Abstract
Objective
To evaluate the linkage of claims from the Utah All Payers Claims Database (APCD) and Utah Cancer Registry (UCR).
Data Sources
Secondary data from 2013 and 2014 Utah APCD and 2013 UCR cases.
Study Design
This is a descriptive analysis of the quality of linkage between APCD claims data and cancer registry cases.
Data Collection/Extraction Methods
We used the LinkPlus software to link Utah APCD and UCR data.
Principal Findings
We were able to link 82.4 percent (9441/11 453) of the UCR reportable cancer cases with APCD claims. Of those linked, 66 percent were perfect matches.
Conclusions
The quality of identifiers is high, evidence that claims data can potentially supplement cancer registry data for use in research.
Keywords: cancer, claims database, linkage, registry
1. INTRODUCTION
An All Payer Claims Database (APCD) is a tool used by public health agencies to “fill critical information gaps for state agencies, to support health care and payment reform initiatives, and to address the need for transparency in health care at the state”.1 An APCD collects claims data across health care insurance providers (payers) and compiles information on claims representing treatment by inpatient and outpatient providers as well as pharmacy claims.2 Fourteen states have APCDs, five are in development, and several more are interested in development.3 The Utah Department of Health (UDOH) is one of the early developers and adopters of an APCD.4
The utility of claims data for cancer surveillance and research has been demonstrated using Medicare claims, with evidence that claims capture cancer treatment that is otherwise under‐reported to central cancer registries.5, 6 However, Medicare data are limited to the population aged 65 and older, whereas an APCD can collect data for all age‐groups.1 An APCD can capture inpatient and outpatient cancer treatment including outpatient pharmacies. As a result, the claims data could be of value for assessing comorbidities at time of diagnosis of cancer, for late effects of treatment, and for recurrence. Thus, APCD data are a significant potential resource for data for cancer surveillance and research, but quality of the data for linkage has not been evaluated.
Our objectives were to evaluate linkage between the Utah APCD and Central Cancer Registry and to describe cancer case characteristics associated with coverage by the APCD.
2. METHODS
2.1. APCD data
Commercial health insurance carriers with 2500 or more covered lives in Utah are required to submit to Utah APCD. Utah's APCD is estimated to represent over 90 percent of individuals covered by group or individual commercial health insurance plans.7 Medicaid claims are reported, but Medicare does not submit claims to the state, nor do the Veterans Health Administration (VHA) or military TRICARE system. Medicare Supplement and Medicare Advantage policies complement the federal Medicare program and are offered through commercial insurers. Because of this when commercial payers submit data to the APCD, claims for care for the Medicare‐eligible population paid under these programs may be included.7 Care that is self‐paid by the patient is not captured by the APCD.
The APCD data structure for inpatient and outpatient claims incorporates data elements from the electronic CMS‐1500 and UB04 claims forms. Each claim includes identifiers for patient, provider, and insurer, date of service, charges, diagnosis codes, and Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes for medical procedures, services, and supplies. The pharmacy claims data structure is based on a National Council for Prescription Drug Programs (NCPDP) standard format, containing identifiers for patient, provider, and insurer, charges, National Drug Code (NDC), and drug name. Data are processed for UDOH, including matching claims for each individual within the APCD, by 3M Health Information Systems, Inc. (“3M”) using a deterministic matching algorithm. The UDOH makes APCD datasets available for research by request, starting with the year 2013.
2.2. Linking to cancer registry data
The Utah Cancer Registry (UCR) is the population‐based central cancer registry for the state of Utah and has been a participant in the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) program8 since 1973. The Utah Cancer Registry is recognized by SEER and by the North American Association for Central Cancer Registries as consistently meeting or exceeding standards of 98 percent completeness of ascertainment of cancer cases among state residents. Data items for each case describe the cancer diagnosis (month and year of diagnosis, cancer site, histology, and stage at diagnosis), patient demographics (age at diagnosis, county of residence, race, and ethnicity), and cancer treatment and survival. UCR data are collected according to a standardized set of cancer registry data definitions and codes.9 Cancer cases reported to the Utah Cancer Registry are subject to manual consolidation and editing by UCR's certified tumor registrars. This includes, as needed, contacting reporting facilities to resolve identifier information if items such as birth date or spelling of the name differ from different reporting sources.
