Abstract
Background:
While severe hemoglobinopathies can be cured with allogeneic blood or marrow transplantation (BMT), the availability of matched donors and toxicities can be problematic. We previously found that nonmyeloablative haploidentical related BMT (haploBMT) with post-transplant cyclophosphamide (PTCy) expanded the donor pool while limiting graft-versus host disease. However, graft failure, albeit with full host hematopoietic recovery, occurred in 50% of patients. Here, we studied whether increasing total body irradiation (TBI) from 200 to 400cGy would improve engraftment while maintaining the safety profile.
Methods:
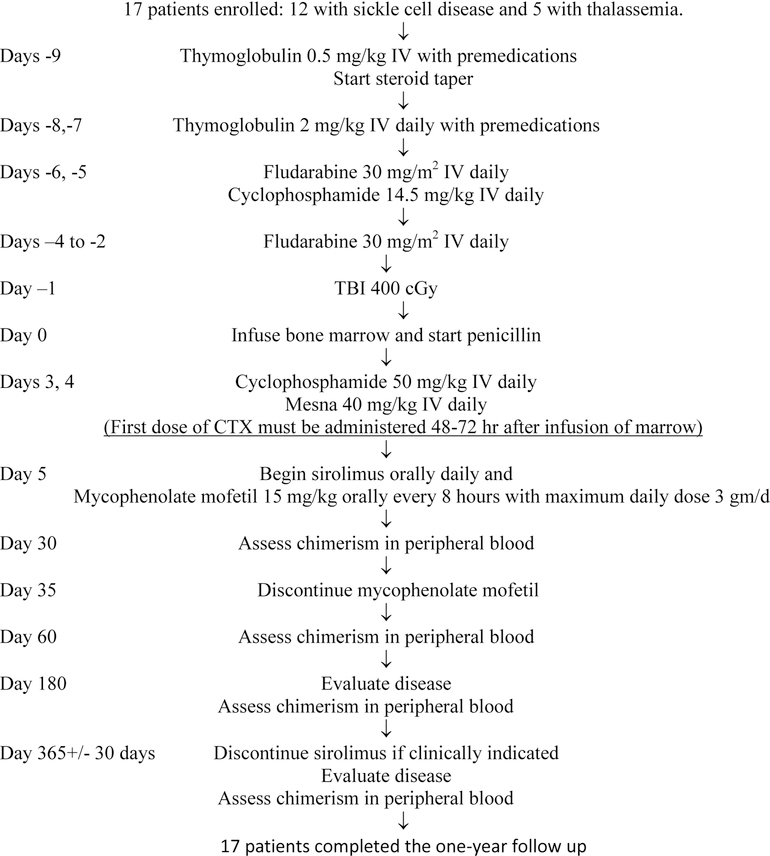
The study is closed to accrual and this is the primary analysis. Twelve consecutive sickle cell disease and five β-thalassemia patients received anti-thymocyte globulin (rabbit) 0.5 mg/kg on day −9 and 2 mg/kg on days −8 and −7; fludarabine 30 mg/m2 on days −6 to −2, cyclophosphamide 14.5 mg/kg on days −6 and −5, and total body irradiation 400 cGy on day −1. Unmanipulated bone marrow was collected and infused on day 0. Graft-versus host disease prophylaxis consisted of PTCy 50 mg/kg/day on days +3 and +4 post transplant; sirolimus to maintain a level of 5–15 ng/dL for one year, and mycophenolate mofetil 15mg/kg per dose (maximum 1 gram) every 8 hours (until day 35) were started on day 5. The primary objective was evaluation of engraftment by intention to treat. Trial registration number: ClinicalTrials.gov NCT00489281.
Findings:
With a median age of 16 (range 6–31 IQR 7.5, 27.5) years, there was 1 graft failure; 13 patients achieved full donor chimerism and 3 exhibited mixed donor-host chimerism. Five patients developed acute graft-versus host disease, and three chronic, all with complete resolution. All patients are alive with a median follow-up of 705 (range 355–1294; IQR 398, 943) days. Only one of the 16 engrafted patients is transfusion dependent. Fourteen have discontinued immunosuppression.
Interpretation:
Increasing TBI to 400cGy significantly reduced graft failure rates while maintaining the safety of haploBMT with PTCy in this small study. These results suggest that engraftment after haploBMT for hemoglobinopathies is possible and primary graft failure, the main problem previously reported, has been solved. Therefore, this curative approach should no longer be restricted to patients with HLA-matched donors.
Funding:
Maryland Stem Cell Research Fund and US National Institutes of Health.
Introduction
Sickle cell disease and β-thalassemia major are severe hemolytic anemias caused by mutations in the β-globin gene. In sickle cell disease, an amino acid substitution in β-globin (β6 glu->Val βS) results in polymerization and red cell sickling that leads to hemolytic anemia, vaso-occlusive crises, strokes, and other end organ damage.(1) In 2010, there were more than 300,000 newborns with sickle cell disease.(2) For adults with sickle cell disease, the average annual cost of medical care exceeds 35,000.00 US dollars.(3) Most adults and many children develop a chronic debilitating condition, leading to high rates of disability and unemployment.(4) The median survival for sickle cell patients in the United States is 40 years(5). Patients with thalassemia require life-long blood transfusions, which predisposes them to iron overload and associated organ-specific complications, along with an increased risk for transfusion-related viral infections including hepatitis B and C.
Allogeneic blood or marrow transplantation (alloBMT) is the only cure for patients with sickle cell disease and thalassemia.(6, 7) Historically, alloBMT for severe-hemoglobinopathies required myeloablative conditioning to enable engraftment. Some adult patients with sickle cell disease have generally been excluded from myeloablative BMT trials because of anticipated excess morbidity and mortality resulting from accumulated disease-related end-organ damage. Finding a suitable donor has also been a challenge. HLA-matched sibling donors are available in less than 10% of potential alloBMT recipients with sickle cell disease.(8) Less than a quarter of African-Americans have HLA-matches in unrelated registries.(9, 10) Accordingly, broader application of alloBMT in severe β - hemoglobinopathies is dependent on novel strategies that address the issues of donor availability as well as limit the toxicity from myeloablative conditioning regimens and graft-versus host disease.
