Abstract
Objectives:
To understand clinicians’ impressions of and decision-making processes regarding an informatics-supported antibiotic timeout program to re-evaluate the appropriateness of continuing vancomycin and piperacillin/tazobactam.
Methods:
We implemented a multi-pronged informatics intervention, based on Dual Process Theory, to prompt discontinuation of unwarranted vancomycin and piperacillin/tazobactam on or after day three in a large Veterans Affairs Medical Center. Two workflow changes were introduced to facilitate cognitive deliberation about continuing antibiotics at day three: (1) teams completed an electronic template note, and (2) a paper summary of clinical and antibiotic-related information was provided to clinical teams. Shortly after starting the intervention, six focus groups were conducted with users or potential users. Interviews were recorded and transcribed. Iterative thematic analysis identified recurrent themes from feedback.
Results:
Themes that emerged are represented by the following quotations: (1) captures and controls attention (“it reminds us to think about it”), (2) enhances informed and deliberative reasoning (“it makes you think twice”), (3) redirects decision direction (“…because [there was no indication] I just [discontinued] it without even trying”), (4) fosters autonomy and improves team empowerment (“the template…forces the team to really discuss it”), and (5) limits use of emotion-based heuristics (“my clinical concern is high enough I think they need more aggressive therapy…”).
Conclusions:
Requiring template completion to continue antibiotics nudged clinicians to re-assess the appropriateness of specified antibiotics. Antibiotic timeouts can encourage deliberation on overprescribed antibiotics without substantially curtailing autonomy. An effective nudge should take into account clinician’s time, workflow, and thought processes.
Keywords: Physician decision-making, Antibiotic discontinuance, Dual Process Theory, Antibiotic stewardship
1. Introduction
Antibiotic use increases bacterial resistance and inappropriate antibiotic use increases this resistance needlessly [1–3]. In turn, the perception of rising bacterial resistance prompts use of broader-spectrum antibiotics, which fuels further bacterial resistance. This feedback cycle seems destined to culminate in a “post-antibiotic era” [4] where antibiotics are not reliably effective [5]. Unfortunately, there are few new antibiotics in development to take their place; therefore, high priority is placed on strategies to curtail inappropriate antibiotic use.
An antibiotic timeout is a scheduled time for clinicians to reevaluate the appropriateness of their patients’ antibiotics [6,7]. It is a compromise between the drive to start broad initial, empiric therapy on one hand and reducing broad-spectrum antibiotic exposure on the other. For example, broad empiric therapy has been recommended for patients with suspected pneumonia or sepsis and who are at risk for more resistant pathogens to minimize the chance that administered antibiotics will have no activity against the pathogen, the identity of which is still unknown during the critical first days that a culture takes to grow [8–10]. To minimize inappropriate antibiotic exposure, timeouts prompt clinicians to tailor antibiotics after the third day of therapy when clinical improvement can be evaluated and the pathogen(s) may be identified [7]. Prior evaluations of timeout or post-prescription review interventions have not observed uniformly improved antibiotic use nor investigated the behavioral underpinnings of the interventions [6,11–16].
The purpose of this qualitative evaluation is to understand the context and experience of clinicians using timeout procedures in order to design more effective antibiotic stewardship interventions. We describe our experience implementing a timeout intervention.
2. Background
Stewardship interventions are often classified as either restrictive or persuasive [5]. Many restrictive programs require prior approval of antibiotic prescriptions by stewards. In this case, the decisional authority to use antibiotics is removed from the clinician, curtailing autonomy. In contrast, many persuasive interventions have stewards making non-binding antibiotic recommendations, thereby preserving clinician autonomy. Traditionally, timeouts are considered persuasive interventions. But as described in the methods below, antibiotic timeouts could be designed with elements of both approaches. Allowing clinicians to retain primary responsibility for antibiotic prescriptions addresses their preference for autonomy [17,18]. Previous studies note that clinicians may be open to guidance but view restriction as a threat to their autonomy [19–21]. Compelling clinicians to own the responsibility for their antibiotic prescriptions may cause them to respond more thoughtfully to these decisions. This work is an exploration and characterization of clinicians’ experience with a goal to gain insights that inform improvements in the design and implementation of future programs.
2.1. The intersection of timeout intervention studies and cognitive models
Timeout intervention studies have produced both favorable and neutral results, possibly due to uncontrolled social and psychological mechanisms that remain poorly understood [22]. The intervention examined here was constructed using our current understanding of antibiotic decision-making during an antibiotic timeout and the use of electronic decision support to reduce the time to review cases and streamline workflow to maximize attention to the decision and minimize the cognitive work of making those decisions.
Dual Process cognitive models constitute a “meta-theory” explaining human attention, motivation and decision-making [23,24] and provide a model with which to understand potential timeout mechanisms. Two systems of memory are posited, both of which are activated simultaneously in various intensities. One is built through successive associations and experience and includes emotional, rational, and situational components (System 1). No actual reasoning is involved and activation is automatic and often without awareness. It is what many people refer to as intuition and provides the kind of pattern-matching knowledge associated with experts. System 1 is a very effective basis for information processing as it is fast, uses common heuristics, and effortlessly activates a dense knowledge structure that includes emotions, values, and well-learned behaviors. Most importantly, it is our default under high cognitive loads. In contrast, System 2 is more rule-based, conscious, deliberative, and slow. It comes into play when accomplishing goals that require more attention, deliberative reasoning, and active learning. These two systems are continuous, simultaneous processes, but with System 1 acting as default in order to preserve cognitive resources [25]. If guidelines are available (e.g. antibiotic prescribing) that can be followed with little thought, or when others are taking responsibility, then fewer System 2 resources will be applied because less deep thinking is required. Even when circumstances require the high intensity effort of deliberate thought, System 1 may engage avoidance strategies, such as when clinicians will just order a broad-spectrum antibiotic (because of the urgency of the situation) and worry about the consequences later (delaying cognitive effort). We used this model to craft our bundled timeout intervention.
