Abstract
Within the Veterans Health Administration (VHA), the largest integrated health care system in the US, approximately 8.5 million Veteran patients receive informal care. Despite a need for training, half of VHA caregivers report that they have not received training that they deemed necessary. Rigorous study is needed to identify effective ways of providing caregivers with the skills they need. This paper describes the Helping Invested Families Improve Veterans’ Experience Study (HI-FIVES), an ongoing randomized controlled trial that is evaluating a skills training program designed to support caregivers of cognitively and/or functionally impaired, community-dwelling Veterans who have been referred to receive additional formal home care services. This two-arm randomized controlled trial will enroll a total of 240 caregiver–patient dyads. For caregivers in the HI-FIVES group, weekly individual phone training occurs for 3 weeks, followed by 4 weekly group training sessions, and two additional individual phone training calls. Caregivers in usual care receive information about the VA Caregiver Support Services Program services, including a hotline number. The primary outcome is the number of days a Veteran patient spends at home in the 12 months following randomization (e.g. not in the emergency department, inpatient or nursing home setting). Secondary outcomes include patient VHA health care costs, patient and caregiver satisfaction with VHA health care, and caregiver depressive symptoms. Outcomes from HI-FIVES have the potential to improve our knowledge of how to maximize the ability to maintain patients safely at home for caregivers while preventing poor mental health outcomes among caregivers.
Keywords: Informal care, Skills training, Randomized control trial, Days at home, Health care costs, Depressive symptoms
1. Introduction
Providing unpaid care for a family member or friend in the home, or informal care, is the most common form of long-term care (LTC) in the U.S. Within the Veterans Health Administration (VHA), approximately 8.5 million Veterans receive informal care [1]. Informal care provides a large benefit to society by allowing adults with cognitive or functional impairments to remain in their preferred setting—the home—and by substituting for costly care such as that provided in nursing homes [2–4]. Informal care also facilitates the aims of the 1999 Millennium Act, which expanded LTC coverage for Veterans and stipulated that Veterans receive care in the least restrictive setting possible—their homes. And yet, there can be unintended negative consequences for the caregivers, including caregiver strain, burden, burnout and depression, which can increase patients’ risk of institution-alization [5–8].
Caregivers need clinical, psychological and support seeking skills to effectively navigate their role as a caregiver (Fig. 1), which could be attained through skills training. Despite expressing a need for training, half of VHA caregivers report that they have not received training that they deemed necessary [9]. Moreover, rigorous study is needed to identify effective ways of providing caregivers with the skills they need.
Fig. 1.
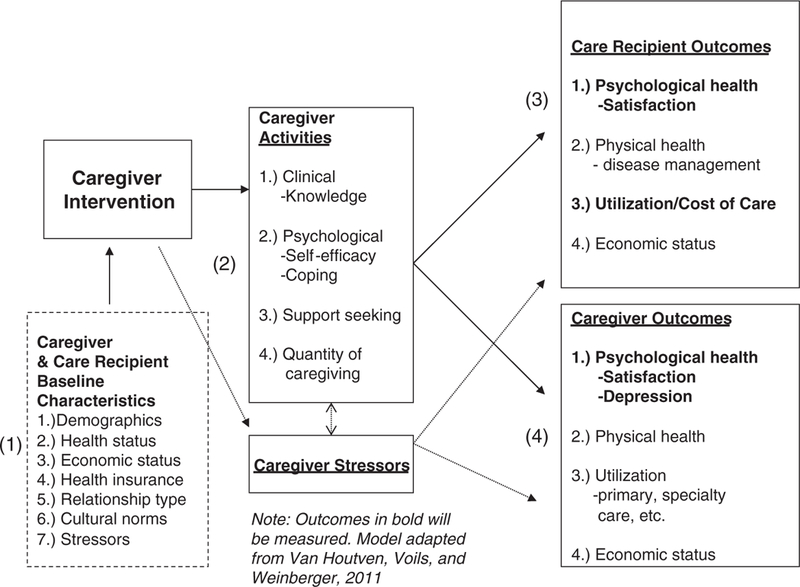
Model of HI-FIVES intervention and care recipient and caregiver outcomes.
Helping Invested Families Improve Veterans’ Experience Study (HI-FIVES) is an ongoing randomized controlled trial that is evaluating a skills training program designed to support caregivers of cognitively and/or functionally impaired, community-dwelling Veterans who may require additional services [9]. HI-FIVES is nationally relevant because other health care payers are also searching for ways to control LTC expenditures. HI-FIVES is novel in several ways. First, by focusing on functionally impaired patients with multimorbidity, rather than patients with a single disease (most often dementia), the intervention may be appropriate for broader patient populations. Second, HI-FIVES is offered when patients are referred for additional services, which may signal that the current care situation is not working. Caregivers whose patients are referred for additional services represent an important target of a skills training program. Third, our primary outcome, days at home, is patient-centered, which is rare as a primary outcome in caregiver trials. Yet such a focus is critical to both improving patients’ quality of life and supporting the VA in its mission to provide care in the least restrictive setting [10–12]. Fourth, we remove financial barriers for the financially-constrained caregivers to address low recruitment and retention rates that are common in many caregiver trials. Finally, in developing HI-FIVES, we collaborated with representatives of the VA Central Office, Patient Care Services, and VA Caregiver Support Program partners, who also serve on our Advisory Board. By involving them throughout the process, we will be well-positioned to implement the caregiver skills training program throughout VA should it prove effective.
