Abstract
Objective
The double-bundle (DB) techniques are considered to yield better stability of the knee compared with single-bundle (SB) for anterior cruciate ligament (ACL) reconstruction. However, most studies followed up patients in short to middle-term within 5 years, and the longer-term efficacy of SB and DB ACL reconstruction is still beyond consensus. The purpose of this meta-analysis is to compare the longer-term efficacy between double-bundle (DB) and single-bundle (SB) techniques.
Methods
PubMed, EMBASE, and Cochrane Library databases were searched for relevant articles published up to November, 2017 with an English language restriction. The searches were limited to human subjects and randomized controlled trials (RCTs). In addition, the reference lists of identified articles were checked manually to avoid missing other potentially eligible studies. This process was performed iteratively until no additional articles could be included. The quality of the included studies was assessed using The Cochrane Collaboration's risk of bias tool. All statistical analyses were performed with Review Manager soft-ware.
Results
A total of five RCTs involving 294 patients were included finally. No studies were excluded due to insufficient data or low quality. The pooled results showed no statistically significant difference between SB and double bundle DB reconstructions for Lysholm, IKDC, pivot shift, KT scores, and the development of osteoarthritis at a minimum of 5 years. No significant heterogeneity was found across all outcomes.
Conclusion
The best available evidence demonstrated that SB and DB techniques could yield similar efficacy for ACL reconstruction. And no superiority was founded in DB ACL reconstruction with a minimal 5-year follow-up. Given that, the relatively simple and proven techniques of SB ACL reconstruction may be preferable for orthopedic surgeons.
Level of evidence: Level I, Therapeutic Study.
Keywords: Anterior cruciate ligament, Reconstruction, Single bundle, Double bundle
Introduction
The anterior cruciate ligament (ACL), which mainly contributes to restricting anterior tibial translation and secondly to restricting rotational movement of the knee, plays an important role in both static and dynamic stability of the knee.1 The ACL injures are usually caused by deceleration, non-contact injuries, jumping, or sideways cutting movements,2 and about 250,000 ACL injuries are reported to happen annually in the United States.3
Patients with ACL injuries are unlikely to keep normal function and stability of the knee, and are susceptible to several secondary injuries including meniscal injuries and knee osteoarthritis (OA).4 The techniques of single-bundle (SB) ACL reconstruction using patellar or hamstring tendons has been greatly evolved and been regarded as the golden standard for the surgical treatment of ACL rupture over the decades. However, the intact ACL consists of the anteromedial bundle and the posterolateral bundle.1 In 1983, Mott et al firstly carried out to reconstruct both anteromedial bundle and the posterolateral bundle of the ACL.5 Till now, the SB and double-bundle (DB) techniques have been greatly improved by updating the methods of grafts, fixation, tunnels position, as well as postoperative rehabilitation. Several authors demonstrated that DB techniques yielded better stability and kinematics of the knee than SB techniques.6 However, techniques are able to reconstruct significant portions of the anteromedial and posterolateral bundles if the tunnels are placed correctly. Essentially, DB techniques demand excellent surgical skills, double fixation materials, and more invasions compared with SB techniques. There is no consensus whether DB techniques are more suitable than SB techniques for standard ACL reconstruction. In a review of overlapping meta-analyses, the available evidence indicated that DB techniques could generate better stability and similar clinical outcomes in short-term follow-up.7 In a recent meta-analysis, Chen et al. reported better rotational stability and osteoarthritis prevention for DB ACL reconstruction in mid-term follow-up.8 However, a mid-term follow-up may be too short to detect the changes of osteoarthritis development, and evidence for longer-term efficacy comparing SB and DB techniques is still lacking.
The purpose of this meta-analysis is to compare the long-term efficacy between DB and SB techniques. Our hypothesis is that DB techniques have a better performance of knee stability than SB techniques for ACL reconstruction.
Methods
The meta-analysis was designed and conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.9
Research strategy
Two authors (ZD and YS) independently searched the PubMed, EMBASE, and the Cochrane Library databases for relevant articles published up to November, 2017. The search algorithm was structured by different combination of keywords: (“Randomized.
Controlled Trials” OR trial OR placebo OR controlled OR Random*) AND (“anterior cruciate ligament” OR “intra-articular knee ligament” OR ACL) AND (injury OR rupture OR torn OR trauma) AND (“single bundle” OR “double bundle” OR “two bundles” OR “anatomic bundle” OR SB OR DB) AND (“Reconstructive Surgical Procedures” OR Arthroscopy OR “Joint instability” OR Reconstructions OR Laxity.
OR rotation OR “rotary motion” OR function). An English language restriction was imposed. The searches were limited to human subjects and randomized controlled trials (RCTs). In addition, the reference lists of identified articles were checked manually to avoid missing other potentially eligible studies. This process was performed iteratively until no additional articles could be included.
