Abstract
Objective
Phonation threshold pressure (PTP), the minimum subglottal pressure (Ps) required for phonation, is sensitive to changes in laryngeal biomechanics and is often elevated with pathology. Little is reported on PTP in children; challenges with task performance and measurement reliability represent barriers to routine clinical assessment. We conducted a pilot study evaluating PTP and Ps measurement reliability in children using labial and mechanical interruption.
Methods
22 subjects aged 4–17 (10.7±3.9) participated. Ten trials were performed for each method; task order was randomized. For labial interruption, subjects produced /pα/ five times at softest (onset PTP) and comfortable amplitude. For mechanical interruption, subjects produced a sustained /α/ while a balloon valve interrupted phonation five times for 250 ms each; mechanical interruption was performed with a mouthpiece and mask. PTP was recorded as the difference between Ps and supraglottal pressure at phonation cessation (offset PTP). Mean PTP and Ps and intra-subject coefficients of variation were compared. Correlations with age were evaluated.
Results
Mean PTP (p<0.001) and Ps (p=0.005) were higher for labial interruption. Intra-subject coefficients of variation for PTP (p=0.554) and Ps (p=0.305) were similar across methods. Coefficient of variation was related to age for mechanical-mask trials only (r=−0.628; p=0.00175).
Conclusion
Differences in means are likely related to differences in task and PTP hysteresis effect. Reliability is comparable with all methods; using a mouthpiece may be preferable to a mask for mechanical interruption. Measurement of PTP is noninvasive, reliable, and may be a useful adjunct in pediatric voice assessment.
Keywords: phonation threshold pressure, pediatric, aerodynamic, subglottal pressure, voice, airflow interruption
INTRODUCTION
Pediatric dysphonia is common. Prevalence rates vary, with estimates of 1% based on the 2012 National Health Interview Survey1 and 6% for a large cohort of 8-year-olds in the United Kingdom.2 Children with dysphonia experience anxiety, discomfort, anger, sadness, and frustration.3,4 Assessment should include videostroboscopic, perceptual, acoustic, and aerodynamic evaluations.5,6 Aerodynamic parameters quantify the inputs to voice production, provide insight into the effort required to produce speech, and represent an important aspect of pediatric voice evaluation.7 Complete assessment requires measurement of subglottal pressure (Ps) and phonation threshold pressure (PTP).
PTP is the minimum Ps required to initiate vocal fold oscillation.8 It is dependent on vocal fold thickness, tissue damping coefficient, prephonatory glottal width, and mucosal wave velocity.9 Multiple studies have demonstrated elevated PTP in disease states, including vocal fatigue,10 vocal fold scar,11 benign mass lesions,12 and dehydration.13,14 Though a potentially useful component of voice assessment, standard implementation is limited in part by measurement reliability.15
The most commonly used method of noninvasive Ps measurement is labial interruption, or measurement of intraoral pressure during repeated utterances of /pi/ or /pα/. During the bilabial stop phase of /p/, intraoral pressure equilibrates with Ps.16 This allows for indirect, noninvasive estimation of Ps. This method is accurate;17 however, it can be somewhat challenging to master the technique and obtain consistent results.18 Further, to estimate PTP, the subject must produce serial utterances at their softest possible phonation. It may be difficult for subjects to do this consistently, particularly young children.
An alternative method is mechanical interruption. This approach uses an external mechanical valve to temporarily interrupt subject airflow, thus allowing for equilibration of supraglottal pressure with Ps; pressure is then measured within the device.19,20 Jiang et al. presented a modification that allowed for measurement of PTP, recorded as Ps minus the supraglottal pressure at the time that phonation ceases during the interruption.20 This method has been used to demonstrate differences in laryngeal function in Parkinson’s disease21 and vocal fold nodules,12 but has never been applied to pediatric subjects.
Chapin et al. compared labial and mechanical interruption for measurement reliability of Ps, mean flow rate, and laryngeal resistance in adult subjects with normal voice.22 Intrasubject variability was compared for each parameter. Mean intrasubject variability was similar for Ps and mean flow rate, but higher for laryngeal resistance with the labial interruption technique. PTP was not evaluated.
Importantly, PTP exhibits a hysteresis effect, where the minimum pressure required to initiate phonation (onset PTP) is lower than that required to sustain it (offset PTP).9,23 This has been demonstrated in mathematical models,9,24,25 physical models,9 and excised larynx experiments.23 Measurement of PTP via labial interruption at the point of softest phonation represents an onset pressure, while measurement of PTP via mechanical interruption at the time phonation ceases represents an offset pressure. This is important to consider when comparing mean values between the two methods.
