Abstract
The incidence of Lyme disease in the USA is 8 per 100 000 cases and 95% of those occur in the Northeastern region. Cardiac involvement occurs in only 1% of untreated patients. We describe the case of a 46-year-old man who presented with chest pressure, dyspnoea, palpitations and syncope. He presented initially with atrial fibrillation with rapid ventricular response, a rare manifestation of Lyme carditis. In another hospital presentation, he had varying degrees of atrioventricular block including Mobitz I second-degree heart block. After appropriate antibiotic treatment, he made a full recovery and his ECG normalised. The authors aim to urge physicians treating patients in endemic areas to consider Lyme carditis in the workup for patients with atrial fibrillation and unexplained heart block, as the associated atrioventricular nodal complications may be fatal.
Keywords: arrhythmias, pacing and electrophysiology, cardiovascular system, infections
Background
Lyme disease is the most commonly reported vector-borne disease in the USA, with an incidence of 8 cases per 100 000 persons per year and 95% of those occur in the Northeastern region.1 It is a tick-borne disease caused by the spirochete Borrelia burgdorferi. Acutely, clinical symptoms include fever, chills, weakness and the dermatological manifestation of erythema migrans at the site of the tick bite. Lack of timely diagnosis and treatment can increase the risk of dissemination causing arthritis, neuropathy and rarely carditis.
Lyme carditis occurs in 1% of untreated patients in the early disseminated phase of infection.1 Although the exact mechanism of cardiac tissue injury is not fully elucidated in Lyme carditis, in addition to direct myocardial invasion by Borrelia burgdorferi, there are also some studies that emphasise the influence of some immunological and autoimmunological processes.2 Cardiac manifestations can occur after a median of 21 days from the onset of exposure.3 Ninety per cent of Lyme carditis presents as high-degree atrioventricular block (AVB), whereas the other 10% is represented by myocarditis, pancarditis or other types of arrhythmias and conduction disorders.3 Typically, cardiac involvement leads to varying severities of first-degree AVB. Surveillance data indicate that patients less commonly present with second-degree or third-degree AVB.4 We herein describe a rare case of Lyme carditis presenting with atrial fibrillation as well as varying degrees of heart block including Mobitz I second-degree AVB.
Case presentation
A 46-year-old male avid hiker with no significant medical history presented to the emergency department with a 3-week history of constant, substernal chest pressure. His chest pain was described as a positional, non-radiating heaviness, improved by leaning forward. He reported dyspnoea on minimal exertion as well as intermittent palpitations and lightheadedness. He had multiple witnessed syncopal events that were occasionally sudden in onset and lasted for a few minutes before regaining consciousness. He had no allergies and was not taking any medications. His father suffered from myocardial infarction at the age of 49. He had a surgical history of lumbar fusion and cholecystectomy. He is married with two children and is unemployed. He is a non-smoker and drinks socially.
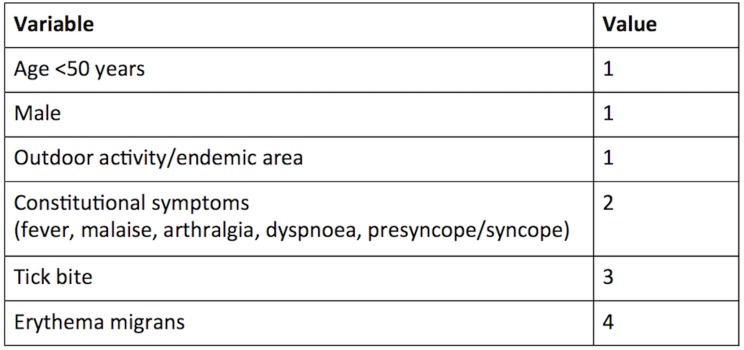
On physical examination, he was diaphoretic with an irregularly irregular tachycardia and a blood pressure of 151/76 mm Hg. His other vital signs including orthostatic blood pressures were normal. He had no murmurs, rubs or gallops. He had no jugular venous distension or oedema. His lungs were clear to auscultation. He did not exhibit any rashes or joint swelling. His ECG showed atrial fibrillation with rapid ventricular response (figure 1). Biochemical investigations including complete blood count, renal function, electrolytes, liver function tests, thyroid hormones and troponins were normal. His chest X-ray, CT pulmonary angiogram and echocardiogram were normal. Due to concerns for unstable angina and his significant family history, a coronary angiogram was performed which was normal.
Figure 1.
ECG showing atrial fibrillation with rapid ventricular response.
