Abstract
Objective
To determine whether women treated by older physicians are more likely to undergo episiotomy.
Data Sources/Study Setting
Hospital discharge data from Pennsylvania for the period 1994 to 2010.
Study Design
We examined the impact of the year in which physicians started delivering babies (a proxy for age) in Pennsylvania on episiotomy rates using a linear probability model with hospital fixed effects.
Data Collection/Extraction Methods
Using diagnosis and procedure codes, we identified women delivering vaginally (N = 1 658 327) and determined the proportion who had an episiotomy.
Principal Findings
The average physician‐level episiotomy rate declined from 54 percent in 1994 to 13 percent in 2010. Rates declined among older and younger physicians, but, at any point in time, women treated by older physicians were more likely to have an episiotomy. A 10‐year difference in physician age is associated with a 6 percentage point increase in episiotomy rates.
Conclusions
Results indicate that older physicians, who entered practice when episiotomy was common, were slow to adjust their practices in response to evidence showing that routine episiotomy is unnecessary.
Keywords: abandonment, childbirth, de‐adoption, obstetric delivery, physicians' practice patterns
1. INTRODUCTION
Episiotomy is a surgical procedure to enlarge the vaginal opening during childbirth. Seven randomized trials published between 1984 and 2004 have found that routine use of episiotomy does not benefit mothers or babies.1 Even though all but one of the trials was published before 1995, episiotomy rates declined slowly during the 1990s and 2000s.2, 3 One explanation is that older physicians, who trained in an era where most women received episiotomies, were slower to adjust their practice patterns in response to the new evidence. Many studies in the medical literature find that older physicians are less likely to adhere to and be aware of current evidenced‐based standards of care.4 It is unclear if differences in stated beliefs translate into differences in how patients are treated and how older and younger physicians differ in their responses to new evidence.
Prior studies have examined how various aspects of physicians' training influence their treatment choices. Of particular relevance to our study, Dranove, Ramanarayanan, and Sfekas5 find that obstetricians' Cesarean delivery rates are influenced by the rates in the hospitals in which they did their residency, but Epstein and Nicholson6 find that training and peer effects explain only a small share of physician‐level variation in Cesarean delivery rates. Janakiraman et al7 show that older physicians are more likely to exhibit persistence in prescribing patterns.
In this paper, we compare trends in the use of episiotomy between older and younger physicians. An episiotomy is a surgical procedure performed during a vaginal delivery. The obstetrician makes an incision beginning at the lower end of the vagina directly toward the anus or at a 45° angle. The incision enlarges the vaginal opening. In rare cases, episiotomy can prevent serious fetal complications or death (eg, if the fetal shoulder gets caught on the pelvic bone).
Since 1984, a number of randomized trials have tested “routine” or “liberal” use of episiotomy against “restrictive” use. Under a routine use policy, obstetricians perform episiotomy to prevent natural perineal tears. Under a restrictive use policy, obstetricians perform episiotomy only if it is necessary to prevent severe maternal and fetal complications. In 2005, the Journal of the American Medical Association published a systematic review of seven trials conducted between 1984 and 2004.1 Episiotomy rates in patients randomized to the routine arm varied between 45 and 83 percent. Rates in patients randomized to the restrictive arm varied between 7.6 and 53 percent. Women randomized to routine episiotomy did not experience lower rates of pain or incontinence. If anything, the trial results suggest that routine use of episiotomy increases the risk of severe lacerations and pain. The review concluded “Our systematic review finds no benefits from [routine] episiotomy.” A review conducted in 20078 reached similar conclusions to the 2005 review: “Restrictive episiotomy policies appear to have a number of benefits compared to routine episiotomy policies.”
There are few external factors that would prevent physicians from reducing their use of episiotomy. Financial incentives are minimal. Following Current Procedural Terminology coding conventions, insurers bundle the payment for episiotomy with the payment for vaginal delivery. The procedure does not require any supplies other than a scalpel and sutures. The incision and postdelivery suturing take about 10 minutes. Episiotomy does not define the specialty of obstetrics in the same way that revascularization procedures define interventional cardiology or administration of chemotherapy defines oncology. Obstetricians who abstain from routine episiotomy do not damage their professional standing. Obstetricians could be sued for failing to perform an episiotomy when an infant experiences adverse outcomes following a prolonged delivery, but they could also be sued for performing an episiotomy if a mother experiences a severe complication.
