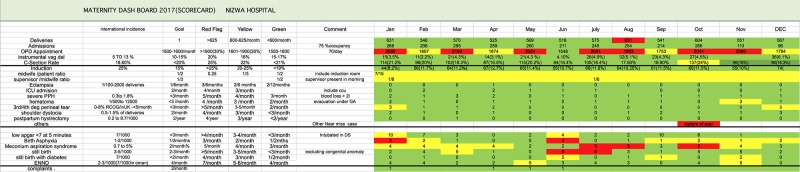
A user-friendly Maternity Dashboard was produced in Microsoft Excel 2016. The display of the dashboard was placed in the delivery suite for a monthly review by frontline staff. It included indicators, international incidences, and local set goals. Upper and lower limits for each parameter were decided by the Maternity Dashboard team. A traffic light color-coded system was used to give immediate visual feedback at the ground level. Green was used when the goals were met, amber to indicate that the goals were not met (i.e., above the lower threshold, but still within the upper threshold), and red was used when the upper threshold was breached. When a parameter falls into the amber zone, action should be taken to restore normalcy (green color) with minimal resources; a careful observation was warranted to ensure patient safety (no immediate risk to patients), and the parameter trend was studied in the following months. However, repeated entry of a single parameter into the amber zone would necessitate corrective action to avoid deterioration to red. Any indicator that fell in the red zone may pose an impending threat to patient safety and needed urgent attention and appropriate action to avoid the quality of maternity care provided from being adversely affected.
Results
The Maternity Dashboard proved impactful in driving changes for the better functioning of the healthcare system at our hospital. Clear and transparent dissemination of data enhanced the decision-making process. Analysis of the recorded data provided a powerful way to project the difference between the actual performance and the expected goals. The green color code, which was frequently assigned in this study, identified the parameters whose performance was up to the gold standard. These parameters were consistently assigned with green color, reflecting the dedication of the health care providers and such an acknowledgment of their efforts encouraged them further to maintain high standards of work.
The areas of weaknesses were highlighted by amber and red colors, which warranted immediate attention to bring the indicator color back to green [Figure 1]. For example, the overbooked outpatient department appointments were found to be consistently in the amber or red zone, unable to turn green within the study period. Meetings were arranged with the medical record department to limit the number of appointments. Walk-in outpatient department appointments were withheld. The clinical staff was advised to refer patients in the low-risk group to their parent centers for follow-up. Meetings were conducted with all the primary and secondary health providers, and the local guidelines for referrals were revised, with persistent monitoring of the decided guidelines. By the end of the year, the parameter showed signs of a return to normalcy. The amber code in case of third/fourth-degree perineal tear and hematomas demanded an audit that would recognize the areas of weaknesses. The midwife-to-patient and supervisor-to-midwife ratios remained consistently in the amber zone throughout the study period, leading to the new enrolment of midwives. Since the new health care providers would need more supervision and further training, one-to-one hands-on training programs and more supervision were arranged in collaboration with the Maternal and Child Health Unit and senior midwives. A request was sent to the higher authorities to employ 15 more midwives to reduce the burden of the over-worked staff, which is still not resolved. The parameters for neonatal outcome measures, such as perinatal asphyxia, meconium aspiration syndrome, and stillbirths fluctuated between the amber and red zone. Monthly perinatal asphyxia cases were presented in perinatal mortality meetings, where the faults were highlighted, and appropriate actions were decided to prevent such incidents in the future. A bereavement team was formed for a detailed case study and counseling of the care provider. Local workshops and e-learning further strengthened cardiotocograph training.
Figure 1.
Screenshot of Maternity Dashboard of Nizwa Hospital, 2017.
Discussion
The clinical dashboard consistently displayed ward and program activities. The transparency of data dissemination between the clinicians and midwives promoted optimal patient care within the department. Early recognition of adverse performance trends supported informed decision-making and resource allocation within the local setting. Monitoring of the various parameters identified the outpatient flow as the main issue that needed immediate action. By repeated meetings with regional heads and local health stakeholders, we were able to control the outpatient flow. Similarly, St. George’s Hospital, UK, had repeatedly experienced a red zone for many women booked for birth. They used the Maternity Dashboard as a tool to convince the Trust Board and local commissioners to reduce the number of bookings keeping patient safety as a priority; the timely induction of labor16 achieved a reduction in the stillbirth rate after the implementation of the remedial measures.
