Abstract
Several extra-articular surgical techniques in addition to anterior cruciate ligament reconstruction have been proposed to better restore rotational instability of the knee. One option is surgical repair of the anterolateral ligament in acute cases to achieve an anatomic reconstruction. An additional augmentation to the repair could allow a load-sharing—and thus protective—effect for the repair during the healing process. The purpose of this Technical Note is to describe a primary repair of the anterolateral ligament with suture tape augmentation (Internal Brace; Arthrex, Naples, FL) in a patient with an acute anterior cruciate ligament tear.
Anterior cruciate ligament (ACL) tears are common sports-related injuries, and reconstruction has been the gold standard for the operative management of an ACL rupture for many years. However, only 63% to 65% of patients who undergo ACL reconstruction after rupture return to their preinjury level of sport, and at least 10.3% have a graft failure by 10 years.1 Owing to these suboptimal outcomes, a renewed interest has developed in the role of the anterolateral structures of the knee in controlling rotatory laxity, as well as their load-sharing properties in conjunction with the ACL graft.2, 3, 4
Recent surgical and imaging studies have shown that the incidence of anterolateral ligament (ALL) injuries associated with ACL tears is about 90% of cases.5 Extra-articular tenodesis surgical techniques have previously been proposed; however, the nonanatomic lateral extra-articular reconstruction techniques have led to concerns about overconstraint of the joint due to altered biomechanics.6 Recently, advancements in the understanding of the anatomy, histology, and biomechanics of the anterolateral aspect of the knee have led to the development of the anatomic ALL reconstruction.7, 8, 9 Surgical repair of the ALL is an option to achieve an anatomic reconstruction in an acute ACL rupture; furthermore, the addition of augmentation of the ALL repair with an internal brace can provide load-sharing and protective properties to the repair and reconstruction. ALL repair with an internal brace will improve rotational stability of the knee and hasten postoperative rehabilitation after ACL reconstruction. The aim of this Technical Note is to present an open technique for ALL repair and augmentation with a suture tape (Video 1).
Surgical Technique
General Preparation
All patients are counseled and consented for ACL reconstruction with ALL repair and/or reconstruction. Patients receive standard preoperative antibiotics and regional anesthesia and are placed in the supine position. Examination under anesthesia is performed on both knees to confirm the injuries of the affected leg. Finally, a tourniquet is applied around the proximal thigh, and the leg is prepared and draped in a sterile fashion.
ACL Reconstruction
An initial diagnostic arthroscopy is performed using standard anterolateral and anteromedial portals. After the preliminary arthroscopy, an oblique 3-cm skin incision is created at the level of the pes anserinus, and the semitendinosus and gracilis tendons are identified and harvested using a closed-eyelet tendon stripper. The 2 tendons are prepared using No. 2 Vicryl suture (Ethicon, Somerville, NJ) with a Bunnell suture technique on both ends of each tendon. The graft is doubled, and the diameter is measured. The femoral end of the graft is marked, and an ACL TightRope (Arthrex, Naples, FL) is placed on the graft. A standard tibial guide is set at 60° and placed at the center of the anatomic footprint of the ACL. The tibial tunnel is drilled in an outside-in manner using a fully threaded drill with the same diameter as the doubled semitendinosus and gracilis graft. On the femoral side, a 25-mm-long bone socket is drilled using an outside-in technique with the Arthrex footprint guide and drill sleeve set at approximately 100° to 110°. The femoral bone tunnel diameter is set using the same doubled semitendinosus and gracilis diameter and drilled with the Flipcutter Retrodrill (Arthrex). By use of a shuttle suture, the graft is passed through the tibial tunnel to the femoral socket and then fixed with the ACL TightRope on the femoral side and a bioabsorbable screw (Bio-Interference Screw; Arthrex) on the tibia, sized 1 mm greater than the graft diameter and 28 or 35 mm in length.