For this study, APCD data files were provided by UDOH for patients with APCD claims in 2013 and 2014. An APCD patient record file, one row per person, was used for linkage. For patients who linked, claims records, multiple rows per patient, were later provided. Both 2013 and 2014 claims data were of interest for cancer cases diagnosed in 2013 because some cancer treatment occurs months after cancer is diagnosed. We matched 2013 UCR cases with treatment claims data from calendar years 2013 and 2014.
Social security numbers (SSNs) were encrypted into a record linkage number (RLN).10 SSN in the UCR data was encrypted using the same key as the APCD. Linkage of APCD patient records to UCR cases diagnosed in 2013 was conducted using LinkPlus software,11, 12 using first name, last name, middle name, maiden name, date of birth, and encrypted SSN. LinkPlus is a software tool developed by CDC and was selected for this study because it is the software used by most central cancer registries to link individuals reported as having a cancer diagnosis to identifiers in other datasets.
Pairs of records that are determined by LinkPlus to match exactly on four identifiers, SSN, last name, first name, and date of birth, are categorized as perfect matches. Pairs of records that match on some but not all of these four identifiers are categorized as partial matches. LinkPlus generates a linkage score for each partial match. Each identifier (SSN, last name, first name, and date of birth) that exactly matches increases the linkage score. Rare names generate a higher positive score than common names that match. Near matches of specific identifiers (eg, Soundex of two similar‐sounding names like Kaitlin and Caitlyn) increase the score, but less so than an exact match. LinkPlus compares residential addresses and flags any nonmatching addresses for partial matches. A manual review of pairs of records categorized by LinkPlus as partial matches was conducted to confirm as linked or no link.
2.3. Data analysis
We summarized UCR 2013 cancer cases linked and not linked to APCD according to number of identifiers matched and the linkage score. Because our interest was in feasibility of using APCD to capture information about cancer cases known to a registry, we calculated the linkage rate as the percent of UCR 2013 cases successfully linked to an APCD patient. We evaluated variation in linkage rate by cancer case characteristics including age at diagnosis and cancer site. We estimated odds ratios (ORs) from a multivariable logistic regression model examining demographic and cancer characteristics for the odds of linking the cancer registry case to an APCD patient. We summarized the number of claims in the APCD by patient, both for medical claims (inpatient and outpatient) and for pharmacy claims.
3. RESULTS
The UCR file included 11 453 individuals with SEER‐reportable cancers diagnosed in 2013. We received APCD identifier records representing 2 945 920 unique patients with 2013 and 2014 claims for linkage. Perfect matches on the four identifiers were found for 6233 cancer cases, partial matches for 3760, and no potential matching record for 1460 (Table 1). Among cases with partial matches, 2262 had high linkage scores and matching addresses and were accepted as matches without manual review. Among partial linkages, the mean and median linkage scores were 25.3 and 24.8, respectively. Partial matches with linkage scores between 23 and 10 were manually reviewed. Partial matches were accepted as linked‐based matching address and/or based on professional judgment that nonmatching fields likely represented key entry errors or similar minor data issues. Among Utah residents with records matched on date of birth, first name, and last name, but missing SSN in one or the other dataset, fewer than 1 percent (6 of 2376) were not confirmed as true links. After the linkage and manual review, 9441 cancer cases, or 82 percent, had confirmed linkage to an APCD record. There were two instances in which one cancer case linked to more than one APCD patient record.
Table 1.
