Abstract
Background:
Living kidney donors remain at low risk of end-stage kidney disease (ESKD), but the risk for obese and overweight donors is increased. The Kidney Disease Improving Global Outcomes (KDIGO) clinical guideline recommends that overweight and obese patients pursue weight loss before donation and maintain a healthy post-donation weight.
Objective:
To determine the trajectory of weight changes before and after living kidney donation.
Design:
Retrospective cohort study.
Setting:
The Living Kidney Donor program in the Champlain Local Health Integration Network at The Ottawa Hospital in Ottawa, Canada.
Patients:
The study included 151 living kidney donors who donated between January 2009 and December 2017.
Measurements:
Date of kidney donation, relationship to the transplant recipient, and cause of ESKD in the transplant recipient were documented. Demographic data, markers of glycemic control, and weights at the time of clinic visits were recorded.
Methods:
The analysis included use of paired Student’s t tests to compare mean differences in weight at kidney donation relative to the time of initial assessment and at last follow-up.
Results:
The median (interquartile range [IQR]) follow-up was 392 (362, 1096) days post-donation. Among donors with normal body mass index (BMI; 18.5-24.9 kg/m2), weight loss occurred before donation (62.8 ± 3.1 kg to 61.5 kg ± 2.9 kg; mean difference 1.1 ± 2.7 kg, P < .01) and did not change significantly post-donation. Among overweight/obese donors (BMI ≥25 kg/m2), weight did not change significantly pre-donation, but increased significantly post-donation (86.0 ± 2.1 kg to 88.8 ± 2.7 kg; mean difference 2.3 ± 0.9 kg, P < .0001).
Limitations:
The single-center design of the study limits generalizability.
Conclusions:
Donors with normal BMI experienced significant weight loss before donation and maintained healthy body weight post-donation. Conversely, donors with BMI ≥25 kg/m2 at donation experienced significant weight gain over 1-year post-donation. Our findings suggest the need for enhanced weight control efforts among obese and overweight kidney donors to reduce the risk of ESKD.
Keywords: kidney transplantation, obesity, living kidney donation
Abrégé
Contexte:
Le risque d’insuffisance rénale terminale (IRT) demeure faible chez les donneurs vivants d’un rein, mais ce risque augmente si le donneur est obèse ou en surcharge pondérale. Les lignes directrices cliniques du KDIGO recommandent que ces derniers perdent du poids avant l’intervention et qu’ils maintiennent un poids santé par la suite.
Objectif:
Suivre les variations du poids avant et après un don vivant de rein.
Type d’étude:
Une étude de cohorte rétrospective.
Cadre:
Le programme de don vivant de rein du Réseau local d’intégration des services de santé de Champlain de l’hôpital d’Ottawa (Canada).
Sujets:
L’étude a inclus 151 individus ayant fait don d’un rein entre janvier 2009 et décembre 2017.
Mesures:
On a recensé la date du don, le lien entre le donneur et le receveur, et la cause de l’IRT chez le receveur. On a également colligé les données démographiques, les marqueurs de contrôle glycémique et le poids des sujets lors des consultations en clinique.
Méthodologie:
Des tests de Student pour échantillons appariés ont été utilisés pour comparer les différences moyennes du poids au moment du don par rapport au poids initial et au poids mesuré lors de la dernière consultation.
Résultats:
Le suivi médian (EIQ) post-don s’est fait sur 392 (362, 1 096) jours. Les donneurs dont l’indice de masse corporelle était normal (IMC: 18,5 à 24,9 kg/m2) avaient perdu du poids avant le don (62,8 ± 3,1 kg à 61,5 kg ± 2,9 kg; différence moyenne: 1,1 ± 2,7 kg; p < 0,01) et l’avaient maintenu après. Le poids des donneurs obèses ou en embonpoint (IMC ≥ 25 kg/m2) était demeuré stable avant le don, mais avait nettement augmenté après (86,0 ± 2,1 kg à 88,8 ± 2,7 kg; différence moyenne: 2,3 ± 0,9 kg; p < 0,0001).
Limite:
L’étude était monocentrique, ce qui limite la généralisation des résultats.