Recently, we showed encouraging results with non-myeloablative alloBMT utilizing related haploidentical donors and post-transplant cyclophosphamide (PTCy).(11) PTCy results in low rates of graft-versus host disease,(12–15) post-BMT lymphoproliferative disorder,(16) and donor derived malignancies.(17) However, despite cures in the majority of patients and low toxicity, the graft failure rate, albeit all with full host recovery, was 50% (one patient suffered secondary graft failure after the manuscript was published). In an attempt to decrease graft failure, we hypothesized that increasing the dose of total body irradiation (TBI) from 200 to 400 cGy before BMT would increase engraftment without increasing transplant-related morbidity and mortality.(18) Such an advance would be impactful; a safe, affordable, life-changing, curative, therapeutic option could be available to essentially any patient in need while limiting late effects including infertility in long-term survivors.
Methods
Study design and participants.
The protocol, ClinicalTrials.gov NCT00489281, whose 200 cGy cohort was previously published,(11) was amended to use 400cGy TBI as approved by the Johns Hopkins Institutional Review Board (IRB). All patients gave IRB-approved informed consent before BMT. A total of 11 (65%) patients received treatment on trial after informed consent was granted in accordance with the Declaration of Helsinki. An additional 6 (35%) patients consented to BMT, but received identical treatment outside of the study as a result of insurance coverage that precluded treatment on a clinical trial. Permission to include these 6 patients in the analysis of outcomes was granted by the Johns Hopkins IRB. Patients aged 2–70 years and receiving their first BMT were eligible. Additional eligibility criteria included good performance status (ECOG 0 or 1; Karnofsky and Lansky 70–100), ability to sign consent (or assent if minors), and the presence of an HLA haploidentical relative willing to donate. Eligible diagnoses included: sickle cell anemia (Hb SS), Hb S/ β° thalassemia, Hb S/ β+ thalassemia, Hb SC disease, Hb SE disease, Hb SD disease, Hb SO-Arab disease, or Hb S/hereditary persistence of fetal hemoglobin, β thalassemia major. In addition, subjects also had to have at least one of the following hemoglobinopathy-related complications already published as indications for BMT in these patients:(6, 8, 19) stroke, magnetic resonance imaging changes indicative of brain parenchymal damage, magnetic resonance angiogram evidence of cerebrovascular disease, abnormal transcranial Doppler velocity, acute chest syndrome requiring exchange transfusion or hospitalization, recurrent vaso-occlusive pain crisis (more than two per year for the last two years), stage I or II sickle lung disease,(20) sickle retinopathy, osteonecrosis, red cell alloimmunization (more than two antibodies) during long-term transfusion, constellation of dactylitis in the first year of life and a baseline hematocrit of 21% and leukocytosis (>13.4 × 103mm3) in the absence of infection during the second year of life, history of invasive pneumococcal disease, pitted red blood cell count >3.5% during the first year of life, or transfusion dependence. The coverage decision by the Centers for Medicare and Medicaid Services to only provide payment of alloBMT for patients with sickle cell disease on a clinical trial that had a comparison arm with non-BMT patients, prompted the closure of this trial in 2017.
Procedures
Donors and grafts.
Relatives who shared at least one HLA haplotype with the patient, did not have sickle cell disease or thalassemia major or intermedia, and were in good health were allowed to serve as donors(11). Donors with sickle cell trait and thalassemia minor were not excluded from bone marrow donation. When more than one donor was available, the donor was selected based on younger age, ABO matching, and CMV serology. If donor anti-HLA antibodies were detected, the next best related match was chosen. Donor bone marrow was harvested with a target yield of 4 × 108 nucleated cells/kg recipient ideal body weight and infused on day 0. The marrow was unmanipulated except that major incompatible ABO grafts had red blood cells depleted by buffy coat preparation and minor ABO incompatible grafts had plasma removed.
HLA Typing.
HLA phenotyping was performed as previously described.(11, 12) Potential family members were initially typed at the HLA-A, HLA-B, and HLA-DRB1 loci at an intermediate resolution level. Family members selected as donors were then further typed at the HLA-C locus at an intermediate resolution level. DRB1 and DQB1 alleles were typed at a high-resolution level. As needed, recipients and potential donors were typed at a high-resolution level for HLA-Cw alleles. Haplotypes were determined based on family studies whenever possible.
Conditioning regimen and graft-versus host disease prophylaxis.
Patients received intravenous anti-thymocyte globulin (rabbit) (Sanofi-Genzyme, Massachusetts USA) 0.5 mg/kg on day −9 and 2 mg/kg on days −8 and −7; intravenous fludarabine (Actaris Group, New Jersey, USA) 30 mg/m2 on days −6 to −2, intravenous cyclophosphamide (Sandoz, New Jersey, USA) 14.5 mg/kg on days −6 and −5, and total body irradiation 400 cGy on day −1. A steroid taper was given to prevent reactions to anti-thymocyte globulin as follows: methylprednisolone 1mg/kg intravenously 1 hour prior anti-thymocyte globulin on days −9 to −7. This dose could be repeated once 3 hours after the first dose. On day −6 and −5, methylprednisolone 0.75 mg/kg/ IV as a single dose; on days −4 and −3, methylprednisolone 0.5 mg/kg/ IV as a single dose; on day −2 methylprednisolone 0.25 mg/kg/ IV as a single dose. Unmanipulated bone marrow was collected and infused on day 0. graft-versus host disease prophylaxis consisted of intravenous cyclophosphamide 50 mg/kg/day on days +3 and +4, and oral sirolimus (Pfizer, New York, USA) to maintain a level of 5–15 ng/dL for at least one year +/− 14 days (or more if mixed chimeras at the judgment of treating physician) as well as oral mycophenolate mofetil (Genentech, South San Francisco, USA) 15mg/kg per dose (maximum 1 gram) every 8 hours (until day 35) that were started on day +5. Patients were allowed to take generic sirolimus and mycophenolate mofetil depending on their pharmacy supply and their insurance coverage.
Outcomes.
Primary endpoint.
The primary endpoint of this study was to evaluate engraftment. Patients had chimerism studies on peripheral blood on days 30, 60, 180, 360, yearly thereafter and as clinically indicated. Chimerism was measured by PCR analysis of variable number of nucleotide tandem repeats unique to donors or recipients on total peripheral blood and isolated CD3+ cells. Graft failure was defined as undetectable DNA of donor origin on at least 2 occasions no less than 1 week apart.
Secondary endpoint.
Secondary endpoint was the description of the toxicities of transplantation in this population.
Statistical analysis.
