Abstract
Objective
The aim of this study was to evaluate the results of fixator assisted correction of the distal femoral valgus deformities and the precision of the correction.
Methods
Seventeen extremities of 13 patients (7 women and 6 men; mean age: 16 ± 5.4 years) who had fixator assisted plating of the distal femur for genu valgum deformity were evaluated. Mechanical axis deviation (MAD) and mechanical lateral distal femoral angles (mLDFA) were measured pre-operatively and post-operatively. mLDFA was graded as perfect if it is between 85° and 90°(85° ≤ x ≤ 90°); overcorrection if it is between 91° and 95° (91° ≤ x ≤ 95°) and undercorrection if it is between 80° and 85° (80° ≤ x < 85°). Measurements beyond those limits were graded as a poor result. The position of the mechanical axis line with respect to center of the knee was graded from zone 1 to zone 4 pre-operatively and post-operatively.
Results
The mean follow-up period was 12.8 ± 3.7 months. The pre-operative and post-operative mLDFA was 70.5°±9.4° (range, 57°–82°) and 87.7° ± 3.5° (range, 80°–94°), respectively (p < 0.001). Based on post-operative standing radiographs, the correction was graded perfect in 12 femurs. The correction in three femurs were graded as overcorrection and graded as undercorrection in two femurs. Sagittal plane correction was also achieved in two femurs. Peroneal nerve decompression was done in three patients (5 extremities) with valgus deformity over 30°. The mechanical axes in all lower extremities were passing through zone 2 or more, pre-operatively, whereas the mechanical axes were in zone 2 or more in five extremities post-operatively.
Conclusion
Fixator assisted plating is an effective treatment modality in patients with distal femoral valgus deformity. Although the technique enables to obtain significant correction in coronal plane it has the disadvantages of over- and undercorrection. Thus, we advise intraoperative confirmation of the correction under fluoroscopic control.
Level of Evidence: Level IV Therapeutic Study.
Keywords: Fixator assisted plating, Femur osteotomy, Genu valgum, Valgus deformity, Deformity Correction
Introduction
The deformities effecting the long bones of the lower extremity may emerge from variety of reasons including trauma sequela, metabolic disorders, skeletal dysplasias, infection and congenital limb deficiencies. Long term effect of malalignment in lower extremity is unpredictable. The valgus and varus deformities may predispose to pain, knee instability, ligament injury and cartilage degeneration. In addition, those deformities around the knee may deteriorate ambulatuar capacity of an individual patient.1, 2, 3
Several treatment options exist for distal femur deformities including growth guided surgery, osteotomy and external fixation or internal fixation. Guided growth utilizing staples or tension band plating is an effective method in patients with open growth plates.4 Although good results have been reported with guided growth in patients having enough growth potential with mild to moderate deformities, the efficacy of the technique has been questioned in obese patients, in patients whose growth plates are close to maturity and in patients with severe mechanical axis deviation.5 Osteotomy and gradual correction through circular frames (ilizarov/hexapod frames) is the treatment of choice in patients who has multiplanar deformities along with limb length inequality. External fixation systems have their own drawbacks including pin site infections, knee stiffness and the discomfort related to frame itself.6, 7
Fixator assisted distal femur correction and retrograde intramedullary nailing has been applied in patients with closed growth plates.8 Since the intramedullary rod violates the growth plates, this technique is not recommended in pediatric age group. Fixator assisted distal femur osteotomy and internal fixation is another option for femur deformities. Good results has been reported utilizing temporary external fixation in order to achieve and maintain correction and then fixation of the osteotomy site with a locking distal femur plate.9 Eidelman et al recommended that the technique shouldn't be used in patients with open growth plates and multiapical deformities. As opposed to original technique we have been using the fixator assisted correction and plating for distal femoral uniplanar and biplanar deformities in pediatric (open growth plates) and adult age group. We report the early clinical and radiological results of these patients in the current study emphasizing on the accuracy of the correction.