3. Method
3.1. Description of the bundled intervention
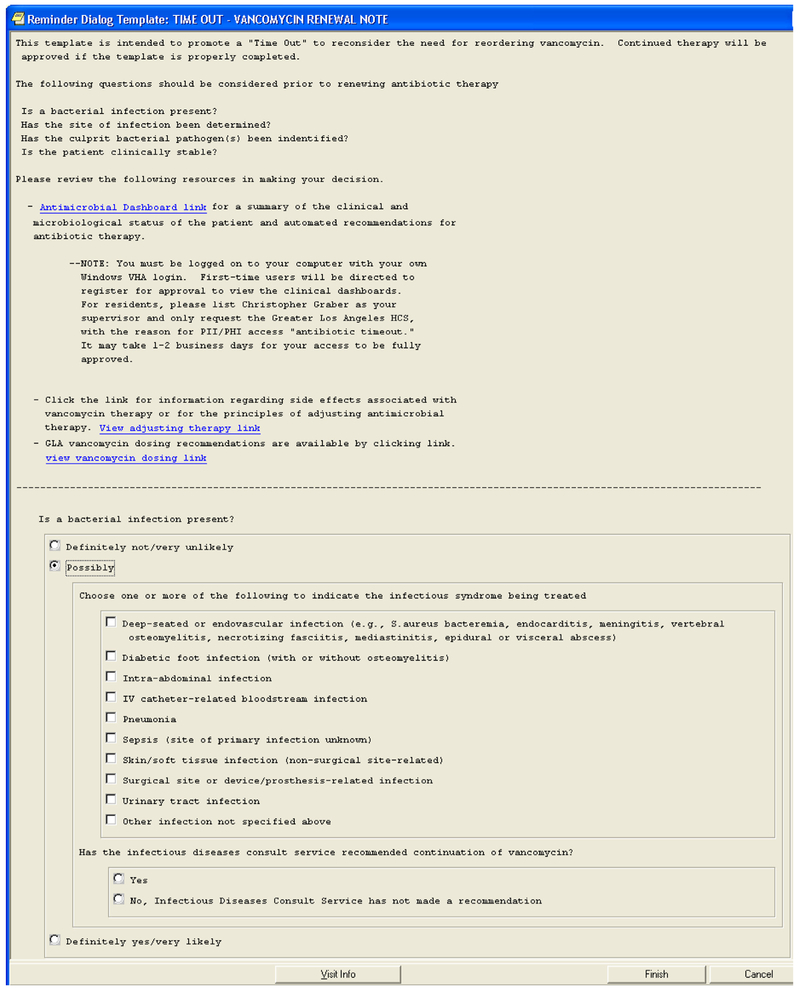
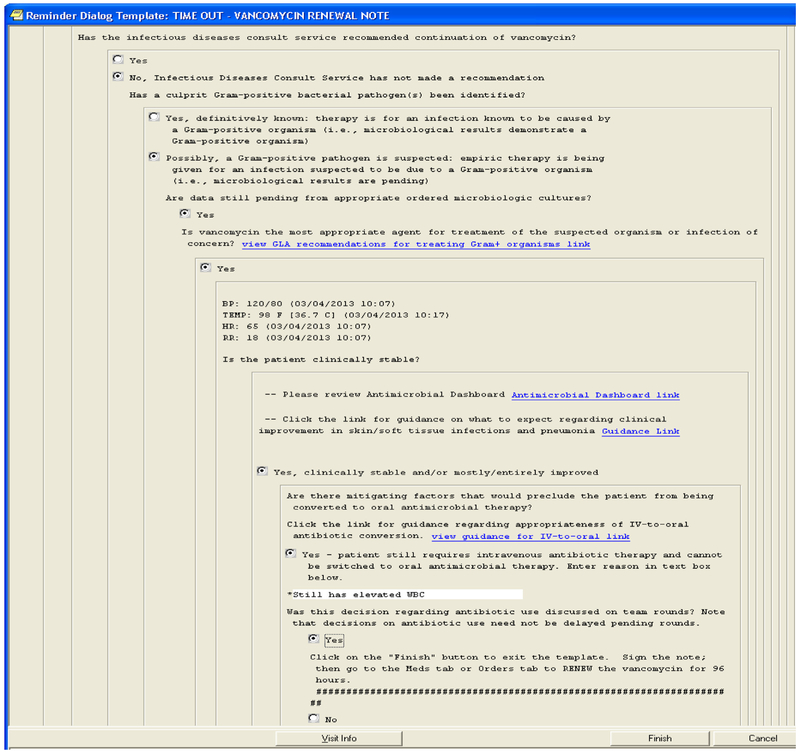
Our antibiotic timeout intervention consisted of four primary components: (1) an electronic antimicrobial dashboard that summarized data potentially useful in antimicrobial decision-making (e.g., temperature, white blood cell count, microbiology tests) and would be expected to support System 1 pattern-matching; (2) a progress note template in the electronic record (templated note) that both guided clinicians through the antimicrobial decision-making process and documented that a timeout took place (Appendix B); (3) education about the timeout through didactic meetings, websites, and flyers; and (4) a promotional campaign utilizing respected clinical champions to increase staff awareness [26]. The progress note template embodied guidelines as formulated and promoted by the antibiotic stewardship program.