Our study contributes to the growing literature on the abandonment (or de‐adoption) of ineffective medical technologies.9, 10, 11, 12, 13, 14, 15, 16 Understanding the factors that contribute to physician‐level variation and promote or retard the abandonment of ineffective treatments is important for designing interventions to better align evidence and practice.
Using 100 percent samples of deliveries from Pennsylvania for the period 1994 to 2010, we test whether women treated by older physicians were more likely to undergo episiotomy compared to women treated by younger physicians.
2. STUDY DATA AND METHODS
2.1. Conceptual framework
Baron17 defines “belief persistence” (also known as “cognitive inertia”) as “the tendency to search for evidence, and to use evidence, in a way that supports beliefs that are already strong for us (prior beliefs) or beliefs that we want to be true” and notes that “The irrational persistence of beliefs is one of the major sources of human folly….”
In one of the first studies to document belief persistence empirically, Bruner and Potter18 showed subjects blurred images and asked them to state beliefs about the content of the images as they slowly came into focus. Subjects who initially viewed blurrier images and subjects for whom the images stayed blurrier for longer periods were slower to provide correct descriptions, a result the researchers attributed to the reluctance of subjects to abandon their initial hypotheses.
Suppose that beliefs about the effectiveness of episiotomy in year t among physicians who entered practice in year j, , can be expressed as a weighted sum of the best available evidence in year t, b t, and the evidence and beliefs that prevailed when they entered practice in year j: . The variables b t and b j are analogous to current and historical prices in research on inertia in consumer choice.19
The parameter θ describes the weight that physicians give to current evidence and beliefs vs the evidence and beliefs that prevailed when they entered practice. If θ < 1, physicians' decisions are subject to belief persistence. While we cannot estimate θ directly, we can infer it from observed treatment patterns.
2.2. Data and sample construction
We measured episiotomy rates using Pennsylvania Inpatient Hospital Discharge Data for the period 1994 to 2010. Hospitals in Pennsylvania are required to report these data to the Pennsylvania Health Care Cost Containment Council. The data are a census of hospital discharges in the state and include variables typically found in hospital billing records. They record patient age, race, insurance type, and International Classification of Diseases, Ninth Revision (ICD‐9) diagnosis and procedure codes. Observations are at the level of the patient admission. A key feature of our data is that they include physician identifiers that can be linked across years, permitting us to measure physician‐level trends in the use of episiotomy. The ICD‐9 codes we used to identify procedures and conditions are listed in Table S1.*
We identified the year of each physician's first and last delivery in the data. The data do not indicate if physicians practiced in other states prior to making their appearance in the Pennsylvania data. Nationally, about 1.7 percent of physicians move between states each year.20 This figure probably overstates the movement of experienced obstetricians into Pennsylvania. Migration rates among specialists are lower, Pennsylvania experienced a net outmigration of physicians between 2006 and 2011, and physician migration is often motivated by changes in practice specialty. When physicians do move, it is often early in their careers, so their beliefs in the first year in which they appear in our data are probably close to their beliefs in their first year of practice.
We included deliveries by physicians who performed an average of 10 or more deliveries per quarter between their entry and exit dates. There were 2 358 789 deliveries by physicians who met the volume‐based inclusion criteria between 1994 and 2010 (out of 2 472 590, including Cesarean deliveries). Our main analysis focuses on the 1 658 327 spontaneous vaginal deliveries.
2.3. Statistical analysis
We estimated the impact of obstetricians' entry year on the likelihood that a patient receives an episiotomy. The delivery is the unit of observation. Physician‐level random effects adjust standard errors for clustering (entry year is constant across physicians, so we cannot include fixed effects). Given the size of the sample and the need to include random effects, we used a linear probability model to facilitate estimation. Physician entry year is the main independent variable of interest.