2. Material and methods
2.1. Study design—overview of the intervention
We are conducting a randomized controlled trial of HI-FIVES, a 9-session, individual and group-based skills training program for caregivers of cognitively and/or functionally impaired, community-dwelling patients who have been referred to either VA Home and Community-Based Services (HCBS) or a geriatric clinic visit. We selected a combined individual and group-based approach because caregivers and patients have benefited from programs with a group component [13]. For example, groups appear to improve depression in caregivers of patients with dementia [14]. Most effective of all appear to be interventions that combine individual and group components. For example, the only consistent evidence that multi-component interventions delayed institutionalization was when a combined individual and group approach was used [13]. These studies suggest that significant decreases in institutionalization of the care recipient and improved mood of caregivers were sustained for three years [15]. We know little about the role of groups in caregivers of multi-morbid patients, yet in our feasibility study the group component was expressed as being critical to caregivers (unpublished data from pilot study).
Patients are referred to VA HCBS or geriatric clinic when they have a recent trigger signaling a need for more support. Following consent and baseline assessments of the caregiver and the patient, caregivers are randomly assigned within cognitive status (moderate–severe versus low–none) and prior super use (e.g. two or more hospitalizations prior to the referral to HCBS or geriatric clinic) with equal allocation to either usual care or HI-FIVES. Those receiving usual care will receive written information about the VA Caregiver Support Program, which is the standard of care for general informal caregivers in the VHA since the initiation of the VA Caregiver Support Program in 2010. Comprising of a national hotline for caregivers as well as full-time caregiver support specialists housed in every VA medical center nationally, the general VA Caregiver Support Program offers training and outreach programs to family and friends caring for Veterans of all eras.1
For caregivers in the HI-FIVES group, weekly individual phone training occurs for 3 weeks, followed by 4 weekly group training sessions. To sustain the intervention, two individual booster calls are made at one and two months after group sessions end. We collect data on our primary outcome (days at home) and secondary outcomes immediately post-treatment, as well as 6 and 12 months post-randomization. A total of 10–12 cohorts (approximately 16–24 caregivers per cohort across both arms) are enrolled over 24 months to reach our enrollment goal of 120 participants in each arm.
2.2. Hypotheses
This study tests the following hypotheses:
Primary:
H1.
The HI-FIVES caregiver skills training program will significantly increase the number of days a patient spends at home in the 12 months following randomization compared to caregivers in usual care.
Secondary:
Compared to patients receiving usual care, during the 12 months following randomization, HI-FIVES will result in a significant:
H2.
Reduction in patients’ total VA health care costs.
H3.
Increase in satisfaction with VHA health care for caregivers and patients.
H4.
Reduction in caregiver depressive symptoms.
2.3. Participant eligibility criteria
The target of this study includes informal caregivers of patients who are at high risk for nursing home entry. Prior to enrollment, the patient identifies the informal caregiver, usually a family member or friend, as the person who helps him or her because of health problems. If there are multiple caregivers, the patient is asked to identify the person who cares for them most. Both the caregiver and patient must qualify for the study.
Exclusion criteria for patients, garnered from the electronic referral data, include:
No telephone number
No VA primary care provider
Referred to receive institutional care
Eligible for hospice, palliative care, or prognosis of less than 6 months to live
Residing in institution
Referred to physical or occupational therapy only.
Additional exclusion criteria for patients, assessed by phone, include:
Has no informal caregiver
Fully independent—no need for informal care
Does not give permission to contact caregiver
Resides in institution (checking again)
Currently in hospital or short-term rehabilitation facility (we can reassess eligibility again at a later point)
Patient is communicative but unable to communicate in English.
The patient’s caregiver faces the following exclusion criteria, assessed by phone:
Not able to attend four weekly group sessions
Not able to communicate via telephone
In active inpatient or outpatient substance abuse treatment
Participating in other caregiver study
Under 18 years of age
Fail cognitive screener (defined as missing 5 or more on SPMSQ) [16]
Informs us that Veteran is in hospital or institution currently (we can reassess eligibility again at a later point)
Voluntarily assesses patient as terminal.
2.4. Recruitment and enrollment procedures
The Durham, North Carolina, VAMC refers patients to LTC using Geriatric and Extended Care (GEC) forms signed by the physician, nurse, and social worker. Using the Veterans Health Information Systems and Technology Architecture (VistA) electronic medical record, we first identify all patients who have a completed GEC form with referral to any VA-covered HCBS program in the past 6 months. HCBS programs include homemaker home health aide services, skilled home health care, home-based primary care, respite care, adult day health care, or home telehealth [17]. Electronic consult data are also used to capture the full universe of home-based primary care referrals and geriatric clinic referrals over the past 6 months. Periodic data extractions will be ongoing throughout the 2-year recruitment period to identify recent referrals. From these records the RA, project coordinator or health educator performs a brief medical record review to ensure that patient status has not changed making them ineligible.
Potentially eligible patients are sent a letter introducing the study and providing the patient the ability to opt out of receiving future contacts from the study team. The research assistant (RA) assesses eligibility by phone by first calling patients and then caregivers. In cases where the caregiver indicates that the patient has cognitive impairment, the RA probes using a protocol about legally authorized representatives (LARs) to explain and explore consent by proxy. Interested and qualifying dyads are invited to an in-person enrollment visit at the Durham VAMC to learn more about the study from the RA; assess their interest in, and eligibility for, participating; obtain informed consent from both caregivers and patients; and obtain HIPAA authorization, including permission to gain medical utilization files from non-VA sources. The caregiver is also asked to sign an authorization to audio record phone conversations between themselves and members of the study team for purposes of obtaining feedback on the intervention and ensuring fidelity to study protocol. Permission to record can be declined but will not prevent the caregiver from participating in the study. At the enrollment visit, upon enrollment, the RA will also distribute VA Caregiver Support materials to all enrolled patients and collect baseline data. Should patients and/or caregivers be unable to provide baseline data during the visit, these measures will be obtained by phone soon thereafter. In either case, randomization will occur after baseline data collection. The RA also gathers from the enrolled caregivers their chosen topics for phone training, being careful to explain that only half of them will receive the phone training (Table 1). If patients are unable to provide consent, their designated LAR may do so on their behalf, following procedures from the Durham VA IRB.
