Abstract
In addition to the TRANSFORMS, FREEDOMS, INFORMS studies, very few publications have identified new cases of skin cancer in patients treated with fingolimod. Here, we present the case of a 52-year-old Caucasian patient with relapsing remitting multiple sclerosis for 19 years, with a phototype II with blue eyes, light brown hair, no personal or family history of melanoma and a low number of naevi (<10). She did not experience intense sun exposure in childhood as well as severe sunburn and did not practise sessions in ultraviolet cabins. This case is distinguished from other published cases, usually superficial spreading malignant melanoma by its unclassifiable histological character. The occurrence of skin cancers in patients with multiple sclerosis remains exceptional, but new cases have recently emerged requiring the strengthening of dermatological follow-up of such patients.
Keywords: multiple sclerosis, dermatology, malignant disease and immunosuppression, neurology (drugs and medicines)
Background
In addition to the TRANSFORMS, FREEDOMS, INFORMS studies, very few publications have identified new cases of skin cancer in patients treated with fingolimod.
Case presentation
Here, we present the case of a 52-year-old Causasian patient with relapsing remitting multiple sclerosis for 19 years, with a phototype II with blue eyes, light brown hair, no personal or family history of melanoma and a low number of naevi (<10). She did not experience intense sun exposure in childhood as well as severe sunburn and did not practise sessions in ultraviolet cabins.
Investigations
This patient with multiple sclerosis has been treated with fingolimod 0.5 mg/day for 3 years following a therapeutic switch of natalizumab for positive seroconversion to John Cunningham virus. Two years later, she presented with a subcutaneous, mobile, nodular lesion of the scalp in the left parietal region. It had a bluish appearance and was non-pulsatile (figure 1). This lesion developed an inflammatory and painful character and a surgical excision was performed. The histological study showed a largely necrotic dermal tumour consisting of a cellular proliferation, positive after Fontana Masson staining. Immunohistochemistry showed positivity with PS100, HMB45 and Melan A, and total cytokeratin negativity. The diagnosis was a Clark Level IV unclassifiable malignant melanoma with a Breslow index of 13 mm (figure 2). Lymph node ultrasonography excluded lymph node involvement in the cervical and supraclavicular areas. Sentinel lymph node technique was done, the final clinical examination did not show a primary site or a sign of clinically regressing melanoma.
Figure 1.

Left parietal nodular cranial lesion.
Figure 2.
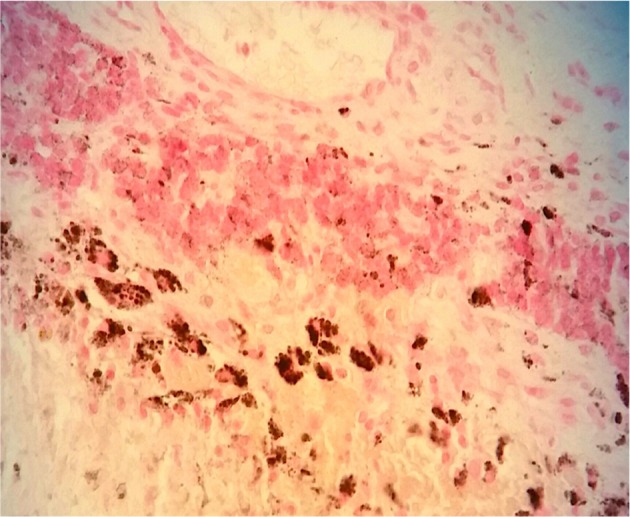
Fontana-Masson colouring which stains the melanic pigment in black in the necrosis and in the few perennial pink cells (×40).
Treatment
Treatment with fingolimod was stopped following this diagnosis, the patient did not present a relapse.