Conclusion:
Les donneurs dont l’IMC était normal au moment du don ont connu une perte de poids significative avant l’intervention qui s’est maintenue post-don. À l’inverse, les donneurs avec un IMC d’au moins 25 kg/m2 au moment du don ont connu un gain pondéral important dans l’année suivant l’intervention. Ces résultats suggèrent que pour réduire les risques d’IRT, il est nécessaire de redoubler d’efforts pour contrôler le poids des donneurs de rein obèses ou en embonpoint.
What was known before
Obesity at the time of kidney donation is associated with a higher risk of end-stage kidney disease (ESKD) in living kidney donors.
What this adds
In a Canadian context, we show that living kidney donors whose body mass index (BMI) is in the overweight or obese categories at the time of kidney donation gain weight after donation.
Introduction
Although living kidney donors remain at low risk of end-stage kidney disease (ESKD),1 obesity confers an increased risk.2-5 At the same time, there is a worldwide obesity epidemic6 that is increasingly being reflected in the living kidney donor candidate pool.7,8 An ESKD risk projection tool developed to support donor candidate evaluation found a 16% increase in ESKD risk among healthy nondonors for every 5 kg/m2 increase above 30 kg/m2 in body mass index (BMI, the weight in kilograms divided by the square of the height in meters).2 Subsequent studies have reported an association between BMI and ESKD risk among living kidney donors. One study found that ESKD risk among donors increased by 7% (adjusted hazard ratio [aHR] = 1.07, 95% confidence interval [CI] = 1.02-1.12) for every 1 kg/m2 increase above 27 kg/m2.3 The development of a post-donation tool to estimate risk of ESKD showed that greater BMI was associated with 61% higher ESKD risk (aHR = 1.61 per 5 kg/m2, 95% CI = 1.29-2.00).4 Another recent study also indicates that higher BMI is associated with ESKD (aHR = 1.34 per 5 kg/m2, 95% CI = 1.10-1.64) in the donor population.5
The Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guideline on the evaluation and care of living kidney donors recommends considering BMI as part of the overall health and long-term risk assessment of donor candidates.9 Specifically, it advises the pursuit of weight loss before donation and the maintenance of healthy body weight after donation to minimize long-term risks of obesity, such as diabetes, cardiovascular disease, and obesity-related glomerulopathy.9 Nonetheless, little is known about changes in BMI among living kidney donors before and after kidney donation. As such, we sought to describe the trajectory of weight changes before and after kidney donation to enhance our understanding of the nature of BMI as a risk factor for the development of ESKD among kidney donors.
Materials and Methods
We undertook a single-center retrospective cohort study of patients who donated a kidney from January 2009 to December 2017. Our donor program keeps a consecutive listing of all patients who undergo initial nursing assessment since January 2009. The initial assessment is defined as the time point when a donor nurse coordinator meets the donor candidate for the first time, following receipt of the standardized patient questionnaire and consent to proceed with donor evaluation. We reviewed all the patient files in the list, including those who presented as donor candidates but did not donate, to ensure that we captured all donors. We reviewed 446 consecutive charts from January 1, 2009 to December 31, 2017. At our center, patients noted to have a BMI of 25 kg/m2 or greater at initial assessment are counseled by a donor nurse coordinator regarding weight management to attain a BMI in the healthy range with dietary changes and increased aerobic activity. Since 2013, our donor program has employed a donor risk assessment tool to estimate long-term cardiovascular risk, which includes BMI. Demographics, height, and weight measures from hospital and clinic visits were collected through chart review. Patients were categorized by BMI at the time of kidney donation. Donors were excluded if there was no weight recorded at the time of kidney donation or after kidney donation. Mean weight at the time of initial assessment, at kidney donation, at 12-month follow-up, and at last follow-up were calculated. Paired Student’s t tests compared mean differences in weight at kidney donation relative to the time of initial assessment and at last follow-up.
