Abstract
Background:
Controversy exists as to the optimal treatment of superior labrum anterior to posterior (SLAP) tears in athletes. There are no systematic reviews evaluating return-to-sport (RTS) rates after arthroscopic SLAP repair and biceps tenodesis.
Purpose:
To compare the overall RTS rates in patients with primary type 2 SLAP tears who were managed with arthroscopic SLAP repair versus biceps tenodesis.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A review was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines by searching the MEDLINE (PubMed), Embase (Elsevier), and Cochrane Library databases. Inclusion criteria were clinical studies that evaluated RTS rates after arthroscopic SLAP repair, arthroscopic SLAP repair with partial rotator cuff debridement, and biceps tenodesis. The studies were analyzed for quality and inclusion in the final analysis. Data relevant to RTS rates were then extracted and compiled, and outcomes were compared.
Results:
Of the 337 studies initially identified, 15 (501 patient-athletes) met inclusion criteria. These consisted of 195 patients who underwent isolated arthroscopic SLAP repair (mean age, 31 years; mean follow-up, 3.2 years), 222 patients who underwent arthroscopic SLAP repair with partial rotator cuff debridement (mean age, 22 years; mean follow-up, 5.1 years), and 84 patients who underwent biceps tenodesis (mean age, 42 years; mean follow-up, 3.3 years). The overall RTS rates were high for all 3 procedures (SLAP repair, 79.5%; SLAP repair with rotator cuff debridement, 76.6%; biceps tenodesis, 84.5%), with biceps tenodesis having the highest overall rate. Biceps tenodesis also had the highest RTS rate at the preinjury level (78.6%) compared with SLAP repair (63.6%) and SLAP repair with rotator cuff debridement (66.7%).
Conclusion:
Primary arthroscopic SLAP repair, arthroscopic SLAP repair with partial rotator cuff debridement, and biceps tenodesis all provide high RTS rates. Biceps tenodesis as an operative treatment of primary SLAP lesions may demonstrate an overall higher RTS rate when compared with traditional SLAP repair in older athletes. More, higher level studies are needed that control for age, level of activity, and type of sport (overhead vs nonoverhead) to determine the efficacy of biceps tenodesis as a primary alternative to arthroscopic SLAP repair in young athletes who present with type 2 SLAP tears.
Keywords: SLAP tear, SLAP repair, biceps tenodesis, return to sport, systematic review
Type 2 superior labrum anterior to posterior (SLAP) tears are the most common SLAP tear variant and are a common cause of pain and disability in young active populations and overhead athletes.2,34 Initially described by Andrews et al,3 type 2 SLAP tears involve the detachment of the superior labrum and biceps anchor from the glenoid rim. These injuries are often a result of either direct trauma to the shoulder or degeneration from chronic overuse.21 Tears from chronic overuse are often encountered in overhead athletes and are proposed to be the result of either deceleration of the arm during the follow-through phase of throwing or the “peel-back mechanism” seen in the cocking phase in abduction and external rotation.3,7 While conservative treatment may be effective in some patients,11 if it fails, arthroscopic SLAP repair using suture anchor fixation is an effective treatment modality, yielding good results in young patients.6,10,14,29,32 However, several authors have reported conflicting patient satisfaction and return-to-sport (RTS) rates after arthroscopic SLAP repair in the older patient population and pitchers.6,10,14,15,19,30
Older age, overhead athlete status, and the presence of rotator cuff abnormalities have been proposed as patient variables significantly associated with either failure or prolonged recovery after type 2 SLAP repair.1,15,18,23,30,33 When failure or persistent pain after arthroscopic SLAP repair occurs, arthroscopic or open biceps tenodesis has been shown to be an effective revision procedure with reliable resolution of pain and improvement in range of motion.16,23,30 Therefore, recent studies have examined the outcomes of biceps tenodesis as an alternative procedure to primary SLAP repair. Controversy exists as to the optimal treatment of type 2 SLAP tears in young active adults and especially in overhead athletes.2 Several studies have directly compared type 2 SLAP repair and biceps tenodesis and found quicker RTS times and improved patient satisfaction in the biceps tenodesis group; however, results are limited by small sample sizes and heterogeneous patient populations, with older patients primarily undergoing biceps tenodesis.5,28 The purpose of this systematic review was to assess the RTS rates in patients with primary type 2 SLAP tears who were managed with arthroscopic SLAP repair as compared with biceps tenodesis.