ALL Repair and Augmentation With Suture Tape
With the knee at 90° of flexion, a 4- to 5-cm-long hockey-stick incision is performed on the lateral aspect of the knee from the lateral femoral condyle to the Gerdy tubercle (Fig 1, Video 1). Of note, the peroneal nerve is located distal to the surgical field and is not in danger during the procedure. After dissection of the skin and subcutaneous tissue, the iliotibial tract (ITT) is visualized. The ITT is incised in line with its fibers to expose the anterolateral capsule. The ALL lesion and capsule are visualized and repaired according to the type of lesion. The first 2.4-mm K-wire is placed at the anatomic tibial insertion of the ALL (Fig 2), midway between the Gerdy tubercle and the fibular head. This point is consistently located approximately 22 mm from the center of the Gerdy tubercle and 11 mm below the joint line.1, 10 After identification of the lateral collateral ligament and popliteus tendon, the femoral anatomic insertion of the ALL is located. The point is positioned just proximal and posterior to the lateral femoral epicondyle, where a second 2.4-mm K-wire is inserted (Fig 2). Interference with the femoral ACL tunnel should be carefully avoided. A suture is looped around the 2 K-wires to check tension during range of motion between 0° and 90° of flexion (Fig 3). The aim is to obtain a bundle that reproduces the ALL biomechanics and is tight in extension and slack in flexion (Sonnery-Cottet et al.6). The K-wires are repositioned if tensioning is determined to be inappropriate. A 4.5-mm-diameter bone socket is drilled on the tibial side over the K-wire, measuring 20 mm in depth. A No. 2 Arthrex FiberTape suture (Internal Brace) is then loaded onto a 4.75-mm-diameter knotless anchor (SwiveLock; Arthrex) and fixed into the tibial bone socket under the ITT (Figs 4 and 5). The FiberWire suture (Arthrex) from the SwiveLock anchor is used for a direct, anatomic repair of the ALL and capsule at their tibial insertion. Next, a 4.5-mm-diameter bone socket is drilled on the femoral side, measuring 20 mm in depth. The FiberTape originating from the tibial anchor is loaded onto a second 4.75-mm-diameter knotless anchor (SwiveLock) (Fig 6). The knee is placed in full extension, and the FiberTape is fixed on the femoral side with manual tension (Fig 7). The final construct consists of an anatomic ALL and capsular repair with a FiberTape Internal Brace fixed on the ALL tibial and femoral insertions. The construct is then checked during range of motion between 0° and 90° of flexion to confirm the absence of overconstraint of the knee. The ITT is closed with No. 0 Vicryl, and the skin is closed in a standard fashion.
Fig 1.
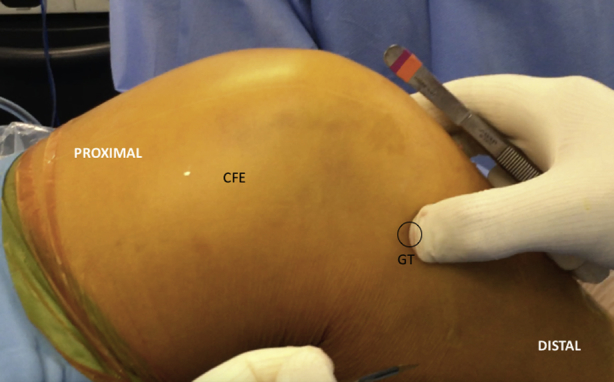
An incision is performed from the epicondylus to midway between the Gerdy tubercle (GT) and fibular head. (CFE, external femoral condyle.)
Fig 2.

The first 2.4-mm K-wire is placed at the anatomic tibial insertion of the ALL, midway between the Gerdy tubercle and the fibular head. The second 2.4-mm K-wire is inserted at the femoral insertion of the ALL, located just proximal and posterior to the lateral femoral epicondyle. (FI, femoral insertion; TI, tibial insertion.)
Fig 3.