Materials and method
This retrospective study was approved by University Ethics Commission. 13 patients (17 extremities) who had fixator assisted plating of the distal femur for genu valgum deformity were evaluated. Pre-operatively all patients were evaluated with long standing lower extremity radiographs and deformity analysis were completed. Deformity apexis were determined and the osteotomies were planned. Mechanical axis deviation (MAD) and mechanical lateral distal femoral angles (mLDFA) were measured pre-operatively and post-operatively. Post-operative mLDFA was graded as perfect if it was between 85° and 90°(85° ≤ x ≤ 90°); overcorrection if it is between 91° and 95° (91° ≤ x ≤ 95°) and undercorrection if it is between 80° and 85° (80° ≤ x < 85°). Measurements beyond those limits were graded as bad result. The translation created at the osteotomy site during correction was also calculated as a percentage of the horizontal length of the osteotomy site. In addition, four zones were determined on both the medial and lateral side of the knee. Those zones were labeled 1, 2, 3, and 4 based on the relationship of the mechanical axis and the center of the knee. Mechanical axis deviation was also expressed as the zones through which the mechanical axis of the lower extremity passed (4) (Fig. 1). Statistical Package for Social Sciences (SPSS) version 17.0 was used for statistical analysis. Wilcoxon signed rank test was applied to compare the pre-operative and post-operative mLDFA. The parents were informed that data concerning the case would be submitted for publication, and they provided consent.
Fig. 1.
Four zones were determined on both the medial and lateral sides of the knee. Zones were labeled 1, 2, 3, and 4, corresponding to the severity of the deformity. Deviation between 0% and 50% falls into zone 1; 51%–100% into zone 2; 101%–200% into zone 3; and >200% into zone 4. Deviations were expressed as a percentage to one half of the width of the tibial plateau.
Surgical technique
All the procedures were done on a radiolucent surgical table by a single surgeon (GY) while the patients were in a supine position. The patient should be placed on the table in a way that the flouroscopy can visualize from the hip center to the ankle in order to verify the relationship between the mechanical axis line and the center of the knee after correction. A tourniquet was used only if the peroneal nerve decompression was scheduled. Peroneal nerve decompression was done in patients with valgus deformity of 30° and more at the beginning of the procedure before correction. A straight lateral incision on the distal thigh starting at the level of the growth plate extending proximally 8–10 cm was utilized. The iliotibial band was split. The vastus lateralis was elevated from the intermuscular septum and retracted anteriorly. Attention should be given not to damage the growth plate if it is still open. At this stage, the plate intended to be used was brought into the surgical field and checked under the flouroscopy for distal screw trajectories with respect to growth plate and the possible osteotomy level was identified. The distal Schanz screw was applied in the epiphysis parallel to the joint line, the proximal Schanz screw was applied perpendicular to the femur shaft proximal to the planned osteotomy site under fluoroscopy (Fig. 2a–e). Although the fixator can be applied either on the medial or lateral side, medial side application was more convenient. Tubular external fixator system was mounted and secured before the osteotomy. Then the osteotomy was applied with an ossilating saw, the external fixator was released and the correction was achieved with the aid of the schanz screws. The correction maneuvers included translation of the distal fragment laterally based on pre-operative deformity analysis and varus correction in an open wedge fashion. It should be kept in mind that the deformity apex in patients with open growth plates is distal to the osteotomy site and proper mechanical axis correction needs translation of the distal femur. The correction should be verified at this stage before definitive plate fixation was applied (Fig. 3a–e). This can be done by using the cautery cable technique under flouroscopy or by measuring anatomic lateral distal femoral angle (aLDFA). An intra-operative antero-posterior radiograph of the femur including the knee can be used to measure aLDFA (normal range = 79°–83°). After the correction was verified the external fixator was tightened and the 4.5 mm distal femur osteotomy plate aap LOQTEQ Berlin, Germany or LISS (Less Invasive Stabilization System) DepuySynthes West Chester PA USA was applied (Fig. 3).