There have been prior large-scale studies evaluating aerodynamic parameters in children26 but few studies reporting specifically on PTP. McAllister and Sundberg used labial interruption at softest phonation to measure PTP in seven children, with a mean of 3.6 cmH2O without specifically reported intrasubject or intersubject variability.27 Stathopoulos and Sapienza measured Ps in twenty 4-year-olds and twenty 8-year-olds at three vocal intensities, with the lowest being 5 dB below the subjects’ comfortable SPL.28 Mean pressure at the soft intensity was approximately 6 cmH2O, but may have been above the phonation threshold. Hsu et al. measured multiple voice parameters including PTP in Mandarin-speaking children after cochlear implantation as well as a group of normal controls.29 PTP was measured via production of serial /pi/ tokens and found to be higher in the implanted subjects.29 Intersubject variability was fairly low (4.6±1.4 cmH2O for implanted subjects versus 2.6±0.4 cmH2O for controls), but intrasubject variability was not reported.
In this study, we conducted an initial pilot study measuring PTP and Ps in children aged 4–17 using both mechanical interruption (with a mouthpiece and a mask) and labial interruption. This is the first application of mechanical interruption to pediatric subjects. Second, this is the first study to date in pediatric subjects focusing specifically on PTP measurement reliability. Third, we compared measurement reliability using both mechanical and labial interruption methods. It may be easier for children to produce the sustained vowel required for mechanical interruption, but they may be more easily startled or distracted by the balloon valve interruption. On the other hand, children may find it challenging to maintain consistency with repeated labial plosives or have difficulty achieving the softest possible phonation, but may prefer the more predictable nature of a subject-controlled interruption. As a component within this aim, we evaluated whether mechanical interruption with a mask versus a mouthpiece was more reliable for measurement of PTP. Last, we evaluated how measurement reliability changed with increasing age.
We hypothesized that measurement reliability for mechanical interruption would be higher with a mouthpiece rather than a mask, as obtaining a tight seal with a mask may be more challenging with children. Second, we hypothesized that measurement reliability would be comparable for the mechanical and labial approaches, but mean PTP would be lower for mechanical interruption, as it represents an offset PTP and is not dependent on production of softest possible phonation. Lastly, we hypothesized that measurement reliability would improve with increasing age.
METHODS
Subjects
This study was approved by the Institutional Review Board of the University of Wisconsin-Madison. Parents provided written consent and subjects provided written or verbal assent to participate. Twenty-two subjects (13 females, 9 males) without history of dysphonia, aged 4–17 (mean: 10.7±3.9 years), participated (table 1). Subjects were recruited via flyers. Each subject underwent perceptual voice analysis using the Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V)30 prior to testing to ensure they were not dysphonic. All ratings were completed by a voice specialized speech pathologist (MNB).
Table 1.
Subject characteristics.
| Number | Age (years) | Sex |
|---|---|---|
| 1 | 13 | F |
| 2 | 17 | M |
| 3 | 17 | F |
| 4 | 11 | M |
| 5 | 15 | F |
| 6 | 10 | M |
| 7 | 13 | F |
| 8 | 8 | M |
| 9 | 11 | M |
| 10 | 13 | F |
| 11 | 5 | F |
| 12 | 13 | M |
| 13 | 14 | F |
| 14 | 5 | F |
| 15 | 4 | M |
| 16 | 11 | M |
| 17 | 14 | F |
| 18 | 12 | M |
| 19 | 5 | F |
| 20 | 8 | F |
| 21 | 10 | F |
| 22 | 6 | F |
Subjects were tested using both labial and mechanical interruption methods. Four tasks were performed, ten times each, for a total of forty trials: labial interruption at comfortable amplitude; labial interruption at softest amplitude; mechanical interruption at comfortable amplitude using a mask; and mechanical interruption at comfortable amplitude using a mouthpiece. Task order was randomized across subjects to prevent learning bias. The subject’s parent was allowed to be present during testing. For younger subjects, parents could provide encouragement to maintain attention.
Experimental setup
The experimental setup is similar to that described previously (figure 1).20,31 The airflow interruption setup was used rather than the KayPENTAX Phonatory Aerodynamic System that was used in the Chapin et al. study22 to allow for more precise audio recording required for estimation of PTP during mechanical interruption. The same device was used for labial and mechanical interruption. The device consisted of a PVC tube containing a condenser microphone (AKG CK77, Harman International Industries, Inc., Stamford, CT) connected to a preamplifier (MP13 Mini-Mic Preamp, Rolls Co., Murray, UT), pressure port, two airflow ports with intervening constant resistance screen, and balloon valve (Series 9340, Hans Rudolph, Inc.) at its distal end. Pressure data were sampled using a Pneumotach amplifier (Series 1110, Hans Rudolph, Inc.) at 10 kHz. Auditory signals were sampled at 10 kHz. Data were collected using a data acquisition board (model USB-6341, National Instruments, Inc., Austin, TX).