Although the use of the Maternity Dashboard was an invaluable experience to analyze the monthly clinical performances, we faced a set of challenges while developing the dashboard. A Maternity Dashboard is a fairly new concept in Oman, and our unit is the pioneer in its implementation. The critical challenge was to select the key performance indicators or QIs and set the benchmark/gold standard to provide safety to the patients. The key performance indicators should be relevant, specific, measurable, achievable, and time-bound. The difficulty lies in the fact that there are no standardized indicators, neither local nor international. There are 290 maternity outcomes,1 compiled from the publications of four professional bodies, which include the RCOG, American College of Obstetricians and Gynecologists, Royal Australian and New Zealand College of Obstetricians and Gynecologists, and the Society of Obstetrician and Gynecologists of Canada. The four bodies suggested using the RCOG produced prototype indicators as they are in line with the good guide indicator.12-16 A survey of consultant-led maternity units in the South West of England Strategic Health Authority region,17 concluded that there was wide variation in the key performance indicators monitored and their definition. They stressed upon the requirement for a meaningful, internationally agreed, standardized core set of maternity QIs, along with their optimal thresholds to avert adverse outcomes. The lack of a common system obstructs the comparison of the QIs and identification of those parameters that need attention. Data collection from all maternity units should be automated and easily accessible to all maternity units, which would help in standardizing the Maternity Dashboard.17-21 Another challenge faced during the establishment of the Maternity Dashboard was the shortage of senior doctors and consultants. Although the junior doctors were well-trained, rectifying the underscored indicators became a demanding task. Continuous shortage of midwives and clinicians was brought to the notice of local and national bodies. However, the gap in recruitment persists. We hope that persistent reminders to the local head of the departments will resolve this ongoing issue soon. Sustenance, or in other words, the consistency in the continuity of the Maternity Dashboard is a challenge, for which the strength, validity, and reliability of the key performance indicators should be periodically revised and modified using integrated data management. Maternity Dashboard demands both individual and collective efforts to continuously improve patient care and outcomes, which warrants a significant time commitment and good quality data.15
Nizwa Hospital in Oman, is an accredited patient-friendly hospital with a mission to provide a high level of health care and ensure patient safety. This can be achieved by continuous monitoring of the QIs in the Maternity Dashboard and taking immediate actions to ameliorate the threats before they manifest into actual harm. Thus, implementation of the Maternity Dashboard could be one of the dynamic tools providing information for quality assurance and exception reporting. The visual representation of data would act as an early warning system, with individual QIs helping in the identification of suboptimal performances that might otherwise pass undetected.
Moreover, the other hospitals in Oman can also adopt such a dashboard as the Ministry of Health electronic portal Al-Shifa is designed to manage the operations of a hospital or a network of healthcare units. The exchange of information all over the world using such a system is not yet possible, but with the advances in technology, it may become attainable in the future.
Conclusion
The concept of Maternity Dashboard was accepted by the quality assurance committee and the Director of Nizwa Hospital. At present, the data, compiled in an Excel sheet, are transmitted manually every month, for display on the dashboard in the delivery suite. In the future, software for the construction of Maternity Dashboard would be developed, using Oman’s Al-Shifa system to disseminate the information to health care providers, locally and nationally. In addition, the clinical dashboard would be introduced in other hospitals and specialties at the regional and tertiary level of the health care system in Oman. In the future, we might be able to compare the quality of performance of various hospitals using similar QIs.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
We acknowledge Dr. Ilham M. Hamdi, FRCOG, Senior Consultant, Jalila Mansoor Al-Mazrooi, MCH Unit Head. Dr Qameriya Am Busaidi, Fetal Medicine Specialist Head of Department, Nizwa Hospital.
References
- 1.Draycott T, Sibanda T, Laxton C, Winter C, Mahmood T, Fox R. Quality improvement demands quality measurement. BJOG 2010. Dec;117(13):1571-1574. 10.1111/j.1471-0528.2010.02734.x [DOI] [PubMed] [Google Scholar]
- 2.Clancy CM, Farquhar MB, Sharp BA. Patient safety in nursing practice. J Nurs Care Qual 2005. Jul-Sep;20(3):193-197. 10.1097/00001786-200507000-00001 [DOI] [PubMed] [Google Scholar]
- 3.Boulkedid R, Alberti C, Sibony O. Quality indicator development and implementation in maternity units. Best Pract Res Clin Obstet Gynaecol 2013. Aug;27(4):609-619. 10.1016/j.bpobgyn.2013.04.001 [DOI] [PubMed] [Google Scholar]
- 4.Department of Health. Quality and performance in the NHS. High-level performance indicators and clinical indicators. [cited 18 July 2018]. Available from: (URL) www.performance.doh.gov.uk/indicat/nhsci.htm.