Inclusion and exclusion criteria
The following selection criteria for inclusive articles were applied: a) design: prospective randomized controlled trails, level 1 or 2; b) population: adults and/or adolescents; c) intervention: anterior cruciate ligament reconstruction; d) comparison: single bundle versus double bundle; e) outcome: at least one of following clinical outcomes: International Knee Documentation Committee (IKDC) scores or grading, Lysholm scores, pivot-shift test, side-to-side differences, and osteoarthritis changes; f) a minimal follow-up of 5 years. Studies were excluded according to following criteria: a) cohort studies, retrospective studies, observational studies, case–control studies, case series or reports, or review; b) animal studies, cadaver studies, or laboratory studies; c) study without comparing SB and DB ACL reconstruction; d) concomitant with posterior cruciate ligament injury or collateral ligaments injury;e) follow-up less than 5 years. Any disagreements between the reviewers was resolved by consensus or by discussion with the corresponding author when consensus was not reached. (Where there was disagreement or doubt, the full article was retrieved. The same two authors independently assessed the full study report to see if it met the review inclusion criteria. The corresponding author was consulted in cases of unresolved disagreement.)
Data extraction
After eligible studies were identified according to predefined selected criteria, the same two authors independently extracted the following data: the first authors, study design, year of publication, the number of patients, patients characteristics, length of follow-up, and the outcomes data. The IKDC grading, classified as A, B, C, and D, were divided into normal group (A and B) and abnormal group (C and D), as well as the outcomes of pivot test which were divided into negative group (A and B) and positive group (C and D). Osteoarthritis changes were grouped into normal and abnormal outcomes according to Kellgren–Lawrence classification. Extracted data were then entered into a standardized Excel (Microsoft Corp) file, and were checked by the corresponding author. Any disagreements between the reviewers was resolved by consensus or by discussion with the corresponding author when consensus was not reached.
Risk of bias assessment
Two authors (YN and JQ) independently assessed the risk of bias for each identified study. The Cochrane Collaboration's risk of bias tool was applied according to six items as follows10: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. Each outcome of these items was expressed as low, unclear, or high bias. Publication bias was not assessed due to the limited number of studies included in this meta-analysis. Any disagreements between the reviewers was resolved by consensus or by discussion with the corresponding author when consensus was not reached.
Statistical analysis
Differences were expressed as risk ratio (RR) or risk difference (RD) with 95% confidence interval (CI) for dichotomous outcomes, and weighted mean differences (WMDs) with 95% CIs for continuous outcomes. Heterogeneity across studies was tested by using I2 statistic. Studies with an I2 statistic of 25%–50% were considered as low heterogeneity, those with an I2 statistic of 50%–75% were considered as moderate heterogeneity, and those with an I2 statistic of >75% were considered as high heterogeneity. Significant heterogeneity was considered when I2 > 50%, or P < 0.1. A fixed-effects model was used for the outcomes data when there was no statistically significant heterogeneity, otherwise a random-effects model was used. A P value <0.05 was judged as statistically significant, except where otherwise specified. All statistical analyses were performed with Review Manager soft-ware (version 5.3; Nordic Cochrane Centre, The Cochrane Collaboration).
Results
Search results
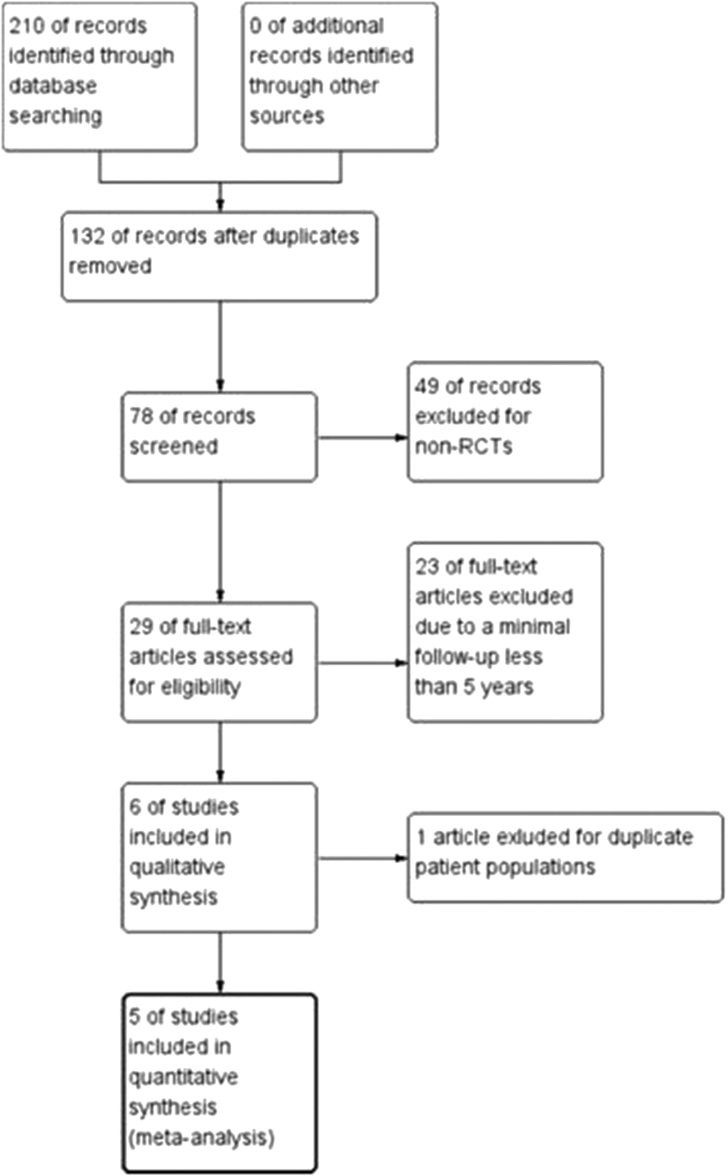
A total of 210 studies were generated by the initial database search. One hundred and thirty-two records were removed due to duplicate studies and, 49 records were excluded based on screening the titles and abstracts. The remaining 29 full-text articles were reviewed for more detail evaluation, and 23 full-text articles were excluded due to a minimal follow-up less than 5 years. Six studies were included in qualitative synthesis, and one of them was excluded due to duplicate patient populations. Eventually, five RCTs that conformed to the inclusion criteria were included in this meta-analysis. The flow diagram of selection process for the meta-analysis is shown in Fig. 1.