Table 1.
Topics for individual skills training phone calls.
| 1. Patient-oriented topics | |
| a. Disease information | d. Managing symptoms at home |
| b. Safety issues such as falls | e. Planning for future (directives) |
| c. Safe home environment, driving | f. Sleep hygiene for patient |
| 2. Caregiver-oriented topics | |
| a. Management of stress | d. Sleep hygiene for self |
| b. How to care for yourself | e. Coping with frustrations |
| c. When/how to ask for more help | f. Relaxation techniques |
Following the enrollment visit and baseline data collection, dyads are randomized to HI-FIVES or usual care via a computer-generated randomization sequence created by the study biostatistician. Randomization is stratified by patient cognitive status (>5 errors versus >5 errors on the Short Portable Mental Status Questionnaire) [18] and being a super user in the prior year (defined as two or more inpatient hospitalizations of any length in the 12 months prior to being referred to HCBS or geriatric clinic). To reduce bias, the RA is blinded to the treatment assignment. The project coordinator or health educator calls each enrolled caregiver as soon as it is feasible to inform caregivers of their group assignment and provides information on what to expect next, including scheduling the first phone training call for intervention subjects (described in Sections 2.5 and 2.6 below).
2.5. Overview of HI-FIVES intervention
The 9-session HI-FIVES program consists of 3 individual phone calls and 4 group sessions (8–12 caregivers/group) over about a 12-week period. The health educator schedules and delivers all training calls. Groups are held at times amenable to caregivers. To maximize peer learning effects, caregivers remain with the same group for all 4 group sessions. In addition, 2 individual booster training calls occur after the last group session (Fig. 2).
Fig. 2.
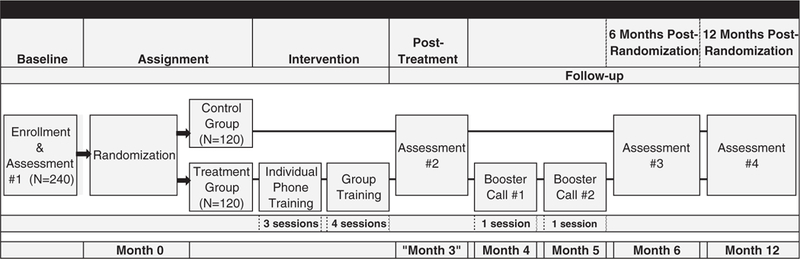
Overview of the study design.
2.5.1. Structure of individual caregiver phone training
A nurse trained in the study protocol, called the health educator, places all phone training calls (the study uses one full-time nurse in this position). The first phone session focuses on medication management, with a focus on medication reconciliation [19]. The impetus to cover medication management by phone, rather than in groups, is so that the caregiver has the patient’s medications in front of him/her before beginning. The action item to complete before the second call is determined by the health educator saying “What is the one thing that you think you could do better for the patient in helping him/her with his/her medications?”
In subsequent calls, the health educator delivers the training topics that caregivers chose to learn about (Table 1) [19]. In the second phone session, the health educator first reintroduces the last action item and gives feedback and encouragement. Then, the health educator moves to the first two priority topics for the remainder of the call. At the end, the health educator asks the caregiver, “What one thing would you be willing to do to make a positive change in your situation”? If the caregiver selected ‘taking better care of myself,’ the action item may be that the caregiver aims to go out to lunch one day with a friend. To finish the call the health educator reminds the caregiver about topics three and four for the third call. The third call follows the same structure, including an action item of the caregiver’s choosing (Table 2). Ideally these phone calls occur weekly, and precede the group training, but may overlap with group training if needed. If the phone and group training overlap, all phone training sessions assigned to an individual caregiver must be completed by the date of the last group session.
Table 2.
Individual and group curriculum modules.