We controlled for physicians' quarterly Cesarean delivery rate to adjust for substitution effects between episiotomy and Cesarean delivery and hospital‐level quarterly episiotomy rates to capture external factors common to physicians within a hospital that influence episiotomy rates. Patient‐level controls included age, race, insurance type, indicators for a previous Cesarean delivery, macrosomia (a large fetus), and uterine scarring (scar tissue can impede delivery), operative delivery, and an indicator for whether the patient resides in a metropolitan county (based on rural‐urban continuum codes21). The model included fixed effects for hospitals that performed more than 20 000 deliveries over the study period. These hospitals account for 74 percent of all deliveries. Smaller hospitals were grouped together as the omitted category. We estimate the model on various subsamples of the data, as described below.
We also estimated three models that examine the impact of physician entry year on induced delivery, operative delivery, and Cesarean delivery. These models are falsification tests. If older physicians tend to perform more high risk deliveries, then women treated by older physicians should also have higher rates of these procedures.
3. RESULTS
3.1. Sample characteristics
The sample contains 1 658 327 spontaneous vaginal deliveries (out of 2 358 789 total deliveries). Of these, 102 895 (6 percent) were operative deliveries. There are 2200 unique physicians who met our minimum volume criteria, including 1076 who were practicing in 1994 and 1035 who were practicing in 2010. There are 401 physicians who were in practice for the entire duration of the study period. Physicians' average annual volume is 90 total deliveries (median 73) and 64 vaginal deliveries (median 51).
The episiotomy rate declined from 54 percent in 1994 to 13 percent in 2010. Among nonoperative deliveries, the rate declined from 50 to 12 percent. Among operative deliveries, the rate declined from 84 to 43 percent.
Table 1 displays means for the variables we included in the regression. Table S2 presents summary statistics for additional patient risk factors. Figure 1 shows trends in the average and interquartile range of physician‐level episiotomy rates.2 The graph includes labels for important events: the publication of two trials,22, 23 the publication of the systematic review in the Journal of the American Medical Association,1 and the release of an American College of Obstetrics and Gynecology's Practice Bulletin on episiotomy24—that may have influenced obstetricians' use of episiotomy.
Table 1.
Physician, hospital, and patient characteristics
| All | By physician entry year | |||||
|---|---|---|---|---|---|---|
| 1994 | 1995‐1998 | 1999‐2002 | 2003‐2006 | 2007‐2010 | ||
| Episiotomy rate | 0.308 | 0.378 | 0.229 | 0.170 | 0.105 | 0.079 |
| Spontaneous only | 0.283 | 0.348 | 0.211 | 0.161 | 0.100 | 0.075 |
| Operative only | 0.694 | 0.749 | 0.551 | 0.435 | 0.328 | 0.308 |
| Physician‐level Cesarean delivery rate | 0.238 | 0.228 | 0.233 | 0.268 | 0.286 | 0.286 |
| Hospital‐level episiotomy rate | 0.269 | 0.316 | 0.228 | 0.174 | 0.111 | 0.087 |
| Patient age | 27.5 | 27.7 | 27.2 | 27.4 | 26.9 | 26.8 |
| Patient asian | 0.018 | 0.015 | 0.020 | 0.022 | 0.029 | 0.027 |
| Patient black | 0.133 | 0.116 | 0.144 | 0.147 | 0.219 | 0.233 |
| Patient white | 0.720 | 0.749 | 0.674 | 0.700 | 0.616 | 0.583 |
| Patient other race | 0.129 | 0.119 | 0.162 | 0.131 | 0.137 | 0.157 |
| Patient uninsured | 0.016 | 0.016 | 0.016 | 0.016 | 0.013 | 0.014 |
| Patient Medicaid | 0.312 | 0.274 | 0.347 | 0.362 | 0.465 | 0.497 |
| Patient private | 0.617 | 0.643 | 0.593 | 0.600 | 0.499 | 0.464 |
| Patient other insurance | 0.055 | 0.067 | 0.045 | 0.022 | 0.023 | 0.025 |
| Patient prior Cesarean delivery | 0.039 | 0.043 | 0.037 | 0.028 | 0.026 | 0.028 |
| Macrosomia | 0.016 | 0.018 | 0.015 | 0.013 | 0.011 | 0.011 |
| Uterine scarring | 0.0004 | 0.0003 | 0.0005 | 0.0003 | 0.0007 | 0.0004 |
| Operative delivery | 0.062 | 0.075 | 0.051 | 0.032 | 0.020 | 0.017 |
| Metro county | 0.898 | 0.894 | 0.921 | 0.874 | 0.915 | 0.912 |
| Teaching hospital | 0.314 | 0.300 | 0.284 | 0.358 | 0.384 | 0.525 |
| N (1000s) | 1658 | 1073 | 275 | 170 | 101 | 40 |
Note: The sample is restricted to vaginal deliveries.