During timeouts, inpatient clinician teams taking care of patients who are receiving three or more days of vancomycin and piperacillin/tazobactam were asked to discuss during rounds whether these antibiotics were appropriate. If the team felt that antibiotics were justified, they filled out a templated note outlining their reasoning [26]. The note, entitled, “Timeout-Vancomycin (or Piperacillin-Tazobactam) Renewal Note” removed the necessity of calling the steward for approval. It also included an attestation that the timeout procedure had taken place [27].
The need to fill out the template note to continue these antibiotics made stopping them the default course of action, as well as the action requiring the least amount of cognitive effort. We anticipated that in this context, the need to justify continued vancomycin or piperacillin/tazobactam would prompt a switch to a more deliberative System 2 cognitive processing with minimal impact on work processes. Since deliberative processing requires substantial cognitive resources, we provided a patient data summary of pertinent information in order to facilitate pattern-matching, e.g., graphs demonstrating a trend toward improved vital signs or an improving white blood cell count.
3.2. Settings and participants
The intervention took place at the West Los Angeles Veterans Affairs (VA) Medical Center, which had a long-standing antimicrobial stewardship program, a strong Pharmacy and Therapeutics Committee, and a prior policy of requiring infectious diseases (ID) approval for vancomycin and piperacillin-tazobactam continuation past 3 days. Details of the intervention are described elsewhere [26], but briefly, the intervention was rolled out in a staged fashion starting on Medicine wards and then successively through the medical and surgical intensive care units and finally throughout the rest of the hospital. The study received approval from the Institutional Review Boards of the University of Utah and the VA Greater Los Angeles Healthcare System.
3.3. Description of procedures
Two weeks after the intervention was implemented on its first wards, six focus groups were conducted with users or potential users of the timeout intervention at the study hospital. There were four internal medicine teams (4–6 members per team), one ICU team (5 members), and a team of three clinical pharmacists [28,29]. Teams included attending physicians and residents. Focus groups were conducted in staff rooms and general clinical areas. In addition, three pharmacists involved in antimicrobial stewardship were interviewed individually. The study team recruited, enrolled, and obtained consent from participants. Two research team members (CW, JB) traveled to Los Angeles to conduct the focus groups.
Focus groups were organized in accordance with standard qualitative research procedures for focus groups, including use of semi-structured questions, a script, and procedures that minimize conformity pressures [29]. The questions themselves were developed and piloted in the VA Salt Lake City Health Care System. The same semi-structured interview script was used for all focus group sessions and interviews. It consisted of an introduction, description of the system, a query for a description of a recent case in which vancomycin was prescribed by members of the team, and how the case was handled based on the timeout system. Participants were also asked to contrast their experience prescribing restricted antimicrobials before and after implementation of the timeout system (Appendix A contains sample questions).
All focus group interviews were audiotaped and transcribed. De-identified transcripts were then loaded into ATLAS@ti, software. Our qualitative analyses used standard qualitative research practices, including multiple reviewers, iterative analysis, and discussion over approximately 40 h over a two-month period by an infectious disease physician, a nurse with human factors background, and a psychologist. Transcripts were pre-coded independently by investigators and discussed in a group, identifying “pre-codes” referring to concepts, categories, and relevant issues (about 37–40). These concepts were refined into categories that clarified the constructs using concept mapping and network visual displays. Finally, after more discussion, the categories were distilled into themes. The process was highly iterative, involving clustering and categorization, followed by discussion and re-coding. When all transcripts were reviewed multiple times with no new constructs identified, thematic codes were developed through a final set of discussion and review [30–32].
4. Results
Five themes emerged and are listed in Table 1. Each theme is subsequently described more fully with illustrative quotes.
Table 1.
Themes from qualitative analysis.
| Themes | Description |
|---|---|
| Captures and controls attention | Timeout oriented and forced attention to the antibiotic renewal task |
| Enhances informed and deliberative reasoning | Timeout prompted clinicians to “think twice” about continuing antibiotics. It structured the reasoning processes and provided useful information to reduce uncertainty |
| Redirects decision direction by making inappropriate vancomycin and piperacillin/tazobactam discontinuation easier than continuation | The process of using something new is effortful. The timeout system required clinicians to stop and think in order to continue targeted antibiotics, which cost time and effort |
| Fosters autonomy and improves team empowerment | Timeout increased personal responsibility and autonomy. The result was a sense of decreased dependency on the infectious disease pharmacist. There was evidence of an adversarial relationship between clinicians and stewards before the intervention |
| Limits use of emotion-based heuristics | This heuristic assumes the strength of the felt emotion is strongly correlated with the logic of decision-making. People answer the question of what they think with what they feel. When clinicians previously sought approval from stewards, they were asked to justify their decisions, which prompted them to “reach” for a reason to support what they had already decided to do |
Theme 1 (Captures and controls attention): The antibiotic timeout program oriented attention to the antibiotic renewal decision
Clinicians noted that the timeout interrupted their normal processes and prompted focus on the necessity of antibiotics. The italicized quotations below are related to the themes. Bold was added to highlight key phrases.