Figure 1.
Schematic of experimental device used for both labial and mechanical interruption. For labial interruption trials, a face mask and intraoral pressure tube were used and the balloon valve was not inflated. For mechanical interruption trials, either a face mask or mouthpiece was used and the balloon valve was inflated five times per trial.
For labial interruption, a silicone mask was used. A variety of sizes were available (Vital Signs Face Masks, Vyaire Medical, Inc., Mettawa, IL). An intraoral pressure tube (0.066″ diameter low density polyethylene tubing) was placed from within the pressure measurement tube to just inside the subject’s lips. We confirmed there was no leak in the system prior to beginning trials by asking subjects to phonate with the balloon valve inflated and confirming phonation was not possible. The balloon valve at the distal end of the device remained attached but was not inflated during trials.
For mechanical interruption, either a mask (the same used for labial interruption) or mouthpiece (Series 9063, Hans Rudolph, Inc.; Soft Bite Mouthpieces, Trident Diving Equipment, Chatsworth, CA) was used. A variety of sizes were available. For trials with a mouthpiece, subjects used a nose clip (Series 9014, Hans Rudolph, Inc.) to prevent air leak through the nose. The balloon valve was operated by a digitally activated custom pressure control valve system. This pressure valve was supplied by a larger pressurized air tank. Data were collected using a customized LabVIEW program (National Instruments, Inc.). The program also provided live feedback during trials on sound pressure level and airflow. Aerodynamic data were calibrated using an analog pressure meter (PC-1H, Glottal Enterprises, Syracuse, NY) and a digital flow meter (FMA-1610A, Omega Engineering, Stamford, CT).
Labial interruption
For each trial, subjects produced five labial interruptions by phonating /pα/ at comfortable amplitude (approximately 75 dB) or as softly as possible into a facemask with the intraoral pressure tube in place. Practice trials were conducted so subjects could learn to create a seal with their lips around the intraoral pressure tube and, for PTP trials, adjust their amplitude to be as soft as possible. Ten trials were performed at comfortable amplitude and at softest amplitude.
Mechanical interruption
For mechanical interruption, subjects produced a sustained /α/ at comfortable amplitude (approximately 75 dB) while five interruptions, each lasting 250 ms, were performed at random intervals of 1–1.5 seconds. Each interruption completely stopped airflow temporarily. A 250 ms interruption was used instead of the previously described 500 ms interruption20 due to the decreased lung volume in children and the desire to avoid subjects running out of breath prematurely. Subjects were instructed to maintain constant effort during the interruption. For trials with a mask, subjects were instructed to hold the mask tight to create a proper seal. Real-time visual feedback on sound pressure level and airflow were provided to ensure subjects maintained constant effort during and across trials. Ten trials were performed each with a mask and a mouthpiece.
Data analysis
A customized LabVIEW program was used for analysis. For labial interruptions, PTP or Ps was measured as the peak pressure immediately before phonation of the labial plosive (figure 2). For mechanical interruption, Ps was measured as the pressure at 150 ms into the interruption.31 PTP was measured as the difference between Ps and supraglottal pressure at the time phonation ceased22 (figure 2). This is done to avoid potential confounding effects of a possible laryngeal adductor reflex, which could theoretically be triggered by the rapid increase in supraglottal pressure caused by the interruption. For all techniques, PTP for the trial was measured as the average of the five interruptions within the trial.
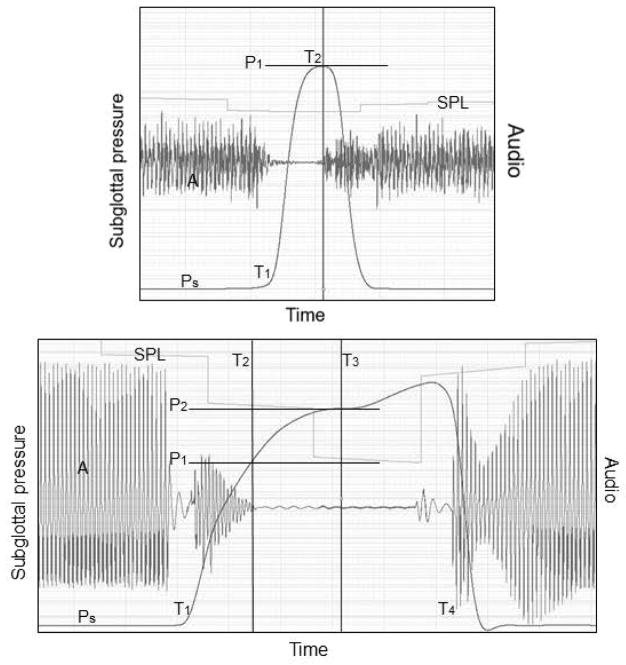
Figure 2.