Figure 1.
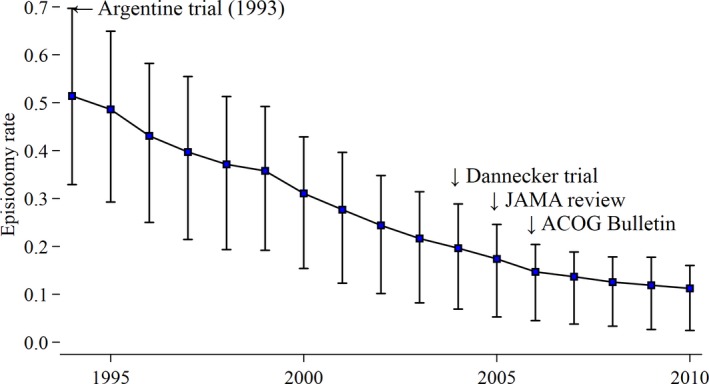
Average and interquartile range of physician‐level episiotomy rates for routine vaginal deliveries. The trendline depicts average physician‐level episiotomy rates. Bars represent the 25th and 75th percentiles of physician‐level rates [Color figure can be viewed at wileyonlinelibrary.com]
Physician‐level episiotomy rates vary widely at any point in time. In 1994, the 25th and 75th percentiles of physician‐level episiotomy rates were 33 percent and 69 percent. The variation is substantially greater than what would be expected based on chance alone.† In 2010, the corresponding percentiles were 2 and 16 percent.
Figure 2 displays trends in episiotomy rates by obstetricians' year of entry cohort. Rates are calculated across patients, not physicians.‡ We combined cohorts into multiyear groups to reduce visual clutter and start measuring trends once all members of the cohort have entered (so the trendline for physicians who entered between 1995 and 1998 starts in 1998). The trends depicted in the graph represent the main finding of the paper. Older obstetricians reduced their use of episiotomy, but, in any given year, older obstetricians were substantially more likely to use episiotomy compared to obstetricians who were new to practice. For example, episiotomy rates among women treated by obstetricians who entered practice in 1994 or earlier were 54 percent in 1994, 32 percent in 2002, and 17 percent in 2010. Rates among physicians who entered practice between 1999 and 2002 were 20 percent in 2002 and 12 percent in 2010.
Figure 2.
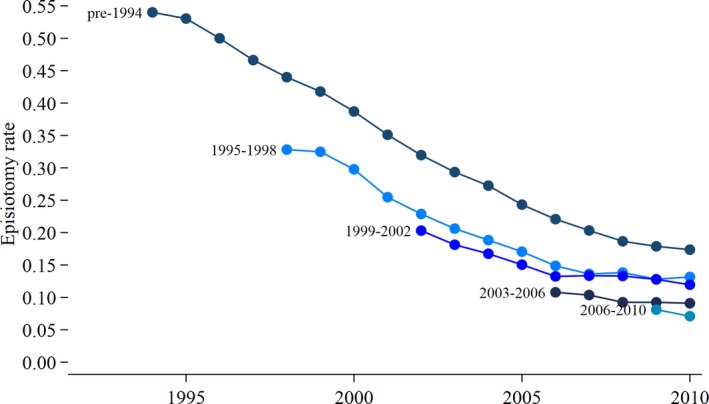
Episiotomy rates by obstetricians' year of entry. Trendlines show the episiotomy rate among patients grouped by the year in which their physician entered practice [Color figure can be viewed at wileyonlinelibrary.com]
Differences are apparent at all points in the distribution of physician‐level rates. For example, the 25th and 75th percentiles of physician‐level rates in 2002 among physicians who entered practice in 1994 are higher than the corresponding percentiles among physicians who entered between 1999 and 2002. The data used to construct the figure include deliveries by obstetricians who exited practice before 2010. The trends look similar if we restrict the sample to deliveries by obstetricians who were still practicing in 2010 (see Figure S1).
