Abstract
Intravascular papillary endothelial hyperplasia (IPEH), also known as Masson's tumor or vegetant intravascular hemangioendothelioma, is a reactive condition representing an exuberant organization and recanalization of a thrombus. It can occur in normal blood vessels or in vascular malformations, perhaps in response to blood vessel injury or thrombosis.
In this report, we present the diagnostic and therapeutic courses of a 55 year-old woman and an 18 year-old man, who had a progressive protruding hand mass following a hand contusion. The pathological examination confirmed the diagnosis of IPEH in both patients.
Keywords: Hand tumor, Intravascular papillary endothelial hyperplasia, Lumbrical tumor, Vascular tumor, Hand contusion injury
Introduction
Intravascular papillary endothelial hyperplasia (IPEH), also known as Masson's tumor or vegetant intravascular hemangioendothelioma, is a reactive condition representing an exuberant organization and recanalization of a thrombus.1 It can occur in normal blood vessels or in vascular malformations, perhaps in response to blood vessel injury or thrombosis. However, the exact pathogenesis of IPEH is still unknown. IPEH was first described by the French pathologist Masson as a neoplastic lesion termed vegetant intravascular hemangioendothelioma.2 In 1976, Clearkin and Enzinger proposed the term IPEH, which is currently known as a non-neoplastic reactive endothelial proliferation.3 IPEH tumors are characterized by multiple endothelial-lined small papillary structures with hyaline stalks. They are identified as partially involving an organizing thrombus within a vein and have been detected in pure and mixed forms. The pure form typically occurs within dilated vascular spaces, and the mixed form develops in a preexisting vascular lesion (i.e., as a hemangioma).1, 4
Case reports
Case 1
A 55-year-old female patient suffered from a progressive protruding mass lesion on the left palm that had persisted for several months. She claimed to have had a left-hand contusion with ecchymosis 2 years previously. On physical examination, the mass was soft, indolent, and located at the left palmar aspect between the 3rd and 4th metacarpals. All laboratory investigations were within normal limits. A lobulated and heterogeneous lesion was observed between the 3rd and 4th flexor digitorum tendons in magnetic resonance images (Fig. 1A).
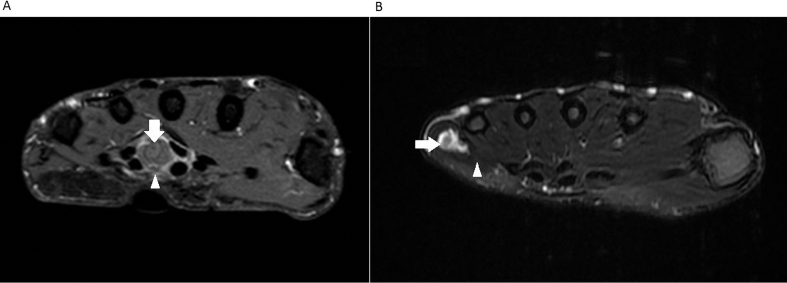
Fig. 1.
(a) Case 1: a lobulated and heterogeneous lesion (arrow) between the 3rd and 4th flexor digitorum tendons and along the lumbrical muscle (arrowhead) (MRI: transection view). (b) Case 2: a lobulated and heterogeneous lesion (arrow) in the subcutaneous layer of ulnar side of the 5th metacarpal shaft along the hypothenar muscle (arrowhead) (MRI: transection view).
On excision, the soft tumor measured 3.3 × 1 × 0.6 cm in size (Fig. 2A) and was confirmed to be located between the 3rd and 4th flexor digitorum tendons and along the lumbrical muscle (Fig. 3). Histopathology confirmed IPEH, including a dilated vascular wall with focal hemorrhage, and a small percentage of fibrinous material, granulation tissue, focal papillary endothelial hyperplasia, and recanalization of the soft tissue (Fig. 4).
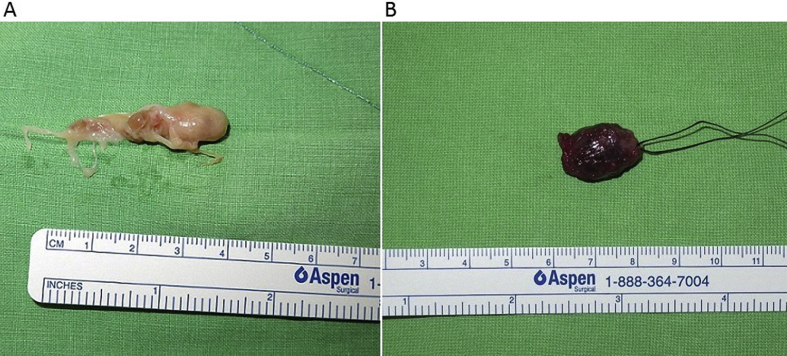
Fig. 2.