“…in this case I was like, I still need this vancomycin [for the case at hand], so let me just click, but if it was like uncomplicated cellulitis or abscess… I would appreciate it because it makes me think.”
“Like as a resident you try to, of course, avoid unnecessary use of antibiotics regardless, so it’s kind of like, it reminds us to think about it…”
Theme 2 (Enhances informed and deliberative reasoning): The Antibiotic Timeout program provided key information to guide and support deliberative reasoning
Clinicians appreciated the way that approval template questions provided structure, prompting them to consider diagnoses and the results of cultures. It also appeared to help organize their thoughts when there were multiple demands on their time, thereby making the cognitive effort of reasoning less burdensome.
“It helps organize…a lot of times medicine algorithms are really great, I mean, it helps you think about different cases and step-by-step action, so I think it’s providing people with a nice way to think about how they’re treating infections…an organized way.”
“Again, it just makes you think more about like the real indication for the big gun.”
“It makes you think twice.”
“You’re avoiding paperwork, but in the process of avoiding paperwork you’re doing more to actually think about infectious disease and medication so.”
“I believe [the new program] kind of asks you like what’s the need for the antibiotic?… They’re supposed to go step by step and it kind of makes them think about does this patient really need antibiotics…”
The program provided salient information that was previously harder to get. The display of the relevant vitals, laboratory, antimicrobial, and microbiology information together (as in a dashboard) in one place was noted as being helpful for evaluating the patient’s clinical status. In addition, the educational resources filled in gaps in knowledge and increased confidence.
“You can already tell he’s getting better just by looking at all those graphs, they’re all turning the right way.”
“There’s also a good link in there if you’re not sure, right, because it asks if you feel it’s clinically necessary and it has a link to all this criteria where if you should suspect MRSA versus MSSA.”
Theme 3 (Redirects decision direction by making inappropriate vancomycin and piperacillin/tazobactam discontinuation easier than continuation): Changes in the burden of clinical decision time and effort management made the antibiotic timeout system appealing
Using the template did take time and effort, even though its structure and interface mitigated that effort. Antibiotic timeouts deterred continuation of inappropriate antibiotics because filling out the template was not felt to be worth the trouble, despite the fact that the template allowed for providers to continue antibiotic therapy by simply asserting that it was necessary. Nevertheless, some felt that the old system, which required communication with the pharmacist, was easier because letting the pharmacist decide was less effort.
“…it just becomes frustrating when there’s something that slows [interns and residents] down even if it’s just for a few minutes…”
“I think [the approval template is] definitely a lot quicker and easier [than the old system].”
“ [the approval template]… seemed like it flowed pretty well and it gave you good options to choose from and didn’t take too long of a time or wasn’t too burdensome.”
“If it was indicated I would have fought for it, but because I thought there was really no indication, I really don’t want to like try to go through this whole process [of the approval template] so I just [discontinued] it without even trying.”
In addition, just knowing that they were being monitored stimulated reconsideration of whether vancomycin was needed and may have triggered a common psychological process – reactance [33]. Reactance occurs as a result of threat to autonomy and, here, manifested itself as an active avoidance of the approval process.
“No, seriously, the fact that they handed me this form in the morning saying, oh, we’re tracking your vanco usage made me not want to use it.”
“Yeah, the use of vanco, but I mean when I was GMED I was thinking, oh, they’re going to check if I’m using…if I’m doing this Timeout so I specifically just [discontinued] it.”
Pharmacists noted that there was a substantial impact on their workflow, increasing the time that they had to go through a case thoroughly.
“Imagine when we get interrupted every single five minutes, you can’t have anything done. You’re in the middle of something and then somebody calls you, you do that, you come back and start all over again, but with this it will now give me more time. I still keep an eye on dose, although I know who is on vanco and who is on Zosyn, but it gives me more time to go into the chart and look even though they submit the Timeout I do go in and see, do they really, really need it? So it makes my day go a lot smoother.”
Theme 4 (Fosters autonomy and improves team empowerment): Clinicians reported a sense of increased autonomy as well as changes in role relationships and dependencies
Prior to the implementation of the antibiotic timeout system, approval for prescriptions of vancomycin or piperacillin-tazobactam at the study hospital required approval by the infectious disease pharmacist or fellow. Following the implementation of the system, clinicians received a hand-delivered clinical summary and documented self-approval of antibiotics. They valued personal responsibility and autonomy. They preferred to make decisions on their own, relying on backup when necessary.
“…I think as the general team, we feel we can manage the antibiotics until it gets to a certain point obviously. We might need some support, but just continuing vancomycin I think we feel comfortable that we could do the template and not to refer to them.”
“You don’t want to seem like a helpless individual.”
“It was like back in the day I would just not care as much because I would just ask ID (infectious disease) but then I started to think about my patients and that they really needed it and a lot of times they didn’t.”
It also prompted teamwork:
“I think the template is good in that it forces the team to really discuss it.”