Estimation of phonation threshold pressure (PTP) for labial (top) and mechanical interruption (bottom). For labial interruption, the PTP is estimated as the peak intraoral pressure (P1) prior to phonation onset (T2). For mechanical interruption, PTP is estimated as supraglottal pressure (P2) at 150 ms (T3; the subject’s subglottal pressure) minus the supraglottal pressure (P1) at the time of phonation cessation (T2). For both figures, A=audio, SPL=sound pressure level, Ps=subglottal pressure trace, T1=onset of interruption, and T4=end of mechanical interruption.
Mean PTP (for labial interruption at softest amplitude and all mechanical interruption trials) and/or Ps (for labial interruption at comfortable amplitude and all mechanical interruption trials) were calculated for each technique across the ten trials. Standard deviation and coefficient of variation (standard deviation divided by the mean) were also calculated. Coefficient of variation was used to reflect intrasubject variability in case there were differences among means of the different methods. Mean PTP and Ps and coefficient of variation of PTP and Ps were compared across the methods using repeated measures analysis of variance (ANOVA) with post-hoc comparisons using Tukey’s test. Repeated measures ANOVA on ranks were used if data did not meet assumptions of parametric testing. Pearson correlation test was performed to determine if mean PTP or coefficient of variation of PTP varied with age. A significance level of α=0.05 was used. SigmaPlot 13.0 (Systat, San Jose, CA) was used for statistical analyses and creation of figures.
RESULTS
Mean CAPE-V score was 1±2 on a scale of 1–100 and all subjects were judged not to have dysphonia perceptually.
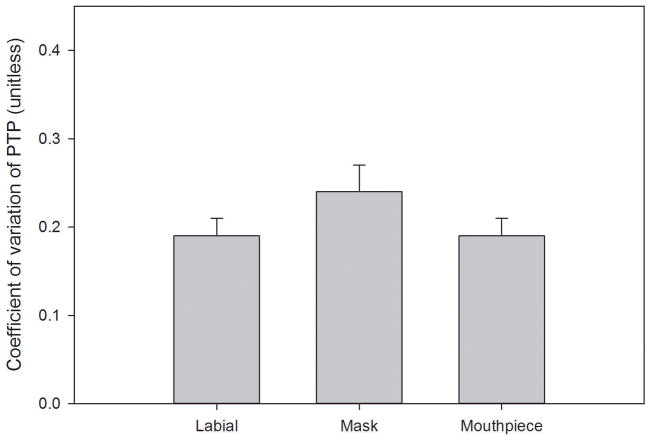
Summary data are presented in table 2. Mean PTP (F=21.086, p<0.001) and Ps (F=5.909, p=0.005) were different across methods. PTP was higher for labial trials compared to mechanical interruption with a mask (p<0.001) or mouthpiece (p<0.001) (figure 3). Ps was higher for labial compared to mechanical interruption with a mouthpiece (p=0.005). Ps and PTP were not different for the two methods of mechanical interruption. Coefficient of variation for PTP (repeated measures ANOVA on ranks, χ2=1.182, p=0.554) and Ps (F=1.221, p=0.305) did not differ significantly across the three methods (figure 4).
Table 2.
Summary data.
| Parameter | Labial interruption | Mechanical-mask | Mechanical-mouthpiece | p-value |
|---|---|---|---|---|
| Mean PTP (cmH2O) | 4.05 ± 0.87 | 2.81 ± 1.16 | 2.59 ±1.12 | <0.001 |
| CV of PTP (unitless) | 0.19 ± 0.11 | 0.24 ± 0.16 | 0.20 ± 0.10 | 0.554 |
| Mean Ps (cmH2O) | 7.72 ± 1.94 | 6.61 ± 1.62 | 6.14 ± 1.83 | 0.005 |
| CV of Ps (unitless) | 0.13 ± 0.06 | 0.12 ± 0.04 | 0.11 ± 0.05 | 0.305 |
PTP = phonation threshold pressure; Ps = subglottal pressure at comfortable amplitude; CV = coefficient of variation. For labial interruption, trials for Ps were performed at comfortable amplitude and trials for PTP were performed at softest possible amplitude. Values are presented as mean ± standard deviation. P-values represent results of repeated measures analysis of variance testing.