(a) Case 1: the soft tumor measured 3.3 × 1 × 0.6 cm in size. (b) Case 2: the soft tumor measured 2.2 × 0.8 × 0.6 cm in size.
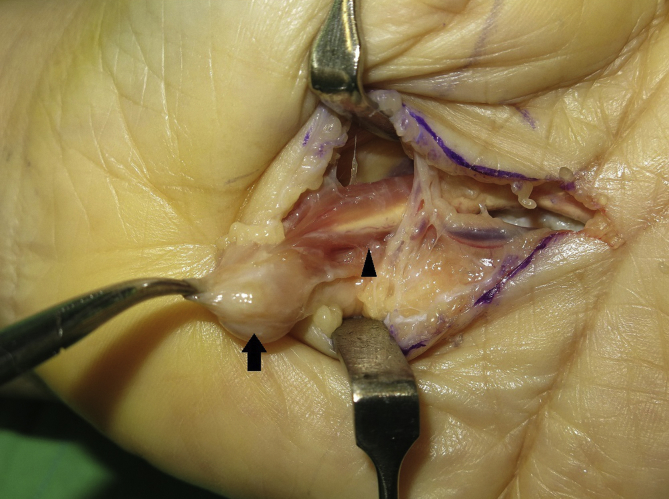
Fig. 3.
Case 1: a soft tumor (arrow) along the lumbrical muscle (arrowhead), located between the 3rd and 4th flexor digitorum tendons.
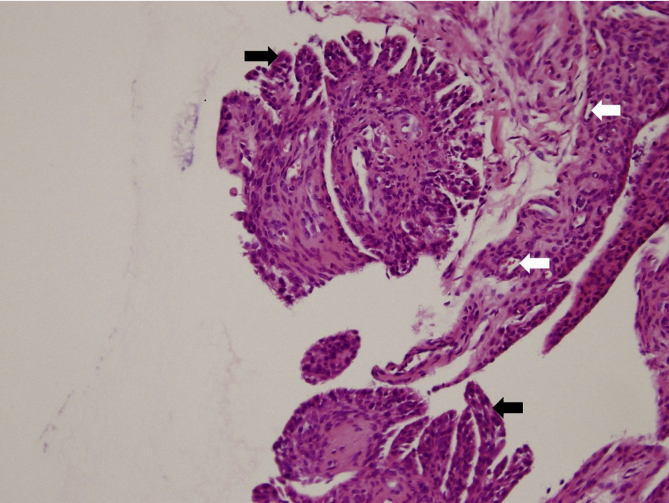
Fig. 4.
The micrograph shows papillary projections with stratified endothelial cells without nuclear atypia (black arrow) surrounding hyalinized stroma accompanied by focal recanalization (white arrow) within the dilated vessels. The histological examination of tumor tissue sections was compatible with a diagnosis of intravascular papillary endothelial hyperplasia (hematoxylin and eosin stain, original amplification × 200).
Case 2
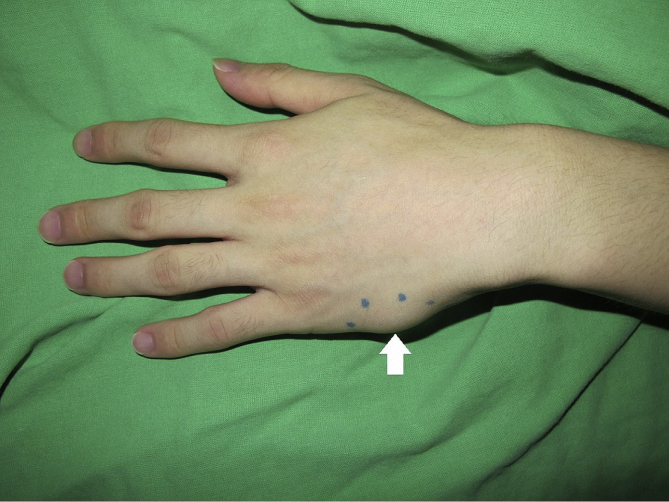
An 18-year-old male patient suffered from a progressive protruding mass lesion on the ulnar side of the left hand with rapid enlargement (Fig. 5) in the recent 2 months after a hand contusion injury caused by a fall. There was a heterogeneously lobulated lesion in the subcutaneous layer of ulnar side of the 5th metacarpal shaft along the hypothenar muscle in magnetic resonance images (Fig. 1B). On excision, the soft tumor measured 2.2 × 0.8 × 0.6 cm in size (Fig. 2B) and was confirmed to be located along the hypothenar muscle. The final histopathology of tumor tissue sections was compatible with a diagnosis of IPEH.