The primary objective of this phase II clinical trial was to obtain a risk-stratified estimates of two-year progression-free survival with a precision of +/− 20% (95% confidence bound). To obtain this precision, it was necessary to accrue at least 50 patients. The hypothesis of this study was that non-myeloablative conditioning with high-dose posttransplant cyclophosphamide would increase the number of sickle cell disease patients eligible for allogeneic transplantation by allowing the safe and effective use of related haploidentical donors. Given the decision by the Centers for Medicare and Medicaid Services mentioned, the study was closed to accrual before reaching the target enrolment, therefore, no attempt was made to perform the planned analysis given the early close of the study. Instead, a description of the results obtained was performed.
Results
Patients and donors.
Seventeen consecutive patients were enrolled between September 24, 2014 2014 and August 1, 2017: 12 (71%) with sickle cell disease and 5 (29%) with β-thalassemia major (full patient characteristics on Table 1). Ten patients (59%) with sickle cell disease patients had previously received hydroxyurea. Data are current as of August 4, 2018. The median age was 16 (range 6–31; IQR 7.7, 27.5). The median follow up is 705 days (range 355–1294; IQR 398, 943). Two (12%) patients received the graft from a major ABO mismatched donor (B to O and A to O), 5 (29%) from a minor ABO mismatched donor, and 10 (59%) were ABO matched. All the donors were related haploidentical family members, and included 7 (41%) siblings, 5 (29%) mothers, 4 fathers (24%), and 1 aunt (6%).(21)
Table 1.
Demographics.
| ID | Diagnosis | Age | Gender | Ethnicity | Donor ABO/Rh | Recipient ABO/Rh | Donor gender | Donor relationship | BMT Indication* |
|---|---|---|---|---|---|---|---|---|---|
| 35 | SS/B0 thalassemia | 20 | F | Arab | A+ | O+ | M | Father | Osteonecrosis, pain, |
| 36 | SS | 6 | F | AA | O+ | O+ | F | Mother | Pain, abnormal TCD |
| 37 | SS | 30 | F | AA | O+ | A+ | M | Father | Pain, TIA x 3, TD |
| 38 | SS | 31 | M | AA | O+ | B+ | M | Brother | Osteonecrosis, pain, |
| 39 | SS | 30 | M | AA | O+ | O+ | M | Brother | Osteonecrosis, pain, ACS |
| 40 | SS/α-thalassemia | 26 | F | Arab | A+ | A+ | M | Father | Pain, stroke |
| 43 | SS | 27 | F | AA | B+ | O+ | F | Sister | Pain, ACS |
| 47 | SS | 28 | F | AA | O+ | O− | F | Aunt | Pain, ACS |
| 48 | SS | 26 | F | AA | O+ | O+ | F | Mother | Pain, ACS, osteonecrosis |
| 50 | SS | 13 | M | AA | B+ | AB+ | F | Sister | Pain, ACS |
| 51 | SS | 13 | F | AA | O+ | O+ | F | Mother | Pain, ACS |
| 52 | SS | 16 | M | AA | O+ | A+ | M | Brother | Stroke |
| 42 | B-Thal | 7 | F | Arab | O+ | O+ | F | Mother | TD |
| 44 | B-Thal | 6 | F | Arab | O+ | O+ | M | Father | TD |
| 45 | B-Thal | 7 | F | Arab | O+ | O+ | F | Mother | TD |
| 46 | B-Thal | 8 | M | Arab | A+ | A+ | M | Brother | TD |
| 49 | B-Thal/Hb D Los Angeles | 16 | F | Arab | O+ | B+ | F | Sister | TD |
SS: sickle cell disease hemoglobin SS, B-Thal: B-thalassemia major, Hb: Hemoglobin, M: male, F: female, AA: African-American, TCD: transcranial Doppler velocity, TIA: transient ischaemic attack, ACS: Acute chest syndrome, TD: Transfusion dependence. Patients 35 and 40 are siblings and were transplanted form the same donor.
See Materials and Methods for study entry requirements.
Engraftment.
Of the 17 patients, 1 (6%) experienced primary graft failure with recovery of host hematopoiesis; 13 (76%) patients achieved full donor chimerism and three (18%) achieved mixed donor-host chimerism. The patient who rejected the graft fully reconstituted host hematopoiesis by day 70. Graft characteristics and chimerism are shown in Table 2. The median time to count recovery was 28 (IQR 22.5, 31.5) and 26 (IQR 15, 34) days respectively.
Table 2. Graft and engraftment information.
Chimerism expressed as percent of donor DNA obtained in peripheral blood samples.
| ID | CD3 dose infused/kg | Nucleated cells infused/kg | CD34 dose infused/kg | Day 30 chimerism unsorted | Day 30 T cell chimerism | Most recent chimerism unsorted | Most recent CD3+chimerism | Days to most recent chimerism | Rejection | On immunosuppression |
|---|---|---|---|---|---|---|---|---|---|---|
| 35 | 7.50E+07 | 5.80E+08 | 6.70E+06 | >95 | 59 | 17 | 81 | 1255 | No | No |
| 36 | 6.70E+07 | 5.10E+08 | 8.90E+06 | 100 | 100 | 100 | 100 | 365 | No | No |
| 37 | 4.00E+07 | 4.60E+08 | 2.90E+06 | 100 | 88 | 100 | 100 | 412 | No | No |
| 38 | 3.40E+07 | 4.80E+08 | 4.00E+06 | 100 | >95 | 100 | 100 | 350 | No | Unknown |
| 39 | 2.50E+07 | 3.80E+08 | 1.00E+06 | 59 | 0 | 0 | 0 | 62 | Yes | Rejected |
| 40 | 3.90E+07 | 5.90E+08 | 2.00E+06 | 42 | 11 | 20 | 70 | 762 | No | Yes |
| 43 | 2.80E+07 | 2.20E+08 | 3.30E+06 | >95 | 81 | 100 | 100 | 365 | No | No |
| 47 | 3.10E+07 | 4.10E+08 | 4.00E+06 | 100 | >95 | 100 | 100 | 384 | No | Yes |
| 48 | 4.50E+07 | 5.10E+08 | 4.70E+06 | 100 | >95 | 100 | 100 | 305 | No | Yes |
| 50 | 5.52E+07 | 4.35E+08 | 4.09E+06 | 100 | 92 | 100 | 100 | 364 | No | Yes |
| 51 | 4.51E+07 | 5.07E+08 | 5.58E+06 | 100 | >95 | 100 | 100 | 352 | No | Yes |
| 52 | 2.88E+07 | 4.51E+08 | 2.53E+06 | >95 | >95 | 100 | 100 | 214 | No | Yes |
| 42 | 4.80E+07 | 7.30E+08 | 2.00E+06 | 85 | 10 | 22 | 13 | 709 | No | Yes |
| 44 | 9.80E+07 | 7.50E+08 | 8.80E+06 | 100 | 76 | 100 | 100 | 680 | No | No |
| 45 | 2.80E+07 | 1.10E+09 | 3.10E+06 | 100 | 100 | 100 | 100 | 463 | No | Yes |
| 46 | 1.10E+08 | 1.50E+09 | 1.80E+07 | 100 | 100 | 100 | 100 | 359 | No | No |
| 49 | 1.04E+08 | 7.27E+08 | 5.45E+06 | 100 | >95 | 100 | 100 | 409 | No | Yes |
| Median | 4.50E+07 | 5.10E+08 | 4.00E+06 | 100 | 81 | 100 | 100 | 365 | ||
| IQR | 2.99E+07, 7.10E+07 | 4.43E+08, 7.285E+08 | 2.715E+06, 6.14E+06 | 95, 100 | 67.5, 95 | 61, 100 | 90.5, 100 | 351, 571.5 | ||
Graft-versus host disease and BMT related toxicities.