Methods
Search Strategy
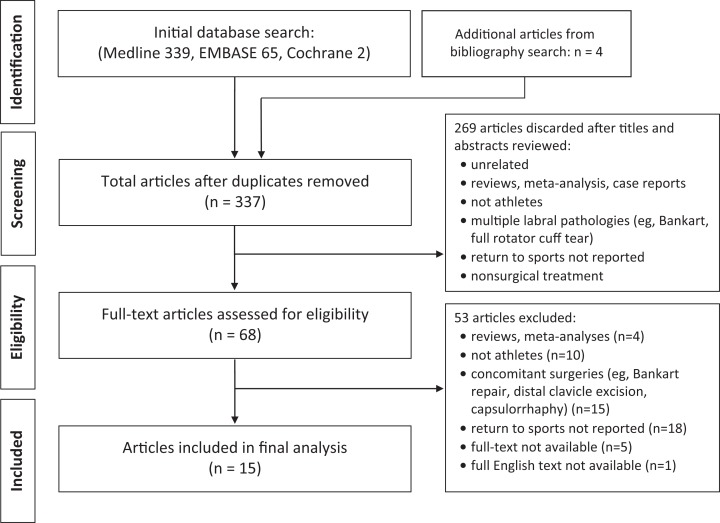
A systematic and rigorous search strategy was developed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Figure 1).24,31 The goal of the search was to identify articles with RTS rates for the following 3 procedures: arthroscopic SLAP repair, arthroscopic SLAP repair with partial rotator cuff debridement, and biceps tenodesis. This search yielded appropriate peer-reviewed articles for a systematic review with 4 phases. In phase 1 (“identification”), electronic databases were searched to find potentially relevant studies evaluating RTS after the surgical treatment of SLAP tears. The MEDLINE (PubMed), Embase (Elsevier), and Cochrane Library databases were searched on March 12, 2018, with the following Boolean search terms: (((superior labrum anterior and posterior repair) or (SLAP repair) or (biceps tenodesis)) AND ((return to sports) or (return to preinjury activity) or (athlete) or (athletics) or (athletic population) or (athlete population) or (return to competition) or (return to athletics))). No filter was applied, to maximize sensitivity.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flowchart of superior labrum anterior to posterior tear systematic reviews.
Eligibility Criteria
All search results were extracted and examined for relevance, and duplicate search results were discarded. In phase 2 (“screening”), titles and abstracts were screened for relevance. Reference lists of relevant articles were also manually searched for other relevant articles screened out of the database algorithms. Articles were filtered based on the following exclusion criteria: (1) non-English text, (2) population not athlete specific, (3) only abstract available, (4) no quantification of RTS outcomes, (5) treatment nonsurgical, (6) treatment not for SLAP tears (eg, biceps tenodesis performed to treat abnormalities other than SLAP tears), (7) surgical treatment including concomitant labral surgery (eg, Bankart repair), (8) studies included patients with full-thickness rotator cuff tears, (9) review article or meta-analysis, or (10) case report. The surgical procedures being reviewed included arthroscopic SLAP repair, arthroscopic SLAP repair with partial rotator cuff debridement, and biceps tenodesis for SLAP tears. In this analysis, we did not exclude studies that incorporated subacromial decompression. Moreover, we included military service members as an athletic population and did not exclude studies on military athletes. In this population, we equated return to full active duty as return to preinjury levels. Only studies that included RTS rates centering on a single surgical procedure or studies that specifically stratified mixed patient populations or surgical treatments were evaluated.
Article Review
In phase 3 (“eligibility”), all articles eligible after the screening phase were evaluated for inclusion criteria and relevant data on RTS rates and outcomes after 1 of the surgical treatments of interest. All articles were reviewed, assessed, and data-mined by 2 independent evaluators (H.A.-R., M.D.). All results were then compared to ensure consistency and accuracy. Any conflicts or issues were resolved by a review of the articles, and the senior author (X.L.) made the final determination.
Data Extraction and Assessment
In phase 4 (“studies included”), articles that met inclusion criteria were analyzed for quality, and data were extracted to be used in the review. The following items of data were extracted from the included articles: author, publication year, journal title, level of evidence, study design, surgical procedure, number of athletes, type of sports, number of participants in sport type, level of athletic participation, mean age at the time of surgery, sex, mean follow-up period, concomitant procedures, percentage of athletes who returned to sport, percentage of athletes who returned to preinjury levels of athletics, number and type of recurrent shoulder injuries, and subsequent procedures needed because of recurrent shoulder instability. A few studies included multiple surgical treatments, in which case treatment types were stratified and analyzed independent of other surgical procedures. In addition, several articles studied a mixed population (ie, nonathletes and athletes). In these cases, if the relevant RTS data were stratified, then only data from the athlete population and/or appropriate treatment group were extracted and included in the review.
Quality Assessment
To assess the quality of each cases series study that was included in the analysis, the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) was used.30 This risk-of-bias tool includes 7 criteria: (1) bias due to confounding, (2) bias in selection of participants, (3) bias in classification of interventions, (4) bias due to deviations from intended interventions, (5) bias due to missing data, (6) bias in measurement of outcomes, and (7) bias in selection of reported result. Each criterion was rated as having a low risk of bias or high risk of bias.
Results
After an extensive literature search and review, 15 studies met inclusion criteria and were incorporated into the final analysis: 11 studies∥ with level 4 evidence and 4 studies4,5,12,25 with level 3 evidence. The extracted data were divided into 3 groups: isolated SLAP repair, SLAP repair with rotator cuff debridement, and biceps tenodesis. Of the 15 articles, 7 studies4,9,20,22,26,27,33 included RTS data exclusively on patients who underwent SLAP repair with no other labral or rotator cuff abnormality (Table 1), 4 studies13,15,17,25 included RTS data on patients who underwent SLAP repair with rotator cuff debridement for concomitant SLAP tears and partial rotator cuff tears (Table 2), 2 studies23,28 included RTS data exclusively on patients who underwent biceps tenodesis for SLAP tears (Table 3), and 2 studies5,12 included RTS data for both biceps tenodesis and isolated SLAP repair (Tables 1 and 3).