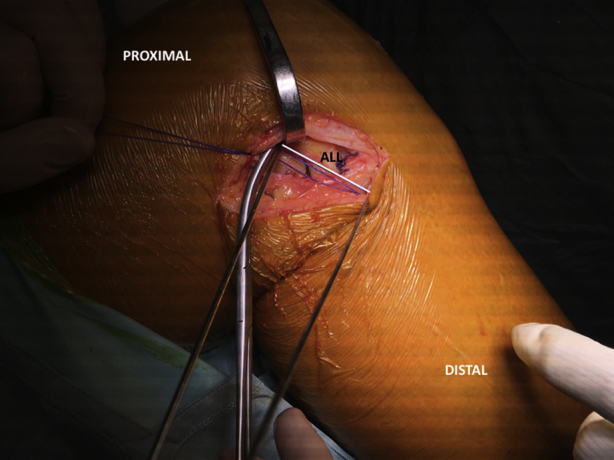
Tension is checked with suture passed over the 2 K-wires. The goal is a graft that is tight in extension and slack in flexion. (ALL, anterolateral ligament.)
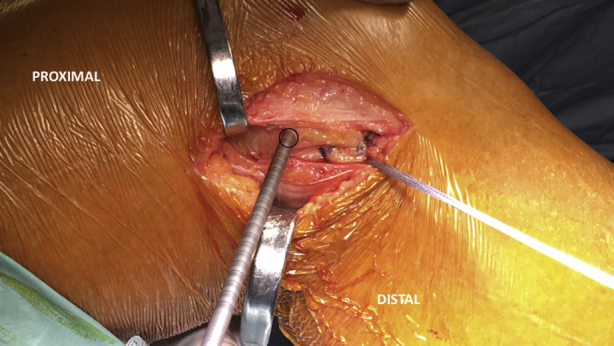
Fig 4.
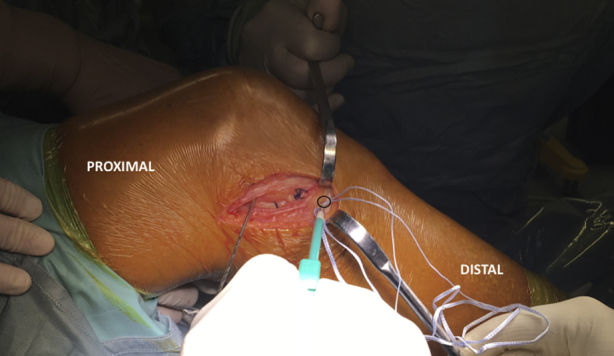
The tibial hole is drilled, measuring 4.5 mm in diameter and 20 mm in depth with regular flute length. The 4.75-mm-diameter SwiveLock anchor is fixed on the tibial side.
Fig 5.
The FiberTape and the FiberWire coming from the anchor are passed under the tibial part of the iliotibial tract (ITT).
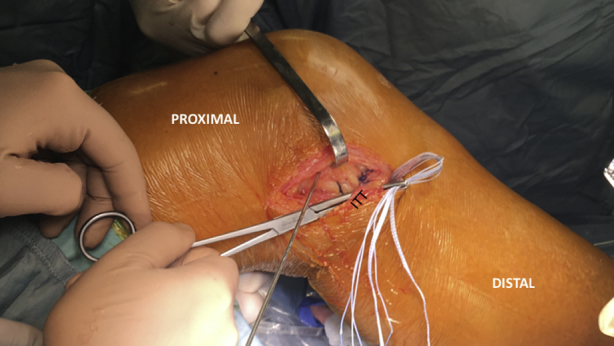
Fig 6.
The femoral hole is drilled, measuring 4.5 mm in diameter and 20 mm in depth with regular flute length, avoiding convergence with the femoral anterior cruciate ligament socket.
Fig 7.