In addition, the relationship with the infectious disease pharmacist appeared to change. Clinicians appreciated the ability to approve their own antibiotics using the template rather than having to contact the infectious disease pharmacist (which they sometimes viewed as a waste of time). In other words, there appeared to be a sense of greater autonomy.
In addition, resident physicians reported that, even with the antibiotic timeout system, the decision to discontinue antibiotics ultimately resided with the attending physician or with infectious disease experts, if involved. To some extent, the timeout program was perceived as useful for minimizing burden on the infectious disease experts and attending physicians. The relationship with attending physicians and infectious disease specialists varied by floor and there was a perception that the template was more useful for general medicine teams (as opposed to intensive care), where decisions were deemed less complicated.
“I have to do what the attending wants.”
“And I don’t feel like we generally make those kinds of decisions on our own without ID (infectious disease) recommendations supporting that.”
Theme 5 (Limits use of emotional-based heuristics): Before timeout implementation, being asked by a steward to justify a decision may have prompted clinicians to “reach” for reasons
The “clinical picture,” acknowledged by both clinician and steward as relatively inaccessible to stewards, was frequently invoked by clinicians and appeared to be the ultimate arbiter of stewardship encounters. Clinicians were either unaware or minimized this tendency to appear to use a rational argument as a substitute for the real reason, worry, or fear of regret.
In general, post-prescription reviews appear to highlight, or perhaps even prompt, the rationalization process (because there was a direct request for a rationale). When pressed for justification of antibiotics, clinicians and stewards asked themselves and each other whether antibiotics were necessary.
“on day 3 I’m going to need to provide some justification for my use of the antibiotic.”
“you call the infectious disease pharmacist, like I need to renew this. And she’s like why? Because he’s got an infection…”
Pharmacists also mentioned that when called, they prompted clinicians to state their thought processes.
“…then too you have to dig in and ask them why [they] want it and go through [it] with them…”
When clinicians considered whether antibiotics were justified, they usually made general, emotion-laden statements about clinical need that lacked grounding in verifiable and objective data.
“…I still need this vancomycin.”
“Well, I mean I won’t…I just, I don’t give people things unless they really need it.”
“Actually, he probably doesn’t need vancomycin at this point”
Pharmacists used similar language:
“I do go in and see, do they really, really need [vancomycin and piperacillin/ tazobactam]?”
When asked why antibiotics were necessary, clinical suspicion was often invoked. Both clinicians and stewards suggested that the clinical picture can only be discerned at the patient’s bedside–meaning that clinicians can see the clinical picture and stewards cannot. One clinician remarked about this limitation of steward review,
“[pharmacists] can review the chart, but it’s I think sometimes tough for them to get a grasp of sort of the whole picture of how the patient truly looks and really getting accurate, I guess, idea of how sick the patient is and what really your … suspicion is for MRSA or something like that.”
From the stewardship perspective: “I know, …99% of the detail…, with the exception of the clinical status currently.”
Clinical judgment was used to rationalize continued vancomycin, even when the evidence present would suggest stopping vancomycin.
“given the nature of how ugly the infection was, we wanted to continue the vanco even though we had some blood cultures growing or some wound cultures growing out that were not actually MRSA.”
Or, the decision could be justified on the basis of an improving clinical picture.
“… and then you see that the patient is improving with that [antibiotic] and why not just continue it for a couple of more days to be on the safe side…”
In any case, interrogation may prompt post hoc reasoning and a reliance on the “reason” that gives them the most freedom and flexibility. These post hoc reasons might have been an attempt to vocalize the automatic pattern-matching activity of System 1 where they have a “hunch” or they have worries that may not seem rational to them, but still feel “right.” Notably, no clinician voluntarily mentioned antibiotic resistance or population as concerns. Resistance was only mentioned when clinicians were musing on why the timeout program was implemented.
The possibility of invoking clinical judgment as a type of privileged information to manipulate approvals was also brought up by clinicians. An adversarial tone was present in both described interactions and in their attitudes toward stewards. The following quotes are from clinicians interviewed together who referenced both the pre-existing program and the timeout.
Clinician 1: “And when we speak to the pharmacist as well, if they’re saying, well, I don’t see why you’re choosing this antibiotic; why don’t you just choose this? We can say to them person to person, look, my concern… my clinical concern is high enough I think they need more aggressive therapy at least for right now and usually they will agree to that because it’s clinical judgment; it comes down to that so the template kind of does the same thing, so…”
Clinician 2: “… You can say that about everybody and put everybody on vancomycin…”
“I don’t see the point of talking to ID (infectious disease) pharmacists… because they usually say, okay… I’m like, oh, why did I have to like take extra time to talk to you just to say…just to hear that you say okay. Like, there’s no critical like thinking involved on the other end…”
It should also be noted that, before the timeout, infectious disease pharmacists felt that residents were not invested in the antibiotic decision.
“And a lot of times when they call me, oh, yeah, have ID (infectious disease) approve it or have ID (infectious disease) discontinue it, but they don’t feel the responsibility at all.”
