Abstract
This study reports the seeming disparity in access to buprenorphine prescriptions among racial/ethnic minorities and individuals with lower income.
Opioid mortality rates continue to increase throughout the United States1; however, growth in buprenorphine hydrochloride treatment for opioid use disorder (OUD) might be limited to communities with higher income and low percentages of racial/ethnic minorities.2 Buprenorphine, a partial opioid agonist, is 1 of 3 evidence-based medications for treating OUD and can legally be prescribed in office-based settings.
To our knowledge, no national studies have examined the differences in the receipt of buprenorphine prescription by race/ethnicity and payment in office-based settings, in which most patients with buprenorphine prescription receive care.3 In this article, we present changes in buprenorphine treatment at office-based visits in the United States since 2004 as well as the race/ethnicity and payment characteristics currently associated with its receipt.
Methods
We combined data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey outpatient department component from 2004 to 2015. The surveys, which provide nationally representative estimates of ambulatory care provided in the United States by non–federally employed physicians, capture physician-reported medications prescribed during each office visit as well as demographic characteristics and expected source of payment. The University of Michigan Institutional Review Board did not require approval for this study, given that secondary analysis of publicly available, nonidentifiable data set is not regulated. Informed consent was not applicable for this type of study.
We limited our sample to visits in which buprenorphine was prescribed, and we aggregated the sample into 4-year periods. We estimated buprenorphine prescription rates by race/ethnicity and payment. We chose the most recent period (2012-2015) to test the association of race/ethnicity with receipt of buprenorphine prescription using logistic regression adjusted for age, sex, and payment method. Analyses were completed in Stata, version 15.1 (StataCorp LLC), and accounted for complex survey design elements to generate nationally representative estimates.
Results
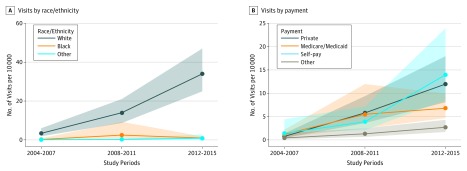
From 2004 to 2015, the number of buprenorphine visits rose from 0.04% to 0.36% of all ambulatory visits, representing 13.4 million visits between 2012 and 2015. From 2012 to 2015, buprenorphine prescription was received at considerably more visits by white patients than patients of other races/ethnicities (12.7 million [95% CI, 8.6 million-16.8 million] vs 363 000 [95% CI, 134 000-594 000]) (Figure). Self-pay and private insurance were the most common payment methods across all years (Table). The number of buprenorphine visits by self-pay patients dramatically increased from 585 568 (95% CI, 0-1.3 million) visits in 2004 to 2007 to 5.3 million (95% CI, 2.5 million-8.5 million) visits in 2012 to 2015, accounting for 39.6% of the visits. After accounting for payment method, sex, and age, we found that black patients had statistically significantly lower odds of receiving buprenorphine prescription at their visits (adjusted odds ratio, 0.23; 95% CI, 0.13-0.44).
Figure. Buprenorphine Visits by Race/Ethnicity and Payment Type, 2004-2015 .
Buprenorphine visits (n = 1369) and 95% CIs per 10 000 visits (shaded areas), grouped by year and stratified by race/ethnicity and payment type. Estimates account for complex survey design elements and are nationally representative.
Table. Demographic Characteristics Associated With Buprenorphine Prescribing in Outpatient Care in the United States in 2004-2007 and 2012-2015.