Results of linkage between Utah All Payer Claims Database (APCD) and Central Cancer Registry by Type of Identifier Matched and Linkage Score
| Linked | No link | |||
|---|---|---|---|---|
| n | Column % | n | Column% | |
| Total | 9441 | 2012 | ||
| Identifiers matched | ||||
| Perfect match on four identifiersa | 6233 | 66.0 | 0 | |
| Partial match | 3208 | 34.0 | 552 | 27.4 |
| Partial matches by identifiers matched | ||||
| DOB, first name, last name | 2370 | 25.1 | 6 | 0.3 |
| DOB, last name, SSN | 371 | 3.9 | 0 | |
| DOB, first name, SSN | 171 | 1.8 | 0 | |
| DOB, last name | 108 | 1.1 | 34 | 1.7 |
| DOB, first name | 67 | 0.7 | 99 | 4.9 |
| SSN, any other combination | 53 | 0.6 | 6 | 0.3 |
| SSN, first name, last name | 39 | 0.4 | 0 | |
| First name, last name | 20 | 0.2 | 207 | 10.3 |
| Other | 7 | 0.1 | 200 | 9.9 |
| No potential matches | 0 | 0 | 1460 | 72.6 |
| Linkage Scoreb | ||||
| >40 | 640 | 6.8 | 0 | |
| 35.1‐40 | 4359 | 46.2 | 0 | |
| 30.0‐35 | 1668 | 17.7 | 0 | |
| 25.1‐30 | 1069 | 11.3 | 0 | |
| 20.0‐25 | 1488 | 15.8 | 6 | 0.3 |
| 15.1‐20 | 193 | 2.0 | 20 | 1.0 |
| 10.0‐15 | 24 | 0.3 | 526 | 26.1 |
| No potential matches | 0 | 0 | 1460 | 72.6 |
Date of birth (DOB), first name, last name, and social security number (SSN).
Score assigned by LinkPlus software.
We examined cancer case characteristics that were associated with differences in likelihood of linking to an APCD patient record (Table 2). Among patients diagnosed with cancer below age 50, 90 percent linked to APCD, as did 87 percent of cases diagnosed between ages 50 and 64. The likelihood of linkage to APCD became lower for cases diagnosed at ages 65 to 74, and 75 and older (77 percent and 75 percent, respectively). Other demographic characteristics associated with a lower linkage rate were Hispanic ethnicity (78 percent, compared to non‐Hispanic whites at 83 percent) and rural residence (76 percent compared to 83 percent of patients living in an urban area). There was some variability in linkage rate according to cancer site, but only the lower linkage rate for colorectal cancer (80 percent compared to 86 percent of breast cancer) was statistically significant in the adjusted model. Medicaid as primary insurance was associated with a high linkage rate of 97 percent, whereas patients who were uninsured or covered by Medicare or other government programs had relatively lower odds of linkage to APCD. Patients who were deceased within 3 months of cancer diagnosis had a low proportion linked to claims.
Table 2.
Reportable cancers diagnosed in Utah 2013 linked to Utah all payer claims database records, by demographic and cancer variables
| Linked | Linkage rate (row %) | Odds ratio | 95% CI | |||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Totala | 9441 | 2012 | 82 | |||
| Age at diagnosis | ||||||
| Under 50 | 1966 | 230 | 90 | 1 | Ref | |