Fig. 1.
The flow diagram of the selection process.
Characteristics of included studies
This meta-analysis finally enrolled a total of 294 patients with a minimal follow-up of 5 years (range, 5–10 years). The baseline characteristics of included studies were present in Table 1. All five studies had a clear description of surgeries. Each of included studies has at least two applicable measurement outcomes. The outcomes data of included studies were listed in Table 2.
Table 1.
Demographic characteristics of included studies.
| Study | Year | Country | Level of Evidence | Sample Size SB DB | Mean Age (years) SB DB | ||
|---|---|---|---|---|---|---|---|
| Zaffagnini | 2011 | Italy | Ⅰ | 39 | 40 | 26 | 27 |
| Adravanti | 2016 | Italy | Ⅰ | 30 | 30 | 28.3 | 26.4 |
| Karikis | 2016 | Sweden | Ⅰ | 50 | 53 | 28 | 30 |
| Beyaz | 2017 | Turkey | Ⅰ | 16 | 15 | 31.1 | 33.5 |
| Jarvela | 2017 | Finland | Ⅱ | 30 | 30 | 30 | 34 |
| Gender (male/female) SB DB< | Minimal Follow-up (year) | Last Seen SB DB | ||
|---|---|---|---|---|
| 20/19 | 22/18 | 8 | 39 | 40 |
| 17/13 | 17/13 | 6 | 25 | 25 |
| 35/15 | 35/18 | 5 | 41 | 46 |
| 16/0 | 15/0 | 8 | 16 | 15 |
| 21/9 | 21/9 | 10 | 23 | 24 |
| Drilling technique | Fixation Tibia Femur |
Graft Type SB DB< | FITS (months) SB DB | |||
|---|---|---|---|---|---|---|
| AM | IS | IS | BPTB | HT | 8.6 | 8.9 |
| TP | IS | End | HT | HT | 4 | 4 |
| AM | IS | IS | HT | HT | 23 | 24 |
| AM | BS | End | HT | HT | 5.5 | 5.2 |
| IO | BS | BS | HT | HT | 12 | 13 |
Abbreviation: AM: Anteromedial; TP: Transportal; IO: In-outside; IS: Interference Screw; End: EndoButton; BS: Bioabsorbable Screw; BPTB: Bone-patellar tendon-bone; HT: Hamstring Tendon; TIFS: from injury to surgery.
Table 2.
Data for pooled analysis.
| Study | SB/DB | Lysholm scores | Side-to- side | IKDC scores | IKDC Grading |
Positive pivot test | OA | |
|---|---|---|---|---|---|---|---|---|
| Zaffagnini | SB | N.A | 0.4 ± 0.6 | 82 ± 20 | N.A | 1/39 | N.A | |
| DB | N.A | 1.1 ± 1.9 | 88 ± 9 | N.A | 1/40 | N.A | ||
| Adravanti | SB | 94.2 ± 15.3 | 1.3 ± 0.8 | N.A | 25/25 | N.A | 2/25 | |
| DB | 96.4 ± 17.3 | 1.4 ± 0.6 | N.A | 25/25 | N.A | 3/25 | ||
| Karikis | SB | 84.3 ± 21.2 | 2.3 ± 2.7 | N.A | N.A | 4/46 | N.A | |
| DB | 90.1 ± 9.1 | 2.2 ± 2.7 | N.A | N.A | 7/45 | N.A | ||
| Beyaz | SB | 81.94 ± 7.15 | 0.6 ± 1.9 | 71.29 ± 9.14 | N.A | N.A | N.A | |
| DB | 81.43 ± 6.45 | −0.1 ± 2 | 70.71 ± 9.44 | N.A | N.A | N.A | ||
| Jarvela | SB | 95 ± 7 | N.A | N.A | 23/23 | 0/23 | 14/23 | |
| DB | 94 ± 7 | N.A | N.A | 24/24 | 1/24 | 18/24 | ||
N.A: not applicable.