For the sake of comparison, we also evaluated differences in Cesarean delivery rates (see Figure S2). In the entire sample, Cesarean delivery rates increased from 20 percent to 32 percent. Differences between physician cohorts are relatively small. For example, in 2002 the Cesarean delivery rate among patients treated by physicians who entered practice in or before 1994 was 26 percent and the rate among patients treated by physicians who entered between 1999 and 2002 was 24 percent. At the physician level, episiotomy rates and Cesarean delivery rates are weakly positively correlated; correlation coefficients calculated annually range from 0.12 percent to 0.23.
3.2. Regression results
Table 2 displays results from the regression model. Hospital fixed effects are not shown. The model indicates that the likelihood that a woman receives an episiotomy is just over one half of a percentage point lower if her obstetrician entered practice in year t vs year t−1. Put another way, there is a 6 percentage point difference in episiotomy rates between obstetricians who entered practice a decade apart.
Table 2.
Results from a linear probability model where the outcome is the receipt of an episiotomy
| Variable | B (SE) |
|---|---|
| Entry year | −0.006 (0.0005)* |
| Quarterly time trend | −0.003 (0.0000)* |
| Physician‐level Cesarean delivery rate | 0.061 (0.0038)* |
| Hospital episiotomy rate | 0.260 (0.0020)* |
| Patient age | −0.005 (0.0001)* |
| Patient asian | 0.044 (0.0025)* |
| Patient black | −0.085 (0.0013)* |
| Patient white | 0.017 (0.0009)* |
| Patient uninsured | −0.066 (0.0029)* |
| Patient Medicaid | −0.056 (0.0014)* |
| Patient private | 0.025 (0.0007)* |
| Patient prior Cesarean delivery | 0.039 (0.0016)* |
| Macrosomia | 0.070 (0.0025)* |
| Uterine scarring | 0.186 (0.0158)* |
| Operative delivery | 0.303 (0.0013)* |
| Metro county | −0.003 (0.0017) |
| Interclass correlation coefficient | 0.08 |
| N | 1 658 327 |
Note: Hospital fixed effects not shown. A coefficient of 0.005 corresponds to a marginal effect of 0.5 percentage points.
Significant at the 1% level.
The coefficient on physicians' Cesarean delivery rate indicates there is a positive association between physicians' use of episiotomy and Cesarean delivery. The coefficient on the hospital episiotomy rate indicates that a woman is more likely to receive an episiotomy if the other physicians at the hospital where she delivers (excluding her own physician) use episiotomy more frequently.
Figure 3 displays point estimates and the 95 percent confidence intervals of the coefficients on entry year from the baseline model and alternative specifications. Note that coefficients are presented as percentage point changes. Full results are presented in Table S2.
Figure 3.
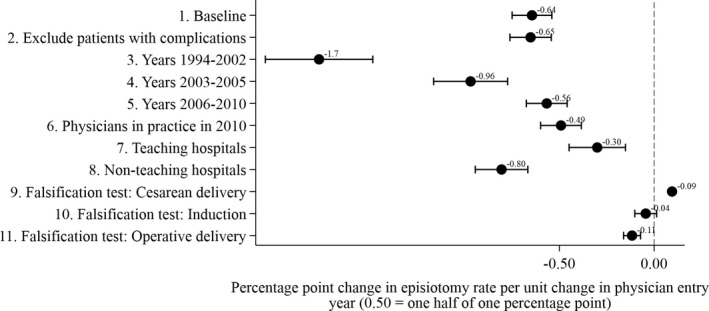
Estimates of the impact of entry year on episiotomy rates from alternative specifications. The dots represent point estimates of the impact of physician entry year on episiotomy rates from linear probability models. Error bars represent 95 percent confidence intervals
Model 2 is the same as the baseline model, but we exclude patients who experienced complications, including having an operative delivery or who had a prior Cesarean delivery.
Models 3‐5 were estimated on various subsamples defined by year. The coefficient on physician entry year is smaller when the sample is restricted to women who delivered between 2003 and 2005 vs 1994 and 2002. Similarly, the coefficient is smaller when the sample is restricted to women who delivered between 2006 and 2010 vs 2003 and 2005.
Model 6 was estimated on the sample of women treated by physicians who were still practicing in 2010.