Figure 3.
Comparison of mean phonation threshold pressure (PTP) across the three methods. Mean PTP was higher for labial interruption compared to either mechanical interruption method. Bars represent mean and error bars represent standard error of the mean.
Figure 4.
Comparison of coefficient of variation (standard deviation divided by the mean) of phonation threshold pressure (PTP) across the three methods. There was no significant difference observed. Bars represent mean and error bars represent standard error of the mean.
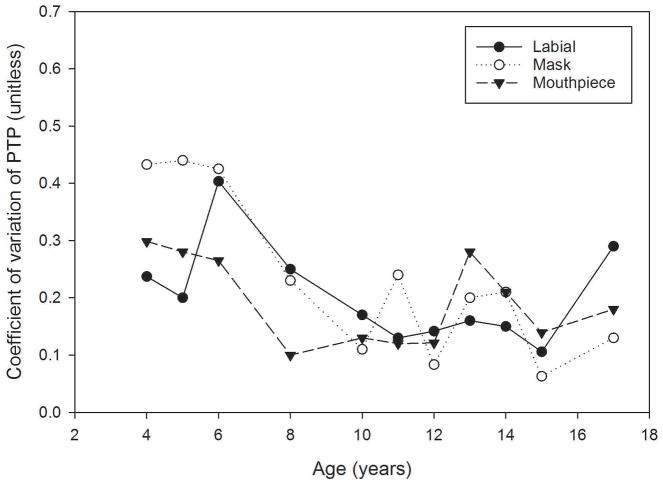
There was no correlation between age and mean PTP for labial interruption (r=−0.281, p=0.206) or mechanical interruption with a mask (r=0.169, p=0.452) or mouthpiece (r=0.0423, p=0.852). There was an inverse correlation between coefficient of variation of PTP and mechanical interruption with a mask (r=−0.628, p=0.00175). There was no correlation between age and coefficient of variation of PTP for labial interruption (r=−0.174, p=0.438) or mechanical interruption with a mouthpiece (r=−0.267, p=0.230) (figure 5).
Figure 5.
Evaluation of coefficient of variation of phonation threshold pressure (PTP) across age for each method. A significant correlation was observed only for mechanical interruption trials with a mask.
DISCUSSION
This is the first study applying mechanical interruption for measurement of PTP in children and the first comparing measurement reliability of PTP for labial and mechanical interruption methods in children. As predicted, mean PTP was different for labial interruption versus mechanical interruption. This is likely due to differences in task and timing of measurement. For labial interruption, subjects phonate as quietly as possible and PTP is estimated as the Ps at that amplitude. This has the advantage of not requiring additional computations other than those usually used for Ps. It has disadvantages of requiring separate trials for estimation of PTP and Ps at comfortable amplitude and also relying on subjects to phonate consistently at their truly softest amplitude which was difficult for younger subjects. In this study, we ensured subjects achieved lowest possible phonation both subjectively by monitoring volume during and across trials and instructing the subject to lower amplitude as much as possible, and quantitatively by ensuring that the minimum sound pressure level was maintained across trials. However, difficulty achieving or maintaining that lowest possible amplitude is an inherent limitation of the labial interruption technique.
Measurement of PTP via labial interruption represents an onset PTP. As has been demonstrated in theoretical, physical, and excised larynx models,9,23–25 PTP exhibits a hysteresis effect, where higher pressure is required to initiate phonation than to sustain it. There has been one study examining this phenomenon in human subjects.32 Five healthy volunteers underwent direct measurement of Ps via cricothyroid membrane puncture. Two subjects exhibited a significant hysteresis effect, while two were equivocal, and one showed higher offset than onset pressure. Of note, there were difficulties in the experiment with needle plugging, limiting data collection. Considering the strong theoretical basis as well as the data from well-controlled excised larynx experimentation, the hysteresis phenomenon appears real and certainly could have contributed to at least part of the disparity in PTP values observed in this study.