| 50‐64 | 3160 | 457 | 87 | 0.99 | 0.83 | 1.19 |
| 65‐74 | 2312 | 642 | 78 | 0.72 | 0.58 | 0.89 |
| 75 and older | 2003 | 683 | 75 | 0.61 | 0.49 | 0.75 |
| Race and ethnicity | ||||||
| Non‐Hispanic white | 8498 | 1772 | 83 | 1 | Ref | |
| Hispanic, any race | 544 | 153 | 78 | 0.72 | 0.58 | 0.89 |
| Black | 77 | 21 | 79 | 0.76 | 0.45 | 1.30 |
| American Indian or Alaskan Native | 48 | 6 | 89 | 3.84 | 1.54 | 9.56 |
| Asian or Pacific Islander | 200 | 41 | 83 | 1.07 | 0.74 | 1.54 |
| Unknown | 74 | 19 | 80 | 0.77 | 0.45 | 1.30 |
| County of residence | ||||||
| Urban | 8361 | 1676 | 83 | 1 | Ref | |
| Rural | 1080 | 336 | 76 | 0.62 | 0.54 | 0.71 |
| Site | ||||||
| Breast | 1463 | 241 | 86 | 1 | Ref | |
| Colorectal | 692 | 177 | 80 | 0.76 | 0.60 | 0.96 |
| Liver and intrahepatic bile duct | 116 | 30 | 79 | 1.07 | 0.67 | 1.73 |
| Lung | 459 | 157 | 75 | 0.81 | 0.62 | 1.05 |
| Melanoma | 1344 | 263 | 84 | 0.98 | 0.78 | 1.23 |
| Other | 4105 | 832 | 83 | 0.94 | 0.78 | 1.13 |
| Pancreas | 177 | 58 | 75 | 0.78 | 0.54 | 1.12 |
| Prostate | 1085 | 254 | 81 | 0.97 | 0.76 | 1.24 |
| Insurance Status at Diagnosisb | ||||||
| Private insurance | 4043 | 342 | 92 | 1 | Ref | |
| Medicaid | 376 | 12 | 97 | 3.05 | 1.69 | 5.50 |
| Medicare | 2488 | 668 | 79 | 0.46 | 0.38 | 0.55 |
| Medicare and Medicaid, NOS | 590 | 223 | 73 | 0.33 | 0.26 | 0.41 |
| Not insured | 250 | 116 | 68 | 0.21 | 0.16 | 0.27 |
| Other Governmentc | 202 | 296 | 41 | 0.07 | 0.05 | 0.08 |
| Unknown | 1492 | 355 | 81 | 0.55 | 0.39 | 0.75 |
| Vital status | ||||||
| Alive | 7439 | 1393 | 84 | 1 | Ref | |
| Deceased under three months | 709 | 271 | 72 | 0.74 | 0.62 | 0.89 |
| Deceased 4‐11 months | 599 | 196 | 75 | 0.81 | 0.67 | 0.99 |
| Deceased after one year | 694 | 152 | 82 | 1.21 | 0.98 | 1.48 |
| Reporting source | ||||||
| Inpatient or Hospital | 8081 | 1680 | 83 | 1 | Ref | |
| Outpatientd | 1328 | 322 | 80 | 0.79 | 0.57 | 1.09 |
| Death certificate or autopsy only | 32 | 10 | 76 | 0.61 | 0.27 | 1.37 |
| Behavior | ||||||
| 0—Benign | 419 | 89 | 82 | 0.81 | 0.63 | 1.06 |
| 1—Borderline | 39 | 6 | 87 | 1.20 | 0.47 | 3.10 |
| 2—In Situ | 1203 | 220 | 85 | 1.09 | 0.92 | 1.31 |
| 3—Invasive | 7780 | 1697 | 82 | 1 | Ref | |
Odds ratio from a multivariable logistic regression model including all variables in this table.
Primary insurance at time of cancer diagnosis as reported to Utah Cancer Registry.
Veterans Health Administration, TRICARE, and Indian Health Services.
Sources include radiation clinics, pathology laboratories, physician offices, and hospital outpatient.
The number of APCD claim records that each unique patient linked to for the period, including the calendar year of his or her cancer diagnosis and the following year, varied widely (Figure 1). In all age‐groups, the minimum end of the range of number of claims was one. The median number of pharmacy claims was higher for older patients.
Figure 1.