| Type of training | Session objectives | Targeted skill type | Targeted outcomes |
|---|---|---|---|
| Individualized telephone training | |||
| Phone call 1 | 1. Introduction | Clinical | CR—days at home; VA cost of healthcare |
| 2. Discussion of medication management | Psychological | ||
| a. Review list of medications for reconciliation | Support seeking | CG—depressive symptoms; satisfaction with VHA | |
| b. Identify purpose of medication and dosing | |||
| 3. Action item on medication management | |||
| Phone call 2 | 1. Questions on last sessions discussion; action item | ||
| 2. Teach about first and second learning topic | |||
| 3. Elicit action item | |||
| Phone call 3 | 1. Questions on last sessions discussion; action item | ||
| 2. Teach about third and fourth learning topics | |||
| 3. Elicit action item | |||
| Group face-to-face training | |||
| Session 1 | 1. Introduction of members to group; codes of behavior | Clinical | CG—psycho-logical health |
| Introduction and caregiving discussion | 2. Overview of program | Psychological | |
| 3. Frustrations and rewards of caregiving | |||
| 4. Helping the Veteran remain independent | |||
| 5. Socializing time | |||
| Session 2 | 1. Basics of daily care, assisting with ADLs | Clinical | CR—days at home; VA cost of healthcare |
| Selected clinical and prevent injury | 2. Safety in the house: home aids, preventing falls, & gun safety | ||
| CG—psychological health | |||
| 3. Safety and medications | |||
| 4. Preventing injury | |||
| a. Proper body mechanics; exercise | |||
| 5. Socializing time | |||
| Session 3 | 1. Doctor & caregiver communication | Clinical | CR—days at home |
| Caring for the caregiver: | 2. Communication between the caregiver and the care recipient and family and friends | Psychological | CG—psychological health |
| Support seeking | CG—depressive symptoms | ||
| 3. Stress management & tips to avoid burnout | |||
| 4. Recognizing depression and burden and tools to get help and treatment | |||
| 5. Socializing time | |||
| Session 4: | 1. Basic information about VA services available to the Veteran—community and institutional | Support seeking | CR—days at home; satisfaction |
| Navigating the VA system/planning for the future | |||
| 2. VA Caregiver Support Program | CG—depressive symptoms; satisfaction | ||
| 3. Information about non-VA caregiver resources | |||
| 4. Preparing for the future: transitions and legal issues | |||
| 5. Socializing time | |||
| Follow-up booster training calls | |||
| Booster call 1 | 1. Questions on individual training phone call #3; group sessions | Psychological | CR—days at home; VA cost of healthcare |
| Support seeking | |||
| 2. Follow-up on last action item | CG—depressive symptoms; satisfaction with VHA | ||
| 3. Elicit action item from group sessions | |||
| Booster call 2 | 1. Follow-up on group session action item | ||
| 2. Progress report on caregiver and Veteran | |||
| 3. Discussion of resource needs and solutions | |||
2.5.2. Organization of group caregiver training
The health educator, a study investigator (CHV), and a VA Caregiver Support Coordinator conduct the 1.25 hour group sessions in a private conference room in the Durham VAMC. The group training relates directly to supporting caregiving activities in the clinical, psychological, and support seeking skill domains (Table 2). With limitations in activities of daily living (ADLs) being common to all study patients, the group training curriculum provides basic education on ADL management (improving clinical skill).
The group training may occur up to several weeks after the individual training has been completed with some caregivers, because it will take time to enroll a critical mass to fill a particular cohort for group training.
2.5.3. Booster calls
One and two months after group training ends (approximately months 4 and 5 of the caregiver’s enrollment date on average, Fig. 2), the health educator conducts booster training calls. In the first, the health educator follows up on the action item from the third training call and asks if there was anything from the group training that requires discussion. If so, they discuss that topic and create an action item. If not, the health educator probes about other possible issues based on recorded notes from previous calls. In the second booster call, the health educator asks about the action item from the prior call, and checks in on how the caregiver and patient are doing more generally. The semi-structured format allows the flexibility to cover topics not on the list that the caregiver finds particularly challenging.
2.6. Usual caregiver care
Usual care includes patient care and caregiver support that are normally offered once the GEC referral process has occurred. This process entails that the patient and caregiver work with an assigned social worker to obtain HCBS. At the enrollment visit, all caregivers receive information about the VA Caregiver Support Program and the national VA caregiver hotline number and they indicate phone training topics of interest. During the phone call when group assignment is revealed, information on the VA Caregiver Support Program will be reviewed. The patients in the usual care group are free to seek medical, psychological and social support, and social services that are available through VAMCs or any other source. The study staff will not be involved in this process and will only obtain assessments at the established times. At the end of the outcomes assessment period, pamphlets on the training topics selected by usual care caregivers will be sent by mail to the caregivers. These are the same pamphlets used in the HI-FIVES curriculum.
2.7. Compensation
Compensating participants for group visit attendance and for all assessments, increases the likelihood of enrollment and decreases the likelihood of study attrition. The payment for a group session reflects the replacement cost of the caregiver’s time (e.g. to hire a sitter for the patient), as well as the cost of transportation and parking. We compensate each treatment caregiver $55 per group session. We will pay these same caregivers $10 each for three individual training 30–45 minute phone calls and $10 for each booster call ($50 total for treatment caregivers). Additionally, we will pay the caregivers in both arms $10 for each of the survey assessments (baseline, post-treatment, 6, and 12 months post-randomization, or $40 total for both groups of caregivers). Thus, the maximum a treatment caregiver can receive is $310 ($55 × 4 + $10 × 5 + $10 × 4). Control caregivers can receive $40 maximum for completing the assessments ($10 × 4).
Enrolled VA patients are not compensated for taking part in assessments at enrollment and by phone. Asking the VA health care satisfaction measure of Veterans takes only a few minutes and is not burdensome to patients. Furthermore, in the pilot study (unpublished), it was common for the caregiver to answer on behalf of the Veteran due to cognitive impairment of the Veteran (36% of cases).
2.8. Measures
Measures come from medical records and interviews conducted by a trained blinded RA either in person (baseline assessment) or on the phone (Table 3).
Table 3.