Additional factors which may contribute to lower observed mean PTP for mechanical interruption are increased subject effort or air leak during an interruption. Estimation of PTP via mechanical interruption requires identification of phonation offset within the interruption. Increased subject effort at interruption onset could result in delayed phonation offset and thus a lower estimation of PTP. Evaluation of auditory traces for a steady decrease helped mitigate this potential issue. Determination of phonation offset using electroglottography (EGG) will be explored in the future.33
Interestingly, mean Ps at comfortable amplitude was also different between labial and mechanical interruption. Each approach has previously been shown to be accurate via simultaneous indirect and direct Ps measurement.17,20 The difference is likely related to the difference in task, with increased pressure created with lip closure required for /pα/ compared to the open mouth required for /α/. Alternative explanations include differences in sound pressure level, though this was kept consistent across methods within each subject. The 150 ms time constant used in Ps estimation for mechanical interruption could potentially be too short; however, this has been demonstrated previously in mathematical and physical models as well as human subjects to be appropriate.31 As Ps was measured at 150 ms, the use of a 250 ms instead of the usual 500 ms interruption during mechanical interruption should not affect measurement; future studies will focus on optimizing interruption duration.
Overall, intrasubject variability for each method was relatively low, approximately 10–13% of the mean for Ps and 19–24% for PTP. Evaluating mechanical interruption alone, variability tended to be higher for trials with a mask than a mouthpiece. Obtaining a perfect seal for labial interruption is not as essential due to use of the intra-oral pressure tube; it is also easier as the subject is controlling the interruption. For mechanical interruption, obtaining a perfect seal is more challenging (due to the external, device-controlled, interruption) and more important to its success (as the subject produces the sustained vowel with an open mouth and thus no intra-oral pressure tube is used). Though different sized masks were available, air leak occurred in a minority of trials, more commonly in younger subjects. If an air leak is present, the phonation offset will either be unclear or not occur. Using a mouthpiece can circumvent this issue. Application of cheek restraints (constant pressure applied to the subject’s cheeks to prevent expansion during the interruption and possible leak around the mask or mouthpiece) could also be evaluated.
Interestingly, a correlation between age and coefficient of variation for PTP measurement was only observed with mechanical interruption using a mask. This is likely related to the aforementioned issues with mask seal and air leak. The lack of a relationship with age for labial interruption and mechanical interruption using a mouthpiece, coupled with the overall reasonable intrasubject variability, suggest that routine clinical measurement of PTP in children is feasible and reliable. PTP is a sensitive indicator of laryngeal biomechanics and the ability of the larynx to function as an energy transducer to produce voice. This study demonstrates that it can be measured in children as young as four with acceptable measurement precision, which is clinically valuable.
Limitations in this study include a low number of subjects at each specific age; this limits our ability to draw strong conclusions on effects of age and intrasubject variability. A prior study by Weinrich et al. presenting normative data for the Phonatory Aerodynamic System used labial interruption to measure mean Ps in 30 male and 30 female pediatric subjects (Weinrich 2013). This demonstrated a trend for decreasing mean Ps with increasing age, though this was not statistically significant. In our study, we did not identify a relationship between mean PTP and age. As vocal fold thickness increases during puberty in males secondary to inferomedial thyroarytenoid hypertrophy (Titze 2000), and vocal fold thickness is related to PTP (Titze 1995), differences in PTP between males and females around the time of puberty may emerge. Evaluation of this potential phenomenon will be the focus of future studies with a larger number of subjects. Second, subjects were asked to phonate at a comfortable rather than standardized sound pressure level. While feedback during trials helped confirm sound pressure level was fairly consistent within a subject across methods, this could contribute to variability in mean measurements across subjects. Third, subjects with dysphonia were not included. This study was intended to confirm that measurement of PTP in healthy subjects was reliable; follow-up investigations will focus on measurement of PTP in children with voice disorders. Real-time visual feedback of sound pressure level and airflow were provided to subjects in this study; evaluation of auditory masking34 may further decrease intra-subject variability.
CONCLUSION
PTP and Ps can be measured reliably in pediatric subjects using either mechanical or labial interruption. If mechanical interruption is used, it is preferable to use a mouthpiece rather than a mask. Documenting the method used for data collection is important, as mean values differ for techniques based on voice task and whether onset versus offset threshold pressure is measured. Clinical measurement of PTP is feasible and may offer valuable quantitative insight into laryngeal function.
Acknowledgments
This study was funded by NIH grant number R01 DC008153 from the National Institute on Deafness and other Communicative Disorders and the Diane M. Bless Endowed Chair, Division of Otolaryngology-Head and Neck Surgery at University of Wisconsin-Madison.
Funding: This study was funded by NIH grant number R01 DC008153 from the National Institute on Deafness and other Communicative Disorders and the Diane M. Bless Endowed Chair, Division of Otolaryngology-Head and Neck Surgery at University of Wisconsin-Madison.