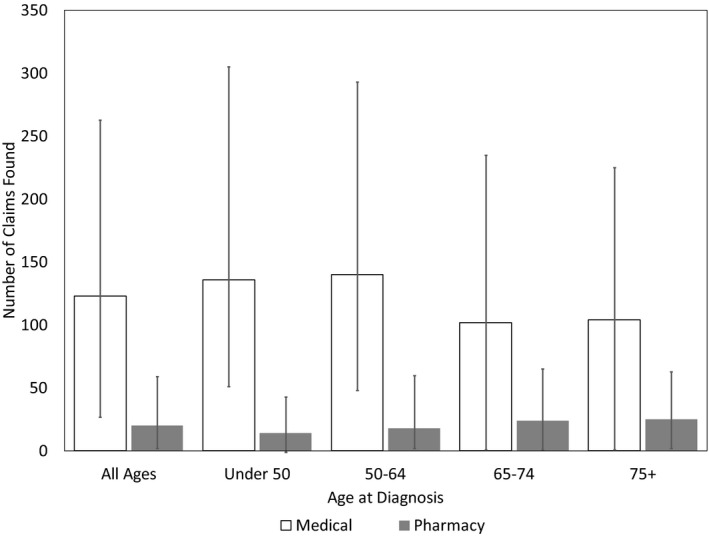
Number of claims Utah All Payers Claims Database claims linked to each Utah Cancer Registry 2013 case by age at diagnosis, median, and interquartile range
4. DISCUSSION
All Payers Claims Databases are increasingly being implemented by states to capture cost data and used to develop a variety of reports using claims data. APCD data represent an important, but underinvestigated, avenue for cancer research. We were able to link a high proportion of the cancer cases in the UCR to patient records in the Utah APCD, particularly for cases younger than 65 years old at diagnosis. The SEER‐Medicare linked database is widely used for research on cancer treatment patterns and outcomes among the population aged 65 years and older,6, 13, 14 but no comparable data resource exists for the population diagnosed with cancer when younger than 65 years of age. The high linkage rate for the under‐65 population in our study indicates that linked state APCD–central cancer registry data will create an opportunity for research on cancer in the under‐65 population.
We found a high proportion of perfect matches on four identifiers, and many partial matches were due to one missing data item and were confirmed as correct linkages. We were able to link many cases even when SSN was missing. This indicates that the quality of identifier data in the Utah APCD is high. Concern about data privacy and security is leading some organizations to examine policies around the use of SSN; we found relatively high linkage success for records with no SSN when name, date of birth, and residence address were known. It was rare that a UCR cancer case linked to more than one APCD patient, evidence that Utah APCD's internal process for deduplication of persons is effective.
Linkage was more successful when age at diagnosis was younger than 65 and for patients with non‐Medicare insurance type and primary site of cancer. The Utah APCD includes claims from commercial insurers, employer self‐funded insurance, and Medicaid. According to Utah Insurance Department information,15 10.3 percent of Utahans are uninsured and 11.2 percent of the population is insured by Medicare. These groups would account for the largest segments of the population whose care would not be included in APCD. Commercial insurers are not required to report if they have fewer than 2500 insured in the state; the exact proportion of Utah residents missed due to this exclusion is not known but is believed to be small. Thus, our overall linkage of just over 82 percent of cancer cases slightly exceeds expectations for the proportion represented in APCD. Further details of the health insurance patterns likely explain the high linkage rate. Some patients who are uninsured before a cancer diagnoses may qualify to enroll in Medicaid after breast or cervical cancer diagnosis16 and so may be included in APCD claims. Among patients enrolled in Medicare, some types of care are still paid by other insurers. This includes Medicare Supplement insurance, Medicare Advantage programs, or care paid through employer insurance plans if the individual is still employed or covered on a spouse's insurance. According to the Kaiser Family Foundation, 20 percent of Medicare enrollees in Utah have Medicare Supplement insurance and 34 percent are covered by Medicare Advantage.17
Electronic health claims datasets represent an excellent resource for improving our understanding or health and health care, although obstacles and limitations exist.18, 19 Cancer registries generate high‐quality cancer incidence and diagnostic information, but lack treatment details, comorbidities, and recurrence. Claims data can potentially fill these cancer data gaps,5, 6, 20 and, as noted above, the linked SEER‐Medicare database has demonstrated the power of linkage of registry data with claims to obtain rich research data for individuals diagnosed with cancer at age 65 and older.14 APCD claims are being accessed for health research in Utah21 and in other states including Oregon,22 Colorado,23 and Massachusetts,24 but to our knowledge this is the first report demonstrating feasibility of linking APCD to a central cancer registry. Demonstrating a high linkage rate of patients is a first step toward using APCD to obtaining additional treatment, comorbidity, and outcome data for cancer research.