Measures and timing of assessments.
| Measure | Baseline | 3-month follow-up (post-intervention) | 6-month follow-up | 12-month follow-up |
|---|---|---|---|---|
| Primary outcome | ||||
| Patient days at home | x | |||
| Secondary outcomes | ||||
| Total health care costs to VA | x | x | ||
| Patient & caregiver satisfaction | x | x | x | x |
| Caregiver depressive symptoms | x | x | x | x |
| Process/adherence measures | ||||
| Moderate to severe cognitive impairment of patient | x | |||
| Priority learning topics and time of day preferred for training | x | |||
| Attendance at group sessions | x | |||
| Feedback on intervention | x | |||
| Additional measures | ||||
| Caregiver objective burden | x | x | x | x |
| Positive aspects of caregiving | x | x | x | x |
| Caregiver subjective burden | x | x | x | x |
| Caregiver relationship satisfaction | x | x | x | x |
| Caregiver health events | x | x | x | x |
| Caregiver work events | x | x | x | x |
| Caregiver and patient demographics | x | |||
| Patient clinical (OARS) | x | |||
| Intervention costs | x | x | x | x |
2.8.1. Primary outcome
Our primary outcome measure is patient days at home during the 12 months post-randomization [20–23]. To calculate this outcome, we subtract from the total number of days a patient is in the study from the number of days in emergency department (ED), hospital or nursing home; the days not at home signal potential failures of effective home-care and are costly to the VA system. We do not count inpatient respite days as a day not at home because these are predictable, scheduled visits and do not reflect similar quality of life interruptions. For both inpatient and nursing home days, we use the admission date and discharge date to calculate days. We consider each unique date in which there is a treat and release ED visit as one day not at home.
We capture both VA- and non-VA days in these settings. Because nearly 40% of Veterans referred to HCBS at the Durham VAMC were under age 65 in FY 2010, we cannot rely on Medicare claims to capture care that is not paid by the VA. Instead we measure the Veteran’s non-VA utilization of ED, hospital or nursing home use using self-report and confirming this utilization. At all assessments, caregivers are asked about any days the Veteran spent at a non-VA ED, in a hospital or in a nursing home since the last assessment. We adapted questions from HERC on non-VA utilization [24], to include nursing home/institutional care. When any visit is reported, the RA (who is blinded to intervention status) requests information about the location and date of the visit or admission. The RA then faxes a cover letter, HIPAA authorization, and VA Form 10–5345 (Authorization to release medical records or health information) to the facility’s medical records department. These procedures were employed successfully to measure all-cause hospitalization in a recent intervention study in which Dr. Weinberger was an investigator [25]. These procedures are critical to minimize any measurement error on our primary outcome.
2.8.2. Secondary outcomes
2.8.2.1. VA health care.
VA health care costs include VA and non-VA contracted care. Total costs of VA utilization are aggregated across inpatient and outpatient fields from the enrollment date up to 6 and 12 months post-randomization for each subject for VA-provided care [26]. This captures all outpatient costs (laboratory, radiology, pharmacy, surgery, nursing, and treat and release ED visits) and inpatient costs (similar categories). Non-VA contracted care costs of inpatient and outpatient care (e.g. care provided to VA patients by contract providers) are also included; these reflect the amount paid to vendors [27].
2.8.2.2. Veteran and caregiver satisfaction with VA health care.
We use the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey to gauge caregiver and patient satisfaction with VA healthcare post-intervention and at 6 months, focusing on a global satisfaction measure about the health plan. We also examine satisfaction with the Veteran’s primary care provider. Wording has been adjusted to obtain the caregiver’s satisfaction with the Veteran’s health care. The CAHPS is at a 6th grade reading level and the global measures of satisfaction show high reliability, ranging from 0.88 (primary care provider) to 0.96 (health plan) [28].
2.8.2.3. Caregiver depressive symptoms.
We use the 10-item Center for Epidemiology Studies Depression (CESD-10) to assess depressive symptoms post-intervention and at 6 months. The CESD-10 is a broadly used and highly reliable instrument, with a retest correlation of 0.71 and kappa statistic of 0.97 (p < .001). It is also strongly negatively correlated with positive affect (r = 0.63) [29]. Effect sizes of 0.2–0.5 are considered significant gains in symptom relief [30].
2.8.3. Process/adherence measures
For caregivers in the HI-FIVES arm, we measure the type and total number of completed phone training sessions (including booster calls), as well as the number of sessions attended during the intervention period. We also collect their chosen action items and their assessment for how it went for them in trying the action items. This allows for exploratory dose–response analyses. For all enrolled caregivers, we measure on the self-reported assessments whether they made calls to the VA Caregiver Support Hotline or to program staff or joined any VA Caregiver Support Programs after group sessions ended, or used any non-VA services such as an Alzheimer’s Association caregiver support group. We also ask participants in the HI-FIVES group open-ended questions about their experience with the program and how we can improve it in the future if it is implemented.
2.8.4. Additional measures
We also collect additional measures, shown in Table 3, that add important descriptive information about the caregiver and patient participants in the study.
2.8.4.1. Intervention costs.
With an eye towards implementation if the program is effective, we also track intervention costs to know how much it would cost to implement elsewhere. Intervention-related costs are primarily comprised of the health educator’s labor costs. We assume that capital costs such as overhead costs, office space and supply costs, and telephone service costs are neutral because implementation would use existing capital. To calculate the health educator’s labor costs, he or she tracks time spent on study tasks; this time is then converted to total hours and then valued using the relevant wage and fringe benefit rates from VA Human Resources data. Throughout the study, we carefully track time required for the following tasks:
Training costs to implement the study.
Initial planning of individual and group skills training sessions. The structure and materials for the sessions were developed prior to initiation of the study, but additional planning time would be required upon implementation.
Reminder calls.
Individual training calls. Preparation for each and documentation post-call.
Group training sessions. Preparation time and all set-up and clean-up activities.
2.9. Data analyses
All of the primary and secondary analyses were defined a priori to evaluate the effect of the caregiver skills training as compared to the usual care arm using an intent-to-treat approach. We include the stratification variables of cognitive impairment and prior super use in these models.