Results
The mean BMI for 216 kidney donors at the time of initial nursing assessment was 29.0 kg/m2. The mean BMI for potential kidney donors (n = 230) who underwent an initial nursing assessment but did not subsequently donate was 28.1 kg/m2. After reviewing 216 charts for those who donated a kidney, a total of 151 consecutive donors were included for analysis. Twenty-one donors were excluded from analysis because there was no weight recorded at the time of kidney donation. Another 44 donors were excluded because there was no weight recorded after donation.
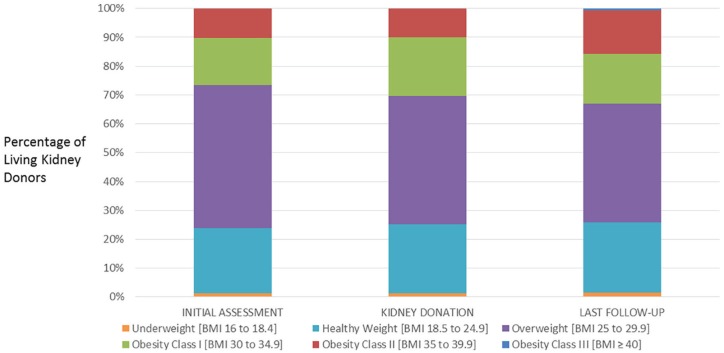
The mean (standard deviation, SD) age of donors was 47 ± 14 years and 60% of donors were female. Donor characteristics, including the number of kidney donors related to the kidney transplant recipient, the number of kidney donors donating to a related recipient with type 2 diabetes mellitus, fasting blood glucose levels, and hemoglobin A1c levels were similar among BMI groups at the time of kidney donation (Table 1). At the time of kidney donation, 2 patients (1.3%) had a BMI less than 18.5 kg/m2 (underweight); 36 (23.8%) had a BMI 18.5 to 24.9 kg/m2 (normal range, healthy weight); 67 (44.4%) had a BMI 25 to 29.9 kg/m2 (overweight); 31 (27.0%) had a BMI 30 to 34.9 kg/m2 (Class I Obesity); and 15 (13.0%) had a BMI 35 to 39.9 kg/m2 (Class II Obesity) (Figure 1). The median (interquartile range, IQR) time from initial assessment to donation was 141 (71, 239) days. The median (IQR) time from kidney donation to last follow-up was 392 (362, 1096) days. In the normal BMI group (18.5-24.9 kg/m2), weight dropped prior to kidney donation from 62.8 ± 3.1 kg to 61.5 ± 2.9 kg (mean difference 1.2 ± 0.8 kg, P < .01) and did not change significantly following donation. Weight increased significantly from 86.0 ± 2.1 kg to 88.77.3 kg ± 2.4 kg (mean difference 2.7 kg ± 1.1 kg, P < .0001) following donation in patients with BMI 25 kg/m2 or greater at the time of initial assessment. Overall, among all donors, weight increased significantly following kidney donation from 79.5 ± 2.5 kg to 81.8 ± 2.7 kg at last follow-up (mean difference 2.3 ± 0.9 kg, P < .0001) (Table 2).
Table 1.
Participant Characteristics at Time of Kidney Donation.
| Normal BMI (n = 36) |
Overweight and obesity class I, IIa
(n = 113) |
Totalb
(n = 151) |
P valuec | |
|---|---|---|---|---|
| Age (y), mean (SD) | 46 (14.4) | 47 (13.1) | 47 (13.5) | .502 |
| Male, n (%) | 9 (25.7) | 52 (45.6) | 61 (40.4) | .032 |
| Donation to related recipient, n (%) | 12 (34.3) | 57 (50.0) | 70 (46.4) | .088 |
| Donation to related recipient with ESKD due to DM2, n (%) | 1/12 (8.3) | 5/57 (8.8) | 6/70 (8.6) | 1.00 |
| Fasting BG (mmol/L), mean (SD) | 4.90 (0.58) | 5.10 (0.47) | 5.05 (0.50) | .042 |
| HbA1c, mean (SD) | 0.054 (0) | 0.054 (0) | 0.054 (0) | .635 |
Note. BMI = body mass index; ESKD = end-stage kidney disease; DM2 = type 2 diabetes mellitus; BG = blood glucose; HbA1c = hemoglobin A1c.
