Abstract
Small bowel obstruction (SBO) is common surgical presenting problem, accounting for roughly 15 000 laparotomies per year in the UK. However, SBO post laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair is uncommon with an estimated incidence of 0.2%–0.5%. The common causes for SBO post-TAPP include inadequate closure, port-site herniation and adhesions. Here, we present a case of adhesional SBO related to stapling device from previous laparoscopic inguinal hernia repair and review alternative methods for mesh fixation. This case reports a rare but life-threatening complication from a commonly performed day case procedure and highlights importance of adequate surgical technique when inserting foreign bodies intra-abdominally. The patient required an emergency laparotomy and small bowel resection, developed postoperative ileus which managed with a nasogastric tube, intravenous fluids and parenteral nutrition and was discharged 12 days postoperatively.
Keywords: gastrointestinal surgery, general surgery, surgery
Background
Small bowel obstruction (SBO) is common surgical presenting problem, accounting for roughly 15 000 laparotomies per year in the UK.1 It usually multifactorial, with high risk factors being hernia, previous surgery causing adhesions, inflammatory bowel disease and malignancy.2 SBO is associated with significant morbidity and a 30-day operative mortality rate of almost 15%.1 3
Non-operative management consists of fluid resuscitation and bowel decompression with nasogastric (NG) drainage. Administration of water-soluble contrast agent has been demonstrated to have therapeutic efficacy4 and also offers prognostic information on those patients unlikely to resolve with conservative management. Risk factors for requiring early operative management include closed loop obstruction, evidence of ischaemia on CT, high grade obstruction, recurrent SBO, abdominal tenderness, tachycardia and feculent NG aspirate.5
Laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair is common day case procedure with a low complication rate. SBO postlaparoscopic TAPP is uncommon and this is usually secondary to inadequate closure, port-site herniation and adhesions.
Here we present a case of SBO secondary an adhesion caused by tack placed at a recent laparoscopic TAPP inguinal hernia repair peritoneum in accordance with Surgical Case Report (SCARE) criteria6 and discuss alternatives to the use of tack for fixation of the mesh into the peritoneum. The patient required an emergency laparotomy and small bowel resection and therefore it highlights the of adequate surgical technique when inserting foreign bodies intra-abdominally.
Case presentation
A 79-year-old man with a medical history of glaucoma and recent laparoscopic inguinal hernia repair presented to the emergency department with abdominal pain and vomiting. The patient was triaged to the resuscitation room as he appeared was septic with a temperature of 35°C (range: 36°C–38°C), white cell count of 16×109/L (range: 4–11×109/L) and lactate of 6.4 mmol/L (range: 0.6–1.4 mmol/L). On examination, the patient was cold, peripherally shut down with a delayed capillary refill time; the abdomen was tender with peritonism without distension. A Focused Assessment for Sonography in Trauma (FAST)scan demonstrated normal calibre aorta and some intra-abdominal free fluid.