Outcome and follow-up
Ensure better dermatological screening of melanoma in patients treated with fingolimod with regular follow-up
Discussion
This case is distinguished from other published cases, usually superficial spreading malignant melanoma by its unclassifiable histological character.1 Although clinical trials or follow-up studies have not revealed any significant differences in the increase of cancers, especially melanomas, a large number of pharmacovigilance cases have been reported in recent years concerning almost all new oral or injectable molecules.2 3 The occurrence of skin cancers in patients with multiple sclerosis remains exceptional, but new cases have recently emerged requiring the strengthening of dermatological follow-up of such patients.
Cases of melanoma have been reported for galitramer, natalizumab (more than 100 cases), dimethyl fumarate, alemtuzumab or cladribine.2–6
The relationship between cancer and multiple sclerosis is very complex to establish, and there is no obvious relationship despite a chronic inflammatory character promoting the cancer risk in such patients. Tumour mechanisms are still poorly understood today and range between a decrease in general immune surveillance or a direct action on a specific receptor present on keratinocytes (fingolimod (SP1) or integrin α4β1 integrin for natalizumab).2 3
We can legitimately ask ourselves the question of the use of immunomodulatory molecules such as fingolimod continuously in such patients, because several studies have already revealed an increased incidence of melanomas or Merkel cell carcinoma in patients treated with immune suppressants.7 Patients with fingolimod should have enhanced dermatological monitoring to detect early this type of skin cancer and must be able to practise regular self-monitoring.
A pharmacovigilance statement was made by a community pharmacist for this case indicating their potential role in the monitoring of such treatments.2 3
Learning points.
Dermatological monitoring should be considered for patients treated with fingolimod.
Patients should be warned of the need for dermatological follow-up.
Patients can be educated to monitor possible melanoma.
Acknowledgments
I thank Professor Dalac, Dr D Michiels-Marzais, Dr A Bourdin, Dr J Berger, Dr Lebrun, Dr Voirin, Dr Guerin, Dr Guillaume for their contributions to this work.
Footnotes
Contributors: YM and OB are involved in conduct, reporting, conception and design of the study. J-FM and SM are involved in data analysis.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Killestein J, Leurs CE, Hoogervorst ELJ, et al. . Five cases of malignant melanoma during fingolimod treatment in Dutch patients with MS. Neurology 2017;89:970–2. 10.1212/WNL.0000000000004293 [DOI] [PubMed] [Google Scholar]
- 2. Sabol RA, Noxon V, Sartor O, et al. . Melanoma complicating treatment with natalizumab for multiple sclerosis: a report from the Southern Network on Adverse Reactions (SONAR). Cancer Med 2017;6:1541–51. 10.1002/cam4.1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lebrun C, Rocher F. Cancer risk in patients with multiple sclerosis: potential impact of disease-modifying drugs. CNS Drugs 2018;32:939–49. 10.1007/s40263-018-0564-y [DOI] [PubMed] [Google Scholar]
- 4. Pace AA, Zajicek JP. Melanoma following treatment with alemtuzumab for multiple sclerosis. Eur J Neurol 2009;16:e70–e71. 10.1111/j.1468-1331.2009.02552.x [DOI] [PubMed] [Google Scholar]
- 5. Haebich G, Mughal A, Tofazzal N. Superficial spreading malignant melanoma in a patient on fingolimod therapy for multiple sclerosis. Clin Exp Dermatol 2016;41:433–4. 10.1111/ced.12770 [DOI] [PubMed] [Google Scholar]
- 6. Conzett KB, Kolm I, Jelcic I, et al. . Melanoma occurring during treatment with fingolimod for multiple sclerosis: a case report. Arch Dermatol 2011;147:991–2. 10.1001/archdermatol.2011.212 [DOI] [PubMed] [Google Scholar]
- 7. Calvi A, De Riz M, Lecchi E, et al. . Merkel cell carcinoma in a patient with relapsing-remitting multiple sclerosis treated with fingolimod. J Neurol Sci 2017;381:296–7. 10.1016/j.jns.2017.09.003 [DOI] [PubMed] [Google Scholar]