Number of patients according to subgroups within this category: Overweight [BMI 25-29.9 kg/m2] = 67 (59.3%); Obese Class I [BMI 30-34.9 kg/m2] = 31 (27.4%); Obese Class II [BMI 35-39.9 kg/m2] = 15 (13.3%).
Includes 2 (1.3%) underweight patients with BMI less than 18.5 kg/m2.
For comparison of “Normal” BMI group with “Overweight or Obesity Class I, II” group: Student’s t test for continuous variables and chi-square test for categorical variables.
Figure 1.
Distribution of kidney donors by BMI, n = 151.
Note. BMI = body mass index.
Table 2.
Mean Weights and Mean Difference in Weight Relative to Time of Kidney Donation.
| BMI 18.5-24.9 kg/m2
(n = 36) |
BMI ≥ 25 kg/m2
(n = 113) |
Overalla
(n = 151) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean weight [kg] (95% CI) |
Mean diff. [kg] (95% CI) | Pb vs REF | Mean weight [kg] (95% CI) |
Mean diff. [kg] (95% CI) | Pb vs REF | Mean weight [kg] (95% CI) |
Mean diff. [kg] (95% CI) | Pb vs REF | |
| Initial assessment | 62.8 (±3.1) | 1.2 (±0.8) | <.01 | 86.2 (±2.2) | 0.20 (±0.61) | .609 | 80.0 (±2.5) | 0.41 (±0.5) | .12 |
| Kidney donation | 61.5 (±2.9) | REF | 86.0 (±2.1) | REF | 79.5 (±2.5) | REF | |||
| Last follow-up | 62.4 (±3.1) | 0.8 (±1.3) | .21 | 88.7 (±2.4) | 2.7 (±1.1) | <.0001 | 81.8 (±2.7) | 2.3 (±0.9) | <.0001 |
Note. BMI = body mass index; CI = confidence interval; diff. = difference; REF = reference.
Includes 2 (1%) “underweight” patients with BMI less than 18.5.
For paired t test with weight at time of kidney donation.
The examination of median weight changes yielded similar results. In the normal BMI group, the median weight (IQR) change from initial assessment to kidney donation was −1.3 (−2.3, 0.4) kg and from donation to last follow-up, the median weight change was 1.0 (−1.4, 2.6) kg. Among donors with BMI 25 kg/m2 or greater at initial assessment, the median weight change from initial assessment to kidney donation was 0 (−1.8, 1.5) kg and from donation to last follow-up, the median weight increase was 2.4 (0.1, 4.8) kg. Overall, among all donors, median weight from initial assessment to kidney donation was 0 (−1.8, 1.1) and median weight increased following kidney donation by 2.0 (−0.6, 4.0) kg.
Trajectory of Weight Changes
Among the total of 151 donors, the weight changes from initial assessment to kidney donation were as follows: 63 (41.7%) gained weight, 73 (48.3%) lost weight, and 15 (9.9%) had no weight change. Among donors who had a BMI 25 kg/m2 or greater at their initial assessment (n = 116), 49 (42.2) gained weight and 67 (57.8%) lost or had no change in weight. Among donors who had a BMI of less than 25 kg/m2 at their initial assessment (n = 33), 13 (39.4%) gained weight, 19 (57.6%) lost weight, and 1 had no change. Among the 2 donors who had a BMI less than 18.5 kg/m2, 1 gained weight and 1 lost weight.
Among the total of 151 donors, the weight changes from kidney donation to last follow-up were as follows: 108 (71.5%) gained weight, 43 (28.5%) lost weight, and no donors maintained the same weight. Among donors who had a BMI 25 kg/m2 or greater at kidney donation (n = 113), 85 (75.2%) gained weight and 28 (24.8%) lost weight and no donors maintained the same weight. Among donors who had a BMI of less than 25 kg/m2 at kidney donation (n = 36), 22 (61.1%) gained weight and 14 (38.9%) lost weight and none of the donors maintained the same weight.