5. Discussion
We present the experience of a hospital transitioning from a strong restrictive program to a timeout program that nudges clinicians to consider whether to continue or discontinue inappropriate vancomycin and piperacillin/tazobactam, while supporting them through the reasoning process when necessary to continue these antibiotics when appropriate. Our results confirmed some of the theoretical underpinnings of the timeout intervention, as well as added clarity on issues of adoption and implementation. From the perspective of dual process theories, the goal was to prompt clinicians to think more deeply about the appropriateness of continuing antibiotics, while at the same time minimizing the cost of that deeper cognitive processing. Our findings suggest that we accomplished that goal in several ways. First, many clinicians reported simply that it “made them think” (Theme: Captures and controls attention). Second, both clinicians and stewards reported having to “think twice” about whether antibiotics were really necessary—an indicator that antibiotic decision-making became more deliberative e.g. system 2 thinking (Theme: Enhances informed and deliberative reasoning). Third, it appeared that the small impediment that the timeout presented to workflow alone was enough to “nudge” [34] clinicians toward not routinely continuing targeted, inappropriate antibiotics in circumstances where the effort was not worth the perceived benefit (Theme: Redirects decision direction). Fourth, clinicians felt empowered to make their own decisions and this may have led to increased feelings of personal responsibility and hence more motivation to attend to the problem. In addition, the intervention may reduce the sometimes adversarial relationship between clinicians and stewards. Reactance on the part of clinicians was noted both to encounters with stewards and to the timeout; however, it seemed personal and manipulative with stewards but limited to a reluctance to perform extra work in the case of the timeout (Theme: Fosters autonomy and improves team empowerment). Finally, the tendency to substitute an emotional reason with a supposedly logical explanation is minimized when the situation for providing such an explanation is less frequent. Ambiguous “clinical suspicions” were frequently used by clinicians to justify antibiotic necessity to stewards. However, making such explanations to others may give the clinicians the false sense that they have engaged in adequate decision-making.
The intervention appears to have made an impact on thought processes, roles, and work processes without major impediments to autonomy. Participant responses suggested a perceived reduction in the time necessary to negotiate the “approval process,” more autonomy, and an increased sense of responsibility. These factors could change the primary team attending phsycian’s involvement by systemizing the decision and creating less dependency on her or his authority. Timeouts may lead to a culture of greater self-sufficiency and changes in infectious disease consultation patterns.
Most other studies of interventions have been of those that have been more classically either restrictive or persuasive. A recent systematic review using the restrictive/persuasive framework concluded that despite larger early effects seen in restrictive interventions, the impact of persuasive and restrictive interventions did not differ at 12 months [5]. Furthermore, the authors suggested that persuasive measures could be used to “win the hearts and minds” of practitioners [5]. Our timeout approach was a blend of both intervention types that appears to have been received well in early implementation. There have been other recent antibiotic stewardship interventions that have used a “nudge” framework [34] but these have been in the outpatient setting [27].
5.1. Implications for practice
Our timeout intervention appeared to encourage clinicians to stop inappropriate vancomycin and piperacillin/tazobactam. However, we noted participants’ language during discussion tended to frame the issue as whether these antibiotics were necessary. To design a timeout where clinicians consider the full meaning of appropriateness, i.e., to give the right drug at the right dose by the right route for the right duration etc., it may be necessary to further frame the timeout to encourage this result. Perhaps the question that clinicians naturally asked, “is this antibiotic necessary,” could be replaced with “is this antibiotic regimen best for my patient, with respect to recovery, adverse events, and resistance?” This might help structure clinician thought processes to contemplate the optimal antibiotic regimen, as well as seldom-considered issues, such as adverse events and resistance.
There may also be a role for improving communication and relationships between stewards and clinicians. Clinicians sometimes felt that there was no value in talking with stewards. If clinicians felt less encroachment on their autonomy and stewards had concrete and applicable information to give and relayed their reasoning to clinicians then clinicians might be more appreciative and place higher value on stewardship consultations. Finally, it may be useful to have clinicians commit to an antibiotic action plan if cultures are negative before culture results come back in order to prevent post hoc justification—for example, by committing to stop vancomycin if culture results come back negative. This would nudge clinicians to abide by a thought-out strategy, instead of rationalizing their course of action post hoc.
5.2. Implications for implementation
Participants reported concerns with time, effort, and work disruption. Because the timeout program needs coordination across teams and attendings, both of whom come and go regularly, orientation to the program needs to be seamless and ongoing. The influence of attending physicians s has been noted previously [35]. Providing links to electronic health record patient summaries, as well as to note templates would be helpful in alerting clinicians. In addition, prior to this implementation, the Antibiotic Dashboard was refreshed on a nightly basis and therefore lacked the most recent clinical and laboratory data (e.g., from that morning).
5.3. Relevance to design of decision support
There may be a valuable role in electronic decision support given the sometimes adversarial relationship between stewardship and clinicians. The timeout program provided an electronic dashboard that concisely demonstrated the patient’s clinical picture and trajectory coupled with a process (note template writing) that forced the author to step through and document the logic of the timeout decision. This last step nudged clinicians to reconsider continuing an antibiotic. Despite this direction, clinicians did not express the same type of resentment that they voiced about stewardship.
A decision support design that has the goal of capturing the attentional resources of clinicians must carefully balance the tension between the pull toward automatic processing and the overt conscious motivation of making an accurate decision. Clinicians will resort to pattern-matching, heuristic processing if the information environment is impoverished (manifested by post hoc rationalization), if tools for controlling their information environment are not available (requiring increased effort), and if the needed information is simply not available. This timeout intervention provided enhanced, easily accessible information and a process that supported some conscious deliberative thought. Future work could focus on enhancing the tool sets available to the clinicians by supporting more “if-then” simulations and population-based information.