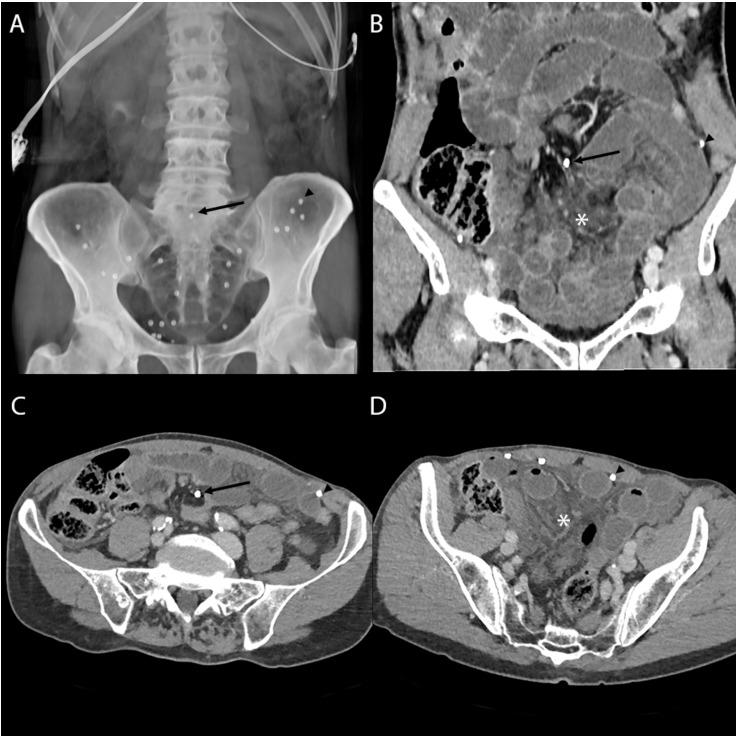
A urinary catheter was placed, and NG drainage established together with administration of intravenous fluid resuscitation and intravenous antibiotics. CT of abdomen and pelvis demonstrated SBO with closed loop and transition points along the vascular pedicle, suspicious for an internal hernia, band adhesion or volvulus (see figure 1). Furthermore, there was marked oedema of the associated mesentery and compression of the superior mesenteric vein at the site of transition and poorly enhancing small bowel loops indicating ischaemia.
Figure 1.
CT: Preoperative CT abdomen and pelvis with intravenous contrast. (A) Volume reformat showing distribution of normally positioned tack staples (arrowhead) and the displaced tack (arrow). (B) Coronal reformat showing the displaced tack (arrow) and the resultant dilated small bowel loops with congested mesentery (asterisk). (C) Axial slice at the level of the displaced tack (arrow). (D) Axial slice through the obstructed small bowel.