Footnotes
Conflicts of interest: Jack J. Jiang held a patent on the mechanical interruption device used in this study that has since expired; he has not received any financial benefit from it.
This study was presented as a poster at the American Broncho-Esophagological Assocation Annual Meeting at National Harbor, Maryland, April 18–22, 2018.
Level of evidence: 3b
References
- 1.Bhattacharyya N. The prevalence of pediatric voice and swallowing problems in the United States. Laryngoscope. 2015;125:746–50. doi: 10.1002/lary.24931. [DOI] [PubMed] [Google Scholar]
- 2.Carding PN, Roulstone S, Northstone K ALSPAC Study Team. The prevalence of childhood dysphonia: A cross-sectional study. J Voice. 2006;20(4):623–30. doi: 10.1016/j.jvoice.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Mornet E, Coulombeau B, Fayoux P, et al. Assessment of chronic childhood dysphonia. Eur Ann Otorhinolaryngol Head Neck Dis. 2014;131(5):309–12. doi: 10.1016/j.anorl.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Connor N, Cohen SB, Theis SM, et al. Attitudes of children with dysphonia. J Voice. 2008;22(2):197–209. doi: 10.1016/j.jvoice.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 5.Cohen W, Wynne D, Kubba H, et al. Development of a minimal protocol for assessment in the paediatric voice clinic. Part 1: evaluating vocal function. Logopedics Phoniatr Vocol. 2012;37:33–8. doi: 10.3109/14015439.2011.638670. [DOI] [PubMed] [Google Scholar]
- 6.Smillie I, McManus K, Cohen W, Lawson E, Wynne DM. The paediatric voice clinic. Arch Dis Child. 2014;99:912–5. doi: 10.1136/archdischild-2013-305683. [DOI] [PubMed] [Google Scholar]
- 7.Brehm SB, Weinrich B, Zieser M, et al. Internat J Pediatr Otorhinolaryngol. 2009;73:1019–23. doi: 10.1016/j.ijporl.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Titze IR. The physics of small-amplitude oscillation of the vocal folds. J Acoust Soc Am. 1988;83:1536–52. doi: 10.1121/1.395910. [DOI] [PubMed] [Google Scholar]
- 9.Titze IR, Schmidt SS, Titze MR. Phonation threshold pressure in a physical model of the vocal fold mucosa. J Acoust Soc Am. 1995;97:3080–4. doi: 10.1121/1.411870. [DOI] [PubMed] [Google Scholar]
- 10.Solomon NP, DiMattia MS. Effects of a vocally fatiguing task and systemic hydration on phonation threshold pressure. J Voice. 2000;14:341–62. doi: 10.1016/s0892-1997(00)80080-6. [DOI] [PubMed] [Google Scholar]
- 11.Rousseau B, Sohn J, Montequin DW, Tateya I, Bless DM. Functional outcomes of reduced hyaluronan in acute vocal fold scar. Ann Otol Rhinol Laryngol. 2004 Oct;113(10):767–76. doi: 10.1177/000348940411301001. [DOI] [PubMed] [Google Scholar]
- 12.Jiang J, Stern J. Receiver operating characteristic analysis of aerodynamic parameters obtained by airflow interruption: A preliminary report. Ann Otol Rhinol Laryngol. 2004;113(12):961–6. doi: 10.1177/000348940411301205. [DOI] [PubMed] [Google Scholar]
- 13.Verdolini K, Titze IR, Fennell A. Dependence of phonatory effort on hydration level. J Speech Hear Res. 1994;37:1001–7. doi: 10.1044/jshr.3705.1001. [DOI] [PubMed] [Google Scholar]
- 14.Jiang J, Verdolini K, Aquino B, Ng J, Hanson D. Effects of dehydration on phonation in excised canine larynges. Ann Otol Rhinol Laryngol. 2000 Jun;109(6):568–75. doi: 10.1177/000348940010900607. [DOI] [PubMed] [Google Scholar]
- 15.Plexico LW, Sandage MJ, Faver KY. Assessment of phonation threshold pressure: A critical review and clinical implications. Am J Speech Lang Pathol. 2011 Nov;20:348–66. doi: 10.1044/1058-0360(2011/10-0066). [DOI] [PubMed] [Google Scholar]
- 16.Smitheran JR, Hixon TJ. A clinical method for estimating laryngeal airway resistance during vowel production. J Speech Hear Disord. 1981;46:138–46. doi: 10.1044/jshd.4602.138. [DOI] [PubMed] [Google Scholar]
- 17.Lofqvist A, Carlborg B, Kitzing P. Initial validation of an indirect measure of subglottal pressure during vowels. J Acoust Soc Am. 1982;72:633–5. doi: 10.1121/1.388046. [DOI] [PubMed] [Google Scholar]