| Variable | 2004-2007 | 2012-2015 | |||
|---|---|---|---|---|---|
| Visits Without Buprenorphine (n = 244 274), %a | Visits With Buprenorphine (n = 183), %a | Visits Without Buprenorphine (n = 204 527), %a | Visits With Buprenorphine (n = 718), %a | Adjusted OR (95% CI)b | |
| Race/ethnicityc | |||||
| White | 83.5 | 90.5 | 83.1 | 94.9 | 1.00 |
| Black | 11.5 | 6.5 | 10.6 | 2.7 | 0.23 (0.13-0.44) |
| Other | 5.0 | 3.0 | 6.3 | 2.4 | 0.27 (0.08-0.90) |
| Payment method | |||||
| Private insurance | 52.0 | 19.8 | 49.2 | 33.9 | 1.00 |
| Medicare/Medicaid | 35.1 | 31.5 | 38.1 | 18.9 | 1.16 (0.74-1.82) |
| Self-pay | 4.5 | 37.8 | 4.5 | 39.6 | 12.27 (6.86-21.91) |
| Other or unknown | 8.5 | 11.0 | 8.2 | 7.5 | 1.35 (0.78-2.35) |
| Sex | |||||
| Female | 58.8 | 47.5 | 58.3 | 39.7 | 1.00 |
| Male | 41.2 | 52.5 | 41.7 | 60.3 | 2.22 (1.82-2.70) |
| Age, y | |||||
| <30 | 29.9 | 40.0 | 25.4 | 30.3 | 1.00 |
| 30-50 | 23.8 | 47.5 | 21.4 | 47.2 | 1.68 (1.33-2.12) |
| >50 | 46.3 | 12.5 | 53.2 | 22.4 | 0.38 (0.27-0.52) |
Abbreviation: OR, odds ratio.
Analyses were completed using survey design elements accounting for visit weight, clustering, and stratification to generate nationally representative estimates.
Adjusted odds ratios (AOR) were generated using logistic regression (1 = buprenorphine prescribed; 0 = no buprenorphine), including the variables reported in the Table. The AOR reflects the OR for buprenorphine treatment for a given visit characteristic during 2012 to 2015. The 2004 to 2007 visit characteristics are provided for comparison; they are not included in the logistic regression.
White (Hispanic and non-Hispanic), black (Hispanic and non-Hispanic), and other (Asian, native Hawaiian/Pacific Islander, American Indian/Alaskan native, and multiple race, both Hispanic and non-Hispanic).
Discussion
This study demonstrates that buprenorphine treatment is concentrated among white persons and those with private insurance or use self-pay. This finding in nationally representative data builds on a previous study that reported buprenorphine treatment disparities on the basis of race/ethnicity and income in New York City.2 It is unclear whether the appearance of a treatment disparity may reflect different prevalence in OUD by race/ethnicity. We did not restrict the analysis to individuals with OUD because the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey are unlikely to accurately capture OUD prevalence, but a recent analysis of the National Survey on Drug Use and Health suggests that the prevalence of opioid misuse is similar for black (3.5%) and white (4.7%) adults.4
Despite the enactment of both mental health parity legislation and Medicaid expansion, the proportion of self-pay buprenorphine visits remained relatively steady across the study period.5 A recent study demonstrated that half of the physicians prescribing buprenorphine in Ohio accepted cash alone,6 and our findings suggest that this practice may be widespread and may be associated with additional financial barriers for low-income populations.
This study provides a snapshot of the national differences in buprenorphine treatment for OUD. With rising rates of opioid overdoses, it is imperative that policy and research efforts specifically address racial/ethnic and economic differences in treatment access and engagement.
References
- 1.Alexander MJ, Kiang MV, Barbieri M. Trends in black and white opioid mortality in the United States, 1979-2015. Epidemiology. 2018;29(5):707-715. doi: 10.1097/EDE.0000000000000858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hansen H, Siegel C, Wanderling J, DiRocco D. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity and race of neighborhoods in New York City. Drug Alcohol Depend. 2016;164:14-21. doi: 10.1016/j.drugalcdep.2016.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breen CT, Fiellin DA. Buprenorphine supply, access, and quality: where we have come and the path forward. J Law Med Ethics. 2018;46(2):272-278. doi: 10.1177/1073110518782934 [DOI] [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality Results from the 2017 National Survey on Drug Use and Health: Detailed Tables. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf. Published September 7, 2018. Accessed April 2, 2019.
- 5.Andrews CM, Grogan CM, Smith BT, et al. Medicaid benefits for addiction treatment expanded after implementation of the Affordable Care Act. Health Aff (Millwood). 2018;37(8):1216-1222. doi: 10.1377/hlthaff.2018.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parran TV, Muller JZ, Chernyak E, et al. Access to and payment for office-based buprenorphine treatment in Ohio. Subst Abuse. 2017;11:1178221817699247. [DOI] [PMC free article] [PubMed] [Google Scholar]