Abstract
We present a case of a 16-year-old girl with interruption of papyracea lamina and herniation of the periorbital fat covered by a bone shell. The patient presents with a history of diplopia and visual disturbances ever since she can remember. Thanks to radiological imaging and biopsy, we have done differential diagnosis with periorbital lipoma, intraosseous lipoma and intramuscular lipoma of medial rectus. Diagnostic for images is necessary for a correct operative planning. Endoscopic sinus surgery with computer-assisted navigation is the safest and most effective method to remove the lesion that was closely related to the medial rectum muscle and to the anterior ethmoidal artery. The patient after surgery and in 1 year of follow-up reports the disappearance of symptoms.
Keywords: ear, nose and throat/otolaryngology; ophthalmology
Background
This report describes the management of a woman with a rare periorbital fat lesion covered by a bone shell, which required medical and surgical collaboration among radiologists, otolaryngologists and ophthalmologists. This lesion is caused by a spontaneous solution of continuity of the papyracea lamina with periorbital fat herniation. Periorbital fat lesions are often associated to lipoma.
Lipomas are circumferential neoformations of mature fat that behave like an independent mass that grows and moves, rather than infiltrates, surrounding tissues. Periorbital lipomas and his variants are very special occurrences in the orbital region.1
Benign lipomas are very not frequent in the orbital region despite the presence of periorbital and retro bulbar fat with an incidence of 0.6%. It is possible that many of these cases were not true lipomas and may have represented orbital fat, as in our case.2 The aim of this paper is to present the correct management and treatment of this exceptionally rare and difficult case.
Case presentation
We present the case of a woman of 16 years with a family history of diabetes, hypertension and adeno-tonsillar surgery.3 The patient suffers from a slight mental retardation that makes the description of subjective symptoms more difficult4–7 and congenital hypothyroidism.8–11 The patient presents with a history of diplopia and visual disturbances ever since she can remember. The ophthalmological examination shows a right eye strabismus, stereopsis absent, oblique lower left eye hyper functioning. The patient arrives in our department of otorhinolaryngology after performing a CT study in the paediatric unit that highlights the presence of a left etmoid-orbitary formation. At rhinofibroscopy: norm trophic turbinates, absence of lesions in the nasal cavities, norm conformated rhino pharyngeal cavity. On the vestibular examination, the patient reports isolated sensations of disequilibrium, does not report vertigo, negative manoeuvres for benign paroxysmal positional vertigo.12
Investigations
The CT study shows a neoformation that protrudes in left ethmoid through a solution of continuity of the papyracea lamina. This lesion medially stretches the medial rectus muscle (figure 1). The relief appears compatible with dermoid cyst or lipoma.
Figure 1.
Coronal plane of the CT skull that highlights a neoformation that protrudes in left ethmoid through a solution of continuity of the papyracea lamina.
We decide to deepen the radiological study with vascular CT and MRI with gadolinium, for a better investigation and a correct operative planning.
The vascular CT study documents the presence of a thin vascular structure, probably arterial, not dissociable from the external, intraorbital profile of the known left ethmoidal lesion.
The presence of an accessory supraorbital cell on the left is associated, a relief that makes further plausible the fact that the described vascular structure can be represented precisely by the anterior ethmoidal artery. Anatomical contiguity is noted on the medial and superior sides of the known lesion with the region of the olfactory fossae on the left.
The MRI study shows the presence of an oval morphology formation, 18×9 mm in size, in correspondence with some ethmoid cells on the left. This lesion presents signal intensities in the T1 sequences. The lesion remains hyper intense both in the scans acquired with the adipose signal cancellation technique and in the T2 sequences. There is no restriction of the diffusivity of the water molecules.
The described lesion is in close relationship with the medial wall of the ipsilateral orbit.
The described relief appears compatible with cystic lesion characterised by fluid content with high protein concentration or mucosal-blood content (figure 2).
Figure 2.