Toxicities were graded per the Common Terminology Criteria for Adverse Events version 5.0 when indicated, as appropriate. Five (29%) patients experienced grade II-IV acute graft-versus host disease, including 4 (23%) with maximal grade II and 1 (6%) with grade III; chronic graft-versus host disease (2 mild, 1 moderate per NIH Consensus) developed in 3 (18%) patients (Table 2). As of their last visit to Johns Hopkins, graft-versus host disease resolved in all cases and all patients are off systemic graft-versus host disease therapy. Sickle cell disease pain crisis after anti-thymocyte globulin was seen in all sickle cell disease patients, 1 (6%) patient developed sirolimus-induced diabetes (grade 3), and 1 (6%) had BK virus hemorrhagic cystitis (grade 3). All patients developed peri-transplant fever. One patient (6%) developed engraftment syndrome, idiopathic pneumonia syndrome, candidemia (grade 3), pneumonia (grade 3), EBV reactivation treated with IVIgG (grade 2), adenovirus, and CMV reactivation (grade 2) in the setting of grade III graft-versus host disease. One patient (6%) with Meniere’s had worsening of his symptoms after exposure to antibiotics (tinnitus grade 2). Patient 1 developed an abnormal karyotype in host cells at 22 months after BMT, although her marrow morphology and flow cytometry continue to show no abnormalities. Her bone marrow karyotype at 36 months after BMT was 46,XX,del(13)(q12q14)[2]/46,sl,del(1)(q32q42),ins(4;?)(q13;?)[4]/46,sl,t(3;6)(q12;p21),add(5)(q34),a dd(20)(q11.2)[2]/46,XX[2]//46,XY[2]. There were no pathologic mutations on a next generation sequencing (NGS) panel. This patient was on hydroxyurea for 3 years before BMT.
Sickle cell disease specific outcomes.
All patients remain alive. Hematologic parameters pre and post BMT can be seen in Table 3. Eleven patients (92%) with sickle cell disease engrafted, and all but 1 (8%) are transfusion independent. The patient who still requires transfusions, Patient 35, received a major ABO mismatched graft (A to O), and continues to have high anti-A titers associated with mixed chimerism. The other recipient of a major ABO incompatible graft, Patient 43, is a full donor chimerism and as such is transfusion independent. None of the engrafted patients have been admitted to the hospital for an acute sickle cell pain crisis since undergoing alloBMT. Patient 40 still has anemia and elevated levels of Hemoglobin S as of last check-up; however, she has not experienced a sickle cell crisis since transplant (>2 years). As of their last follow-up, only one (8%) patient is still on immunosuppression.
Table 3A.
Hematologic parameters for patients with sickle cell disease.
| ID | Bilirubin pre-BMT (mg/dL) | Most Recent Bilirubin (mg/dL) | Absolute reticulocytes pre-BMT (1000xmm3) | Most Recent absolute reticulocytes (1000xmm3) | Hb (g/dL) pre-BMT | Most Recent Hb (g/dL) | Donor Hb (g/dL) | LDH (U/L) pre-BMT | Most Recent LDH (U/L) | Donor Hb S (%) | Most Recent Hb S (%) | Most Recent MCV (fL) | Donor MCV (fL) | Transfusion Independence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 35 | 1.6 | 1.2 | 133.2 | 193.4 | 12.5 | 9.4 | 16.2 | 556 | 223 | 31.8 | 33.5 | 86.5 | 77.8 | No |
| 36 | 1.3 | 0.2 | 467.8 | 51.4 | 8.2 | 12.4 | 12.5 | 566 | 425 | 38.9 | 37.2 | 80.6 | 85.2 | Yes |
| 37 | 7.3 | 0.2 | 556.4 | 80.8 | 7.4 | 10.4 | 12.8 | 495 | 220 | 33.7 | 35.1 | 89.6 | 87.3 | Yes |
| 38 | 2.3 | 0.3 | 56.7 | 127 | 9.3 | 16.8 | 15.7 | 212 | 411 | 38.3 | 37.1 | 81.2 | 82.4 | Yes |
| 39 | 3.5 | 2 | 302 | 302 | 7.5 | 9.5 | 15.8 | 523 | 353 | 37.7 | <5 | 89.8 | 85.2 | No |
| 40 | 0.4 | 0.3 | 100.8 | 42.7 | 8.3 | 8.7 | 16.2 | 155 | 209 | 32 | 76.2 | 60 | 77.8 | Yes |
| 43 | 2.5 | 0.5 | 273.4 | 87.7 | 9.9 | 13.4 | 12.7 | 297 | 158 | 31.9 | 33 | 87.6 | 81.1 | Yes |
| 47 | 4.4 | 0.2 | 798.8 | 175.4 | 7.3 | 10.5 | 13.8 | 632 | 332 | N/A | 0 | 92.7 | 92.3 | Yes |
| 48 | 0.4 | 0.2 | 200.1 | 64.6 | 9 | 11 | 12.8 | 302 | 290 | 37.4 | 37.8 | 83.9 | 83.8 | Yes |
| 50 | 1.8 | 0.2 | 167 | 54.8 | 9.3 | 12.6 | 11.7 | N/A | 208 | 31.5 | 30.2 | 71.5 | 77.1 | Yes |
| 51 | 3.3 | 0.3 | 542.4 | 144.3 | 8.3 | 13.9 | 12.6 | 346 | 229 | 35.2 | 35.9 | 81.6 | 84 | Yes |
| 52 | 5.7 | 0.6 | 234.8 | 65.2 | 10.9 | 14.7 | 13.1 | 428 | 419 | N/A | <5 | 99.8 | 91.6 | Yes |
| Median | 2.4 | 0.3 | 254.1 | 80.8 | 8.65 | 11.7 | 12.95 | 428 | 229 | 34.45 | 35.5 | 85.2 | 83.9 | |
| IQR | 1.375, 4.175 | 0.2, 0.575 | 141.65, 523.75 | 57.25, 167.625 | 7.675, 9.75 | 9.725, 13.775 | 12.625, 15.775 | 297, 556 | 211.75, 396.5 | 31.875, 37.85 | 11.3, 37.175 | 80.75, 89.75 | 78.625, 86.775 |
Thalassemia major specific outcomes.