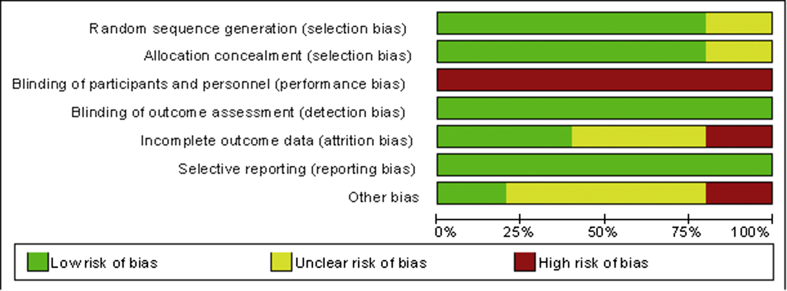
Risk of bias in included studies
The authors’ judgements about each risk of bias item for each included study were present in Fig. 2, and judgements about each risk of bias item present as percentages across all included studies were shown in Fig. 3. The percentages of performance bias were highest since none of five studies report the blinding of participants and personnel. Only one study did not clearly report the procedures of randomization and allocation concealment,11 hence an unclear risk bias was considered across this study. All studies clearly reported the blinding of outcome assessment. Only two studies clearly reported the reasons for lost follow-up. The study by Jarvela et al. had a more than 20% lost follow-up,12 which was rated as having a high risk of attribution bias. Beyaz et al. enrolled only male patients,13 which may result a high risk of potential other bias.
Fig. 2.
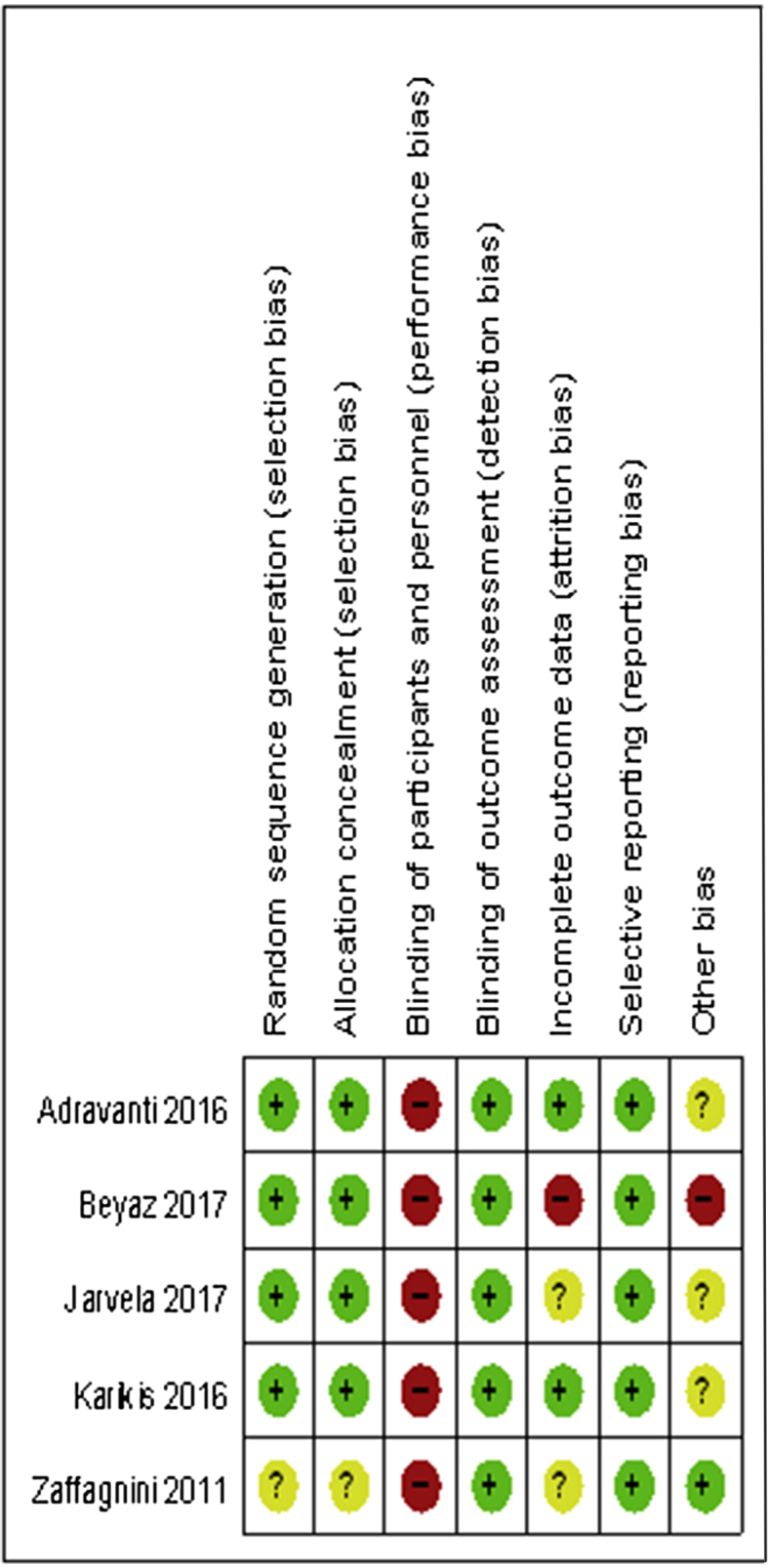
Risk of bias summary.