TABLE 1.
Demographic Data for Included Isolated SLAP Repair Studiesa
| Author (Year) | LOE | Type of Surgery | No. of Athletes | Sports Played | Level of Play | Age at Surgery, Mean (Range), y | Sex Ratio, M:F | Mean Follow-up, y | Concomitant Procedures |
|---|---|---|---|---|---|---|---|---|---|
| Park et al27 (2013) | 4 | Isolated SLAP repair | 24 | 16 baseball, 3 javelin, 3 volleyball, 2 badminton (all overhead) | 12 collegiate, 10 professional, 2 national team | 22.7 (19-30) | 3:1 | 3.82 | None |
| Ek et al12 (2014) | 3 | Isolated SLAP repair | 10 | NR | NR | 31 (21-43) | All male | 2.9 | Subacromial debridement if needed |
| Maier et al22 (2013) | 4 | Isolated SLAP repair | 24 | 2 volleyball, 4 soccer (2 goalkeepers, 2 field players), 1 boxing, 1 climbing, 4 tennis, 1 badminton, 3 fitness (weightlifting), 1 basketball, 3 swimming, 2 cycling, 1 running, 1 Nordic walking | 24 amateur level | 36.45 (NR) | 5:1 | 3.85 | None |
| O’Brien et al26 (2002) | 4 | Isolated SLAP repair | 31 | NR | NR | 39 (16-71) | 28:3 | 3.7 | 6 acromioplasty for impingement |
| Boesmueller et al4 (2012) | 3 | Isolated SLAP repair | 21 | 1 kickboxing, 4 strength training, 2 volleyball, 1 soccer, 3 tennis, 1 military, 1 triathlon, 1 basketball, 3 martial arts, 1 field hockey, 1 handball, 2 multiple sports | 8 recreational, 13 competitive | 28 (18-44) | 20:1 | 2.5 | None |
| Boileau et al5 (2009) | 3 | Isolated SLAP repair | 10 | 7 overhead, 3 nonoverhead | 4 collegiate, 5 professional, 1 no organized sport | 37 (19-57) | All male | 2.9 | None |
| Cohen et al9 (2006) | 3 | Isolated SLAP repair | 29 | 8 throwing (6 pitchers, 2 fielders), 21 nonthrowing (football, lacrosse, hockey, skiing, volleyball, soccer) | NR | 34 (16-56) | NR | 3.67 | None |
| Yung et al33 (2008) | 4 | Isolated SLAP repair | 16 | 13 overhead, 3 nonoverhead | 5 national varsity/national level, 11 recreational | 24.2 (15-38) | 13:3 | 2.3 | None |
| Kim et al20 (2002) | 4 | Isolated SLAP repair | 30 | 18 overhead, 12 contact | 12 collegiate, 11 professional, 7 recreational | 26 (16-35) | 15:2 | 2.75 | None |
aF, female; LOE, level of evidence; M, male; NR, not reported; SLAP, superior labrum anterior to posterior.
TABLE 2.
Demographic Data for Included SLAP Repair With Rotator Cuff Debridement Studiesa
| Author (Year) | LOE | Type of Surgery | No. of Athletes | Sports Played | Level of Play | Age at Surgery, Mean (Range), y | Sex Ratio, M:F | Mean Follow-up, y | Concomitant Procedures |
|---|---|---|---|---|---|---|---|---|---|
| Gilliam et al15 (2018) | 4 | SLAP repair with rotator cuff debridement if needed | 133 | All baseball | 18 professional, 63 collegiate, 47 high school, 4 unable to recall level at time of injury | 19.5 (10.3-31.0) | All male | 6.5 | None |
| Neri et al25 (2011) | 3 | SLAP repair with rotator cuff debridement if needed | 23 | 20 baseball, 1 volleyball, 1 tennis, 1 water polo (all overhead) | 17 professional, 6 collegiate | 25 (18-45) | All male | 3.2 | None |
| Ide et al17 (2005) | 4 | SLAP repair with rotator cuff debridement if needed | 40 | 19 baseball, 5 handball, 4 volleyball, 3 basketball, 3 softball, 2 racquetball, 2 goalkeeping, 2 swimming (all overhead) | 36 competitive, 4 recreational | 24 (15-38) | 33:7 | 3.4 | None |
| Enad et al13 (2007) | 4 | SLAP repair with rotator cuff debridement if needed | 26 | Military activity and other unspecified sport activity | 26 competitive | 31.6 (22-41) | NR | 2.5 | Subacromial decompression if needed |
aF, female; LOE, level of evidence; M, male; NR, not reported; SLAP, superior labrum anterior to posterior.
TABLE 3.