2.9.1. Primary outcome: days at home
At 12 months post-treatment, Veterans with caregivers in the skills training program (HI-FIVES) will have clinically significant increases in days at home compared to Veterans in usual care (H1). As described in the Measures section above, the cross-sectional measure of days at home will be defined as the total number of days not in the emergency department, nursing home, or inpatient ward. The date of randomization will be “day 0” for all patients, and the maximum total possible number of days at home will be 365 for all patients. Based upon our pilot data, we anticipate that approximately 40% to 50% of patients will remain at home for the entire duration of 365 days. Therefore, the distribution of this count variable will be skewed with a “stack” at 365 days. To make this outcome variable easier to deal with analytically, our first step will be to calculate each patients’ days not at home by subtracting their number of days at home from 365. This converts the “stack” at 365 to a “stack” at zero.
Standard analysis techniques for count variables, such as days not at home, include Poisson or Negative Binomial regression. We anticipate, however, that our primary outcome will have an excess of zeros above what is to be expected from either a Poisson or Negative Binomial process. Common approaches for analyzing this type of data are the zero-inflated Poisson (ZIP) model and the zero-inflated negative binomial (ZINB) model [31]. Consequently, the first step in our analysis plan will be to determine the distribution that best fits the primary outcome: Poisson, Negative Binomial, ZIP, or ZINB. More formally, the Vuong test [32] will be used to first determine if the distribution has an excess of zeros, and a test for over-dispersion will be used to determine if a ZINB model is superior to the ZIP alternative. We will use the count-data regression model which best fits our data to test the primary hypothesis that Veterans with caregivers in HI-FIVES will have significantly less days not at home (e.g. more days at home) than Veterans in usual care.
The treatment comparison of mean days not at home over 12 months post-treatment, will be estimated using the procedures COUNTREG and GENMOD in the latest version of SAS (Cary, NC). We do not anticipate many patient deaths (i.e., <10%); however, in subsequent analyses, we will look carefully at the outcomes for the patients who die and conduct sensitivity analyses of different ways of including them. Patients who die will be observed for a shorter period of time, and we will construct their days at home using this smaller length of time. We also expect that these patients might have fewer days at home, so their values may be outliers or influential values in the sensitivity analyses.
In addition to this approach, we will also consider models that assess the time to any utilization e.g., ED visit, inpatient hospitalization or nursing home use. Because nursing home entry is rare, we will examine all types of utilization simultaneously using a competing risk hazard model. In fact, since there can be multiple re-entries to health care utilization (e.g., multiple ER visits), we will consider repeated measures (e.g., frailty) hazard models. Together, these two approaches—the cross-sectional analysis based on counts and the time to event model—will provide a comprehensive picture of the primary outcome, days not at home.
2.9.2. Total VA health care costs
At 12 months post-treatment, Veterans with caregivers in the skills training program (HI-FIVES) will have significant reductions in total VA health care costs compared to Veterans in usual care (H2).
Each Veteran’s VA total health care utilization costs will be summarized across VA and non-VA contracted care. We will first examine the proportion of zeros, skewness and kurtosis of the overall cost distribution to determine whether we need to use one-part or two-part models (if there is a significant percentage of zeros) to test this secondary hypothesis. If there is not a significant percentage of zeros— i.e., most patients incur some positive cost—then we will use a single generalized linear model as our primary analytic strategy. If the data and residuals exhibit substantial skewness or kurtosis, costs will be transformed (i.e., log or square root) to estimate an ordinary least squares equation, and predictions will be retransformed using the appropriate smearing estima-tor. If kurtosis is not substantial, we will estimate generalized linear models and use the modified Park test to identify the most appropriate generalized linear model distribution and link function. Alternatively, if there is a significant percentage of zeros, we will use a two-part model to estimate differences in total VA health care costs for Veterans with caregivers in HI-FIVES as compared to Veterans in usual care. In the first part of the model, we will use logistic regression to predict the probability of incurring any VA health care costs. In the second part of the model, we will use a generalized linear model to predict and test differences in estimated costs for each treatment arm conditional upon having a non-zero cost. Similar to the one-part model, we will examine if the positive costs need to be transformed, and we will use the modified Park test to identify the most appropriate generalized linear model and link function for the second part of the two-part model.
2.9.3. Depressive symptoms and satisfaction
Post-treatment, caregivers and Veterans with caregivers in the skills training program (HI-FIVES) will have significantly higher satisfaction with VHA health care compared to caregivers and Veterans in usual care (H3).
Post-treatment, caregivers in the skills training program (HI-FIVES) will have clinically significantly lower depressive symptoms compared to caregivers in usual care (H4).
A linear mixed model will be used to estimate changes in satisfaction and depressive symptoms over time and test H3 and H4 [33]. Linear mixed models are a flexible and powerful analytic tool for repeated continuous measures, such as satisfaction and depressive symptoms. We will assume an unstructured covariance matrix to represent the correlation between caregivers’ repeated measures. The mixed effects model parameters will be estimated and tested using SAS PROC MIXED (SAS Institute, Cary, NC) and we will interpret the sign, magnitude, and significance of the effect of being in the HI-FIVES group on the respective outcomes compared to usual care. The pilot feasibility study found that group dynamics were an important component of the intervention; therefore, we will also test whether we need to include an additional group-level random effect to these models to account for the correlation between intervention–arm caregivers in the same training group.