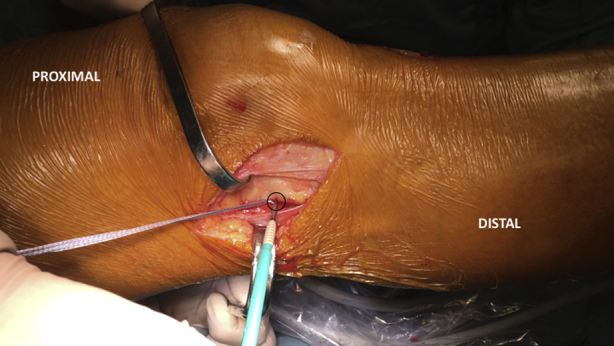
The 4.75-mm-diameter SwiveLock anchor is fixed on the femoral side under manual tension of the tape with the knee in full extension.
Rehabilitation
Immediately postoperatively, the knee is placed in full extension with a locked brace that is worn for 2 weeks. Weight bearing in the locked brace is allowed the day after surgery. Continuous passive motion between 0° and 90° is initiated the day after surgery, with a goal of reaching full range of motion within 4 weeks. Physical therapy is begun at 2 weeks after surgery, focusing on early range of motion, muscle control, and restoration of function. The brace is removed at 2 weeks postoperatively. Patients begin sport-specific training at 3 months. Pivoting sports are allowed if the neuromuscular function has recovered, which usually occurs within 6 months.
Discussion
Despite the adequate clinical results of ACL reconstruction techniques that have been reported, concerns remain about the ability to fully control the pivot-shift phenomenon.11 The role of secondary restraints in the lateral aspect of the knee has been clearly shown, and several lateral extra-articular procedures have been proposed, which take advantage of the long lever arm to act as a lateral tenodesis.12, 13, 14 We therefore report a technique that incorporates anatomic repair of the structures on the anterolateral aspect of the knee with a suture tape augmentation to provide improved control of the pivot shift after ACL reconstruction without overconstraint of the knee.
The ALL has been described as a distinct structure located proximally and posteriorly to the lateral femoral epicondyle and extending to a point midway between the Gerdy tubercle and fibular head on the tibia.2 The biomechanical role of this ligamentous structure in controlling rotational stability of the knee and the pivot-shift phenomenon, as well as the role of its anatomic reconstruction, has recently been shown by several navigated studies.4, 15 Ferretti et al.5 furthermore noted that in 90% of cases in which a systematic exposure of the lateral compartment was performed at the time of acute ACL reconstruction, a visible injury to the secondary anterolateral restraints was noted. These findings are consistent with historical results reported when a lateral incision was standardly performed during historical open, double-incision ACL reconstructions.16, 17, 18 A similar prevalence of injury to the secondary restraints was documented using magnetic resonance imaging in acute ACL tears.19
Clinical studies have supported the repair and reconstruction of these lateral structures of the knee in conjunction with anatomic ACL reconstruction. Sonnery-Cottet et al.6 showed that ACL reconstruction with an additional ALL reconstruction using hamstring autograft had good clinical outcomes and, significantly, a reduction in the failure rate at 2 years of follow-up. However, in recent years, techniques have shifted from nonanatomic procedures20, 21, 22 to procedures that attempt to reproduce the anatomy using soft-tissue grafts such as gracilis tendon and fascia lata grafts.6, 10, 23 However, the role of reconstructive surgery should be to replicate the anatomy. If an anatomic structure is torn, the goal should be to reconstruct its anatomy as closely to the native anatomy as possible.24
For this reason, acute repair of a ligamentous structure (rather than a replacement) should be considered an option to restore the normal anatomy. In addition, augmentation with an internal brace has been proposed to protect the ligament repair during the healing process, acting as a seat-belt support that would ensure the anatomic length of the ligament. Materials used for an internal brace must be safe, compatible, and robust enough to allow early mobilization. FiberTape is an ultrahigh-strength, 2-mm-wide tape with a similar structure to FiberWire suture. The tape provides broad compression and increased resistance to tissue cut through, making it an excellent choice for repair augmentation techniques.