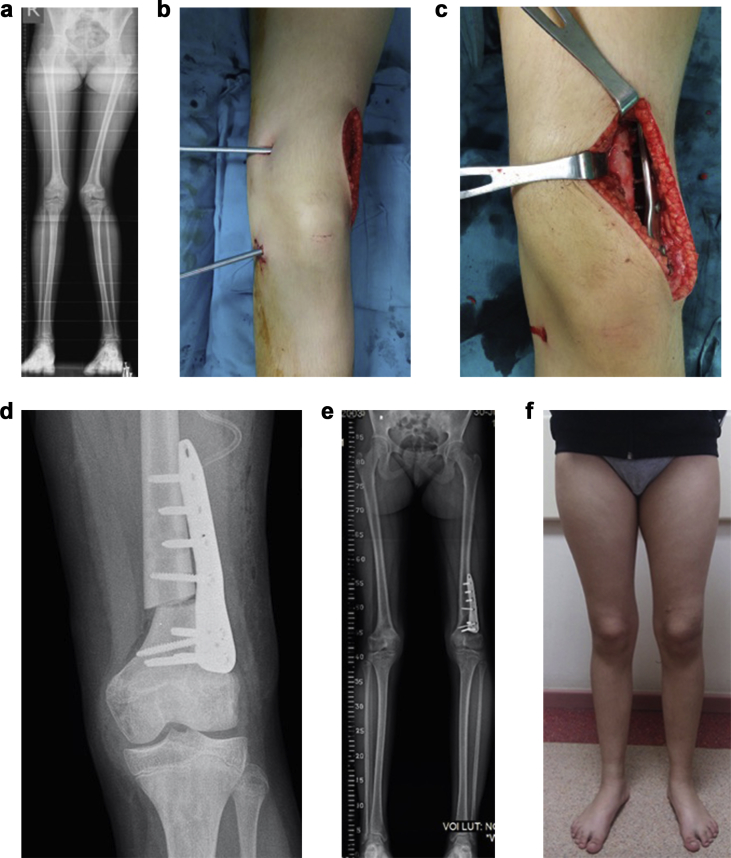
Fig. 2.
a-f: Twelve years-old female patient. a-Pre-operative erect leg lower extremity radiograph showing idiopathic genu valgum deformity. b-medially applied Schanz pins before correction c-distal femur plate was applied after correction d-intraoperative anteroposterior femur radiograph showing correction e,f-three months post-operative radiographs and clinical picture.
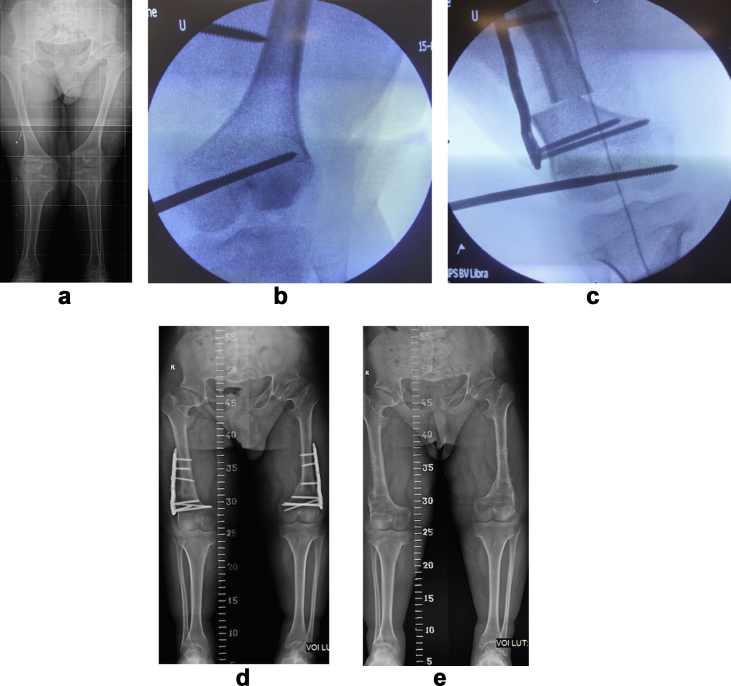
Fig. 3.
a-e. Eighteen years old male patient with achondroplasia. a-Pre-operative erect leg lower extremity radiographs showing genu valgum b,c-the fixator was applied from the lateral side and the correction was achieved. Correction was verified with a cautery cable technique d,e-he had early plate removal at six months post-operatively due soft tissue irritation.