All patients were diagnosed and started on transfusion programs between the ages of 3 and 18 months, and all required chelation for transfusion-associated iron overload. Just prior to BMT, all patients were treated with oral deferasirox alone or in combination with parenteral deferoxamine to lower serum ferritin to a level around or below 1000 ng/ml. Liver biopsies completed on all patients pre-BMT confirmed evidence of hepatic iron deposition with minimal hepatocellular inflammation and portal fibrosis. All patients also received hydroxyurea at a minimum dose of 15mg/kg/day for at least 8 weeks prior to BMT. After BMT, 4 (80%) of 5 patients are fully engrafted and 1 (20%) exhibits mixed donor-host chimerism. All 5 (100%) are transfusion independent (median time from BMT to last red cell transfusion 17, range 13–157, days (IQR 14, 119 days). Hematologic parameters before and after BMT as well as donors’ (for comparison) are shown in Table 3. Three (60%) of the 5 patients are off immunosuppression at last follow-up.
Discussion
In this study, 17 patients underwent a non-myeloablative haploidentical BMT with 400cGy TBI. Transplant was well tolerated and 13 patients achieved full donor chimerism, 3 mixed chimerism, and only 1 graft failure. Of these patients, only three are still on immunosuppression. This is in sharp contrast with our previous experience utilizing lower doses of TBI(11).
AlloBMT was first shown to cure sickle cell disease in the early 1980s, but its use has been restricted by difficulties finding matched sibling donors and transplant-related morbidity and mortality especially in the setting of myeloablative conditioning. Non-myeloablative conditioning has reduced the toxicity, but even with HLA-identical donors has been associated with graft failure and universal mixed chimerism in both thalassemia and sickle cell disease patients.(22) Although resolution of symptoms related to the hemoglobinopathy can still occur with mixed chimerism, many such patients remain on long-term immunosuppression and can slowly lose chimerism over years.(23) The addition of PTCy to non-myeloablative conditioning(11, 24) has expanded the donor pool such that most sickle cell disease patients can now safely undergo alloBMT. Unfortunately, a higher rate of graft failure was observed with the HLA-haploidentical donors.(11) Here, we demonstrate that increasing the TBI dose in the conditioning regimen from 200 cGy to 400 cGy improved engraftment; only one graft failure and 3 mixed chimeras were observed in 17 hemoglobinopathy patients receiving non-myeloablative conditioning and PTCy, without increasing morbidity or mortality. Importantly, donors were secured for all 17 consecutive patients referred for alloBMT on this cohort of the trial, demonstrating that most patients with severe hemoglobinopathies referred for BMT are no longer limited by lack of donor availability.
The one engrafted patient (Patient 35) who remains transfusion dependent after receiving a major ABO incompatible allograft is the result of mixed donor-recipient chimerism and persistent host immunity producing high levels of anti-donor RBC antibody. The other recipient of a major ABO incompatible graft (Patient 43) is a full donor chimerism and transfusion independent. Of note, 2 of the sickle cell patients with mixed donor-recipient chimerism are sisters (patients 35 and 40) who both received allografts from their father. None of the 11 engrafted patients with sickle cell disease have been admitted after the alloBMT for sickle cell disease related pain crises, and all patients with β-thalassemia are transfusion independent. Moreover, only 3 engrafted patients are still on immunosuppression.
An abnormal karyotype is present in host cells of one patient in the cohort (Patient 35). Not only had this patient received hydroxyurea for 3 years before BMT, but she also has mixed donor-recipient chimerism. There are a few reports of therapy-related myeloid neoplasm in sickle cell disease patient treated with long-term hydroxyurea.(25–27) Whether the addition of BMT will increase this risk in unknown.(28) Moreover, this patient currently has normal marrow morphology without any molecular abnormalities associated with therapy-related myeloid neoplasm (t-MN) on NGS testing. Importantly, clonal cytogeneic abnormalities after BMT should not be considered diagnostic of t-MN, as they can be transient or may not progress; however, while no clinical t-MN has developed in this patient, longer follow-up is needed.(29)
Several groups have attempted to improve outcomes for patients with severe hemoglobinopathies. The potential impact of our data may be best appreciated in comparison with published observations. Recent studies using alternative stem cell sources, reduced intensity conditioning platforms, or both to expand the donor pool and or limit transplant-related toxicity for patients with severe sickle cell disease and thalassemia have produced disappointing results. Graft-versus host disease, opportunistic infection and mortality following myeloablative conditioning remained problematic for children with thalassemia even when augmented graft-versus host disease prophylaxis was used(30). Utilization of haploidentical donors following myeloablative conditioning have produced mixed results. Depletion of TRCab+ and CD19+ cells from stem cell grafts reportedly improved engraftment when compared to CD34+ selected grafts but were still associated with extensive chronic graft-versus host disease, post-transplant lymphoproliferative disease, and delayed immune reconstitution(31). By contrast, use of haploidentical donors and PTCy resulted in excellent rates of engraftment and overall survival albeit in the context of full intensity conditioning and two additional blocks of pre-transplant, immunosuppressive therapy.(32) Multicenter trials using a alemtuzumab, fludarabine, and melphalan based regimen and either cord blood or bone marrow grafts from matched unrelated donors for children with sickle cell disease(33, 34) or thalassemia (35) were recently conducted. Unfortunately, outcomes were limited by unacceptably high rates of graft failure(33) mortality(34), extensive chronic graft-versus host disease and viral reactivation(34, 35). While some efforts to combine haploidentical donors and reduced intensity, nonmeyloablative, preparative regimens were plagued but suboptimal donor engraftment(11, 23), a recent study demonstrated more robust donor chimerism with augmented conditioning in a small number of patients with sickle cell disease(15).