Changes in BMI From Donation to Last Follow-Up
The median (IQR) increase in BMI was 0.78 (−0.19, 1.49) kg/m2 among the entire group of 151 donors. Among donors who had a BMI 25 kg/m2 or greater at kidney donation, median BMI increased by 0.82 (0.01, 1.64) kg/m2, and among donors who had a BMI of less than 25 kg/m2 at kidney donation, BMI increased by 0.39 (−0.49, 0.98) kg/m2.
Other Donor Outcomes
At last follow-up, there was no difference in estimated glomerular filtration rate among donors across BMI groups and none of the kidney donors had developed diabetes mellitus.
BMI Distribution for Kidney Donors Without a Post-Donation Weight and Donor Candidates Declined for Donation
Regarding the 44 donors excluded from the study due to the absence of weights after kidney donation, their mean age was 46 years, 41% were male, 45% were overweight, and 23% had Class I Obesity, similar to the donors included in the study. The BMI distribution (n, %) at the time of initial assessment for the 230 donor candidates who did not donate a kidney was: underweight 4 (1.7%), healthy weight 64 (27.8%), overweight 89 (38.7%), Class I Obesity 41 (17.8%), Class II Obesity 25 (10.9%), and Class III Obesity (BMI ≥40 kg/m2) 7 (3.0%). The reasons for decline attributable to weight or other metabolic features were diabetes (n = 14), metabolic syndrome (n = 2), gestational diabetes (n = 6), prediabetes (n = 9), and BMI by itself (n = 1).
Discussion
Despite KDIGO recommendations that patients who are overweight or living with obesity pursue weight loss before kidney donation and maintain a healthy weight after kidney donation, this is not what we observed at our center despite routine counseling about weight management. Significant weight gain occurred among patients with BMI 25 kg/m2 or greater following kidney donation. To our knowledge, this is the first study to describe the trajectory of weight changes before and after kidney donation in Canada.
We found that donors with a normal BMI (18.5-24.9 kg/m2) experienced weight loss prior to kidney donation and maintained it afterward. In contrast, donors already classified as overweight or living with obesity at the time of kidney donation (BMI 25 kg/m2 or greater) did not have a significant weight gain prior to kidney donation but then did so within only 12 months afterward, and this weight gain persisted. Similarly, the only other study to examine weight changes around kidney donation showed that few donors lost weight prior to donation and most gained weight after kidney donation, particularly donors who lost weight before donation to achieve a BMI of 30 kg/m2 or less. Furthermore, weight gain after kidney donation was associated with an increased risk of type 2 diabetes and hypertension.10 In 2014, 20% of Canada’s general population self-reported a height and a weight that placed them in the obese category, up from approximately 15% in 2003.11 In our study, the proportion of kidney donors with obesity at the time of kidney donation was higher at 30%. This is concerning given that obesity is linked to the development of diabetes and hypertension, which are the most common causes of ESKD in Canada.
Limitations of our study include its retrospective nature and the possibility that there was selection bias related to the exclusion of approximately 10% of donors who did not have a weight recorded at the time of kidney donation. Other limitations include the relatively short post-donation follow-up and missing follow-up data from donors who came from another city or country and therefore did not follow-up with our program. Inactivity following surgery may have contributed to the trend of increasing weight following kidney donation, but this was not seen in the group with a healthy BMI and this finding would not be expected beyond the usual recovery time of 4 to 6 weeks. Although we did not have waist circumference measurements, this data would be additive to BMI data because higher waist circumference is associated with higher mortality and has not been examined among living kidney donors.12 The single-center design of the study also limits generalizability.
Our findings suggest the need for enhanced weight control efforts among kidney donors who are overweight or living with obesity, to reduce the risk of developing diabetes, cardiovascular disease, and ESKD. Current weight loss counseling in the donor clinic is likely ineffective because donor coordinators and nephrologists lack knowledge around obesity management. Time constraints and the inherent difficulty in effectively treating obesity in any population may also play a role. The recent US Preventive Services Task Force review of weight loss and weight loss maintenance interventions concluded that adults in the general population with a BMI of 30 kg/m2 or greater should be referred for multicomponent behavioral interventions within or outside a primary care setting (grade B recommendation). Further studies in the general population are needed to determine interventions for those who are classified as being overweight due to insufficient data, because they were often combined with adults with class I and II obesity in previous studies.13 Living kidney donor programs can support weight loss by counseling donors about the importance of weight loss and if accepted, direct referral for behavioral intervention to a weight management program and consultation with a donor’s primary care physician about weight loss services offered by their primary care program. However, further studies are needed to evaluate whether weight loss strategies will impact on long-term donor outcomes, including ESKD, diabetes, and hypertension.