Models 7 and 8 restrict samples to deliveries performed in teaching and nonteaching hospitals. The results indicate that older obstetricians in teaching hospitals are more likely to use episiotomy than younger obstetricians, but the magnitude of the cohort effect is much smaller than in nonteaching hospitals (0.3 percentage points vs 0.8 percentage points). These results are consistent with the idea that teaching hospitals foster a culture of evidenced‐based medical practice and attract physicians who are open to changing their beliefs. Overall, episiotomy rates are lower in teaching hospitals (21 percent vs 27 percent for nonteaching hospitals). By comparison, the Cesarean delivery rate is 25 percent in nonteaching hospitals and 26 percent in teaching hospitals.
Models 9‐11 show the impact of physician entry year on induced delivery, operative delivery, and Cesarean delivery. The model for Cesarean delivery was estimated using all 2 358 789 deliveries in the sample. The models for induced and operative delivery were estimated on the sample of vaginal deliveries, similar to the baseline model. In all cases, the coefficients, though significant for two of the procedures, are close to “0.”
4. DISCUSSION
Both older and younger physicians reduced their use of episiotomy as evidence on the lack of benefit from episiotomy accumulated. However, at any point in time, women treated by older physicians were significantly more likely to have an episiotomy. There are many possible explanations, but the results are consistent with the theory that older physicians are slow to update beliefs and practice patterns in response to new evidence. The gradual accumulation of evidence on the effectiveness of episiotomy provides a source of exogenous variation in the beliefs physicians were exposed to when they entered medical practice. Physicians did not have to invest in any specialized equipment or training to respond to new evidence. There are no switching costs or technological lock‐in effects that prevent obstetricians from adjusting their use of the procedure. Guidelines recommending against use of routine episiotomy simply ask physicians to engage in a practice—delivering a baby without episiotomy—that most have performed hundreds if not thousands of times over the course of their careers. While we cannot observe beliefs directly, there is a close correspondence between obstetricians' beliefs about the effectiveness of episiotomy and their use of episiotomy.25 The case of episiotomy illustrates a root cause of variation in physician practice patterns and the sometimes slow translation of evidence into practice: a reluctance among physicians to let go of the beliefs that prevailed when they entered practice.
As shown in models 3 to 5, the impact of physician entry year on episiotomy rate is smaller in more recent periods. Mounting evidence that routine episiotomy is unnecessary may have led to a narrowing of differences in beliefs between older and younger physicians. This result is consistent with the idea that evidence narrows practice variation. However, this result must be interpreted cautiously because episiotomy rates are bounded from below. Differences may shrink naturally as rates trend toward “0.”
We compared the episiotomy rates we estimated in Pennsylvania to previously published estimates from other geographic areas to assess generalizability. Compared to rates calculated using the National Hospital Discharge Survey, the episiotomy rate for nonoperative deliveries in Pennsylvania was 20 percentage points higher in 1994 but similar in 2004 (the last year for which data are available).2 Over the period 2003 to 2008, episiotomy rates in Pennsylvania were similar to the rates calculated using hospital discharge data from nine large states, not including Pennsylvania,3 and a multihospital database,26 and declined by a similar amount.
Our results may be biased by unobserved differences in patient risk factors between older and younger physicians. The temporality of the patient‐physician assignment process mitigates against selection effects. Most women choose an obstetrician long before the second trimester ultrasound, when it is possible to predict fetal head circumference with some degree of certainty. The uncertain timing of childbirth introduces an additional element of randomness into the assignment process. Women select an obstetrical practice, but, in the 85 percent of cases when delivery is spontaneous, the delivery is performed by the obstetrician within the practice who happens to be on call when the woman presents at the hospital. A physician may request assistance from a colleague during a difficult delivery, but only the original physician bills for the procedure. Referral of a difficult case occurs rarely if at all.
If older physicians are more likely to use episiotomy because they treat more high risk cases, they should also be more likely to use other procedures for high risk cases. However, we find that differences between older and younger physicians in the use of Cesarean delivery, induction, and operative delivery are small. Though there is a general sense that some of these procedures are overused, these procedures, unlikely episiotomy, have not been evaluated in major randomized trials. These results, combined with the minimal differences in patient risk factors across cohorts (Table S1), suggest that differences in episiotomy rates between older and younger physicians are not due to differences in patient risk factors.