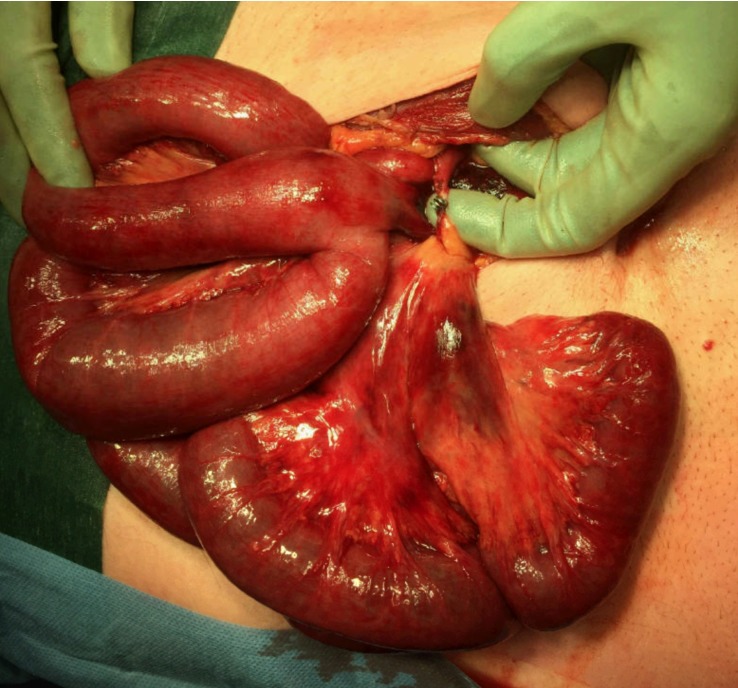
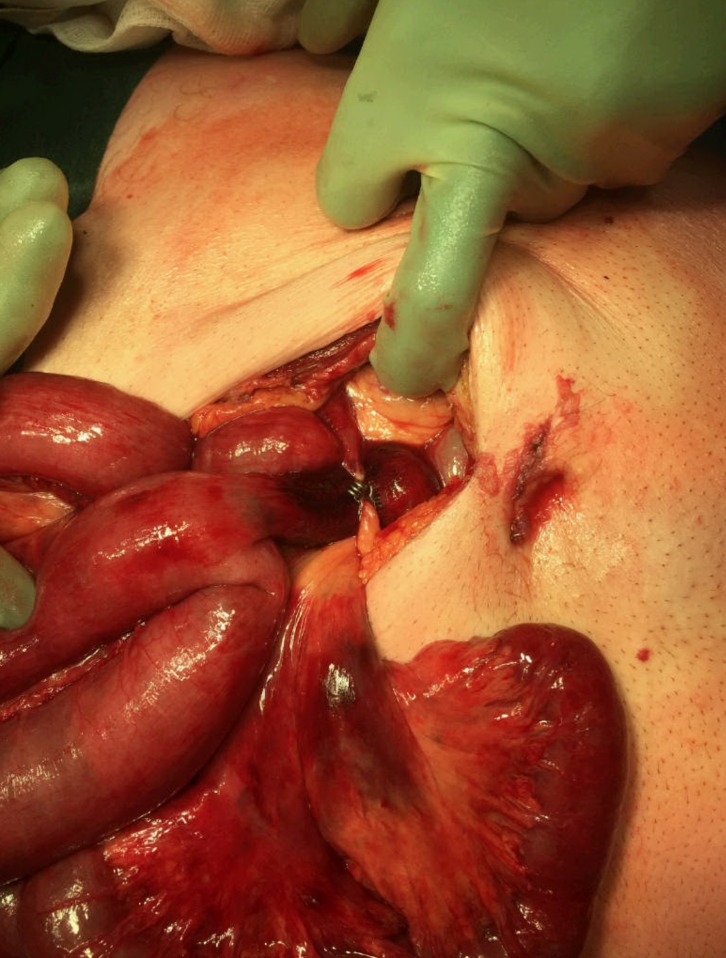
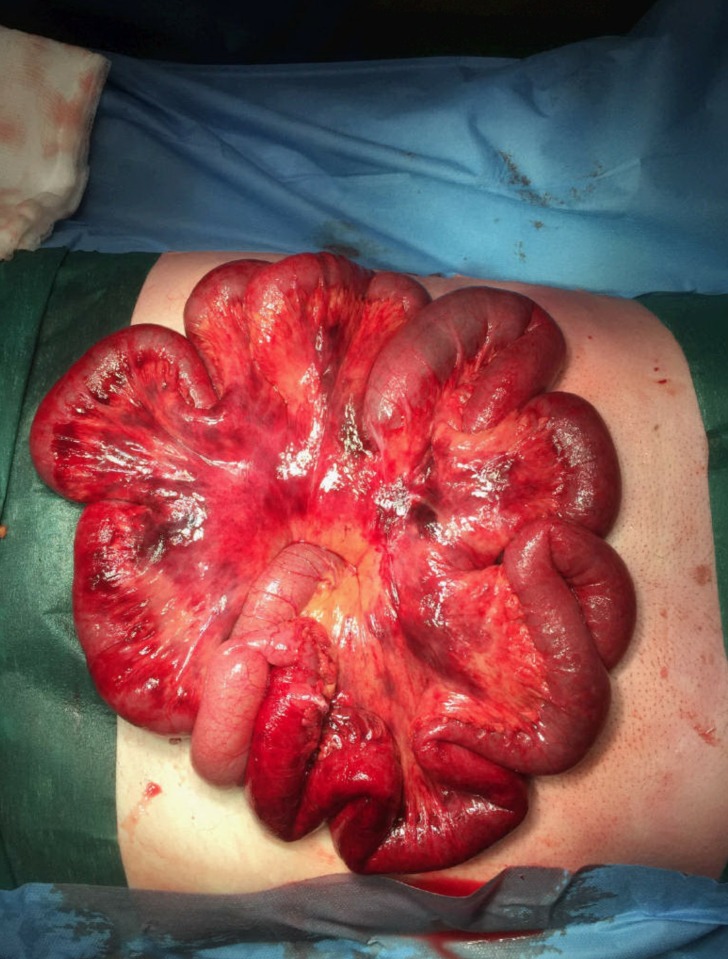
Based on clinical and radiological findings, emergency laparotomy was recommended, and informed consent obtained. Intraoperatively, a ProTack (Medtronic) from previous laparoscopic TAPP inguinal hernia repair was the cause for the adhesion (see figure 2). In addition, a Meckel’s diverticulum was also intimately related with the band adhesion (see figure 3). The single band adhesion was divided around the tack and the Meckel’s diverticulum excised. Although the small bowel was initially considered to have borderline viability, it recovered with warming and a period of observation (see figure 4). Postoperatively, the patient developed ileus which was successfully managed with an NG tube, intravenous fluids and parenteral nutrition. The patient was discharged home after 12 days.