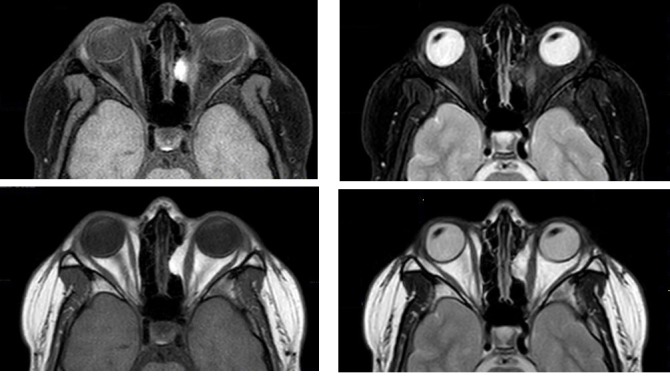
Axial plane of MRI skull that highlights the presence of an oval morphology formation, 18×9 mm in size, in correspondence with some ethmoid cells on the left, on T1-weighted and T2-weighted imagings with and without adipose signal cancellation.
Treatment
Endoscopic sinus surgery (ESS) is performed with computer-assisted navigation (CAN).13 CAN is an important support in the most complex cases of endoscopic surgery, for example, cranial malformation, invasive tumours, inverted papillomas, extraneous bodies, reinterventions.14–16 We decided to treat the lesion with CAN support and with an ophthalmologist in the operating room because the periorbital lesion is closely related to the medial rectum and to the anterior ethmoidal artery. Surgery was performed under general anaesthesia. Uncinectomy is performed with medium meatotomy and opening of the bulla etmoidalis. We proceed with opening of the large agger nasi cell and identification of the frontal recess. The region of the suspected neoformation is enclosed in a bone shell. Bone portion is removed with exposure of a periorbital fat lesion that is taken for histological study. The ophthalmologist in the operating room advises us not to be too aggressive in removing the lesion to avoid damaging the medial rectum.
Outcome and follow-up
The patient after the operation reports the disappearance of diplopia and visus disorders. Histological examination showed the lipid nature of the lesion. The patient performs follow-up after 1 month with MRI study and ophthalmological examination. At the MRI study with gadolinium, the disappearance of the previously known lesion with respect of the medial rectus muscle is documented. Ocular motility and visual field in the norm. We performed a radiological follow-up with an eye examination after 6 months, all the tests carried out were normal. We also recommended an eye examination with a study of ocular motility and visual field each year with radiological study in the event of ocular symptomatology.
Discussion
In the literature are not described cases of spontaneous interruption of papyracea lamina with herniation of the periorbital fat. This injury was probably caused by a frontal-ethmoid sinusitis in early age, with rupture of the papyracea lamina and rearrangement of the adjacent bone cells.
The particularity of this case is the doubtful radiological interpretation (cystic lesion with fluid content of serous-proteic or mucosal-hematic nature, dermoid cyst or lipoma). The adipose nature of the lesion was defined only after excision and histological study.
This type of lesion is in differential diagnosis with periorbital lipoma, intraosseous lipoma and intramuscular lipoma of medial rectus.
Orbital lipomas are well circumscribed and arise mainly from the anterior orbit; they are frequently clinically palpable before the occurrence of possible exophthalmos. They show gradual growth and are asymptomatic; they manifest chronic mass effect on adjacent structures where they are quite large. Lipomas are independent masses that grow and move, rather than infiltrates, surrounding tissues.17 18 In our case, the mass is not well circumscribed and has relationships that are too tight with the surrounding structures to be a lipoma.
Intraosseous lipomas are even very rarer and represent proliferation of the fat tissue within the marrow of normal trabecular bone. They represent 0.08% of all bone tumours. They have been reported in fronto-ethmoidal sinuses. Intraosseous lipomas contain a mixture of adipose tissue, lamellar and woven bone. Central calcification and a thick rim of surrounding sclerosis have low signal intensity on T1-weighted and T2-weighted sequences.19 20 In our case, the neoformation does not contain within the lamellar bone or signs of calcification, but it is covered externally by a bone shell.
Intramuscular lipomas primarily occur in the large muscles of the trunk and limbs and represent about 1.8% of all lipomatous lesions. The head and neck are very rare sites of occurrence. They differ histologically from typical lipomas in that they infiltrate the skeletal muscle and are associated with significant muscle fibres atrophy. The resulting tumour mass thus incorporates interspersed degenerated fibres bundles amidst the mature lipocytes.21 In our case, on biopsy it is not indicated the presence of muscle fibres analysed in adipose tissue.