Results
Thirteen patients (7 females-6 males) (17 legs) with the mean age of 16 ± 5.4 years were evaluated. The diagnosis of the patients includes: Fibular hemimelia (3 patients), metaphyseal/epiphyseal dysplasia (3 patients), mucopolysaccharidosis (2 patients), idiopathic genu valgum (3 patients), genu valgum secondary to eight-plate epiphysiodesis (1 patient), achondroplasia (1 patient) The mean follow-up period was 12.8 ± 3.7 months. The pre-operative and post-operative mLDFA was 70.5°±9.4° (range, 57°–82°) and 87.7°±3.5° (range, 80°–94°) (p < 0.001.), respectively Table 1. The mean correction in mechanical axis deviation was 46.3 ± 28.3 mm. Based on post-operative standing radiographs, the correction was graded perfect in 12 femurs. The correction in three femurs was graded as overcorrection and it was graded as undercorrection in two femurs. Three patients (4 extremities) had simultaneous tibial osteotomies and plate fixation. Sagittal plane correction was also achieved in two femurs. Peroneal nerve decompression was done in three patients (5 extremities) with valgus deformity over 30°. Two of these patients had mucopolysaccaridosis. The mean lateral translation of the distal fragment at the osteotomy level was 19.8% ± 16.4%. The mechanical axises in all lower extremities were passing through zone 2 or more pre-operatively, whereas the mechanical axises were in zone 2 in four legs and in zone 3 in one leg (9-year-old MPS patient) in post-operative period. All osteotomies except one were healed in three months. The patient with a delayed union had mucopolysaccharidosiss (MPS). At the final follow-up there was no non-union. None of the patients had peroneal nerve palsy. All patients were allowed full weight bearing at the end of six weeks except one who had delayed union. One patient with MPS who had undercorrection of her deformity had recurrence of genu valgum and she underwent repeat tibial osteotomies and eight-plate hemiepiphysiodesis on bilateral distal medial femurs. One patient had irritation of the soft tissue over the plate during knee range of motion and he underwent early plate removal at six months (18 years old patient with achondroplasia). There was no restriction in knee range of motion at the final follow-up. There was no infection.
Table 1.
Patient demographics and summary of the radiological data.
| Patient No. | Side | Age (yr) | Gender | Diagnosis | Pre mLDFA (°) | Post mLDFA (°) | Change in MAD (mm) | Pre. Zone | Post. zone | P. nerve decom. | Additional surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | L | 12 | f | Idiopathic genu valgum | 70 | 87 | 63 | 3 | 2 | _ | |
| 2 | R | 12 | m | Epiphyseal dysplasia | 79 | 88 | 27 | 2 | 1 | _ | |
| 3 | R | 9 | f | MPS Type IV | 57 | 85 | 90 | 4 | 3 | + | Tibial osteotomy |
| L | 60 | 82 | 77 | 4 | 2 | + | Tibial osteotomy | ||||
| 4 | L | 9 | m | Epiphyseal dysplasia | 61 | 89 | 98 | 4 | 2 | _ | Tibial osteotomy |
| 5 | R | 28 | m | Fibuler hemimelia | 81 | 89 | 52 | 3 | 1 | _ | Tibial osteotomy |
| 6 | R | 17 | m | Fibuler hemimelia | 82 | 94 | 81 | 4 | 1 | – | Tibial osteotomy |
| 7a | L | 15 | f | Metaphyseal dysplasia | 61 | 86 | + | ||||
| 8 | R | 20 | m | MPS Type IV | 61 | 86 | 17 | 2 | 1 | + | |
| L | 62 | 80 | 10 | 3 | 2 | + | |||||
| 9 | R | 20 | f | Fibuler hemimelia | 81 | 93 | 33 | 3 | 1 | _ | |
| 10 | R | 21 | f | Idiopathic genu valgum | 77 | 89 | 32 | 2 | 1 | _ | |
| 11 | L | 15 | f | Genu valgum after 8- plate epiphysiodesis | 80 | 88 | 23 | 3 | 1 | _ | |
| 12 | R | 12 | f | Idiopathic genu valgum | 77 | 87 | 49 | 3 | 1 | _ | Lateral release-MPFL reconstruction |
| L | 81 | 92 | 32 | 2 | 1 | _ | Lateral release-MPFL reconstruction | ||||
| 13 | R | 18 | m | Achondroplasia | 63 | 87 | 23 | 2 | 1 | – | |
| L | 67 | 89 | 43 | 3 | 1 | – |
No= Number, yr = year, Pre = pre-operative, post = post-operative, mLDFA = mechanical lateral distal femoral angle, (°) = degrees, MAD = mechanical axis deviation, mm = millimeter, P. Nerve Decomp. = peroneal nerve decompression, L = left, R = right, f = female, m = male, MPS = mucopolysaccaridosis.
The patient was non-ambulatory, mechanical axis deviation in terms of zones was not calculated.