Finally, we have one outcome that is collected on both members of the caregiver dyad, satisfaction with care. We will expand the model described above to explore this additional source of information and correlation. The methods we will consider include: multi-level mixed models (e.g., with multiple random effects); combined mixed and time series (e.g., AR1) models; as well as “multiple informants” models which assess bivariate outcomes (like paired dyadic data), but allow for separate regression estimates for patient and caregiver [33].
2.10. Power and sample size considerations
The sample size estimate for the study, n = 120 caregivers per group, is based on the primary hypothesis that the caregiver skills training program will significantly reduce patient days not at home over 12 months for a clinically relevant duration as compared to usual care. Our hypothesized clinically relevant difference is to increase the number of days at home by 2.5 days over the 12 month follow-up. To be able to detect a mean difference of 2.5 days at home (i.e., mean reduction of days not at home from 18 to 15.5 days based on our pilot data mean of 18 days) with 85% power and a two-sided type I error rate of 5%, we need to have 100 caregivers and patients in each arm with complete follow up. We anticipate that approximately 15% of caregivers will not complete the study due to death of the patient or other attrition therefore we will enroll and randomize 240 caregivers and Veterans (120 caregivers and Veterans in each arm).
Williamson et al. noted that ZIP and ZINB models need a larger sample size than the standard Poisson or Negative Binomial methods—essentially because the excess of zeros reduces the number of subjects actually contributing to the count N 0 [34]. Therefore, we base our sample size estimate on the mean number of Poisson counts using methods described by Williamson et al. for ZIP models [34].
3. Discussion (n = 486)
This study is a significant contribution for the following reasons. First, enhancing community-based care and controlling LTC expenditures remain as important goals across all public payers—VA, Medicare, and Medicaid. Identifying innovative strategies to support caregivers is essential to achieving both goals. Second, supporting caregivers of Veteran patients is a national priority for the VHA, as evidenced by recent federal legislation to directly pay and train caregivers of defined cohorts of Veterans (Caregivers and Veterans Omnibus Health Services Act of 2010, PL 111–163). We can inform this emerging legislative effort by examining how efforts to remove financial barriers and encourage participation in training affect key patient and caregiver outcomes. We can also provide the VHA with information on how to minimize the negative mental health effects that some caregivers experience, such as higher rates of depression and strain compared to non-caregivers or non-military affiliated caregivers [5–8,35]. Our program aims to complement emerging VHA efforts to support caregivers, such as through needed mental health services for caregivers, by providing them direct support and informational support about the VHA services available to them and their patients. Third, patients referred for additional services, such as HCBS, are at a crisis point in their health and functional status. Referral also means that caregivers are at high risk of burnout. Thus, referral to home and community-based services signals that the current care situation may be not working. More services are needed to successfully support the patient in the home. By providing caregivers with the training and skills required to maintain these vulnerable patients at home, HI-FIVES may optimize patient outcomes and reduce patient costs in the short and long terms. Fourth, HI-FIVES is based on conceptual models and prior evidence in ways that would be feasible to disseminate in typical VA clinical settings at relatively low cost and effort. Fifth, there is evidence that the most strained caregivers, who are often the most economically strained, do not participate in caregiver studies. Removing financial barriers will facilitate involvement by even the most economically vulnerable caregivers. Sixth, HI-FIVES will serve caregivers of patients with a broad range of functional impairments. Most research and community-based programs for caregivers support specialized sub-populations, e.g., caregivers of dementia patients. Yet in an era of expanded supports for caregivers of Veterans in the VA health care system, effective programs are needed that serve a broader group of at-risk patients—those with functional impairment and multimorbidity. These patients are at heightened risk of nursing home entry and we need to understand how best to support them and their family caregivers. Last, involvement of the advisory board ensures that the program is implementable if found to be effective. Our goal is to create a program that can be utilized elsewhere in the VA healthcare system and beyond, and the guidance of an advisory board is vital to optimize the ability to both create a practical program and operationalize the implementation.
Acknowledgments
This project is supported by, the U.S. Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development Service (IIR 11–345). Dr. Weinberger is supported by the the U.S. Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Research Career Scientist Program (RCS 91–408). We thank the members of the study’s advisory board, for excellent input and expertise on the study: Peggy Becker, Thomas Edes, Margaret Kabat, Christy Knight, Jennifer Martindale-Adams, Linda Nichols, Kenneth Shay, Scott Trudeau, and Laura Wray.
Footnotes
1 For qualifying caregivers of post-9/11 era veterans incurred or aggravated a serious injury in the line of duty on or after September 11, 2001, comprehensive support is available, including a stipend. Our patient population is more typical of caregivers supported by the general program and referrals to the comprehensive program do not occur through HCBS or geriatric clinic referral, thus we will not likely interact with caregivers in the comprehensive program.
References
- [1].UHF. Shining the light on challenges and solutions http://www.unitedhealthfoundation.org/veterans/caregivers_of_veterans.html.