4.1. Limitations
This study was conducted using one cancer registry and one state APCD and therefore may not be generalizable in other settings. Our results indicate that certain groups such as the uninsured, veterans, rural populations, and Hispanics will be missed or under‐represented in APCD, limitations that must be recognized for future research using linked APCD–cancer registry data. The value of linkage to APCD may vary depending on cancer registry completeness. For the over‐65 population, the absence of Medicare claims within the APCD will be a significant limitation for research on cancer treatment and outcomes in that age‐group. Although we found that a significant proportion of this age‐group did link to APCD, even among those who did link, any care paid by Medicare would be missed. In Utah, the APCD is working toward incorporating Medicare into APCD to address this limitation.
5. CONCLUSION
Researchers or surveillance organizations using data accrued through electronic linkage may have more confidence in the data if partial matches are manually confirmed. We used LinkPlus linkage scores to efficiently focus manual review on a limited number of cases. APCD data users should be prepared to manage datasets with up to thousands of claims per patient.
All Payers Claims Database datasets are a promising tool for surveillance, having the potential to provide treatment and comorbidity details that are not reliably obtained through normal cancer registry operations. Because data are reported from many payers, each cancer case can potentially be followed in the APCD even when the patient changes his or her health care provider or health insurance. The promise of APCD for improving cancer surveillance, however, can only be realized if claims for the same patient are correctly linked within APCD, if accurate identifiers are present to support linkage to cancer registry data, and if coverage of the population of individuals diagnosed with cancer is adequate. In this study, we have demonstrated that the quality of Utah APCD data for linkage is high and that successful linkage can be carried out based on encrypted SSN. Users of APCD data should be aware of the data limitations for Medicare and uninsured populations. We conclude that the Utah APCD has high‐quality identifier data and that it will be feasible to match to other datasets for surveillance and research purposes.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: Supported by NCI SEER RRSS HHSN261201300017I/HHSN26100008. The Utah Cancer Registry is funded by the National Cancer Institute's SEER Program, Contract No. 75N91018D000016, the US Center for Disease Control and Prevention's National Program of Cancer Registries, Cooperative Agreement No. NU58DP0063200‐01, with additional support from the University of Utah and Huntsman Cancer Foundation. Disclosures: None.
Garvin JH, Herget KA, Hashibe M, et al. Linkage between Utah All Payers Claims Database and Central Cancer Registry. Health Serv Res. 2019;54:707–713. 10.1111/1475-6773.13114
REFERENCES
- 1. Porter J, Love D, Peters A, Sachs J, Costello A. All‐Payer Claims Database Council. The basics of All‐Payer Claims Databases: A primer for states. Robert Wood Johnson Foundation; 2014. https://www.apcdcouncil.org/publication/basics-all-payer-claims-databases-primer-states. Accessed January 11, 2019.
- 2. Rocco P, Kelly AS, Beland D, Kinane M. The New Politics of US Health Care Prices: Institutional reconfiguration and the emergence of all‐payer claims databases. J Health Polit Policy Law. 2017;42(1):5‐52. [DOI] [PubMed] [Google Scholar]
- 3. All‐Payer Claims Database Council . APCD Council Interactive State Report Map. http://www.apcdcouncil.org/state/map. Accessed June 22, 2015.
- 4. Utah Department of Health . The Utah All Payer Database (APD). Utah Health Status Update. Salt Lake City; 2009. health.utah.gov/opha/publications/hsu/09Jul_APD.pdf. Accessed January 11, 2019.