Acknowledgments
We thank the living kidney donors who have improved the lives of patients with end-stage kidney disease, the devoted transplant surgeons, and the dedicated nurse coordinators and clerk who lead donors through their donation experience.
Footnotes
List of Abbreviations: BG, blood glucose; BMI, body mass index; CI, confidence interval; Diff., difference; DM2, type 2 diabetes mellitus; ESKD, end-stage kidney disease; HbA1c, hemoglobin A1c; KDIGO, Kidney Disease Improving Global Outcomes; kg, kilograms; REF, reference; SD, standard deviation.
Ethics Approval and Consent to Participate: This study was approved by The Ottawa Hospital Research Ethics Board.
Consent for Publication: We have the authors consent for publication.
Availability of Data and Materials: All data generated are included in this article.
Author Contributions: A.B. participated in the study design, data analysis, result interpretation, and paper writing. S.H. participated in the chart review and data collection. J.E., K.D.B., and G.K. participated in the performance of the research and paper writing. E.G.C. participated in the study design, data analysis, result interpretation, and paper writing.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Edward G. Clark  https://orcid.org/0000-0002-6767-1197
https://orcid.org/0000-0002-6767-1197
References
- 1. Bailey P, Edwards A, Courtney AE. Living kidney donation. BMJ. 2016;354:i4746. [DOI] [PubMed] [Google Scholar]
- 2. Grams ME, Sang YS, Levey AS, et al. Kidney-failure risk projection for the living kidney-donor candidate. N Engl J Med. 2016;374:411-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Locke JE, Reed RD, Massie A, et al. Obesity increases the risk of end-stage renal disease among living kidney donors. Kidney Int. 2017;91:699-703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Massie AB, Muzaale AD, Luo X, et al. Quantifying postdonation risk of ESRD in living kidney donors. J Am Soc Nephrol. 2017;28:2749-2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wainright JL, Robinson AM, Wilk AR, Klassen DK, Cherikh WS, Stewart DE. Risk of ESRD in prior living kidney donors. Am J Transplant. 2018;18(5):1129-1139. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization (WHO). Global health observatory data. http://www.who.int/gho/ncd/risk_factors/overweight/en/. Accessed February 21, 2018.
- 7. Mandelbrot DA, Pavlakis M, Danovitch GM, et al. The medical evaluation of living kidney donors: a survey of US transplant centers. Am J Transplant. 2007;7(10):2333-2343. [DOI] [PubMed] [Google Scholar]
- 8. Taler SJ, Messersmith EE, Leichtman AB, et al. Demographic, metabolic, and blood pressure characteristics of living kidney donors spanning five decades. Am J Transplant. 2013;13(2):390-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lentine KL, Kasiske BL, Levey AS, et al. KDIGO clinical practice guideline on the evaluation and care of living kidney donors. Transplantation. 2017;101(8, suppl 1):S1-S109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Issa N, Sanchez OA, Kukla A, et al. Weight gain after kidney donation: association with increased risks of type 2 diabetes and hypertension. Clin Transplant. 2018;32(9):e13360. [DOI] [PubMed] [Google Scholar]
- 11. Statistics Canada. https://www150.statcan.gc.ca/n1/pub/82-625-x/2015001/article/14185-eng.htm. Accessed February 11, 2019.
- 12. US Preventive Services Task Force, Curry SJ, Krist AH, et al. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US preventive services task force recommendation. JAMA. 2018;320(11):1163-1171. [DOI] [PubMed] [Google Scholar]
- 13. Jacobs EJ, Newton CC, Wang Y, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170(15):1293-1301. [DOI] [PubMed] [Google Scholar]