Fig. 5.
Case 2: a progressive protruding mass lesion on the ulnar side of the left hand with rapid enlargement (arrow).
Discussion
The exact pathogenesis of IPEH is unknown, but an unusual organization of the thrombus following trauma is considered to play a role.5, 6 In a pathologic series of 91 cases, patient ages varied from 9 months to 78 years.4 Moreover, younger patients were more likely to present with the mixed form of IPEH tumors.4 In addition, IPEH most often arises in female patients, and a history of trauma only occurs in about 4% of all patients.4 Because its clinical signs and symptoms are nonspecific and variable, it is a diagnostic challenge. The patient's history of any trauma, a physical examination, ultrasound and computed tomography can help to distinguish IPEH from other kinds of vascular hand lesions. While the exact pathogenesis of IPEH is still unclear, an unusual form of thrombus organization following a trauma is considered to play a role. The release of beta-fibroblast growth factor (β-FGF) from macrophages attracted to the site can trigger endothelial cell proliferation, which in turn, induces the release of more β-FGF, leading to a vicious cycle.7 According to our analysis of the literature, IPEH usually presents as a palpable mass that most commonly occurs in the fingers, head, and neck.1, 4, 7, 8, 9 Moreover, an IPEH lesion over the hand along the intrinsic muscle, including lumbrical muscle or hypothenar muscle, is relatively rare. Therefore, distinguishing between reactive and neoplastic intravascular lesions of the hand is important. We hope that the detailed images presented for the two cases will enable the visual differentiation of an IPEH from other common hand tumors.
Conflict of interest
None.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Chi-Yu Wang, Email: bibokingbiboking@gmail.com.
Chung-Chih Hong, Email: wholeworld@office365.ndmctsgh.edu.
Zheng-Yi Huang, Email: ak-600@office365.ndmctsgh.edu.
Chih-Hsin Wang, Email: super-derrick@yahoo.com.tw.
References
- 1.Kuo T., Sayers C.P., Rosai J. Masson's “vegetant intravascular hemangioendothelioma:” a lesion often mistaken for angiosarcoma. Study of seventeen cases located in the skin and soft tissues. Cancer. 1976;38:1227–1236. doi: 10.1002/1097-0142(197609)38:3<1227::aid-cncr2820380324>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Steffen C. The man behind the eponym: C. L. Pierre Masson. Am J Dermatopathol. 2003;25:71–76. doi: 10.1097/00000372-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Clearkin K.P., Enzinger F.M. Intravascular papillary endothelial hyperplasia. Arch Pathol Lab Med. 1976;100:441–444. [PubMed] [Google Scholar]
- 4.Hashimoto H., Daimaru Y., Enjoji M. Intravascular papillary endothelial hyperplasia. A clinicopathologic study of 91 cases. Am J Dermatopathol. 1983;5:539–546. doi: 10.1097/00000372-198312000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Johraku A., Miyanaga N., Sekido N. A case of intravascular papillary endothelial hyperplasia (Masson's tumor) arising from renal sinus. Jpn J Clin Oncol. 1997;27:433–436. doi: 10.1093/jjco/27.6.434. [DOI] [PubMed] [Google Scholar]
- 6.Kim H.S., Park E.J., Lee J.H. Intravascular papillary endothelial hyperplasia in the kidney of a child. Virchows Arch. 2000;436:398–400. doi: 10.1007/s004280050466. [DOI] [PubMed] [Google Scholar]
- 7.Erol O., Ozcakar L., Uygur F., Kecik A., Ozkaya O. Intravascular papillary endothelial hyperplasia in the finger: not a premier diagnosis. J Cutan Pathol. 2007;34:806–807. doi: 10.1111/j.1600-0560.2006.00689.x. [DOI] [PubMed] [Google Scholar]
- 8.Sartore L., Voltan A., Tomat V., Salmaso R. Masson's disease in hand surgery: a clinicopathologic study of four cases. J Hand Surg Eur. 2011;36:694–697. doi: 10.1177/1753193411407035. [DOI] [PubMed] [Google Scholar]
- 9.Pantanowitz L., Muc R., Spanger M., Sonnendecker H., McIntosh W.A. Intravascular papillary endothelial hyperplasia (Masson's tumor) manifesting as a lateral neck mass. Ear Nose Throat J. 2000;79:809–810. 812. [PubMed] [Google Scholar]