Figure 2.
Intraoperative photography: misplaced laparoscopic tack from previous laparoscopic transabdominal preperitoneal inguinal hernia repair causing a band adhesion.
Figure 3.
Intraoperative photography: Meckel’s diverticulum under the band adhesion.
Figure 4.
Intraoperative photography: congested small bowel and oedematous bruised mesentery after band release.
Outcome and follow-up
Postoperatively, the patient developed ileus which was successfully managed with an NG tube, intravenous fluids and parenteral nutrition. The patient was discharged home after 12 days. Following discharge, patient was readmitted 10 days later with SBO which managed with NG tube and intravenous fluids. Since the readmission, patient has remained well without further hospital readmissions at 4 months.
Discussion
The overall complication rate of TAPP is low and it is estimated that the incidence of SBO after TAPP is between 0.2%–0.5%.7 SBO post-TAPP can be attributed to inadequate closure, port-site herniation and adhesional band formation postoperatively.7 As a result, we have only identified a few case reports case like ours where a retained staple during TAPP repairs caused mechanical small obstruction.7–9 Although uncommon, this case report highlights several important clinical learning points. First, the recognition of sepsis and the initial management with intravenous fluids and antibiotics by the emergency team. It is well known that early management of sepsis with intravenous crystalloid fluids and intravenous antibiotics within an hour of suspecting sepsis improves overall survival.10 Second, the identification that the source of sepsis as intra-abdominal requiring the involvement of surgical and radiology teams. Third, the recognition of SBO with signs of bowel ischaemia such as poorly enhancing bowel loops and oedema11 requiring early emergency surgery.
The national audit of small bowel obstruction study identified that evidence of ischaemia on CT and closed loop obstruction to be risk factors for early operative management5 and the national emergency laparotomy audit suggested that early operative management <72 hours is associated with a lower 30-day mortality,1 all of which were illustrated in this case.
TAPP is a commonly used technique for laparoscopic inguinal hernia repair.12 This technique involves placing a mesh in the preperitoneal plane to cover the defect at the myopectineal orifice.12 This technique is commonly used as it is quicker to learn than the totally extraperitoneal (TEP) technique and there is no difference in hernia recurrence rate.12 The TAPP technique has disadvantages of an overall low but higher risk of visceral injury and port-site herniation in comparison to TEP.12
Postoperative pain is a product of mesh fixation rather than the surgical technique employed in fixation.12–15 There are several methods of mesh fixation including tacks, staples, suture or fibrin, each with its own advantages and disadvantages.15 16 There are no well-designed appropriately powered randomised clinical trials comparing all the different methods for mesh fixation with appropriate long term follow-up.17
Some studies suggest that tack and staples are associated with increased pain, worse mobility and increased mesh sensation in comparison to suture.16 18 Several meta-analyses comparing outcomes of staple versus fibrin glue fixation showed no difference in hernia recurrence rates compared with staple/tack fixation, but decreased incidence of chronic inguinal pain and some suggested fibrin glue as the preferred technique.13 15–17 19 20
In addition, a large meta-analysis demonstrated that no mesh fixation in laparoscopic inguinal hernia repair does not increase the risk of hernia recurrence.14 It is comparable with tack mesh fixation in terms of operation time, postoperative pain, postoperative complications and length of hospital stay.14 Based upon the results of their study the authors suggested that no mesh fixation approach could be adopted routinely and safely in laparoscopic inguinal hernia repair.14
A recent study demonstrated that the use of fibrin was cheaper than the use of tack in their centre and they have therefore changed their practice and advocated the practice of using fibrin glue for mess fixation.21
Overall, the literature suggests that the use of tacks for mesh fixation is more expensive with a smaller but relative higher complication rate than other methods such as fibrin or suture.13 18 In this case report we have highlighted a very uncommon but significant life-threatening complication from the use of tack for fixation of mesh. The use of tack is likely to be technically easier and faster than suturing through the mesh. However one study suggest a faster operative time with fibrin glue when comparing it to tacks.21
In conclusion, fibrin glue or suture should be the preferred method for surgeons who are competent in these mesh fixation techniques. In cases where surgeons are not competent in laparoscopic suturing or using fibrin glue, the use of adhesive mesh can be used an alternative or a no fixation technique. If fixation with tack is required, surgeons should check that this is appropriately fixed to the abdominal wall and away from bowel or mesentery to avoid complications such as the one described in this case report.