Other potentially curative approaches (gene therapy and genome editing) for severe hemoglobinopathies are being studied. Since gene therapy and future genome editing approaches use autologous stem cells, no donor is required and the risk of graft-versus host disease is avoided. However, myeloablative conditioning is currently required for engraftment after autologous BMT with gene corrected stem cells.(36, 37) Myeloablative conditioning can be associated with substantial risk of infertility, morbidity, and mortality even in patients with moderate end organ toxicity, which will ultimately exclude many patients with sickle cell disease and thalassemia from such protocols. Further, currently gene therapy for thalassemia is not curative for most patients in that it does not eliminate transfusion needs, and recent concerns have been raised about the safety of clinical gene editing approaches.(37, 38)
The current study has clear limitations. Due to the U.S. Government’s decision on funding clinical trials for sickle cell disease patients, this line of investigation had to be stopped before it was completed limiting the total number of individuals transplanted, and the conclusions that can be drawn from smaller patient cohort. Furthermore, this was a single center study and patients with very severe co-morbidities were ineligible for enrollment. While a follow up of 705 days (IQR 398, 943) is adequate to suggest an improvement on engraftment over our previous experience, and to corroborate the low rates of acute and chronic graft-versus-host disease, it may not be enough for other complications such as secondary malignancies, infertility, or maintenance of the graft in the long term, particularly on patients that are mixed chimeras. However, at the same time, the improvement on engraftment compared to other series published, including our own, suggests this observation is an important finding.
In summary, despite several trials describing the universal availability and safety of haploBMT for hemoglobinopathies,(11, 23) recent reports on novel therapies for this disease continue to comment on the limited availability of donors and the toxicity alloBMT.(39) Our data demonstrate that increasing TBI from 200cGy to 400 cGy allows for stable engraftment and is well tolerated in hemoglobinopathy patients receiving haploBMT. Moreover, the majority develop full donor chimerism and can safely have their immunosuppression stopped after one year. Major ABO incompatible donors should be avoided when possible as mixed chimerism with persistent host anti-donor RBC antibodies can cause prolonged transfusion dependence. The American Society of Hematology (http://www.hematology.org/Research/Recommendations/Sickle-Cell/3151.aspx last accessed December 10, 2018) and National Institutes of Health (https://www.nih.gov/about-nih/who-we-are/nih-director/testimony-21st-century-cures-implementation-updates-fda-nih last accessed December 10, 2018) have recently introduced important initiatives to cure sickle cell disease. The encouraging results of this study warrants further investigation to determine if the curative potential of alloBMT can extend beyond the traditionally small fraction of patients with severe hemoglobinopathies with matched donors and fit enough to receive myeloablative conditioning.
Figure 1.
Study schema
Table 3B.
Hematologic parameters for patients with B-Thalassemia.
| ID | Bilirubin pre-BMT (mg/dL) | Most Recent Bilirubin (mg/dL) | Absolute Reticulocytes pre-BMT (1000xmm3) | Most Recent absolute reticulocytes (1000xmm3) | Hb (g/dL) pre-BMT | Most Recent Hb (g/dL) | Donor Hb (g/dL) | LDH (U/L) pre-BMT | Most Recent LDH (U/L) | Most Recent MCV (fL) | Donor MCV (fL) | Ferritin pre-BMT (ng/mL) | Most Recent Ferritin (ng/mL) | Transfusion Independence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 42 | 0.7 | 0.2 | 23.3 | 44.4 | 9.5 | 8.7 | 10.2 | 193 | 274 | 64.9 | 62 | 626 | 429 | Yes |
| 44 | 0.4 | 0.3 | 6.1 | 61.1 | 7 | 10.8 | 12.1 | 174 | 189 | 56.4 | 58.4 | 370 | 188 | Yes |
| 45 | 0.5 | 0.2 | 5.9 | 120.4 | 10.4 | 9 | 10 | 301 | 269 | 57.8 | 61.4 | 1331 | 356 | Yes |
| 46 | 1.3 | 0.5 | 11.6 | 82.3 | 11.1 | 8.9 | 12.4 | 143 | 251 | 53.7 | 55.9 | 881 | 702 | Yes |
| 49 | 0.9 | 0.4 | 23.3 | 87.6 | 6.9 | 12.7 | 11.4 | N/A | 203 | 82.1 | 83.5 | 743 | 1011 | Yes |
| Median | 0.7 | 0.3 | 11.6 | 82.3 | 9.5 | 9 | 11.4 | 183.5 | 251 | 57.8 | 61.4 | 743 | 429 | |
| IQR | 0.45, 1.1 | 0.2, 0.45 | 6, 23.3 | 52.75, 104 | 6.95, 10.75 | 8.8, 11.75 | 10.1, 12.25 | 150.75 274 | 196, 271.5 | 55.05, 73.5 | 57.15, 72.75 | 498, 1106 | 272, 856.5 |
Hb: hemoglobin, LDH: lactic dehydrogenase, MCV: mean corpuscular volume, BMT: bone marrow transplant. Pre-BMT values were transfused, *comparison vs donor.
Research in context.
Evidence before this study
Allogeneic blood or marrow transplantation is a curative therapy available for patients with severe haemoglobinopathies (i.e. thalassaemia and sickle cell disease). Unfortunately, the vast majority of patients who need a transplant lack a matched donor and/or cannot withstand myeloablative conditioning. More than 95% of patients will have an unaffected related haploidentical donors, i.e., siblings, parents, and even second degree relatives such as aunts and uncles, but high rates of mortality related to graft-versus-host disease have limited the use of such donors historically. However, improved graft versus host preventive strategies such as post-transplant cyclophosphamide are now associated with very low rates of graft versus host disease even with mismatched donors. In fact, allogeneic transplantation using reduced intensity conditioning with post-transplant cyclophosphamide has been associated with very low rates of graft versus host disease and transplant-related mortality following related haploidentical donor transplantation for more than a decade. The limitation has been a 30–40% risk of graft loss that has been non-fatal because of uniform host recovery.
We searched MEDLINE for articles published in English until October 19, 2018. The terms searched were “haploidentical transplantation for sickle cell disease” and “ haploidentical transplantation for thalassemia”. Haploidentical BMT has been attempted, but the published studies are small and plagued by high rates of graft failure and transplant-related toxicities.
Added value of this study
We show for the first time that haploidentical bone marrow transplantation results in a high percentage (> 90%) of donor engraftment with minimal risk of GVHD. Importantly, most patients achieve full donor chimerism and are able to discontinue immunosuppression. We have now solved the problem of graft loss. The increase of TBI from 200 to 400 cGy on day −1 improved engraftment without increasing toxicity.