Demographic Data for Included Biceps Tenodesis Studiesa
| Author (Year) | LOE | Type of Surgery | No. of Athletes | Sports Played | Level of Play | Age at Surgery, Mean (Range), y | Sex Ratio, M:F | Mean Follow-up, y | Concomitant Procedures |
|---|---|---|---|---|---|---|---|---|---|
| Pogorzelski et al28 (2018) | 4 | Open subpectoral biceps tenodesis | 16 | 1 baseball, 1 basketball, 4 multiple sports, 1 martial arts, 1 rock climbing, 1 volleyball, 2 weightlifting, 1 running, 2 skiing, 1 snowboarding, 1 soccer (11 overhead, 5 nonoverhead) | Recreational | 38 (21-45) | NR | 3.4 | None |
| Ek et al12 (2014) | 3 | Open subpectoral biceps tenodesis | 11 | NR | NR | 47 (30-59) | NR | 2.6 | Subacromial debridement if needed |
| Boileau et al5 (2009) | 3 | Arthroscopic biceps tenodesis | 15 | 8 overhead, 7 nonoverhead | 1 recreational, 5 collegiate, 6 professional, 3 no organized sport | 52 (28-64) | 3:2 | 2.8 | None |
| McCormick et al23 (2014) | 4 | Open subpectoral biceps tenodesis | 42 | Military activity | Active military duty | 39.2 (18-50) | 5:1 | 3.5 | 15% of patients required subacromial debridement |
aF, female; LOE, level of evidence; M, male; NR, not reported.
Overall, these studies included 501 patient-athletes, of whom 195 patients underwent isolated arthroscopic SLAP repair, 84 patients underwent biceps tenodesis, and 222 patients underwent arthroscopic SLAP repair with rotator cuff debridement. While a majority of patients included were overhead athletes, we were not able to isolate the RTS rates for overhead athletes for multiple reasons: (1) many studies included mixed athletic populations that could not be stratified; (2) some studies did not specify the specific sport, or sport type, played by the patients; and (3) the scarcity of RTS data after biceps tenodesis for SLAP tears would have substantially limited the sample size in this group.
The RTS data for the included studies and a summary of results for the 3 treatment groups are included in Tables 4 and 5, respectively. All included studies had a minimum mean follow-up of 2 years.
TABLE 4.
Return-to-Sport Data for All Included Studiesa
| Author (Year) | Return to Sport, % (n) | Return to Preinjury Level of Sport, % (n) | Subsequent Procedures | Other Relevant Findings/Complications |
|---|---|---|---|---|
| Pogorzelski et al28 (2018) | 100 (16/16) | 68.8 (11/16) | None reported | One patient suffered from adhesive capsulitis and was treated nonoperatively. Among overhead athletes, 80% returned to sport at the same, or slightly below, preinjury level. |
| Ek et al12 (2014) (biceps tenodesis) | 73 (8/11) | 73 (8/11) | None reported | The mean time for patients to RTS was reported to be 6.8 months postoperatively. One failed tenodesis, presenting with a “Popeye” deformity at latest follow-up. No revision or corrective surgery was needed in this case. |
| Boileau et al5 (2009) (biceps tenodesis) | 87 (13/15) | 87 (13/15) | None reported | None reported |
| McCormick et al23 (2014) | 81 (34/42) | 81 (34/42) | None reported | All surgical procedures were performed for failed SLAP repair and in active military members. |
| Gilliam et al15 (2018) | 64 (85/133) | 64 (85/133) | 9 revision labral repairs, 1 biceps tenodesis | 59% of pitchers were able to return to play at preinjury levels, while 76% of nonpitchers were able to do so. Moreover, of those who did not return to sport, 67% said that it was because of the surgical procedure. Furthermore, overall, 7.5% (10/133) of the SLAP repairs failed. Rotator cuff tears above 25% were excluded from this study. |
| Neri et al25 (2011) | 83 (19/23) | 57 (13/23) | None reported | Partial-thickness rotator cuff tears (defined as <10%-40% thickness tears) were present in 8 of 23 (35%) athletes. Only 12% of those with concomitant rotator cuff tears returned to prior levels of sport. On average, those who returned to sport did so at 8.8 months postoperatively. |
| Ide et al17 (2005) | 95 (38/40) | 75 (30/40) | None reported | Two patients could not return to their previous sport at any level. Both had positive active compression and pain in the anterior apprehension test position. |
| Enad et al13 (2007) | 100 (26/26) | 77 (20/26) | None reported | There were 30 total military patients, with 26 active in sports; 29 (97%) returned to full military duty at a mean of 4.4 months. One patient did not return to full duty because of recurrent pain and catching. |
| Ek et al12 (2014) (SLAP repair) | 60 (6/10) | 60 (6/10) | None reported | The mean time for patients to RTS was reported to be 8.2 months postoperatively. Postoperative stiffness occurred in 2 cases; it was treated conservatively with physical therapy and subsequently resolved. |
| Park et al27 (2013) | 50 (12/24) | 50 (12/24) | None reported | There was a trend toward a higher return rate in the other overhead athletes (75%) compared with the baseball players (38%), but the sample size was too limited to make this statistically significant. There were also 2 failed repairs with radiologically confirmed retearing of the labrum. |