Learning points.
An assessment of appropriate fixation of tack or staples during laparoscopic transabdominal preperitoneal (TAPP) should be advocated as any foreign body place in intra-abdominally can be adhesiogenic.
Surgeons should be encouraged to learn more than one appropriate mesh fixation techniques for laparoscopic TAPP inguinal hernia repair.
Early recognition of intra-abdominal sepsis and adequate resuscitation and the use of CT imaging allows for early intervention and management of bowel ischaemia secondary to adhesional obstruction.
Acknowledgments
Dr Vincent Leung (FRCR), who reported CT imaging, created figure 1 and also reviewed manuscript prior to publication.
Footnotes
Contributors: ANSS: wrote manuscript. EK: collected data and reviewed manuscript. NF: collected data and edited manuscript. JRM: operated on patient, collected photographs and reviewed manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Peacock O, Bassett MG, Kuryba A, et al. Thirty-day mortality in patients undergoing laparotomy for small bowel obstruction. Br J Surg 2018;105:1006–13. 10.1002/bjs.10812 [DOI] [PubMed] [Google Scholar]
- 2. Bower KL, Lollar DI, Williams SL, et al. Small Bowel Obstruction. Surg Clin North Am 2018;98:945–71. 10.1016/j.suc.2018.05.007 [DOI] [PubMed] [Google Scholar]
- 3. Teixeira PG, Karamanos E, Talving P, et al. Early operation is associated with a survival benefit for patients with adhesive bowel obstruction. Ann Surg 2013;258:459–65. 10.1097/SLA.0b013e3182a1b100 [DOI] [PubMed] [Google Scholar]
- 4. Choi HK, Chu KW, Law WL. Therapeutic value of gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment: a prospective randomized trial. Ann Surg 2002;236:1–6. 10.1097/00000658-200207000-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee MJ, Sayers AE, Wilson TR, et al. Current management of small bowel obstruction in the UK: results from the National Audit of Small Bowel Obstruction clinical practice survey. Colorectal Dis 2018;20:623–30. 10.1111/codi.14016 [DOI] [PubMed] [Google Scholar]
- 6. Agha RA, Fowler AJ, Saeta A, et al. The SCARE Statement: Consensus-based surgical case report guidelines. Int J Surg 2016;34:180–6. 10.1016/j.ijsu.2016.08.014 [DOI] [PubMed] [Google Scholar]
- 7. Fitzgerald HL, Orenstein SB, Novitsky YW. Small bowel obstruction owing to displaced spiral tack after laparoscopic TAPP inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 2010;20:e132–e135. 10.1097/SLE.0b013e3181dfbc05 [DOI] [PubMed] [Google Scholar]
- 8. Tagliaferri EM, Wong Tavara SL, Abad de Jesus JL, et al. Small bowel obstruction SBO after TAPP repair caused by a self-anchoring barbed suture device for peritoneal closure: case report. J Surg Case Rep 2018;2018:rjy165 10.1093/jscr/rjy165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Köhler G, Mayer F, Lechner M, et al. Small bowel obstruction after TAPP repair caused by a self-anchoring barbed suture device for peritoneal closure: case report and review of the literature. Hernia 2015;19:389–94. 10.1007/s10029-014-1301-1 [DOI] [PubMed] [Google Scholar]