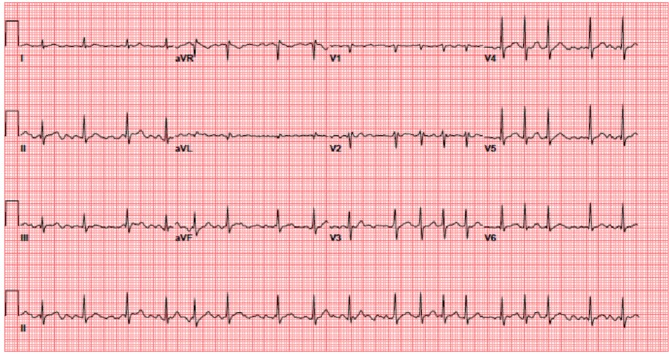
He reverted spontaneously to sinus rhythm with a PR interval of 200 ms (120–200) within 24 hours and was discharged on aspirin 81 mg once daily and Metoprolol tartrate 12.5 mg twice daily. In a cardiology follow-up visit, his symptoms had recurred. A repeat ECG on this second presentation revealed sinus rhythm and first-degree AVB with marked PR interval prolongation of 440 ms (figure 2). On reflection and further questioning, the patient recalled a large homogeneous erythematous leg rash that preceded his symptoms by 3 weeks. He had presented to his primary care physician at that time and was diagnosed with cellulitis and received a course of cephalexin of unknown duration.
Figure 2.

ECG showing first-degree heart block with a PR interval of 440 ms.
His metoprolol was discontinued and he was urgently admitted. On admission, his ECG showed second-degree Mobitz I AVB with 5:4 AV conduction (figure 3). His high-sensitivity C reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were 7.0 mg/L (1–3) and 21 mm/h (0–15), respectively. His Lyme C6 peptide was positive. A Western blot assay confirmed active Lyme disease. He was commenced on intravenous ceftriaxone 2 grams once daily.
Figure 3.
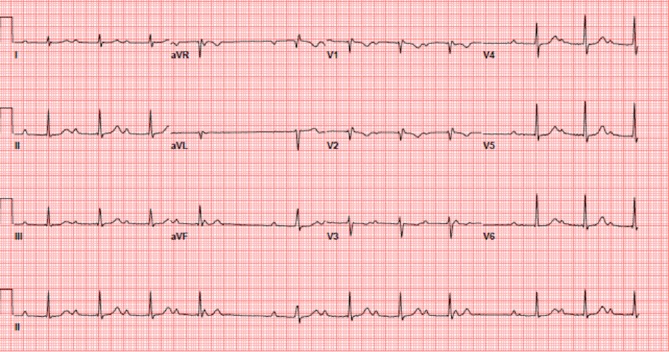
ECG showing Mobitz type I second-degree AV block with 5:4 AV conduction. AV, atrioventricular.
Outcome and follow-up
He was monitored closely on telemetry with daily ECGs. His repeat ECG within 24 hours showed improvement in the PR interval to 382 ms and subsequently to 345 ms by day 3. By day 4, his PR interval improved to <300 ms. He was unable to tolerate oral antibiotics secondary to gastritis. His aspirin was discontinued and pantoprazole 40 mg two times per day was started. Infectious disease advised completion of 3 weeks of intravenous ceftriaxone. A peripherally inserted central line was placed. Following completion of his antibiotics, he was seen at the cardiology outpatient clinic where he had complete resolution of his symptoms. His ECG revealed normal sinus rhythm with a PR interval of 156 ms (figure 4). His Holter monitor did not reveal any AVB or atrial fibrillation.
Figure 4.
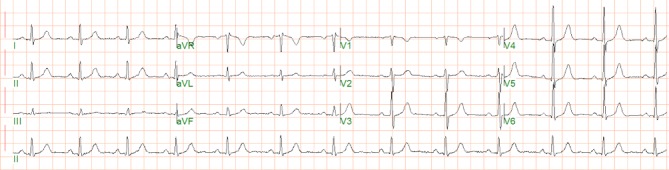
ECG showing normal sinus rhythm with a PR interval of 156msec.