| Maier et al22 (2013) | 75 (18/24) | 58 (14/24) | 2 revisions | Four patients who returned to sport at a lower level cited shoulder-related reasons for sport impairment. |
| O’Brien et al26 (2002) | 87 (27/31) | 52 (16/31) | 1 revision | 44% of patients were documented to have positive impingement signs after surgery. |
| Boesmueller et al4 (2012) | 86 (18/21) | 86 (18/21) | 1 revision | Thirteen patients had mild to moderate residual pain. |
| Boileau et al5 (2009) (SLAP repair) | 20 (2/10) | 20 (2/10) | 4 biceps tenodeses | Four SLAP repairs failed and were treated with biceps tenodesis. |
| Cohen et al9 (2006) | 93 (27/29) | 48 (14/29) | 1 revision | Seven patients had impingement at follow-up, and 2 patients had instability. One patient had a retear that was explained by noncompliance of postoperative restrictions. |
| Yung et al33 (2008) | 94 (15/16) | 94 (15/16) | None reported | The mean time for patients to RTS was reported to be 9.4 months postoperatively, although it was stated that overhead athletes took a longer period of time to return to preinjury levels. Only 1 elite handball athlete did not RTS at last follow-up, citing pain and weakness of the supraspinatus. |
| Kim et al20 (2002) | 100 (30/30) | 90 (27/30) | None reported | Although 27 patients returned to preinjury levels of sport and competition, only 14 athletes graded their RTS a zero, representing no limitation in sport activities. This study also defined moderate to no limitations in athletic ability as successful return to preinjury levels, such that anything above 80% of the preinjury level was considered a successful RTS. |
aRTS, return to sport; SLAP, superior labrum anterior to posterior.
TABLE 5.
Comparison of Return-to-Sport Rates for Different SLAP Tear Proceduresa
| Procedure | No. of Athletes | No. of Studies | Return to Sport, % (n) | Return to Preinjury Level of Sport,b % (n) | Return to Preinjury Level of Sport,c % (n) |
|---|---|---|---|---|---|
| Isolated SLAP repair | 195 | 9d | 79.5 (155/195) | 63.6 (124/195) | 80.0 (124/155) |
| SLAP repair with rotator cuff debridement | 222 | 4 | 76.6 (170/222) | 66.7 (148/222) | 87.1 (148/170) |
| Biceps tenodesis | 84 | 4d | 84.5 (71/84) | 78.6 (66/84) | 93.0 (66/71) |
aSLAP, superior labrum anterior to posterior.
bPercentage of total athletes.
cPercentage of athletes who returned to sport.
Isolated Arthroscopic SLAP Repair
Studies that evaluated RTS after isolated SLAP repair documented a wide range of RTS rates, 20% to 100%, with a mean rate of 79.5% among all patients. Of the athletes who returned to sport, 80.0% were able to return to preinjury levels of performance, but this only amounted to 63.6% of total athletes returning to preinjury levels of performance. The mean age of athletes in this group was 31 years, with a mean follow-up of 3.24 years.
Arthroscopic SLAP Repair With Rotator Cuff Debridement
Four studies13,15,17,25 included RTS rates among athletes who had SLAP tears with partial rotator cuff tears that were managed with SLAP repair and rotator cuff debridement. Between these studies, RTS rates ranged from 64% to 100%, with a mean RTS rate of 76.6% among all patients. Of these athletes who returned to sport, 87.1% were able to return to preinjury levels of performance; this amounted to 66.7% of total athletes returning to preinjury levels of performance. Only 1 study13 included concomitant treatment outside of SLAP repair and rotator cuff debridement, with 8 patients who underwent subacromial debridement. The mean age of athletes in this group was 22 years, with a mean follow-up of 5.13 years.
Biceps Tenodesis
Studies examining RTS after biceps tenodesis for SLAP tears showed a range of RTS rates of 73% to 100%, with a mean rate of 84.5% among all patients. Of those who returned to sport, 93.0% achieved preinjury performance levels, while 78.6% of the total athletes who underwent biceps tenodesis returned to preinjury levels. Of the 4 studies, 1 study5 evaluated outcomes after arthroscopic biceps tenodesis, and the other 3 studies12,23,28 analyzed outcomes after subpectoral biceps tenodesis. Moreover, 3 of these studies5,12,28 only reported patients undergoing primary surgery for the SLAP lesion, while the fourth study23 evaluated biceps tenodesis as a revision procedure after SLAP repair failure. If these revision cases were excluded, the RTS rate would be 88.1%, with 76.2% of all patients returning to preinjury levels of performance. The mean age of athletes in this group was 42 years, with a mean follow-up of 3.26 years.
Quality Assessment
The quality and resultant risk-of-bias assessment is summarized in Table 6. Eleven of the 15 included studies had some potential for bias due to confounding factors and participant selection bias. This was likely the result of not having homogeneous patient populations. Seven of the 15 included studies had some risk of bias due to missing data from patient loss to follow-up. Moreover, all studies had some risk of bias in outcome measures, as RTS is often a subjective measure.
TABLE 6.