Fig. 3.
Risk of bias graph.
Measurement outcomes
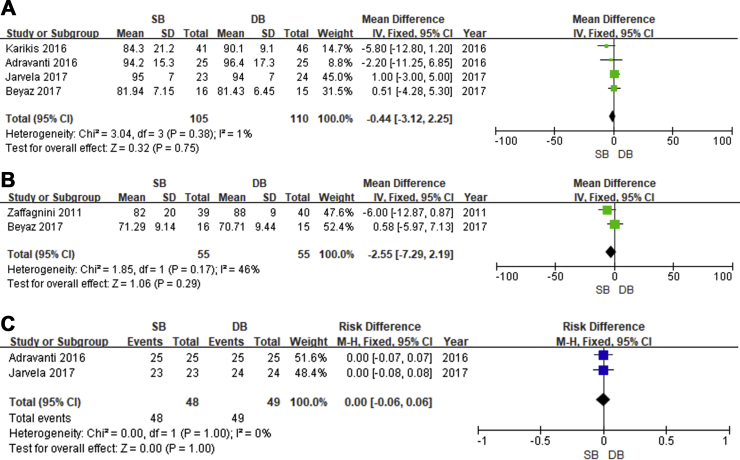
1. Lysholm scores
Four of selected studies provided eligible data for the pooled analysis of Lysholm scores. The results demonstrated than there was no significance of the Lysholm scores between SB group and DB group (P = 0.75; MD, −0.44; 95%CI −3.12, 2.25). Evidence showed low heterogeneity (P = 0.38, I2 = 1%), and no significant heterogeneity was found (Fig. 4).
2. IKDC scores
Fig. 4.
ALysholm scores. B Subjective IKDC scores. C IKDC grading.
Four studies reported eligible data for the pooled analysis of IKDC scores. Two studies provided subjective IKDC scores, and the others provided IKDC grading. Subjective IKDC scores was not significantly different between SB group and DB group (P = 0.29; MD, −2.55; 95%CI −7.29, 2.19), as well as IKDC grading (P = 1.0; RD, 0; 95%CI −0.06, 0.06). Evidence of subjective IKDC scores showed low heterogeneity (P = 0.17, I2 = 46%,Fig. 5), and evidence of IKDC grading showed no heterogeneity (P = 1.0, I2 = 0%, Fig. 4).
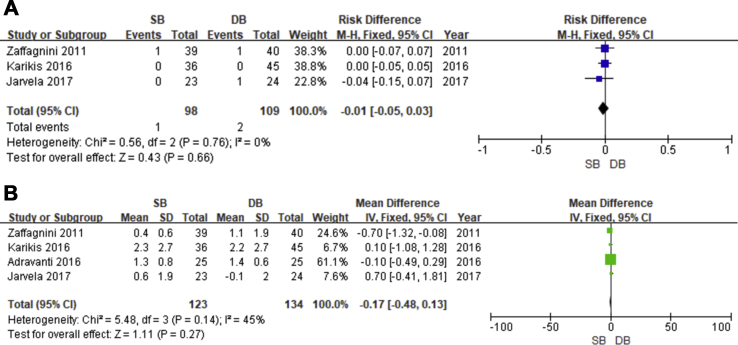
3. Pivot-shift test
Fig. 5.
Pivot-shift test.
Three studies reported the results of pivot test for pooling data at the final follow-up evaluation. The results of pooled analysis indicated no significant difference between SB group and DB group (P = 0.66; RD, −0.01; 95%CI −0.05, 0.03). There was no significant heterogeneity across these studies (P = 0.76, I2 = 0%, Fig. 4).
4. Side-to-side differences
Four studies provided the data of side-to-side differences measured by arthrometric instruments (KT-1000/2000). No significant difference was found between SB group and DB group (P = 0.27; MD, −0.17; 95%CI −0.48, 0.13). A low heterogeneity existed across the pooled analysis (P = 0.14, I2 = 45%, Fig. 5).
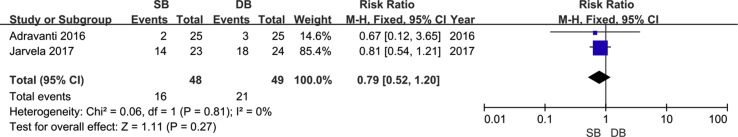
5. Osteoarthritis changes
Only two studies assessed the osteoarthritis changes according to Kellgren–Lawrence Classification at the final follow-up. The results demonstrated no significant difference between SB group and DB group (P = 0.27; RD, 0.79; 95%CI 0.52, 1.20). Evidence showed no heterogeneity (P = 0.81, I2 = 0%, Fig. 6).