Discussion
Genu valgum deformity may cause knock knees and deteriorate feet positioning during the stance phase. The patellofemoral joint subluxates laterally as the Q angle increases which in turn may cause patellofemoral joint instability. In long term, mechanical loading on the lateral compartment of the knee, potentially, may cause meniscal and chondral degeneration eventually leading to osteoarthritis. Correction of the genu valgum deformity can balance the load distribution in the knee and prevent long term effects of malalignment.1, 2, 3
The majority of the literature regarding distal femur osteotomies for genu valgum and varum deformities involves adult patients. The osteotomy can be applied closer to the joint line in adult patients, thus simple open/close wedge osteotomies can achieve the treatment goal.10, 11, 12, 13, 14, 15 On the other hand the level of the growth plate should be taken into consideration while deciding on the osteotomy level and the fixation method used in pediatric patients and the correction should include translation when necessary. Eidelman et al reported good results in six patients (seven legs) with fixator asisted plating in genu valgum deformities. Their patients included adolescents and young adults with a mean age of 16.1 years. The growth plates were closed in all patients. They recommended that the technique shouldn't be used in patients with open growth plates and in patients with multiplane deformities.9 Five patients (seven femurs) had open growth plates in our study. All these patients had significant deformity correction. We also achieved coronal and sagittal plane correction in one patient (two femurs) with good result. We believe that, fixator assisted plating in distal femur can also be used in patients with open growth plates and multiplane deformities as opposed to Eidelman et al.
Although there are special plate designs for the lateral distal femur in adult patients, a convenient plate design is hard to find in pediatric patients.14 One of the main reason for this is the fact that the osteotomy site is proximal to the deformity apex which is usually very close to the physis and knee. Since the osteotomy is proximally seated in order to protect physis, a proper mechanical axis correction needs translation of the distal fragment laterally which makes the plate application cumbersome. The fixator holds the osteotomy site corrected in a translated position while the plate is applied on the lateral side. It is essential to apply a locking plate in order to maintain the correction. The mean translation at the level of the osteotomy is 18.2 ± 15.7% in our study. The translation may interfere with healing but the amount of translation did not affect the union rates and all the osteotomies were healed at the end of three months except one in our patients.
Eight-plate hemiepiphysiodesis has been used in lower extremity deformities of pediatric age patients with excellent results.16 Although our study group includes patients with open growth plates their ages were close to maturity. In addition, the youngest patient was a nine-year-old girl with mucopolysaccharidosis (MPS) with severe mechanical axis deviation (104 mm on right, 102 mm on left lower extremity). Older age would preclude the desired effect of hemiepiphysiodesis in this patient population and an osteotomy option was selected.17
One of the most common and precise method of deformity correction in long bones is the external fixation. Pin tract infections, patient discomfort and pain with physical therapy are the main disadvantages of external fixation.6 The bulky soft tissue envelope around the femur makes external fixation treatment even more difficult. On the other hand, Seah et al compared external fixation and fixator asisted plating in distal femur deformities in adult patients. They reported satisfactory and similar results with both techniques. They reported no difference in the accuracy of deformity correction.18 Although it is possible to get good results with both technique, we believe that the treatment with external fixation is best for patients with deformity and limb length discrepancy (LLD). Our study group included patients with no or negligible LLD.
The precision of the correction with an acute maneuver utilizing an external fixator is one of the main concerns in fixator asisted plating. Two techniques can be used in order to verify the correction: The cautery cable technique and intraoperative long radiographs of the operated leg. The cautery cable technique was used if the correction was achieved in an acute manner in the tibia as well. Anteroposterior radiographs of the femur were obtained in two patients who had hexapod external fixators applied for valgus deformities of the tibia. Although the satisfactory correction was confirmed intraoperatively we had under corrections (2 femurs) and overcorrections (3 femurs). The patient who had undercorrection was a nine-year-old girl with MPS. Her epiphysises in the distal femur and proximal tibia were irregular and underdeveloped which prevents optimum evaluation through flouroscopy or radiographs. We believe that a knee arthrogram would be very helpful in those patients with epiphyseal irregularities. Since all those patients had significant correction in their mechanical axis the clinical end result was satisfactory.
One of the drawback of our study is the lack of a control group. Although we believe that the assistance of external fixator during the correction and fixation period makes the surgical procedure easier, we are not sure if we would get the same clinical and radiological results without a fixator. Second drawback would be the small number of patients. But our patient group is the largest patient group treated with fixator assisted plating for distal femur deformities. In addition, our patient group includes patients with open growth plate and biplanar deformities as opposed to previous recommendations.
Conclusion
Fixator assisted plating for distal femur valgus deformities is a safe and reliable method for correction. The technique provides significant correction in pediatric patients as well. The accuracy of the correction should be carefully verified intraoperatively by radiographs or cautery cable method in order to prevent over/under correction.
Conflicts of interest
None of the authors have a conflict of interest.