Risk of Bias in Included Studies
| Author (Year) | Bias Due to Confounding | Bias in Selection of Participants | Bias in Classification of Interventions | Bias Due to Deviations From Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of Reported Result |
|---|---|---|---|---|---|---|---|
| Park et al27 (2013) | High | High | Low | Low | Low | High | Low |
| Ek et al12 (2014) | High | High | Low | Low | High | High | Low |
| Maier et al22 (2013) | Low | Low | Low | Low | Low | High | Low |
| O’Brien et al26 (1998) | Low | Low | Low | Low | Low | High | Low |
| Boesmueller et al4 (2012) | High | Low | Low | Low | Low | High | Low |
| Boileau et al5 (2009) | High | High | Low | Low | Low | High | Low |
| Cohen et al9 (2006) | Low | High | Low | Low | High | High | Low |
| Yung et al33 (2008) | High | High | Low | Low | Low | High | Low |
| Kim et al20 (2003) | High | Low | Low | Low | High | High | Low |
| Pogorzelski et al28 (2018) | High | High | Low | Low | High | High | Low |
| McCormick et al23 (2014) | High | High | Low | Low | Low | High | Low |
| Neri et al25 (2011) | High | High | Low | Low | High | High | Low |
| Enad et al13 (2007) | High | High | Low | Low | High | High | Low |
| Gilliam et al15 (2018) | High | High | Low | Low | Low | High | Low |
| Ide et al17 (2005) | Low | High | Low | Low | High | High | Low |
Discussion
The purpose of this systematic review was to determine the RTS rate after arthroscopic SLAP repair and biceps tenodesis in athletes with SLAP tears. We also included patients undergoing SLAP repair with rotator cuff debridement as a separate group, as this is a relatively common concomitant procedure in the available studies and may represent a different patient group. Overall, the RTS rates for all 3 procedures were high (SLAP repair: 79.5%; SLAP repair with rotator cuff debridement: 76.6%; biceps tenodesis: 84.5%), with biceps tenodesis having the highest overall RTS rate. Furthermore, biceps tenodesis also had the highest RTS rate at the preinjury level (78.6%) compared with both SLAP repair (63.6%) and SLAP repair with rotator cuff debridement (66.7%).
Although these pooled data provide some valuable information on return to overall sport participation after SLAP repair and biceps tenodesis, the results are limited because of the heterogeneity of the study populations included. Moreover, without conducting a meta-analysis, we cannot say for certain that one type of surgery is superior to another, especially given the differences in age and sporting activity level between the 3 groups. Additionally, a randomized controlled trial ultimately would be needed to determine which procedure is optimal for RTS after a SLAP tear in athletes. The ability to return to playing sport and to preinjury activity levels can be very different for pitchers, overhead athletes, military personnel, and nonoverhead athletes. Traditionally, primary SLAP repair has been performed on younger athletes, and biceps tenodesis has been reserved for older patients or patients who failed primary SLAP repair. The lack of age-matched, large randomized studies comparing the 2 procedures limits our results and should be controlled for in future prospective studies. Our data support the need for such studies, as the mean age for patients who underwent biceps tenodesis was 42 years while that for patients who underwent isolated SLAP repair was 31 years.
A number of studies have reported consistently good results with pain relief and improved shoulder function after SLAP repair for type 2 lesions. Denard et al10 examined the outcomes of all arthroscopically repaired SLAP tears in 55 patients at a mean follow-up of 77 months. They found that in 87% of the cases, a good or excellent outcome was achieved as measured by the American Shoulder and Elbow Surgeons (ASES) and University of California, Los Angeles (UCLA) scores. Additionally, 82% of patients were able to return to sport. Although not statistically significant, they found that age older than 40 years was a variable associated with worse outcomes. Park et al27 confirmed these findings in a study evaluating the clinical outcomes of type 2 SLAP repair in elite overhead athletes. The authors retrospectively reviewed 24 overhead athletes and found that SLAP repair significantly improved visual analog scale for pain (5.7 to 2.0), subjective shoulder function, and ASES scores (55.8 to 87.1). However, they noted that only 50% of patients were able to return to sport. Furthermore, baseball players only had a 38% RTS rate compared with 75% for overhead athletes in other sports. Similarly, Gilliam et al15 found that despite improvement in Kerlan-Jobe Orthopaedic Clinic (KJOC) scores, the RTS rate after SLAP repair was 64%. Baseball pitchers had a 59% RTS rate versus 76% for nonpitchers. These 3 studies, along with others, have shown that arthroscopic type 2 SLAP repair does provide consistent improvement in pain and shoulder function; however, the ability to return to sport in overhead athletes, baseball players, and especially pitchers has been less consistent. The variability in RTS rates for different populations of athletes highlights the limitation of pooled data owing to the heterogeneity of the type of sports included in each of these studies.