Cesarean delivery rates have increased over time (from 20 to 32 percent), which could affect trends in episiotomy rates if Cesarean deliveries are now performed on women who would have been good candidates for episiotomy in the past. However, in our data, episiotomy rates and Cesarean delivery rates at the physician level are positively correlated. The results are consistent with Klein et al,25 who find that “…physicians who use episiotomy frequently and routinely often do so as part of an interventionist pattern or style of practice.”
The degree of physicians' belief persistence has implications for policies related to technology adoption and physician certification. Many costly medical treatments diffuse rapidly into routine clinical practice without having been previously evaluated in a randomized controlled trial. If physicians adjust their beliefs in response to new evidence, there is little risk that permitting early adoption of a treatment will lead to widespread overuse if the treatment is later found to be ineffective. However, if practice patterns are subject to belief persistence, physicians may be slow to abandon outdated practices. Once diffused, technologies will remain entrenched.27, 28 The greater the degree of belief persistence, the greater should be the barriers to adoption of untested therapies.
Based on research showing that older physicians are less likely to adhere to current evidenced‐based standards of care,4 many medical specialty societies have started requiring physicians to recertify every 10 years. Since 2011, the Medicare program has paid bonuses to physicians who pass these “maintenance of certification” exams. Many physicians resent the time and cost of the exams. The controversy over maintenance of certification is only part of a larger debate about how to ensure the cognitive and clinical competency of older physicians.29 Belief persistence poses an obstacle to the translation of evidence into practice and provides a justification for polices, such as maintenance of certification, that provide older physicians with an opportunity to identify mismatches between their practice patterns and current evidence.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: The authors are employed by Emory University.
Howard DH, Hockenberry J. Physician age and the abandonment of episiotomy. Health Serv Res. 2019;54:650‐657. 10.1111/1475-6773.13132
ENDNOTES
We are unaware of studies that have examined the sensitivity and specificity of claims data for measuring the receipt of an episiotomy. However, a physician would be considered delinquent if he consistently failed to record episiotomy in the medical record. Using the medical record, hospital billing staff code the procedure in the data. Hospital fixed effects in our empirical analysis adjust for any differences in coding practices across hospitals.
Using Monte Carlo simulation, we estimated that if all patients had the same underlying probability of undergoing an episiotomy in 1994 (40.6 percent), the interquartile range of physician‐level rates would have been 7 percent percentage points, only one‐fifth of the observed interquartile range of 33 percentage points.
The average rate across physicians closely tracks the average across all deliveries.
REFERENCES
- 1. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr K. Outcomes of routine episiotomy: a systematic review. JAMA. 2005;293:2141‐2148. [DOI] [PubMed] [Google Scholar]
- 2. Frankman E, Wang L, Bunker C, Lowder J. Episiotomy in the United States: has anything changed? Am J Obstet Gynecol. 2009;200:571‐577. [DOI] [PubMed] [Google Scholar]
- 3. Shen YC, Caughey A, Chung W, Howard DH. Can major systematic reviews influence practice patterns? A case study of episiotomy trends. Arch Gynecol Obstet. 2013;288:1285‐1293. [DOI] [PubMed] [Google Scholar]
- 4. Choudhry N, Fletcher R, Soumerai S. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142:260‐273. [DOI] [PubMed] [Google Scholar]
- 5. Dranove D, Ramanarayanan S, Sfekas A. Does the market punish aggressive experts? Evidence from Cesarean sections. B E J Econom Anal Policy. 2011;11(2):650‐33. [Google Scholar]
- 6. Epstein AJ, Nicholson S. The formation and evolution of physician treatment styles: an application to Cesarean sections. J Health Econ. 2009;28:1126‐1140. [DOI] [PubMed] [Google Scholar]