- [2].Van Houtven C, Norton E. Informal care and medicare expenditures: testing for heterogeneous treatment effects. J Health Econ 2008;27:134–56. [DOI] [PubMed] [Google Scholar]
- [3].Charles KK, Sevak P. Can family caregiving substitute for nursing home care? J Health Econ November 2005;24(6):1174–90. [DOI] [PubMed] [Google Scholar]
- [4].Bolin K, Lindgren B, Lundborg P. Informal and formal care among single-living elderly in Europe. Health Econ 2007;17(3):393–409. [DOI] [PubMed] [Google Scholar]
- [5].Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc May 2003;51(5):657–64. [DOI] [PubMed] [Google Scholar]
- [6].Gaugler JE, Kane RL, Kane RA, Clay T, Newcomer RC. The effects of duration of caregiving on institutionalization. Gerontologist February 2005;45(1):78–89. [DOI] [PubMed] [Google Scholar]
- [7].Sorensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. Gerontologist June 2002;42(3):356–72. [DOI] [PubMed] [Google Scholar]
- [8].Nichols LO, Martindale-Adams J, Burns R, Graney MJ, Zuber J. Translation of a dementia caregiver support program in a health care system—REACH VA. Arch Intern Med 2011;171(4):353–9. [DOI] [PubMed] [Google Scholar]
- [9].Van Houtven C, Oddone E, Weinberger M. Informal and formal care infrastructure and perceived need for caregiver training for frail veterans referred to VA home and community-based services. J Chronic Dis 2010;6:57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Konetzka RT, Karon SL, Potter DE. Users of medicaid home and community-based services are especially vulnerable to costly avoidable hospital admissions. Health Aff (Millwood) June 2012;31(6):1167–75. [DOI] [PubMed] [Google Scholar]
- [11].Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG. Potentially avoidable hospitalizations of dually eligible Medicare and Medicaid beneficiaries from nursing facility and home- and communitybased services waiver programs. J Am Geriatr Soc May 2012;60(5):821–9. [DOI] [PubMed] [Google Scholar]
- [12].Woodcock C, Stockwell I, Tripp A, Milligan C. Rebalancing long-term services and supports: progress to date and a research agenda for the future Baltimore: UMBC; June 2011. [Google Scholar]
- [13].Goy E, Freeman M, Kansagara D. A systematic evidence review of interventions for nonprofessional caregivers of individuals with dementia; 2010. [PubMed]
- [14].Thompson CA, Spilsbury K, Hall J, Birks Y, Barnes C, Adamson J. Systematic review of information and support interventions for caregivers of people with dementia. BMC Geriatr 2007;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mittelman MS, Ferris SH, Shulman E, Steinberg G, Levin B. A family intervention to delay nursing home placement of patients with Alzheimer’s disease. A randomized controlled trial. JAMA 1996;276(21):1725–31. [PubMed] [Google Scholar]
- [16].Toseland RW, Smith TL. The impact of a caregiver health education program on health care costs. Res Soc Work Pract 2006;16(1):9–19. [Google Scholar]
- [17].VA. Eligibility criteria for home and community based services Available at: http://www.va.gov/geriatrics/Guide/LongTermCare/Eligibility.asp# . [Accessed May 6, 2013].
- [18].Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc Oct 1975;23(10):433–41. [DOI] [PubMed] [Google Scholar]
- [19].Kopelowicz A, Zarate R, Gonzalez Smith V, Mintz J, Liberman RP. Disease management in Latinos with schizophrenia: a family-assisted, skills training approach. Schizophr Bull 2003;29(2):211–27. [DOI] [PubMed] [Google Scholar]
- [20].Lawton MP, Brody EM, Saperstein AR. A controlled study of respite service for caregivers of Alzheimer’s patients. Gerontologist February 1989;29(1):8–16. [DOI] [PubMed] [Google Scholar]
- [21].Van Houtven C, Voils C, Weinberger M. An organizing framework for informal caregiver interventions: detailing caregiving activities and caregiver and care recipient outcomes to optimize evaluation efforts. BMC Geriatr March 2011;11(77). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med 2006;145(10):727–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Gitlin LN, Reever K, Dennis MP, Mathieu E, Hauck WW. Enhancing quality of life of families who use adult day services: short- and longterm effects of the adult day services plus program. Gerontologist October 2006;46(5):630–9. [DOI] [PubMed] [Google Scholar]
- [24].Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev April 2006;63(2):217–35. [DOI] [PubMed] [Google Scholar]
- [25].DeWalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, et al. Comparison of a one-time educational intervention to a teach-to-goal educational intervention for self-management of heart failure: design of a randomized controlled trial. BMC Health Serv Res 2009;9:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].VIReC. VIReC research user guide: VHA decision support system clinical national data extracts; 2009. 1–137 [Hines, IL: ]. [Google Scholar]
- [27].Smith M, Chow A. Fee basis data: a guide for researchers Menlo Park, CA: VA Palo Alto, Health Economics Resource Center; 2010. [Google Scholar]
- [28].Hargraves JL, Hays RD, Cleary PD. Psychometric properties of the Consumer Assessment of Health Plans Study (CAHPS) 2.0 adult core survey. Health Serv Res December 2003;38(6 Pt 1):1509–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Andreson E, Malmgren J, Carter W, Patrick D. Screening for depression in well older adults: evaluation of a short form of the CES D. Am J Prev Med 1994;4:77–84. [PubMed] [Google Scholar]
- [30].Schulz R, O’Brien A, Czaja S, Ory M, Norris R, Martire LM, et al. Dementia caregiver intervention research: in search of clinical significance. Gerontologist October 2002;42(5):589–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Long J. Regression models for categorical and limited dependent variables Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- [32].Vuong Q. Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica 1989;57(2):307–33. [Google Scholar]
- [33].Fitzmaurice G, Laird N, Ware J. Applied longitudinal analysis Wiley; 2004. [Google Scholar]
- [34].Williamson J, Lin H, Lyles R, Hightower A. Power calculations for ZIP and ZINB models. J Data Sci 2007;5:519–34. [Google Scholar]
- [35].Tanielian T, Ramchand R, Fisher M, Sims C, Harris R, Harrell M. Military caregivers: cornerstones of support for our nation’s wounded, ill, and injured veterans RAND; 2013. [PMC free article] [PubMed] [Google Scholar]