On CT study, lipomas appear as low attenuation lesions, sometimes with a finely defined capsule, and have attenuation values between −20 and −120 Hounsfield units.22 On MRI, lipomas are hyper intense on T1-weighted imaging, and exhibits low signal intensity with fat suppression on T2-weighted images.2 In our case, the lesion remains hyper intense in the scans acquired with the adipose signal cancellation technique probably due to the presence of residues of an old phlogistic process.
The development of ESS has lead the surgeon to remove sinus-nasal pathologies endoscopically, extending the indications of a purely endoscopic approach to include benign and malignant tumours.23–25 We preferred endoscopic resection for removal of the mass with the support of CAN to avoid damaging the medial rectum and anterior ethmoid artery, in close relationship with the lesion.26 27
Learning points.
This is a case of interruption of papyracea lamina with herniation of the periorbital fat covered by a bone shell. Thanks to radiological imaging and biopsy, we have done differential diagnosis with periorbital lipoma, intraosseous lipoma and intramuscular lipoma of medial rectus.
Diagnostic for images is necessary for a correct operative planning.
Endoscopic sinus surgery with computer-assisted navigation is the safest and most effective method to remove the lesion that was in close relationship with the medial rectum muscle and with the anterior ethmoidal artery.
Footnotes
Contributors: BG developed the concept and design of the study and treated the patient. FGazia is corresponding author, was preparing the manuscript. CG performed follow-up examinations and literature research. FGalletti critically revised the manuscript for important intellectual content and gave the final approval of the version to be submitted.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. Rootman J. Diseases of the orbit: a multidisciplinary approach. 2nd ed Philadelphia: Lippincott Williams & Wilkins, 2003:54–62. 270. [Google Scholar]
- 2. Shah NB, Chang WY, White VA, et al. . Orbital lipoma: 2 cases and review of literature. Ophthalmic Plast Reconstr Surg 2007;23:202–5. 10.1097/IOP.0b013e318050ca52 [DOI] [PubMed] [Google Scholar]
- 3. Motta G, Motta S, Cassano P, et al. . Effects of guidelines on adeno-tonsillar surgery on the clinical behaviour of otorhinolaryngologists in Italy. BMC Ear Nose Throat Disord 2013;13:13:1 10.1186/1472-6815-13-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Naro A, Leo A, Bruno R, et al. . Reducing the rate of misdiagnosis in patients with chronic disorders of consciousness: Is there a place for audiovisual stimulation? Restor Neurol Neurosci 2017;35:511–26. 10.3233/RNN-170741 [DOI] [PubMed] [Google Scholar]
- 5. Gazia F, Abita P, Alberti G, et al. . NICU Infants & SNHL: Experience of a western Sicily tertiary care centre. Acta Medica Mediterranea 2019;35:1001–7. [Google Scholar]
- 6. Naro A, Bruno R, Leo A, et al. . Twist and turn into chronic disorders of consciousness: Potential role of the auditory stapedial reflex. Restor Neurol Neurosci 2017;35:77–85. 10.3233/RNN-160655 [DOI] [PubMed] [Google Scholar]
- 7. Leo A, Naro A, Cannavò A, et al. . Could autonomic system assessment be helpful in disorders of consciousness diagnosis? A neurophysiological study. Exp Brain Res 2016;234:2189–99. 10.1007/s00221-016-4622-8 [DOI] [PubMed] [Google Scholar]
- 8. Bruno R, Aversa T, Catena M, et al. . Even in the era of congenital hypothyroidism screening mild and subclinical sensorineural hearing loss remains a relatively common complication of severe congenital hypothyroidism. Hear Res 2015;327:43–7. 10.1016/j.heares.2015.04.018 [DOI] [PubMed] [Google Scholar]
- 9. Galletti B, Bruno R, Catalano N, et al. . Follicular carcinoma on a radio-treated ectopic lingual thyroid. Chirurgia 2016;29:88–91. [Google Scholar]