No funding was received for this work from any organizations.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Janakiramanan N., Teichtahl A.J., Wluka A.E. Static knee alignment is associated with the risk of unicompartmental knee cartilage defects. Orthop Res. 2008 Feb;26(2):225–230. doi: 10.1002/jor.20465. [DOI] [PubMed] [Google Scholar]
- 2.Zhai G., Ding C., Cicuttini F., Jones G. A longitudinal study of the association between knee alignment and change in cartilage volume and chondral defects in a largely non-osteoarthritic population. J Rheumatol. 2007 Jan;34(1):181–186. [PubMed] [Google Scholar]
- 3.Tetsworth K., Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25(3):367–377. [PubMed] [Google Scholar]
- 4.Yilmaz G., Oto M., Thabet A.M. Correction of lower extremity angular deformities in skeletal dysplasia with hemiepiphysiodesis: a preliminary report. J Pediatr Orthop. 2014 Apr-May;34(3):336–345. doi: 10.1097/BPO.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 5.Oto M., Yılmaz G., Bowen J.R., Thacker M., Kruse R. Adolescent Blount disease in obese children treated by eight-plate hemiepiphysiodesis. Eklem Hastalik Cerrahisi. 2012 Apr;23(1):20–24. [PubMed] [Google Scholar]
- 6.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990 Jan;(250):81–104. [PubMed] [Google Scholar]
- 7.Bar-On E., Horesh Z., Katz K. Correction of lower limb deformities in children with renal osteodystrophy by the Ilizarov method. J Pediatr Orthop. 2008;28(7):747–751. doi: 10.1097/BPO.0b013e318186eb99. [DOI] [PubMed] [Google Scholar]
- 8.Kocaoglu M., Eralp L., Bilen F.E., Balci H.I. Fixator-assisted acute femoral deformity correction and consecutive lengthening over an intramedullary nail. J Bone Joint Surg Am. 2009 Jan;91(1):152–159. doi: 10.2106/JBJS.H.00114. [DOI] [PubMed] [Google Scholar]
- 9.Eidelman M., Keren Y., Norman D. Correction of distal femoral valgus deformities in adolescents and young adults using minimally invasive fixator-assisted locking plating (FALP) J Pediatr Orthop B. 2012 Nov;21(6):558–562. doi: 10.1097/BPB.0b013e328358f884. [DOI] [PubMed] [Google Scholar]
- 10.Healy W.L., Anglen J.O., Wasilewsky S.A. Distal femoral varus osteotomy. J Bone Joint Surg Am. 1988;70(1):102–109. [PubMed] [Google Scholar]
- 11.McDermott P.A., Finkelstein J.A., Farine I. Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am. 1988;70:110–116. [PubMed] [Google Scholar]
- 12.Miniaci A., Grossman S.P. Jacob RP Supracondylar femoral varus osteotomy in the treatment of valgus knee deformity. Am J Knee Surg. 1990;3:65–73. [Google Scholar]
- 13.Finkelstein J.A., Gross A.E. Davis A Varus osteotomy of the distal part of the femur: a survivorship analysis. J Bone Joint Surg Am. 1996;78(9):1348–1352. doi: 10.2106/00004623-199609000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Puddu G., Cipolla M., Cerullo G., Franco V., Giannì E. Which osteotomy for a valgus knee. Int Orthop. 2010 Feb;34(2):239–247. doi: 10.1007/s00264-009-0820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Omidi-Khashani F., Hasankhani I.G., Mazlumi M., Ebrahimzadeh M.H. Varus distal femoral osteotomy in young adults with valgus knee. J Orthop Surg Res. 2009;13(4):4–15. doi: 10.1186/1749-799X-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stevens P.M. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orhop. 2007 Apr-May;27(3):253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 17.Cooper G.A., Southorn T., Eastwood D.M., Bache C.E. Lower extremity deformity management in MPS IVA, morquio-Brailsford syndrome: preliminary report of hemiepiphysiodesis correction of genu valgum. J Pediatr Orthop. 2016 Jun;36(4):376–381. doi: 10.1097/BPO.0000000000000464. [DOI] [PubMed] [Google Scholar]
- 18.Seah K.T., Shafi R., Fragomen A.T., Rozbruch S.R. Distal femoral osteotomy: is internal fixation better than external? Clin Orthop Relat Res. 2011 Jul;469(7):2003–2011. doi: 10.1007/s11999-010-1755-0. [DOI] [PMC free article] [PubMed] [Google Scholar]