- 5. Lau EC, Mowat FS, Kelsh MA, et al. Use of electronic medical records (EMR) for oncology outcomes research: Assessing the comparability of EMR information to patient registry and health claims data. Clin Epidemiol. 2011;3:259‐272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Noone A‐M, Lund JL, Mariotto A, et al. Comparison of SEER treatment data with Medicare claims. Med Care. 2014;54(9):e55‐e64. 10.1097/MLR.0000000000000073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Office of Health Care Statistics . Utah All Payer Claims Database 2013‐2014 Claims Centric Limited Data Set (CcLDS): User Manual; 2015. http://stats.health.utah.gov/wp-content/uploads/2018/08/APCD_ClaimsCentric_Limited_Use_Datamart_User_Manual_20180814.pdf. Accessed January 11, 2019.
- 8. Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: A national resource. Cancer Epidemiol Biomarkers Prev. 1999;8(12):1117‐1121. [PubMed] [Google Scholar]
- 9. Thornton M, ed. Standards for Cancer Registries, Volume II, Data Standards and Data Dictionary. Twenty First Edition, Record Layout Version 18. North American Association of Central Cancer Registries (NAACCR); 2018. http://datadictionary.naaccr.org/. Accessed January 11, 2019.
- 10. Meux E. Encrypting personal identifiers. Health Serv Res. 1994;29(2):247‐256. [PMC free article] [PubMed] [Google Scholar]
- 11. National Program of Cancer Registries . Registry Plus™ Link Plus Features and Future Plans. Atlanta, GA: Centers for Disease Control and Prevention; 2018. https://www.cdc.gov/cancer/npcr/tools/registryplus/lp_features.htm. Accessed January 11, 2019. [Google Scholar]
- 12. Campbell KM, Deck D, Krupski A. Record linkage software in the public domain: A comparison of Link Plus, The Link King, and a ‘basic’ deterministic algorithm. Health Informat J. 2008;14(1):5‐15. [DOI] [PubMed] [Google Scholar]
- 13. Warren JL, Mariotto A, Melbert D, et al. Sensitivity of Medicare claims to identify cancer recurrence in elderly colorectal and breast cancer patients. Med Care. 2016;54(8):e47‐e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER‐Medicare data: Content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(8 Suppl.):IV‐3‐18. [DOI] [PubMed] [Google Scholar]
- 15. State of Utah Insurance Department . 2015 Health Insurance Market Report; 2015. https://insurance.utah.gov/wp-content/uploads/2015HealthMarketReport.pdf. Accessed January 11, 2019.
- 16. Lee NC, Wong FL, Jamison PM, et al. Implementation of the National Breast and cervical cancer early detection program: The beginning. Cancer. 2014;120(Suppl. 16):2540‐2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kaiser Family Foundation . Kaiser Family Foundation Analysis of Centers for Medicare and Medicaid Services Medicare Current Beneficiary Survey; 2018.
- 18. Mues KE, Liede A, Liu J, et al. Use of the Medicare database in epidemiologic and health services research: A valuable source of real‐world evidence on the older and disabled populations in the US. Clin Epidemiol. 2017;9:267‐277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Newman D, Herrera CN, Parente ST. Overcoming barriers to a research‐ready national commercial claims database. Am J Manag Care. 2014;20(11 Spec No. 17):eSP25‐30. [PubMed] [Google Scholar]
- 20. Lipscomb J, Gillespie TW. State‐level cancer quality assessment and research: building and sustaining the data infrastructure. Cancer J. 2011;17(4):246‐256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Scammon DL, Tomoaia‐Cotisel A, Day RL, et al. Connecting the dots and merging meaning: using mixed methods to study primary care delivery transformation. Health Serv Res. 2013;48(6 Pt 2):2181‐2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sun BC, Chi DL, Schwarz E, et al. Emergency department visits for nontraumatic dental problems: A mixed‐methods study. Am J Public Health. 2015;105(5):947‐955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bartels K, Fernandez‐Bustamante A, McWilliams SK, Hopfer CJ, Mikulich‐Gilbertson SK. Long‐term opioid use after in patient surgery – a retrospective cohort study. Drug Alcohol Depend. 2018;187:61‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Figueroa JF, Frakt AB, Lyon ZM, Zhou X, Jha AK. Characteristics and spending patterns of high cost, non‐elderly adults in Massachusetts. Healthcare. 2017;5(4):165‐170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