6. Limitations
Data for this study were collected early in the implementation phase of an intervention. A follow up study would have allowed for investigation of unintended consequences, e.g., whether antibiotics might be discontinued inappropriately because of reactance or whether antibiotics would be left as is until the timeout, even if it became apparent that they were unnecessary at an earlier time. Also, respondents may have been inclined to make more positive comments to the interviewers who were involved in the study. Potentially different themes could have emerged after a longer period of use. In addition, the study was conducted at one facility and may not be completely generalizable across different geographical areas. The teaching role of the hospital also makes the implementation process more applicable to hospitals with training programs, particularly because many intervention components mainly interfaced with trainees. Characteristics peculiar to VA may also limit applicability in other settings. Finally, the study uses qualitative data and the findings should be viewed as suggestive.
Interviewees noted that the timeout grabbed their attention and “made [them] think,” but recounting that this occurred this way is not necessarily the same as what they actually experienced. They likely did not notice that their direction of focus had been changed at the time.
7. Conclusions
A timeout intervention appeared to cause both deeper cognitive processing and increased deliberative attention (System 2) to several areas of antibiotic decision-making—a finding anticipated by Dual Process theories. Increased attention to the task of antibiotic decisions, changes in the relationship with stewards, increased sense of autonomy and increased patterns of non-specific justification patterns were observed. Using Dual Process theories to guide the development and implementation of timeout interventions may ultimately lead more consistently to higher quality antibiotic practice.
Acknowledgements
The authors acknowledge the Veterans Informatics and Computing Infrastructure, VHA Office of Informatics and Analytics, and VHA National Infectious Disease Service for their tireless support building the infrastructure necessary to make this and projects like it possible.
Funding
This work was supported by contract 200-2011-42039 from the Centers for Disease Control and Prevention to The University of Utah. It was also supported by using resources and facilities at the VA Greater Los Angeles Healthcare System and the VA Salt Lake City Health Care System. In addition, M. J. was supported by a Department of Veterans Affairs Career Development Award (CDA 10-030-02).
Appendix A.
Questions: Antibiotic Timeout Focus Group
Tell me about your experience with the Antibiotic Timeout system?
How did the Antibiotic Timeout system influence your decision making?
What did you find useful about the Antibiotic TimeOut system?
What was not useful?
How was the interaction with the system and its features?
How did the system impact your decisions?
Do you think this system should be implemented throughout VA?
What could be done to improve the system technically?
What could be done to improve the system impact on clinical reasoning?
How important are other peoples’ opinions to your willingness to adopt use of this system?
What barriers to adoption do you see?
What would facilitate adoption of the system?
Appendix B. Sample view of the antibiotic renewal template
Footnotes
Conflict of interest
No conflicts.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Centers for Disease Control and Prevention, Department of Veterans Affairs, the US government or any of the affiliated institutions.
References
- [1].McGowan JE Jr., Antimicrobial resistance in hospital organisms and its relation to antibiotic use, Rev. Infect. Dis. 5 (1983) 1033–1048. [DOI] [PubMed] [Google Scholar]
- [2].Huttner A, Harbarth S, Carlet J, et al. , Antimicrobial resistance: a global view from the 2013 World Healthcare-Associated Infections Forum, Antimicrob. Resist. Infect. Control 2 (2013) 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2013. [Google Scholar]
- [4].Chan M, Combat Drug Resistance: No Action Today, No Cure Tomorrow, World Health Organization, 2011. [Google Scholar]
- [5].Davey P, Brown E, Charani E, et al. , Interventions to improve antibiotic prescribing practices for hospital inpatients, Cochrane Database Syst. Rev. 4 (2013). CD003543. [DOI] [PubMed] [Google Scholar]
- [6].Lee TC, Frenette C, Jayaraman D, et al. , Antibiotic self-stewardship: traineeled structured antibiotic time-outs to improve antimicrobial use, Ann. Intern. Med. 161 (2014) S53–S58. [DOI] [PubMed] [Google Scholar]
- [7].Srinivasan A, Let’s Take an Antibiotic Time Out, <http://blogs.cdc.gov/safehealthcare/?p=1026> (accessed 05.03.13).