The goal of this article is to describe a technique for repair of the ALL and augmentation with an internal brace. The aim of this technique is to obtain a stable knee and reduction of the pivot-shift phenomenon postoperatively. By protecting the ligament repair using an internal brace during the initial healing phase, an augmentation can support early mobilization and improved outcomes. In comparison to previously described extra-articular techniques—either nonanatomic, such as extra-articular reconstruction, or anatomic, such as ALL reconstruction—no additional graft is needed, which allows for decreased donor-site morbidity. The ligament is repaired and protected by an internal brace, which allows for restoration of joint biomechanics and avoidance of knee overconstraint. Moreover, the protective seat-belt effect of the internal brace can allow for earlier mobility, which can decrease the risk of knee arthrofibrosis after acute ACL reconstruction. In addition, ALL repair with internal brace augmentation leads to less postoperative pain and swelling in comparison to the extra-articular tenodesis techniques, thus allowing for earlier initiation of postoperative rehabilitation, beginning the day after surgery.
The proposed technique has some disadvantages (Table 1). A second skin incision is needed on the femoral side to expose the anterolateral capsule and allow direct visualization of the tear and its subsequent repair. With improvement of magnetic resonance imaging techniques and 3-T magnets for the diagnosis of ALL tears, it will be possible to understand the type of lesion and its extension. Understanding the characteristics of the lesion preoperatively can allow for the decision to perform a minimally invasive ALL internal brace procedure subcutaneously or to perform a second surgical approach for a direct repair. Concerning fixation, care must be taken to avoid confluence with the ACL tunnel on the femoral side. Finally, no clinical and radiologic results are reported in this article because we have only recently described the proposed technique and do not have adequate minimum follow-up to appropriately report clinical outcomes.
Table 1.
Indication, Advantages, and Disadvantages of ALL Reconstruction Using Internal Brace
Indications
|
Advantages
|
Disadvantages
|
ACL, anterior cruciate ligament; ALL, anterolateral ligament.
In conclusion, the ALL is an important secondary stabilizer of the ACL for controlling rotational stability of the knee and the pivot-shift phenomenon. A goal of ACL reconstruction is to reduce the pivot shift, which can be accomplished by evaluation and appropriate management of this secondary restraint. An option in acute ACL reconstruction is repair of the ALL to restore the ligament instead of reconstructing it. The addition of an ALL internal brace can protect the graft during the healing process, thus allowing for earlier rehabilitation.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
With the knee at 90° of flexion, a 4- to 5-cm-long hockey-stick incision is made on the lateral aspect of the knee, extending from the lateral femoral condyle to the Gerdy tubercle. The peroneal nerve is located distal to the surgical field and is not in danger during the procedure. After dissection of the skin and subcutaneous tissue, the iliotibial band is visualized and incised along its fibers to expose the anterolateral capsule. The lesions of the anterolateral ligament (ALL) and capsule are visualized and recorded. The injury is directly repaired according to the type of lesion. The first 2.4-mm K-wire is placed at the anatomic tibial insertion of the ALL, midway between the Gerdy tubercle and the fibular head. This point is located approximately 22 mm from the center of the Gerdy tubercle and 11 mm below the joint line. The lateral collateral ligament and popliteus tendon are first visualized and protected. Then, a second 2.4-mm K-wire is inserted at the femoral insertion of the ALL, located just proximal and posterior to the lateral femoral epicondyle. Any possible interference with the femoral anterior cruciate ligament (ACL) tunnel should be carefully avoided. Tension is then checked during range of motion between 0° and 90° of flexion. The aim is to obtain a bundle that is tight in extension and slack in flexion, which reproduces the function of the ALL. A bone socket measuring 20 mm in depth and 4.5 mm in diameter is drilled on the tibial side. A No. 2 FiberTape suture is loaded onto a 4.75-mm knotless anchor and fixed on the tibial side under the iliotibial tract. The 2 FiberWire sutures from the anchor and the 2 FiberTapes loaded onto the anchor are then used to repair the ALL and capsule on the tibial insertion using a free needle. Next, a bone socket measuring 20 mm in depth and 4.5 mm in diameter is drilled on the femoral side. The FiberTape from the previously placed tibial anchor is loaded onto a second 4.75-mm knotless anchor. The knee is then placed in full extension, and the FiberTape is fixed on the femoral side with manual tension. The final construct consists of an anatomic ALL repair with a FiberTape augmentation fixed on both the tibial and femoral anatomic insertions. The iliotibial tract is then sutured with No. 0 Vicryl, and the skin incision is closed in a standard fashion.