Implications of all the available evidence
Curative allogeneic bone marrow transplantation should no longer be considered a therapy that is available to a small fraction of patients with severe hemoglobinopathies - i.e., those with matched donors and fit enough to receive myeloablative conditioning. The availability of haploidentical family donors, the high engraftment rate, and low toxicity, raises the bar for other exciting potential curative options (gene therapy and genome editing) that require currently myeloablative conditioning.
Acknowledgements:
The authors would like to thank the patients, their families, and their caregivers. Funded in part by 2013-MSCRFII-0082; (PI: RAB); and by National Institutes of Health Grants P01 CA015396 (PI: RJJ) and P30 CA006973 (PI: William Nelson, MD). Presented in part, at the Late Breaking Abstracts session (LBA-3), American Society for Blood and Marrow Transplantation 2018 BMT Tandem Meeting, Salt Lake City, Utah.
The trial was registered with ClinicalTrials.gov, number NCT00489281.
Role of funding source.
Funded in part by 2013-MSCRFII-0082; (PI: RAB); and by National Institutes of Health Grants P01 CA015396 (PI: RJJ) and P30 CA006973 (PI: William Nelson, MD). The funders had no role in the study design, data collection, data analysis, interpretation of results, or writing of the report. KC, RJJ, and JB-M had access to the data. All authors approved the manuscript. The corresponding author had full access to all of the data and had the final responsibility to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data sharing
Patient-level data will not be shared.
Conflict of Interest Disclosures:
Dr. Ali reports consulting and research funding from Celgene, consulting, Advisory Board, research funding from Aduro Biotech, Advisory Board from Bristol Myers-Squibb, Advisory Board from Amgen, Advisory Board from Takeda, outside the submitted work.
Dr. Bolaños-Meade reports DSMB fees from Incyte Corporation, outside the submitted work.
Dr. Brodsky reports grants from Maryland State Stem Cell Fund/TEDCO, during the conduct of the study; Scientific Advisory Board and research funding from Alexion Pharmaceutical, and Achillion Pharmaceutical, outside the submitted work.
Dr. Cooke reports grants from MSCRF, grants from NIH, during the conduct of the study
Dr. Luznik reports Advisory Board fees from AbbVie, speaking engagement from Merck, grants from Gennentech, Advisory Board fees from Pharamacyclics.
Dr. Symons reports belonging to the Speaker’s Bureau for Jazz pharmaceuticals re: Defetilio. she helped create the slideset, speak about veno-occlussive disease pathophysiology as well as treatment. Dr. Terezakis reports a scientific grant from ASELL and a scientific grant from Elekta Industries, outside the submitted work.
Dr. Wagner-Johnston reports other from Advisory Board fees from Gilead, other from Bayer, other from JUNO, other from ADC Therapeutics, other from Janssen, outside the submitted work.
The other authors declared no conflict of interest.
References
- 1.Lorey FW, Arnopp J, Cunningham GC. Distribution of hemoglobinopathy variants by ethnicity in a multiethnic state. Genet Epidemiol 1996;13(5):501–12. [DOI] [PubMed] [Google Scholar]
- 2.Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN. Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med 2013;10(7):e1001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Hartzema AG. The cost of health care for children and adults with sickle cell disease. Am J Hematol 2009;84(6):323–7. [DOI] [PubMed] [Google Scholar]
- 4.Ballas SK, Bauserman RL, McCarthy WF, Waclawiw MA. The impact of hydroxyurea on career and employment of patients with sickle cell anemia. J Natl Med Assoc 2010;102(11):993–9. [PubMed] [Google Scholar]
- 5.Lanzkron S, Carroll CP, Haywood C Jr. Mortality rates and age at death from sickle cell disease: U.S., 1979–2005. Public Health Rep 2013;128(2):110–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernaudin F, Socie G, Kuentz M, Chevret S, Duval M, Bertrand Y, et al. Long-term results of related myeloablative stem-cell transplantation to cure sickle cell disease. Blood 2007;110(7):2749–56. [DOI] [PubMed] [Google Scholar]
- 7.Walters MC, Patience M, Leisenring W, Eckman JR, Scott JP, Mentzer WC, et al. Bone marrow transplantation for sickle cell disease. N Engl J Med 1996;335(6):369–76. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh MM, Kang EM, Fitzhugh CD, Link MB, Bolan CD, Kurlander R, et al. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med 2009;361(24):2309–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dehn J, Buck K, Maiers M, Confer D, Hartzman R, Kollman C, et al. 8/8 and 10/10 high-resolution match rate for the be the match unrelated donor registry. Biol Blood Marrow Transplant 2015;21(1):137–41. [DOI] [PubMed] [Google Scholar]
- 10.Justus D, Perez-Albuerne E, Dioguardi J, Jacobsohn D, Abraham A. Allogeneic donor availability for hematopoietic stem cell transplantation in children with sickle cell disease. Pediatr Blood Cancer 2015;62(7):1285–7. [DOI] [PubMed] [Google Scholar]
- 11.Bolaños-Meade J, Fuchs EJ, Luznik L, Lanzkron SM, Gamper CJ, Jones RJ, et al. HLA-haploidentical bone marrow transplantation with posttransplant cyclophosphamide expands the donor pool for patients with sickle cell disease. Blood 2012;120(22):4285–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant 2008;14(6):641–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brodsky RA, Luznik L, Bolaños-Meade J, Leffell MS, Jones RJ, Fuchs EJ. Reduced intensity HLA-haploidentical BMT with post transplantation cyclophosphamide in nonmalignant hematologic diseases. Bone Marrow Transplant 2008;42(8):523–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood 2011;118(2):282–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saraf SL, Oh AL, Patel PR, Sweiss K, Koshy M, Campbell-Lee S, et al. Haploidentical Peripheral Blood Stem Cell Transplantation Demonstrates Stable Engraftment in Adults with Sickle Cell Disease. Biol Blood Marrow Transplant 2018;24(8):1759–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanakry JA, Kasamon YL, Bolaños-Meade J, Borrello IM, Brodsky RA, Fuchs EJ, et al. Absence of post-transplantation lymphoproliferative disorder after allogeneic blood or marrow transplantation using post-transplantation cyclophosphamide as graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant 2013;19(10):1514–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Majzner RG, Mogri H, Varadhan R, Brown P, Cooke KR, Bolanos-Meade J, et al. Post-Transplantation Cyclophosphamide after Bone Marrow Transplantation Is Not Associated with an Increased Risk of Donor-Derived Malignancy. Biol Blood Marrow Transplant 2017;23(4):612–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sobecks RM, Dean R, Rybicki LA, Chan J, Theil KS, Macklis R, et al. 400 cGy TBI with fludarabine for reduced-intensity conditioning allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2008;42(11):715–22. [DOI] [PubMed] [Google Scholar]