- 5.Gaspar J, Chagas J, Osanan GC, Cruz-Correa R, Reis ZS. Maternal and neonatal healthcare information system: development of an obstetric electronic health record and health care indicators dashboard. ITBAM 2013. Springer, Berlin, Heidelberg. p. 62-76. [Google Scholar]
- 6.World Health Organization. Monitoring, evaluation and review of national health strategies: a country- led platform for information and accountability. Geneva: WHO. November 2011.
- 7.Majeed A, Lester H, Bindman AB. Improving the quality of care with performance indicators. BMJ 2007. Nov;335(7626):916-918. 10.1136/bmj.39337.539120.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stone-Griffith S, Englebright JD, Cheung D, Korwek KM, Perlin JB. Data-driven process and operational improvement in the emergency department: the ED Dashboard and Reporting Application. J Healthc Manag 2012. May-Jun;57(3):167-180, discussion 180-181. 10.1097/00115514-201205000-00006 [DOI] [PubMed] [Google Scholar]
- 9.Khemani S, Patel P, Singh A, Kalan A, Cumberworth V. Clinical dashboards in otolaryngology. Clin Otolaryngol 2010. Jun;35(3):251-253. 10.1111/j.1749-4486.2010.02143.x [DOI] [PubMed] [Google Scholar]
- 10.Health Department of Intrapartum-related deaths: 500 missed opportunities. Chief Medical Officer’s annual report 2006. Chapter 6: Intrapartum-related deaths: 500 missed opportunities. London: The Stationery Office; 2007 [cited 18 July 2018]. Available from: https://webarchive.nationalarchives.gov.uk/20130105021806/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4135795.
- 11.Bakos KK, Zimmermann D, Moriconi D. Implementing the clinical dashboard at VCUHS. NI 2012 (2012). 2012;2012:011. [PMC free article] [PubMed]
- 12.Arulkumaran S, Chandraharan E, Mahmood T, Louca O, Mannion C. Maternity dashboard -clinical performance and governance scorecard. RCOG. Good Practice 2008;7:1-8. [Google Scholar]
- 13.Pencheon D. The good indicators guide: understanding how to use and choose indicators. NHS Institute for Innovation and Improvement; 2008. [Google Scholar]
- 14.Chandraharan E, Arulkumaran S. The role of clinical dashboards in improving patient care: experience with the ‘Maternity Dashboard’. Ceylon Med J 2016. Jun;61(2):83-85. 10.4038/cmj.v61i2.8291 [DOI] [PubMed] [Google Scholar]
- 15.Muhammad S, Chandraharan E. The maternity dashboard: how effective is it in improving maternity care? Obstetrics, Gynaecol Reprod Med 2016;26(9):276-279 . 10.1016/j.ogrm.2016.06.002 [DOI] [Google Scholar]
- 16.Draycott TJ, Crofts JF, Ash JP, Wilson LV, Yard E, Sibanda T, et al. Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol 2008. Jul;112(1):14-20. 10.1097/AOG.0b013e31817bbc61 [DOI] [PubMed] [Google Scholar]
- 17.Yigitbasioglu O, Velcu O. A review of dashboards in performance management: implications for design and research. Int J Account Inf Syst 2012;13(1):41-59 . 10.1016/j.accinf.2011.08.002 [DOI] [Google Scholar]
- 18.Simms RA, Ping H, Yelland A, Beringer AJ, Fox R, Draycott TJ. Development of maternity dashboards across a UK health region; current practice, continuing problems. Eur J Obstet Gynecol Reprod Biol 2013. Sep;170(1):119-124. 10.1016/j.ejogrb.2013.06.003 [DOI] [PubMed] [Google Scholar]
- 19.Mitchell PH. Defining patient safety and quality care. In: Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008. [PubMed] [Google Scholar]
- 20.Lilford R, Mohammed MA, Spiegelhalter D, Thomson R. Use and misuse of process and outcome data in managing performance of acute medical care: avoiding institutional stigma. Lancet 2004. Apr;363(9415):1147-1154. 10.1016/S0140-6736(04)15901-1 [DOI] [PubMed] [Google Scholar]
- 21.Sprague AE, Dunn SI, Fell DB, Harrold J, Walker MC, Kelly S, et al. Measuring quality in maternal-newborn care: developing a clinical dashboard. J Obstet Gynaecol Can 2013. Jan;35(1):29-38. 10.1016/S1701-2163(15)31045-8 [DOI] [PubMed] [Google Scholar]