References
- 1.Anderson M.J., Browning W.M., III, Urband C.E., Kluczynski M.A., Bisson L.J. A systematic summary of systematic reviews on the topic of the anterior cruciate ligament. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116634074. 2325967116634074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LaPrade R.F. Editorial commentary: It is all about how one defines the anatomy. Arthroscopy. 2016;32:849–850. doi: 10.1016/j.arthro.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Roessler P.P., Schuttler K.F., Heyse T.J., Wirtz D.C., Efe T. The anterolateral ligament (ALL) and its role in rotational extra-articular stability of the knee joint: A review of anatomy and surgical concepts. Arch Orthop Trauma Surg. 2016;136:305–313. doi: 10.1007/s00402-015-2395-3. [DOI] [PubMed] [Google Scholar]
- 5.Ferretti A., Monaco E., Fabbri M., Maestri B., De Carli A. Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy. 2017;33:147–154. doi: 10.1016/j.arthro.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Sonnery-Cottet B., Barbosa N.C., Tuteja S., Daggett M., Kajetanek C., Thaunat M. Minimally invasive anterolateral ligament reconstruction in the setting of anterior cruciate ligament injury. Arthrosc Tech. 2016;5:e211–e215. doi: 10.1016/j.eats.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helito C.P., Demange M.K., Bonadio M.B. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med. 2013;1 doi: 10.1177/2325967113513546. 2325967113513546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daggett M., Busch K., Sonnery-Cottet B. Surgical dissection of the anterolateral ligament. Arthrosc Tech. 2016;5:e185–e188. doi: 10.1016/j.eats.2015.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pomajzl R., Maerz T., Shams C., Guettler J., Bicos J. A review of the anterolateral ligament of the knee: Current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy. 2015;31:583–591. doi: 10.1016/j.arthro.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Ferretti A., Monaco E., Fabbri M., Mazza D., De Carli A. The fascia lata anterolateral tenodesis technique. Arthrosc Tech. 2017;6:e81–e86. doi: 10.1016/j.eats.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferretti A., Monaco E., Vadalà A. Rotatory instability of the knee after ACL tear and reconstruction. J Orthop Traumatol. 2014;15:75–79. doi: 10.1007/s10195-013-0254-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson L.L. Lateral capsular ligament complex: Anatomical and surgical considerations. Am J Sports Med. 1979;7:156–160. doi: 10.1177/036354657900700302. [DOI] [PubMed] [Google Scholar]
- 13.Monaco E., Ferretti A., Labianca L. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20:870–877. doi: 10.1007/s00167-011-1640-8. [DOI] [PubMed] [Google Scholar]
- 14.Caterine S., Litchfield R., Johnson M., Chronik B., Getgood A. A cadaveric study of the anterolateral ligament: Re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2014;23:3186–3195. doi: 10.1007/s00167-014-3117-z. [DOI] [PubMed] [Google Scholar]
- 15.Rasmussen M.T., Nitri M., Williams B.T. An in vitro robotic assessment of the anterolateral ligament, part 1: Secondary role of the anterolateral ligament in the setting of an anterior cruciate ligament injury. Am J Sports Med. 2016;44:585–592. doi: 10.1177/0363546515618387. [DOI] [PubMed] [Google Scholar]
- 16.Ferretti A., Conteduca F., De Carli A., Fontana M., Mariani P.P. Results of reconstruction of the anterior cruciate ligament with the tendons of semitendinosus and gracilis in acute capsulo-ligamentous lesions of the knee. Ital J Orthop Traumatol. 1990;16:452–458. [PubMed] [Google Scholar]
- 17.Dodds A.L., Gupte C.M., Neyret P., Williams A.M., Amis A.A. Extra-articular techniques in anterior cruciate ligament reconstruction: A literature review. J Bone Joint Surg Br. 2011;93:1440–1448. doi: 10.1302/0301-620X.93B11.27632. [DOI] [PubMed] [Google Scholar]