- 7. Janakiraman R, Dutta S, Sismeiro C, Stern P. Physicians' persistence and its implications for their response to promotion of prescription drugs. Manage Sci. 2008;54(6):1080‐1093. [Google Scholar]
- 8. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;21:CD000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Howard DH, Roback JD, Murphy DJ. Trends in transfusion rates after the FOCUS trial. J Comp Eff Res. 2018;7:113‐120. [DOI] [PubMed] [Google Scholar]
- 10. Howard DH, David G, Hockenberry J. Selective hearing: physician‐ownership and physicians' response to new evidence. J Econ Manag Strategy. 2017;26:152‐168. [Google Scholar]
- 11. Howard DH, Soulos PR, Chagpar AB, Mougalian S, Killelea B, Gross CP. Contrary to conventional wisdom, physicians abandoned a breast cancer treatment after a trial concluded it was ineffective. Health Aff. 2016;35:1309‐1315. [DOI] [PubMed] [Google Scholar]
- 12. Smieliauskas F, Lam S, Howard DH. Impact of negative clinical trial results for vertebroplasty on vertebral augmentation procedure rates. J Am Coll Surg. 2014;219:525‐533. [DOI] [PubMed] [Google Scholar]
- 13. Howard DH, Shen YC. Trends in PCI volume after negative results from the COURAGE trial. Health Serv Res. 2014;49:153‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Niven DJ, Rubenfeld GD, Kramer AA, Stelfox HT. Effect of published scientific evidence on glycemic control in adult intensive care units. JAMA Intern Med. 2015;175(5):801‐809. [DOI] [PubMed] [Google Scholar]
- 15. Deyell MW, Buller CE, Miller LH, et al. Impact of National Clinical Guideline recommendations for revascularization of persistently occluded infarct‐related arteries on clinical practice in the United States. Arch Intern Med. 2011;171:1636‐1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Duffy SQ, Farley DE. The protracted demise of medical technology. The case of intermittent positive pressure breathing. Med Care. 1992;30:718‐736. [DOI] [PubMed] [Google Scholar]
- 17. Baron J. Thinking and Deciding. Cambridge, UK: Cambridge University Press; 2008:203. [Google Scholar]
- 18. Bruner J, Potter M. Interference in visual recognition. Science. 1964;144:424‐425. [DOI] [PubMed] [Google Scholar]
- 19. Dubé JP, Hitsch GJ, Rossi P. State dependence and alternative explanations for consumer inertia. RAND J Econ. 2010;41:417‐445. [Google Scholar]
- 20. Ricketts T. The migration of physicians and the local supply of practitioners: a five‐year comparison. Acad Med. 2013;88:1913‐1918. [DOI] [PubMed] [Google Scholar]
- 21. United States Department of Agriculture . Rural‐Urban Continuum Codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed October 12, 2016.
- 22. Argentine Episiotomy Trial Collaborative Group . Routine vs selective episiotomy: a randomized controlled trial. Lancet. 1993;342:1517‐1518. [PubMed] [Google Scholar]
- 23. Dannecker C, Hillemanns P, Strauss A, Hasbargen U, Hepp H, Anthuber C. Episiotomy and perineal tears presumed to be imminent: randomized controlled trial. Acta Obstet Gynecol Scand. 2004;83:364‐368. [DOI] [PubMed] [Google Scholar]
- 24. American Congress of Obstetricians and Gynecologists . ACOG practice bulletin. Episiotomy. Clinical management guidelines for obstetrician‐gynecologists. Obstet Gynecol. 2006;107:957‐1962. [PubMed] [Google Scholar]
- 25. Klein MC, Kaczorowski J, Robbins JM, Gauthier RJ, Jorgensen SH, Joshi AK. Physicians' beliefs and behavior during a randomized controlled trial of episiotomy: consequences for women in their care. CMAJ. 1995;153:769‐779. [PMC free article] [PubMed] [Google Scholar]
- 26. Friedman AM, Ananth CV, Prendergast E, D'Alton ME, Wright JD. Variation in and factors associated with use of episiotomy. JAMA. 2015;313:197‐199. [DOI] [PubMed] [Google Scholar]
- 27. Phelps CE. Diffusion of information in medical care. J Econ Perspect. 1992;6:23‐42. [DOI] [PubMed] [Google Scholar]
- 28. Redberg RF. Evidence, appropriateness, and technology assessment in cardiology: a case study of computed tomography. Health Aff. 2007;26:86‐95. [DOI] [PubMed] [Google Scholar]
- 29. Kupfer J. The graying of US physicians. JAMA. 2016;315:341‐342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