- [8].Marquet K, Liesenborgs A, Bergs J, et al. , Incidence and outcome of inappropriate in-hospital empiric antibiotics for severe infection: a systematic review and meta-analysis, Crit. Care 19 (2015) 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kollef MH, Broad-spectrum antimicrobials and the treatment of serious bacterial infections: getting it right up front, Clin. Infect. Dis. 47 (Suppl 1) (2008) S3–S13. [DOI] [PubMed] [Google Scholar]
- [10].American Thoracic S, Infectious diseases society of A. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia, Am. J. Respir. Crit. Care Med. 171 (2005) 388–416. [DOI] [PubMed] [Google Scholar]
- [11].Lesprit P, Duong T, Girou E, et al. , Impact of a computer-generated alert system prompting review of antibiotic use in hospitals, J. Antimicrob. Chemother. 63 (2009) 1058–1063. [DOI] [PubMed] [Google Scholar]
- [12].Manuel O, Burnand B, Bady P, et al. , Impact of standardised review of intravenous antibiotic therapy 72 hours after prescription in two internal medicine wards, J. Hosp. Infect. 74 (2010) 326–331. [DOI] [PubMed] [Google Scholar]
- [13].Lesprit P, Landelle C, Brun-Buisson C, Clinical impact of unsolicited post-prescription antibiotic review in surgical and medical wards: a randomized controlled trial, Clin. Microbiol. Infect. 19 (2013) E91–E97. [DOI] [PubMed] [Google Scholar]
- [14].Cosgrove SE, Patel A, Song X, et al. , Impact of different methods of feedback to clinicians after postprescription antimicrobial review based on the Centers For Disease Control and Prevention’s 12 Steps to Prevent Antimicrobial Resistance Among Hospitalized Adults, Infect. Control Hosp. Epidemiol.: Off. J. Soc. Hosp. Epidemiol. Am. 28 (2007) 641–646. [DOI] [PubMed] [Google Scholar]
- [15].Cosgrove SE, Seo SK, Bolon MK, et al. , Evaluation of postprescription review and feedback as a method of promoting rational antimicrobial use: a multicenter intervention, Infect. Control Hosp. Epidemiol.: Off. J. Soc. Hosp. Epidemiol. Am. 33 (2012) 374–380. [DOI] [PubMed] [Google Scholar]
- [16].Delory T, De Pontfarcy A, Emirian A, et al. , Impact of a program combining pre-authorization requirement and post-prescription review of carbapenems: an interrupted time-series analysis, Eur. J. Clin. Microbiol. Infect. Dis. 32 (2013) 1599–1604. [DOI] [PubMed] [Google Scholar]
- [17].Cabana MD, Rand CS, Powe NR, et al. , Why don’t physicians follow clinical practice guidelines? A framework for improvement, JAMA, J. Am. Med. Assoc. 282 (1999) 1458–1465. [DOI] [PubMed] [Google Scholar]
- [18].Hulscher ME, Grol RP, van der Meer JW, Antibiotic prescribing in hospitals: a social and behavioural scientific approach, Lancet Infect. Dis. 10 (2010) 167–175. [DOI] [PubMed] [Google Scholar]
- [19].Stach L, Hedican E, Herigon J, et al. , Clinicians’ attitudes towards an antimicrobial stewardship program at a children’s hospital, J. Pediat. Infect. Dis. Soc. 1 (2012) 190–197. [DOI] [PubMed] [Google Scholar]
- [20].Srinivasan A, Song X, Richards A, et al. , A survey of knowledge, attitudes, and beliefs of house staff physicians from various specialties concerning antimicrobial use and resistance, Arch. Intern. Med. 164 (2004) 1451–1456. [DOI] [PubMed] [Google Scholar]
- [21].Cotta M, Robertson M, Tacey M, et al. , Attitudes towards antimicrobial stewardship: results from a large private hospital in Australia, Healthc. Infect. 19 (2014) 89–94. [Google Scholar]
- [22].Davis R, Campbell R, Hildon Z, et al. , Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review, Health Psychol. Rev. (2014) 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Norman GR, Eva KW, Diagnostic error and clinical reasoning, Med. Educ. 44 (2010) 94–100. [DOI] [PubMed] [Google Scholar]
- [24].Croskerry P, Clinical cognition and diagnostic error: applications of a dual process model of reasoning, Adv. Health Sci. Educ.: Theory Pract. 14 (Suppl 1) (2009) 27–35. [DOI] [PubMed] [Google Scholar]
- [25].Kahneman D, Thinking, Fast and Slow, Farrar, Straus and Giroux, New York, 2013. [Google Scholar]
- [26].Graber C, Jones M, Glassman P, et al. , Taking an antibiotic time-out: utilization and usability of a self-stewardship time-out program for renewal of vancomycin and piperacillin-tazobactam, Hosp. Pharm. 50 (2015) 1011–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Meeker D, Knight TK, Friedberg MW, et al. , Nudging guideline-concordant antibiotic prescribing: a randomized clinical trial, JAMA Int. Med. 174 (2014) 425–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Morgan D, Focus Groups as Qualitative Research, Sage, Thousand Oaks, London, New Delhi, 1997. [Google Scholar]
- [29].Krueger R, Casey M, Focus Groups: A Practical Guide for Applied Research, Sage, Thousand Oaks, London, New Delhi, Singapore, 2000. [Google Scholar]
- [30].Hsieh HF, Shannon SE, Three approaches to qualitative content analysis, Qual. Health Res. 15 (2005) 1277–1288. [DOI] [PubMed] [Google Scholar]
- [31].Patton M, Qualitative Research & Evaluation Methods, third ed., Sage, Thousand Oaks, CA, 2002. [Google Scholar]
- [32].Morgan DL, Focus Groups as Qualitative Research/Morgan David L., Sage Publications, Thousand Oaks, Calif, 1997. [Google Scholar]
- [33].Fransen ML, Smit EG, Verlegh PW, Strategies and motives for resistance to persuasion: an integrative framework, Front Psychol. 6 (2015) 1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Thaler RH, Sunstein CR, Nudge: Improving Decisions about Health, Wealth, and Happiness, Penguin Books, New York, 2009. [Google Scholar]
- [35].Livorsi D, Comer A, Matthias MS, et al. , Factors influencing antibiotic-prescribing decisions among inpatient physicians: a qualitative investigation, Infect. Control Hosp. Epidemiol. 36 (2015) 1065–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]