Because of the difficulty in achieving high RTS rates in select populations after arthroscopic SLAP repair, biceps tenodesis as a primary procedure has emerged as a good surgical option. McCormick et al23 were the first to show that biceps tenodesis as a revision procedure for failed SLAP repair can provide consistently good results. They evaluated 42 patients for a mean 3.5 years after biceps tenodesis and reported an 81% RTS rate, with a statistically significant improvement in ASES, Single Assessment Numeric Evaluation (SANE), Western Ontario Shoulder Instability Index (WOSI), and shoulder range of motion values. Boileau et al5 recently showed that biceps tenodesis is an effective primary procedure for type 2 SLAP tears. In this study, 10 patients underwent SLAP repair, and 15 patients underwent arthroscopic biceps tenodesis. Of patients who underwent biceps tenodesis, 87% returned to sport or to prior levels of sport participation, whereas 20% of patients in the SLAP repair group were unable to do so. It must be noted that the mean age of the biceps tenodesis group was 52 years versus 37 years in the SLAP repair group. This difference in ages may explain the RTS rates, as older athletes are more likely to participate at lower levels of competition and may put less strain on their shoulders compared with younger athletes.
Although again limited by the heterogeneity of the study populations with wide age ranges, our analysis agrees with that of Boileau et al5 in that primary biceps tenodesis is an effective procedure for SLAP tears and allows a high rate of RTS, especially in the older athletic population. However, in professional baseball players, Chalmers et al8 reported that of the 17 players who underwent biceps tenodesis, the overall rate of return to baseball was 35%, and only 17% of pitchers compared with 80% of positional players were able to return to prior levels of play. This discrepancy in outcomes highlights the differences between overhead compared with nonoverhead athletes. The majority of the studies that we included in this review did not separate these 2 groups. Controversy still exists in the optimal management of SLAP tears in overhead athletes, as there is a paucity of studies with level 1 or 2 evidence on the outcomes of primary biceps tenodesis compared with SLAP repair in this patient group.2
A limitation of this systematic review is the inability to control for a diverse population of athletes in the included studies. Most included studies had a mixed population of overhead athletes of all ages and had a combination of baseball pitchers and nonpitchers. Additionally, some studies included professional athletes along with amateur high school and collegiate athletes. Moreover, we also included military personnel as athletes. While these populations have many similarities, they often have differing degrees of rehabilitation, standards for returning to activity/sport, and shoulder usage. As previously stated, the minimum follow-up was 2 years. While this is a nontrivial amount of time, it is possible that some patients may have restricted or stopped sporting activity after the follow-up period; therefore, the data from this study may not be representative for long-term RTS. As discussed previously, this study is also limited by how “return to sport” was defined. There is disagreement in the literature on what is meant by the term and whether it means returning to sport at preinjury levels or just successfully returning to sport participation, and often, this is a subjective measure based on the patient. While an analysis of these studies may be helpful in forming expectations for both patients and surgeons, comparing surgical outcomes from these pooled studies may be limited by population heterogeneity, lack of randomized controlled trials, or meta-analysis of comparative studies. However, to our knowledge, this systematic review does provide valuable pooled data from the currently available literature on RTS after isolated SLAP repair, SLAP repair with rotator cuff debridement, and biceps tenodesis.
Conclusion
This systematic review assessed the difference in RTS rates in patients with primary SLAP tears. Based on our review, primary arthroscopic SLAP repair, arthroscopic SLAP repair with rotator cuff debridement, and biceps tenodesis all provide high RTS rates after surgery. Although limited by the heterogeneity of the study populations, these pooled data do provide orthopaedic surgeons with valuable information to counsel patients and athletes. Future age-matched comparative studies are needed to further elucidate the optimal treatment for a SLAP tear in overhead compared with nonoverhead athletes as well as various athlete populations to allow RTS.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: X.L. has received consulting fees from DePuy Mitek, Stryker, and Tornier and hospitality payments from Encore Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abbot AE, Li X, Busconi BD. Arthroscopic treatment of concomitant superior labral anterior posterior (SLAP) lesions and rotator cuff tears in patients over the age of 45 years. Am J Sports Med. 2009;37:1358–1362. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad CS. Editorial commentary: the shoulder biceps tendon and baseball continue their controversial relationship. Arthroscopy. 2018;34:752–753. [DOI] [PubMed] [Google Scholar]
- 3. Andrews JR, Carson WG, Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337–341. [DOI] [PubMed] [Google Scholar]
- 4. Boesmueller S, Mayerhofer S, Huf W, Fialka C. Short-term clinical results after arthroscopic type II SLAP repair. Wien Klin Wochenschr. 2012;124:370–376. [DOI] [PubMed] [Google Scholar]