Fig. 6.
OA changes.
Discussion
The most interesting findings of our meta-analysis were that there was no statistically or clinically significant difference in post-operative knee stability between SB and DB ACL reconstructions. No statistically significant difference between two techniques in Lysholm, IKDC, pivot shift, KT scores, or the development of osteoarthritis was demonstrated at a minimum of 5 years. Comparable efficiency was not beyond expectation since only one study showed the superior performance in the DB group compared to SB group.11 Low levels of evidence were prevalent in the most studies focusing on ACL reconstruction,14 and high-quality studies were relatively rare but indispensable to draw a conclusion with strong confidence level from controversies. Prospective RCTs are regarded as the optimum choice to perform a meta-analysis.13
Lysholm and subjective IKDC scores are commonly used patient-reported outcomes for evaluating patients with ACL rupture and ACL reconstruction. Lysholm et al. initiatively established the knee scoring scale in 1982 and subsequently published a revised version, which was prevalent as an important knee-specific psychometric parameter for athletic injury.16, 17 It is established that the Lysholm scores are valid as patient-administered scores and, are responsive to change at early time points of ACL reconstruction.18 However, the sensitivity of the Lysholm scoring scale was found to be low.19 There are at least eight similar meta-analyses involved with the Lysholm scores.8, 20, 21, 22, 23, 24, 25, 26, 27 Only one meta-analysis detected a significant difference between SB and DB ACL reconstruction.8 The IKDC Subjective Knee Form was originally created as a knee-specific, patient-administrated outcome measure to assess changes in symptoms, function, and sports activity in patients treated for a variety of knee injuries and conditions. The validity, reliability, and responsiveness of the IKDC Knee Form have been confirmed in the adults and adolescents.28, 29 Only one analogous study found the superiority of subjective IKDC scores in DB group compared than SB group,21 while other studies did not detect a significant difference.8, 19, 20, 23 Statistic significances of IKDC grading were found in six previous meta-analyses in favor of DB ACL reconstruction,21, 22, 24, 25, 26, 27 and Chen et al and Li et al did not detect a significant difference.8, 23 With regard to our outcomes of knee function scores, the IKDC grading deserved the primary disagreement with previous studies. It is noteworthy that these meta-analyses with controversy only include studies with short-term follow-up.
Knee stability was commonly examined by KT-1000/2000 (anteroposterior stability) and pivot test (rotary stability). The Lachman test is primarily applicable to assess the anteroposterior stability of the knee. In theory, there should not be any difference between the two techniques at least in the short term, as the strength of the double-bundle techniques is primarily the control of not anteroposterior but rotary stability.30 It is feasible to question where the superiority of DB techniques in anteroposterior stability derives. The statistical significance is unlikely to yield any clinical impact since the detected difference between SB and DB group is very small as ranged from 0.56 to 0.74 mm.24, 27 There was a trend towards a superior outcome of pivot-shift test for DB ACL reconstruction in the most of previous meta-analyses8, 21, 22, 23, 24, 25, 26, 27,while only two of them suggested that DB group and SB group could generate similar outcome regarding pivot-shift test.20, 31 This trend seems to be plausible since the posterior-lateral bundle, which is reestablished in DB technique, is considered to provide better rotational stability.32 However, only one of the four involved studies saw a better outcome of pivot-shift test for DB group.11 And further in a recent meta-analysis, Chen et al demonstrated that DB group yielded a better performance of pivot-shift than SB group in mid-term follow-up, whereas a significant difference was not detected in a subgroup analysis of relatively longer-term follow-up.8 It is noteworthy that the controversial result of residual rotational instability after ACL reconstruction is still lack of an objective evaluation.
The evidence is well established that ACL injuries deserve a contributor to the progression of osteoarthritis.33, 34 Whether ACL reconstruction could sufficiently prevent the development of osteoarthritis after ACL rupture still remains to be elucidated.35, 36 Data were pooled from three involved studies to analyze osteoarthritis after ACL reconstruction according to Kellgren–Lawrence classification,12, 37, 38 which is ranked as the most widely used instrument for the radiographic diagnosis of osteoarthritis.39 A statistically significant difference was not detected between DB and SB ACL reconstruction in this meta-analysis, as well the three involved studies.12, 37, 38 Researchers seldom investigate the changes of osteoarthritis when they are comparing the results of DB and SB techniques. Previous studies with long-term follow-up have demonstrated that the techniques of ACL reconstruction have little or no impact on the progression of osteoarthritis.40, 41, 42 Interestingly, Zhang et al. and Song et al. suggested a more effective prevention of progressive osteoarthritis for DB techniques compared with SB.43, 44 However, the short- and mid-term follow-up may be too short to detect potentially significant differences in the prevalence of osteoarthritis between the SB and DB group. Furthermore, the development of osteoarthritis is primarily influenced by the condition of concomitant chondral and meniscal damage, delayed length to surgery, and body mass index (BMI).45
To the best of our knowledge, there are at least ten meta-analyses focusing on comparing DB with SB ACL reconstruction.8, 20, 21, 22, 23, 24, 25, 26, 27, 31 Most of them reported better outcomes of knee stability for DB group compared with SB group. All studies enrolled in the present meta-analysis have a minimal longer-term follow-up than any previous meta-analyses. It should be acknowledged that DB ACL reconstruction requires longer operation time, expenditure of double fixation materials, and technical difficulty in revision. Furthermore, the DB techniques require excellent surgical skills and a longer learning curve.46 Given that the SB techniques yield similar efficacy with DB techniques in long-term follow-up and is more cost-effective,47, 48 the SB techniques may be more suitable as the standard techniques of ACL reconstruction.