- 10. Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013;41:580–637. 10.1097/CCM.0b013e31827e83af [DOI] [PubMed] [Google Scholar]
- 11. Furukawa A, Kanasaki S, Kono N, et al. CT diagnosis of acute mesenteric ischemia from various causes. AJR Am J Roentgenol 2009;192:408–16. 10.2214/AJR.08.1138 [DOI] [PubMed] [Google Scholar]
- 12. Jacob BP, Ramshaw B. Society of American Gastrointestinal Endoscopic Surgeons. The SAGES manual of hernia repair. New York: Springer, 2013:610. [Google Scholar]
- 13. Kaul A, Hutfless S, Le H, et al. Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc 2012;26:1269–78. 10.1007/s00464-011-2025-2 [DOI] [PubMed] [Google Scholar]
- 14. Sajid MS, Ladwa N, Kalra L, et al. A meta-analysis examining the use of tacker fixation versus no-fixation of mesh in laparoscopic inguinal hernia repair. Int J Surg 2012;10:224–31. 10.1016/j.ijsu.2012.03.001 [DOI] [PubMed] [Google Scholar]
- 15. Shah NS, Fullwood C, Siriwardena AK, et al. Mesh fixation at laparoscopic inguinal hernia repair: a meta-analysis comparing tissue glue and tack fixation. World J Surg 2014;38:2558–70. 10.1007/s00268-014-2547-6 [DOI] [PubMed] [Google Scholar]
- 16. Ross SW, Oommen B, Kim M, et al. Tacks, staples, or suture: method of peritoneal closure in laparoscopic transabdominal preperitoneal inguinal hernia repair effects early quality of life. Surg Endosc 2015;29:1686–93. 10.1007/s00464-014-3857-3 [DOI] [PubMed] [Google Scholar]
- 17. Shi Z, Fan X, Zhai S, et al. Fibrin glue versus staple for mesh fixation in laparoscopic transabdominal preperitoneal repair of inguinal hernia: a meta-analysis and systematic review. Surg Endosc 2017;31:527–37. 10.1007/s00464-016-5039-y [DOI] [PubMed] [Google Scholar]
- 18. Ayiomamitis GD, Zaravinos A, Stathakis PC, et al. Tacks-free transabdominal preperitoneal (TAPP) inguinal hernioplasty, using an anatomic 3-dimensional lightweight mesh with peritoneal suturing: pain and recurrence outcomes-initial experience. Surg Laparosc Endosc Percutan Tech 2013;23:e150–e155. 10.1097/SLE.0b013e31828b830d [DOI] [PubMed] [Google Scholar]
- 19. Sajid MS, Ladwa N, Kalra L, et al. A meta-analysis examining the use of tacker mesh fixation versus glue mesh fixation in laparoscopic inguinal hernia repair. Am J Surg 2013;206:103–11. 10.1016/j.amjsurg.2012.09.003 [DOI] [PubMed] [Google Scholar]
- 20. Li J, Ji Z, Zhang W. Staple Fixation Against Adhesive Fixation in Laparoscopic Inguinal Hernia Repair: A Meta-Analysis of Randomized Controlled Trials. Surg Laparosc Endosc Percutan Tech 2015;25:471–7. 10.1097/SLE.0000000000000214 [DOI] [PubMed] [Google Scholar]
- 21. Connolly M, Connolly M, Ramirez MG. Cost comparison of fibrin sealant versus tack screws for mesh fixation in laparoscopic repair of inguinal hernia. Hosp Pract 2018;46:233–7. 10.1080/21548331.2018.1500369 [DOI] [PubMed] [Google Scholar]