- 19.Vermylen C Hematopoietic stem cell transplantation in sickle cell disease. Blood Reviews 2003;17(3):163–6. [DOI] [PubMed] [Google Scholar]
- 20.Powars D, Weidman JA, Odom-Maryon T, Niland JC, Johnson C. Sickle cell chronic lung disease: prior morbidity and the risk of pulmonary failure. Medicine (Baltimore) 1988;67(1):66–76. [PubMed] [Google Scholar]
- 21.Elmariah H, Kasamon YL, Zahurak M, Macfarlane KW, Tucker N, Rosner GL, et al. Haploidentical Bone Marrow Transplantation with Post-Transplant Cyclophosphamide Using Non First-Degree Related Donors. Biology of Blood and Marrow Transplantation 2018;24(5):1099–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathews V, Savani BN. Conditioning regimens in allo-SCT for thalassemia major. Bone Marrow Transplant 2014;49(5):607–10. [DOI] [PubMed] [Google Scholar]
- 23.Fitzhugh CD, Hsieh MM, Taylor T, Coles W, Roskom K, Wilson D, et al. Cyclophosphamide improves engraftment in patients with SCD and severe organ damage who undergo haploidentical PBSCT. Blood Adv 2017;1(11):652–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frangoul H, Evans M, Isbell J, Bruce K, Domm J. Haploidentical hematopoietic stem cell transplant for patients with sickle cell disease using thiotepa, fludarabine, thymoglobulin, low dose cyclophosphamide, 200 cGy tbi and post transplant cyclophosphamide. Bone Marrow Transplant 2018;53(5):647–50. [DOI] [PubMed] [Google Scholar]
- 25.Aumont C, Driss F, Lazure T, Picard V, Creidy R, De BS, et al. Myelodysplastic syndrome with clonal cytogenetic abnormalities followed by fatal erythroid leukemia after 14 years of exposure to hydroxyurea for sickle cell anemia. Am J Hematol 2015;90(7):E131–E2. [DOI] [PubMed] [Google Scholar]
- 26.Baz W, Najfeld V, Yotsuya M, Talwar J, Terjanian T, Forte F. Development of myelodysplastic syndrome and acute myeloid leukemia 15 years after hydroxyurea use in a patient with sickle cell anemia. Clin Med Insights Oncol 2012;6:149–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor JG, Darbari DS, Maric I, McIver Z, Arthur DC. Therapy-related acute myelogenous leukemia in a hydroxyurea-treated patient with sickle cell anemia. Ann Intern Med 2011;155(10):722–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Janakiram M, Verma A, Wang Y, Budhathoki A, Suarez LJ, Murakhovskaya I, et al. Accelerated leukemic transformation after haplo-identical transplantation for hydroxyurea-treated sickle cell disease. Leuk Lymphoma 2018;59(1):241–4. [DOI] [PubMed] [Google Scholar]
- 29.Showel MM, Brodsky RA, Tsai HL, Briel KM, Kowalski J, Griffin CA, et al. Isolated clonal cytogenetic abnormalities after high-dose therapy. Biol Blood Marrow Transplant 2014;20(8):1130–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khandelwal P, Davies SM, Dandoy CE, El-Bietar J, Grimley MS. Augmenting GVHD Prophylaxis in Allogeneic Hematopoietic Stem Cell Transplant for Beta Thalassemia Major Reduces Acute GVHD Incidence and Severity without Impacting Engraftment. Biology of Blood and Marrow Transplantation 2017;23(3):S237–S8. [Google Scholar]
- 31.Gaziev J, Isgro A, Sodani P, Paciaroni K, De AG, Marziali M, et al. Haploidentical HSCT for hemoglobinopathies: improved outcomes with TCRalphabeta(+)/CD19(+)-depleted grafts. Blood Adv 2018;2(3):263–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anurathapan U, Hongeng S, Pakakasama S, Sirachainan N, Songdej D, Chuansumrit A, et al. Hematopoietic stem cell transplantation for homozygous beta-thalassemia and beta-thalassemia/hemoglobin E patients from haploidentical donors. Bone Marrow Transplant 2016;51(6):813–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kamani NR, Walters MC, Carter S, Aquino V, Brochstein JA, Chaudhury S, et al. Unrelated donor cord blood transplantation for children with severe sickle cell disease: results of one cohort from the phase II study from the Blood and Marrow Transplant Clinical Trials Network (BMT CTN). Biol Blood Marrow Transplant 2012;18(8):1265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shenoy S, Eapen M, Panepinto JA, Logan BR, Wu J, Abraham A, et al. A trial of unrelated donor marrow transplantation for children with severe sickle cell disease. Blood 2016;128(21):2561–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shenoy S, Walters MC, Ngwube A, Soni S, Jacobsohn D, Chaudhury S, et al. Unrelated Donor Transplantation in Children with Thalassemia using Reduced-Intensity Conditioning: The URTH Trial. Biol Blood Marrow Transplant 2018;24(6):1216–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ribeil JA, Hacein-Bey-Abina S, Payen E, Magnani A, Semeraro M, Magrin E, et al. Gene Therapy in a Patient with Sickle Cell Disease. N Engl J Med 2017;376(9):848–55. [DOI] [PubMed] [Google Scholar]
- 37.Thompson AA, Walters MC, Kwiatkowski J, Rasko JEJ, Ribeil JA, Hongeng S, et al. Gene Therapy in Patients with Transfusion-Dependent beta-Thalassemia. N Engl J Med 2018;378(16):1479–93. [DOI] [PubMed] [Google Scholar]
- 38.Kosicki M, Tomberg K, Bradley A. Repair of double-strand breaks induced by CRISPR-Cas9 leads to large deletions and complex rearrangements. Nat Biotechnol 2018;36(8):765–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cai L, Bai H, Mahairaki V, Gao Y, He C, Wen Y, et al. A Universal Approach to Correct Various HBB Gene Mutations in Human Stem Cells for Gene Therapy of Beta-Thalassemia and Sickle Cell Disease. Stem Cells Transl Med 2018;7(1):87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]