There are several limitations in the meta-analysis. Mere five studies were collected, which could render outcomes to beβerror due to the small sample size. Moreover, several variables, such as grafts type, fixation methods, and anatomic or non-anatomic reconstruction, may add accidental impacts to postoperative outcomes of ACL reconstruction. Unfortunately, a subgroup analysis could not be performed due to insufficient data. The research strategy was limited to English and was only involved with three databases.
Conclusion
A review of 5 studies demonstrated that SB and DB ACL reconstructions showed no statistical differences in Lysholm and IKDC scores, pivot shift and side-to-side KT tests, and Kellgren–Lawrence osteoarthritis classification at a minimum 5 year follow up. DB techniques could not yield any better performance than SB techniques for ACL reconstruction. Given that, the relatively simple and proven techniques of SB ACL reconstruction may be preferable for orthopedic surgeons.
Acknowledgement
We declare that we have no financial and personal relationships with other people or organizations that can inappropriately influence our work, there is no professional or other personal interest of any nature or kind in any product, service and/or company that could be construed as influencing the position presented in, or the review of, the manuscript entitled.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Zhenyue Dong, Email: dongzhenyue@yeah.net.
Yingzhen Niu, Email: missniu99@163.com.
Jianchao Qi, Email: 763467725@qq.com.
Yifan Song, Email: 812547699@qq.com.
Fei Wang, Email: doctorwf@yeah.net.
References
- 1.Amis A.A., Dawkins G.P. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br. 1991;73:260–267. doi: 10.1302/0301-620X.73B2.2005151. [DOI] [PubMed] [Google Scholar]
- 2.Griffin L.Y., Agel J., Albohm M.J. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Swenson D.M., Collins C.L., Best T.M., Flanigan D.C., Fields S.K., Comstock R.D. Epidemiology of knee injuries among U.S. High school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45:462–469. doi: 10.1249/MSS.0b013e318277acca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lohmander L.S., Englund P.M., Dahl L.L., Roos E.M. The long-term consequence of anterior cruciate ligament and meniscus injuries: Osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 5.Mott H.W. Semitendinosus anatomic reconstruction for cruciate ligament insufficiency. Clin Orthop Relat Res139. 1983:90–92. [PubMed] [Google Scholar]
- 6.Kondo E., Merican A.M., Yasuda K., Amis A.A. Biomechanical comparison of anatomic double-bundle, anatomic single-bundle, and nonanatomic single-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2011;39:279–288. doi: 10.1177/0363546510392350. [DOI] [PubMed] [Google Scholar]
- 7.Mascarenhas R., Cvetanovich G.L., Sayegh E.T. Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:1185–1196. doi: 10.1016/j.arthro.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Chen G., Wang S. Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: a meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015;8:14604–14614. [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Higgins J.P., Altman D.G., Gotzsche P.C. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zaffagnini S., Bruni D., Marcheggiani Muccioli G.M. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings acl reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc. 2011;19:390–397. doi: 10.1007/s00167-010-1225-y. [DOI] [PubMed] [Google Scholar]
- 12.Jarvela S., Kiekara T., Suomalainen P., Jarvela T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 10-year results. Am J Sports Med. 2017;45:2578–2585. doi: 10.1177/0363546517712231. [DOI] [PubMed] [Google Scholar]
- 13.Beyaz S., Güler Ü.Ö., Demir Ş. Tunnel widening after single- versus double-bundle anterior cruciate ligament reconstruction: a randomized 8-year follow-up study. Arch Orthop Trauma Surg. 2017 Nov;137(11):1547–1555. doi: 10.1007/s00402-017-2774-z. [DOI] [PubMed] [Google Scholar]
- 14.Samuelsson K., Desai N., McNair E. Level of evidence in anterior cruciate ligament reconstruction research: a systematic review. Am J Sports Med. 2013;41:924–934. doi: 10.1177/0363546512460647. [DOI] [PubMed] [Google Scholar]
- 16.Lysholm J., Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 17.Tegner Y., Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 18.Briggs K.K., Lysholm J., Tegner Y., Rodkey W.G., Kocher M.S., Steadman J.R. The reliability, validity, and responsiveness of the lysholm score and tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37:890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 19.Bengtsson J., Mollborg J., Werner S. A study for testing the sensitivity and reliability of the lysholm knee scoring scale. Knee Surg Sports Traumatol Arthrosc. 1996;4:27–31. doi: 10.1007/BF01565994. [DOI] [PubMed] [Google Scholar]