- 10. Freni F, Galletti B, Galletti F, et al. . Improved outcomes for papillary thyroid microcarcinoma care: active surveillance and case volume. Ther Adv Endocrinol Metab 2018;9:185–6. 10.1177/2042018818773609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sun H, Zanghì GN, Freni F, et al. . Continuous and intermitted nerve monitoring in thyroid surgery: two complementary devices. Gland Surg 2018;7(Suppl 1):S80–S81. 10.21037/gs.2018.02.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ciodaro F, Mannella VK, Nicita RA, et al. . Therapeutic efficacy of the Galletti-Contrino manoeuvre for benign paroxysmal positional vertigo of vertical semicircular canals in overweight subjects. Eur Arch Otorhinolaryngol 2018;275:2449–55. 10.1007/s00405-018-5086-1 [DOI] [PubMed] [Google Scholar]
- 13. Galletti B, Gazia F, Freni F, et al. . Endoscopic sinus surgery with and without computer assisted navigation: A retrospective study. Auris Nasus Larynx 2018. 10.1016/j.anl.2018.11.004 [DOI] [PubMed] [Google Scholar]
- 14. Galletti F, Cammaroto G, Galletti B, et al. . Technetium-99m (⁹⁹mTc)-labelled sulesomab in the management of malignant external otitis: is there any role? Eur Arch Otorhinolaryngol 2015;272:1377–82. 10.1007/s00405-014-2938-1 [DOI] [PubMed] [Google Scholar]
- 15. Freni F, Galletti B, Bruno R, et al. . Multidisciplinary approach in the removal of post-trauma foreign bodies in the head and neck district: Cases report and review of literature. Acta Medica Mediterranea 2019;35:405–10. [Google Scholar]
- 16. Galletti B, Mannella VK, Santoro R, et al. . Ear, nose and throat (ENT) involvement in zoonotic diseases: a systematic review. J Infect Dev Ctries 2014;8:17–23. 10.3855/jidc.4206 [DOI] [PubMed] [Google Scholar]
- 17. Koganei Y, Ishikawa S, Abe K, et al. . Orbital lipoma. Ann Plast Surg 1988;20:173–82. 10.1097/00000637-198802000-00017 [DOI] [PubMed] [Google Scholar]
- 18. Poweleit AC. Congenital lipoma of the orbit. J Ky Med Assoc 1978;76:20. [PubMed] [Google Scholar]
- 19. Lanisnik B, Didanovic V. Sphenoclival intraosseus lipoma: case report and literature review. Skull Base 2007;17:211–4. 10.1055/s-2007-977462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Elsurer C, Hancı D, Cakir A, et al. . Isolated intraosseous lipoma of the ethmoid sinus. J Craniomaxillofac Surg 2013;41:718–20. 10.1016/j.jcms.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 21. Dutton JJ, Wright JD. Intramuscular lipoma of the superior oblique muscle. Orbit 2006;25:227–33. 10.1080/01676830600575519 [DOI] [PubMed] [Google Scholar]
- 22. Behrendt S, Werner JA, Jänig U. Lipoma of the orbit. Orbit 1996;15:101–4. 10.3109/01676839609150076 [DOI] [Google Scholar]
- 23. Sireci F, Martines F, De Bernardi F, et al. . Chapter 9: Canine Fossa Puncture for the Management of Maxillary Sinusitis Gilbert H, Handbook of Surgical Procedures: Nova publisher. [Google Scholar]
- 24. Ciodaro F, Freni F, Mannella VK, et al. . Use of 3D Volume Rendering Based on High-Resolution Computed Tomography Temporal Bone in Patients with Cochlear Implants. Am J Case Rep 2019;20:184–8. 10.12659/AJCR.914514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Galletti B, Gazia F, Freni F, et al. . Chronic Otitis Media Associated with Cholesteatoma in a Case of the Say-Barber-Biesecker-Young-Simpson Variant of Ohdo Syndrome. Am J Case Rep 2019;20:175–8. 10.12659/AJCR.913893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sireci F, Martines F, Salvago P, et al. ; Complications and Their Management in Endoscopic Sinus Surgery (ESS) Gilbert H, ed Handbook of Surgical Procedures. Chapter 7; Nova publisher. [Google Scholar]
- 27. Sireci F, Speciale R, Sorrentino R, et al. . Nasal packing in sphenopalatine artery bleeding: therapeutic or harmful? Eur Arch Otorhinolaryngol 2017;274:1501–5. 10.1007/s00405-016-4381-y [DOI] [PubMed] [Google Scholar]