Discussion
Lyme carditis is a rare complication of Lyme disease. All cases of Lyme disease are reportable to state and local health departments. Approximately 26 000 persons are diagnosed with Lyme disease in the USA each year.5 Rates of Lyme disease have increased disproportionately among young men for unknown reasons with a male predominance of 3 to 1.6 7
The cardiac conduction system is more frequently involved in Lyme carditis; however, the myocardium and pericardium can also be involved.8 Typically, patients experience palpitations, chest pain, dyspnoea and syncope. Hospitalisation is recommended for patients with first-degree AVB and a PR interval of >300 ms or those with second-degree or third-degree AVB as approximately one third of patients end up requiring temporary pacing.8 Prolonged QTc interval, sinus tachycardia, sinus bradycardia, asystolic pauses and other supraventricular tachyarrhythmias can occur.
Lyme disease is confirmed via two-tier testing.9 The first test is an enzyme immunoassay followed by western blot confirmatory assay. The more recent C6 peptide test is an alternative first step that identifies conserved peptide called C6, which is a component of the spirochete’s variable surface antigen VIsE1.9 If this test is positive or equivocal and the patient has had symptoms for ≤30 days, usually an IgM western blot is performed. If the patient has had symptoms for ≥30 days, an IgG western blot is performed.
According to the Centers for Disease Control and Prevention (CDC), approximately 40% of patients who develop Lyme carditis will have had the classical erythema migrans rash as compared with 70% of patients with other manifestations of Lyme disease.1 Some studies have found that in fact, <10% of patients present with a rash depicting central clearance but rather more commonly present with homogeneous erythema.10 This may have explained our patient’s misdiagnosis of cellulitis. Generally, the prognosis is great when appropriate antimicrobial treatment is commenced in a timely fashion with most achieving recovery within 1–2 weeks of initiation.8
Results of a systematic review in January 2019 of all published cases of Lyme carditis with high-degree AVB by Besant et al stimulated the development of a risk stratification tool called the Suspicious Index in Lyme Carditis (SILC) score utilising the acronym COSTAR (constitutional symptoms, outdoor activities, male sex, tick bite, age <50 and erythema migrans rash) (figure 5). Our patient’s calculated SILC score is 9 indicating a high likelihood for Lyme carditis.11
Figure 5.
The SILC score evaluates likelihood that high-degree heart block is caused by Lyme carditis (low (0–2); intermediate (3–6); high (7–12)). SILC, Suspicious Index in Lyme Carditis.
A rare number of cases surrounding young 20-year-old male patients have been described in the literature or anecdotally to present with atrial fibrillation, all of which had a favourable outcome after completion of antibiotic treatment.5 12 Varying degrees of AVB minutes to hours apart are also unusual such as in our patient who presented with atrial fibrillation, second-degree Mobitz I heart block and profound first-degree heart block. It has been hypothesised that these alterations may be due to dual AV node physiology where the antegrade block in the fast pathway causes abrupt PR prolongation, as described in one previous case report.12 Early recognition of reversible AVB caused by Lyme disease will likely avoid unnecessary permanent pacemaker use.8 Some patients with symptomatic high-degree AVB may require temporary pacing. The externalised temporary permanent pacemaker with temporary endocardial screw-in leads maintains superior stability and allows earlier patient mobilisation when compared with standard transvenous temporary pacemakers.13
For patients with an intermediate or high SILC score and high-degree AVB or other cardiac manifestations of Lyme carditis, empiric intravenous antibiotics should be administered immediately while serology is pending. Serologically confirmed Lyme disease should be treated with intravenous antibiotics for 14 days followed by oral antibiotics such as doxycycline for 4–6 weeks.14 For asymptomatic bradycardia on admission, cardiac monitoring is vital as patients can rapidly deteriorate and progress to complete AVB or asystole. Symptomatic bradycardia with high-risk ECG features such as alternating bundle branch block should receive externalised temporary permanent pacemaker.14
If 1:1 AV conduction is not restored by 14 days, then a permanent pacemaker is recommended which is removed when this is achieved.14 Guidelines suggest that if 1:1 AV conduction is restored within 14 days, then a pre-discharge stress test is recommended to assess the stability of AV conduction. If 1:1 AV conduction is maintained >120 beats/min, then the patient can be discharged on oral antibiotics and if conduction fails at <90 beats/min, then a permanent pacemaker is recommended.14 Outpatient ECG and clinical follow-up should be arranged within 4 weeks postdischarge to confirm the lack of rhythm or conduction abnormalities.
For physicians treating patients in endemic areas, Lyme carditis must be considered in the workup for patients with atrial fibrillation and unexplained heart block, as the associated AV nodal complications may be fatal.
Learning points.
Lyme carditis occurs in 1% of untreated patients.
In patients with unexplained heart block, atrial fibrillation or cardiac symptoms, physicians should enquire about possible exposure to tick bites.