- 18.Hertegard S, Guaffin J, Lindestad PA. A comparison of subglottal and intraoral pressure measurements during phonation. J Voice. 1995;9:149–55. doi: 10.1016/s0892-1997(05)80248-6. [DOI] [PubMed] [Google Scholar]
- 19.Bard MC, Slavit DH, McCaffrey TV, Lipton RJ. Noninvasive technique for estimating subglottic pressure and laryngeal efficiency. Ann Otol Rhinol Laryngol. 1992;101:578–82. doi: 10.1177/000348949210100706. [DOI] [PubMed] [Google Scholar]
- 20.Jiang J, O’Mara T, Conley D, Hanson D. Phonation threshold pressure measurements during phonation by airflow interruption. Laryngoscope. 1999;109:425–32. doi: 10.1097/00005537-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Jiang J, O’Mara T, Chen HJ, et al. Aerodynamic measurements of patients with Parkinson’s disease. J Voice. 1999;13:583–91. doi: 10.1016/s0892-1997(99)80012-5. [DOI] [PubMed] [Google Scholar]
- 22.Chapin WJ, Hoffman MR, Rieves AL, Jiang JJ. Comparison of labial and mechanical interruption for measurement of aerodynamic parameters. J Voice. 2011;25(3):337–41. doi: 10.1016/j.jvoice.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Regner MF, Tao C, Zhuang P, Jiang JJ. Onset and offset phonation threshold flow in excised canine larynges. Laryngoscope. 2008;118:1313–7. doi: 10.1097/MLG.0b013e31816e2ec7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lucero JC. The minimum lung pressure to sustain vocal fold oscillation. J Acoust Soc Am. 1995;98(2):779–84. doi: 10.1121/1.414354. [DOI] [PubMed] [Google Scholar]
- 25.Lucero JC. A theoretical study of the hysteresis phenomenon at vocal fold oscillation onset-offset. J Acoust Soc Am. 1999;105(1):423–31. doi: 10.1121/1.424572. [DOI] [PubMed] [Google Scholar]
- 26.Weinrich B, Salz B, Hughes M. Aerodynamic measurements: Normative data for children ages 6:0 to 10:11 years. J Voice. 2005;19(3):326–39. doi: 10.1016/j.jvoice.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 27.McAllister A, Sundberg J. Data on subglottal pressure and SPL at varied vocal loudness and pitch in 8- to 11-year-old children. J Voice. 1998;12(2):166–74. doi: 10.1016/s0892-1997(98)80036-2. [DOI] [PubMed] [Google Scholar]
- 28.Stathopoulos ET, Sapienza C. Respiratory and laryngeal measures of children during vocal intensity variation. J Acoust Soc Am. 1993;94(5):2531–43. doi: 10.1121/1.407365. [DOI] [PubMed] [Google Scholar]
- 29.Hsu HW, Fang TJ, Lee LA, et al. Multidimensional evaluation of vocal quality in children with cochlear implants: a cross-sectional, case-controlled study. Clin Otolaryngol. 2014;39:32–8. doi: 10.1111/coa.12213. [DOI] [PubMed] [Google Scholar]
- 30.Kempster GB, Gerratt BR, Verdolini Abbott K, Barkmeier-Kraemer J, Hillman RE. Consensus auditory-perceptual evaluation of voice: Development of a standardized clinical protocol. Am J Speech Lang Pathol. 2009 May;18:124–32. doi: 10.1044/1058-0360(2008/08-0017). [DOI] [PubMed] [Google Scholar]
- 31.Hoffman MR, Baggott CD, Jiang J. Reliable time to estimate subglottal pressure. J Voice. 2009 Mar;23(2):169–74. doi: 10.1016/j.jvoice.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Plant RL, Freed GL, Plant RE. Direction measurement of onset and offset phonation threshold pressure in normal subjects. J Acoust Soc Am. 2004;116:3640–3646. doi: 10.1121/1.1812309. [DOI] [PubMed] [Google Scholar]
- 33.Rieves AL, Regner MF, Jiang JJ. Phonation threshold pressure estimation using electroglottography in an airflow redirection system. Laryngoscope. 2009;119:2378–83. doi: 10.1002/lary.20611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoffman MR, Jiang JJ. Estimating subglottal pressure via airflow interruption with auditory masking. J Voice. 2009 Nov;23(6):653–7. doi: 10.1016/j.jvoice.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]