- 18.Ferretti A., Monaco E., Wolf M.R., Guzzini M., Carli A., Mazza D. Surgical treatment of Segond fractures in acute anterior cruciate ligament reconstruction. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117729997. 2325967117729997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Helito C.P., Helito P.V., Bonadio M.B. Correlation of magnetic resonance imaging with knee anterolateral ligament anatomy: A cadaveric study. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115621024. 2325967115621024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lemaire M. Rupture ancienne du ligament croisé antérieur du genou. J Chir. 1967;93:311–320. [Google Scholar]
- 21.Galway R.D., Beaupre A., MacIntosh D.L. Pivot shift: A clinical sign of symptomatic anterior cruciate insufficiency. J Bone Joint Surg Br. 1972;54:763–764. [Google Scholar]
- 22.Slocum D.B., Larson R.L. Pes anserinus transplantation. J Bone Joint Surg Am. 1968;50:226–242. [PubMed] [Google Scholar]
- 23.Helito C.P., Bonadio M.B., Gobbi R.G. Combined intra- and extra-articular reconstruction of the anterior cruciate ligament: The reconstruction of the knee anterolateral ligament. Arthrosc Tech. 2015;4:e239–e244. doi: 10.1016/j.eats.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Musahl V., Rahnemai-Azar A.A., van Eck C.F., Guenther D., Fu F.H. Anterolateral ligament of the knee, fact or fiction? Knee Surg Sports Traumatol Arthrosc. 2016;24:2–3. doi: 10.1007/s00167-015-3913-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
With the knee at 90° of flexion, a 4- to 5-cm-long hockey-stick incision is made on the lateral aspect of the knee, extending from the lateral femoral condyle to the Gerdy tubercle. The peroneal nerve is located distal to the surgical field and is not in danger during the procedure. After dissection of the skin and subcutaneous tissue, the iliotibial band is visualized and incised along its fibers to expose the anterolateral capsule. The lesions of the anterolateral ligament (ALL) and capsule are visualized and recorded. The injury is directly repaired according to the type of lesion. The first 2.4-mm K-wire is placed at the anatomic tibial insertion of the ALL, midway between the Gerdy tubercle and the fibular head. This point is located approximately 22 mm from the center of the Gerdy tubercle and 11 mm below the joint line. The lateral collateral ligament and popliteus tendon are first visualized and protected. Then, a second 2.4-mm K-wire is inserted at the femoral insertion of the ALL, located just proximal and posterior to the lateral femoral epicondyle. Any possible interference with the femoral anterior cruciate ligament (ACL) tunnel should be carefully avoided. Tension is then checked during range of motion between 0° and 90° of flexion. The aim is to obtain a bundle that is tight in extension and slack in flexion, which reproduces the function of the ALL. A bone socket measuring 20 mm in depth and 4.5 mm in diameter is drilled on the tibial side. A No. 2 FiberTape suture is loaded onto a 4.75-mm knotless anchor and fixed on the tibial side under the iliotibial tract. The 2 FiberWire sutures from the anchor and the 2 FiberTapes loaded onto the anchor are then used to repair the ALL and capsule on the tibial insertion using a free needle. Next, a bone socket measuring 20 mm in depth and 4.5 mm in diameter is drilled on the femoral side. The FiberTape from the previously placed tibial anchor is loaded onto a second 4.75-mm knotless anchor. The knee is then placed in full extension, and the FiberTape is fixed on the femoral side with manual tension. The final construct consists of an anatomic ALL repair with a FiberTape augmentation fixed on both the tibial and femoral anatomic insertions. The iliotibial tract is then sutured with No. 0 Vicryl, and the skin incision is closed in a standard fashion.