- 5. Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37:929–936. [DOI] [PubMed] [Google Scholar]
- 6. Brockmeier SF, Voos JE, Williams RJ, 3rd, et al. Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Joint Surg Am. 2009;91:1595–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Burkhart SS, Morgan CD. The peel-back mechanism: its role in producing and extending posterior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy. 1998;14:637–640. [DOI] [PubMed] [Google Scholar]
- 8. Chalmers PN, Erickson BJ, Verma NN, D’Angelo J, Romeo AA. Incidence and return to play after biceps tenodesis in professional baseball players. Arthroscopy. 2018;34:747–751. [DOI] [PubMed] [Google Scholar]
- 9. Cohen DB, Coleman S, Drakos MC, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22:136–142. [DOI] [PubMed] [Google Scholar]
- 10. Denard PJ, Ladermann A, Burkhart SS. Long-term outcome after arthroscopic repair of type II SLAP lesions: results according to age and workers’ compensation status. Arthroscopy. 2012;28:451–457. [DOI] [PubMed] [Google Scholar]
- 11. Edwards SL, Lee JA, Bell JE, et al. Nonoperative treatment of superior labrum anterior posterior tears: improvements in pain, function, and quality of life. Am J Sports Med. 2010;38:1456–1461. [DOI] [PubMed] [Google Scholar]
- 12. Ek ET, Shi LL, Tompson JD, Freehill MT, Warner JJ. Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tenodesis. J Shoulder Elbow Surg. 2014;23:1059–1065. [DOI] [PubMed] [Google Scholar]
- 13. Enad JG, Gaines RJ, White SM, Kurtz CA. Arthroscopic superior labrum anterior-posterior repair in military patients. J Shoulder Elbow Surg. 2007;16:300–305. [DOI] [PubMed] [Google Scholar]
- 14. Friel NA, Karas V, Slabaugh MA, Cole BJ. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19:859–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gilliam BD, Douglas L, Fleisig GS, et al. Return to play and outcomes in baseball players after superior labral anterior-posterior repairs. Am J Sports Med. 2018;46:109–115. [DOI] [PubMed] [Google Scholar]
- 16. Gupta AK, Bruce B, Klosterman EL, McCormick F, Harris J, Romeo AA. Subpectoral biceps tenodesis for failed type II SLAP repair. Orthopedics. 2013;36:e723–e728. [DOI] [PubMed] [Google Scholar]
- 17. Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33:507–514. [DOI] [PubMed] [Google Scholar]
- 18. Kanatli U, Ozturk BY, Bolukbasi S. Arthroscopic repair of type II superior labrum anterior posterior (SLAP) lesions in patients over the age of 45 years: a prospective study. Arch Orthop Trauma Surg. 2011;131:1107–1113. [DOI] [PubMed] [Google Scholar]
- 19. Katz LM, Hsu S, Miller SL, et al. Poor outcomes after SLAP repair: descriptive analysis and prognosis. Arthroscopy. 2009;25:849–855. [DOI] [PubMed] [Google Scholar]
- 20. Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84:981–985. [DOI] [PubMed] [Google Scholar]
- 21. Li X, Lin TJ, Jager M, et al. Management of type II superior labrum anterior posterior lesions: a review of the literature. Orthop Rev (Pavia). 2010;2:e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maier D, Jaeger M, Ogon P, Bornebusch L, Izadpanah K, Suedkamp NP. Suture anchors or transglenoidal sutures for arthroscopic repair of isolated SLAP-2 lesions? A matched-pair comparison of functional outcome and return to sports. Arch Orthop Trauma Surg. 2013;133:227–235. [DOI] [PubMed] [Google Scholar]
- 23. McCormick F, Nwachukwu BU, Solomon D, et al. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. Am J Sports Med. 2014;42:820–825. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 25. Neri BR, ElAttrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of type II superior labral anterior posterior repairs in elite overhead athletes: effect of concomitant partial-thickness rotator cuff tears. Am J Sports Med. 2011;39:114–120. [DOI] [PubMed] [Google Scholar]
- 26. O’Brien SJ, Allen AA, Coleman SH, Drakos MC. The trans-rotator cuff approach to SLAP lesions: technical aspects for repair and a clinical follow-up of 31 patients at a minimum of 2 years. Arthroscopy. 2002;18:372–377. [DOI] [PubMed] [Google Scholar]
- 27. Park JY, Chung SW, Jeon SH, Lee JG, Oh KS. Clinical and radiological outcomes of type 2 superior labral anterior posterior repairs in elite overhead athletes. Am J Sports Med. 2013;41:1372–1379. [DOI] [PubMed] [Google Scholar]
- 28. Pogorzelski J, Horan MP, Hussain ZB, Vap A, Fritz EM, Millett PJ. Subpectoral biceps tenodesis for treatment of isolated type II SLAP lesions in a young and active population. Arthroscopy. 2018;34:371–376. [DOI] [PubMed] [Google Scholar]
- 29. Popp D, Schoffl V. Superior labral anterior posterior lesions of the shoulder: current diagnostic and therapeutic standards. World J Orthop. 2015;6:660–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41:880–886. [DOI] [PubMed] [Google Scholar]
- 31. Vrabel M. Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Oncol Nurs Forum. 2015;42:552–554. [DOI] [PubMed] [Google Scholar]
- 32. Werner BC, Brockmeier SF, Miller MD. Etiology, diagnosis, and management of failed SLAP repair. J Am Acad Orthop Surg. 2014;22:554–565. [DOI] [PubMed] [Google Scholar]
- 33. Yung PS, Fong DT, Kong MF, et al. Arthroscopic repair of isolated type II superior labrum anterior-posterior lesion. Knee Surg Sports Traumatol Arthrosc. 2008;16:1151–1157. [DOI] [PubMed] [Google Scholar]
- 34. Zhang AL, Kreulen C, Ngo SS, Hame SL, Wang JC, Gamradt SC. Demographic trends in arthroscopic SLAP repair in the United States. Am J Sports Med. 2012;40:1144–1147. [DOI] [PubMed] [Google Scholar]