Prompt recognition and early, appropriate antibiotic therapy for Lyme disease is essential.
Hospitalisation and intravenous antibiotics are recommended for patients with first-degree atrioventricular B and a PR interval of >300 ms or those with second-degree or third-degree heart block.
Patients must be monitored on cardiac telemetry, as temporary pacing may be required in one third of patients.
According to the Center for Disease Control and Prevention, approximately 40% of patients who develop Lyme carditis will have had the classical erythema migrans rash as compared with 70% of patients with other manifestations of Lyme disease.
A risk stratification tool called the Suspicious Index in Lyme Carditis score can be utilised in the workup of patients.
The externalised temporary permanent pacemaker with temporary endocardial screw-in leads maintains superior stability and allows earlier patient mobilisation.
Footnotes
Contributors: AZ: was the primary author for writing the case and discussion. AH, NN and MM: contributed to writing the case. DL and RH: edited the case report and were the senior physicians primarily responsible for the patient’s care.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. CDC. Lyme Disease. 2018. https://www.cdc.gov/lyme/datasurveillance/index.html
- 2. Raveche ES, Schutzer SE, Fernandes H, et al. Evidence of Borrelia autoimmunity-induced component of Lyme carditis and arthritis. J Clin Microbiol 2005;43:850–6. 10.1128/JCM.43.2.850-856.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rostoff P, Gajos G, Konduracka E, et al. Lyme carditis: epidemiology, pathophysiology, and clinical features in endemic areas. Int J Cardiol 2010;144:328–33. 10.1016/j.ijcard.2009.03.034 [DOI] [PubMed] [Google Scholar]
- 4. Forrester JD, Mead P. Third-degree heart block associated with lyme carditis: review of published cases. Clin Infect Dis 2014;59:996–1000. 10.1093/cid/ciu411 [DOI] [PubMed] [Google Scholar]
- 5. Kennel PJ, Parasram M, Lu D, et al. A case of lyme carditis presenting with atrial fibrillation. Case Rep Cardiol 2018;2018:1–5. 10.1155/2018/5265298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bacon RM, Kugeler KJ, Mead PS. Centers for Disease Control and Prevention (CDC). Surveillance for Lyme disease--United States, 1992-2006. MMWR Surveill Summ 2008;57:1–9. [PubMed] [Google Scholar]
- 7. Munk PS, Ørn S, Larsen AI. Lyme carditis: persistent local delayed enhancement by cardiac magnetic resonance imaging. Int J Cardiol 2007;115:e108–e110. 10.1016/j.ijcard.2006.05.068 [DOI] [PubMed] [Google Scholar]
- 8. Wan D, Blakely C, Branscombe P, et al. Lyme carditis and high-degree atrioventricular block. Am J Cardiol 2018;121:1102–4. 10.1016/j.amjcard.2018.01.026 [DOI] [PubMed] [Google Scholar]
- 9. Wormser GP, Schriefer M, Aguero-Rosenfeld ME, et al. Single-tier testing with the C6 peptide ELISA kit compared with two-tier testing for Lyme disease. Diagn Microbiol Infect Dis 2013;75:9–15. 10.1016/j.diagmicrobio.2012.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smith RP, Schoen RT, Rahn DW, et al. Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans. Ann Intern Med 2002;136:421–8. 10.7326/0003-4819-136-6-200203190-00005 [DOI] [PubMed] [Google Scholar]
- 11. Besant G, Wan D, Yeung C, et al. Suspicious index in Lyme carditis: Systematic review and proposed new risk score. Clin Cardiol 2018;41:1611–6. 10.1002/clc.23102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wenger N, Pellaton C, Bruchez P, et al. Atrial fibrillation, complete atrioventricular block and escape rhythm with bundle-branch block morphologies: an exceptional presentation of Lyme carditis. Int J Cardiol 2012;160:e12–e14. 10.1016/j.ijcard.2012.01.004 [DOI] [PubMed] [Google Scholar]
- 13. Wang C, Chacko S, Abdollah H, et al. Treating lyme carditis high-degree AV block using a temporary-permanent pacemaker. Ann Noninvasive Electrocardiol 2018:e12599 10.1111/anec.12599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yeung C, Baranchuk A. Diagnosis and treatment of lyme carditis: JACC review topic of the week. J Am Coll Cardiol 2019;73:717–26. 10.1016/j.jacc.2018.11.035 [DOI] [PubMed] [Google Scholar]