- 20.Meredick R.B., Vance K.J., Appleby D., Lubowitz J.H. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36:1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 21.Xu M., Gao S., Zeng C. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29:357–365. doi: 10.1016/j.arthro.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 22.Li Y.L., Ning G.Z., Wu Q. Single-bundle or double-bundle for anterior cruciate ligament reconstruction: a meta-analysis. Knee. 2014;21:28–37. doi: 10.1016/j.knee.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Li X., Xu C.P., Song J.Q., Jiang N., Yu B. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: an up-to-date meta-analysis. Int Orthop. 2013;37:213–226. doi: 10.1007/s00264-012-1651-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Eck C.F., Kopf S., Irrgang J.J. Single-bundle versus double-bundle reconstruction for anterior cruciate ligament rupture: a meta-analysis--does anatomy matter? Arthroscopy. 2012;28:405–424. doi: 10.1016/j.arthro.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 25.Kongtharvonskul J., Attia J., Thamakaison S., Kijkunasathian C., Woratanarat P., Thakkinstian A. Clinical outcomes of double- vs single-bundle anterior cruciate ligament reconstruction: a systematic review of randomized control trials. Scand J Med Sci Sports. 2013;23:1–14. doi: 10.1111/j.1600-0838.2011.01439.x. [DOI] [PubMed] [Google Scholar]
- 26.Zhu Y., Tang R.K., Zhao P., Zhu S.S., Li Y.G., Li J.B. Double-bundle reconstruction results in superior clinical outcome than single-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1085–1096. doi: 10.1007/s00167-012-2073-8. [DOI] [PubMed] [Google Scholar]
- 27.Tiamklang T., Sumanont S., Foocharoen T., Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:Cd008413. doi: 10.1002/14651858.CD008413.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lertwanich P., Praphruetkit T., Keyurapan E., Lamsam C., Kulthanan T. Validity and reliability of Thai version of the international knee documentation committee subjective knee form. J Med Assoc Thai. 2008;91:1218–1225. [PubMed] [Google Scholar]
- 29.Irrgang J.J., Anderson A.F., Boland A.L. Responsiveness of the international knee documentation committee subjective knee form. Am J Sports Med. 2006;34:1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 30.Bjornsson H., Desai N., Musahl V. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:696–739. doi: 10.1007/s00167-013-2666-x. [DOI] [PubMed] [Google Scholar]
- 31.Desai N., Bjornsson H., Musahl V. Anatomic single- versus double-bundle acl reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22:1009–1023. doi: 10.1007/s00167-013-2811-6. [DOI] [PubMed] [Google Scholar]
- 32.Mae T., Shino K., Miyama T. Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy. 2001;17:708–716. doi: 10.1053/jars.2001.25250. [DOI] [PubMed] [Google Scholar]
- 33.Cinque M.E., Dornan G.J., Chahla J., Moatshe G., LaPrade R.F. High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med. 2018;8 doi: 10.1177/0363546517730072. 2011-2019. [DOI] [PubMed] [Google Scholar]
- 34.Ajuied A., Wong F., Smith C. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42:2242–2252. doi: 10.1177/0363546513508376. [DOI] [PubMed] [Google Scholar]
- 35.Hoffelner T., Resch H., Moroder P. No increased occurrence of osteoarthritis after anterior cruciate ligament reconstruction after isolated anterior cruciate ligament injury in athletes. Arthroscopy. 2012;28:517–525. doi: 10.1016/j.arthro.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 36.Luc B., Gribble P.A., Pietrosimone B.G. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49:806–819. doi: 10.4085/1062-6050-49.3.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karikis I., Desai N., Sernert N., Rostgard-Christensen L., Kartus J. Comparison of anatomic double- and single-bundle techniques for anterior cruciate ligament reconstruction using hamstring tendon autografts: a prospective randomized study with 5-year clinical and radiographic follow-up. Am J Sports Med. 2016;44:1225–1236. doi: 10.1177/0363546515626543. [DOI] [PubMed] [Google Scholar]
- 38.Adravanti P., Dini F., de Girolamo L., Cattani M., Rosa M.A. Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a prospective randomized controlled trial with 6-year follow-up. J Knee Surg. 2017;30:898–904. doi: 10.1055/s-0037-1598176. [DOI] [PubMed] [Google Scholar]
- 39.Kohn M.D., Sassoon A.A., Fernando N.D. Classifications in brief: Kellgren-lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474:1886–1893. doi: 10.1007/s11999-016-4732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barenius B., Ponzer S., Shalabi A., Bujak R., Norlen L., Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42:1049–1057. doi: 10.1177/0363546514526139. [DOI] [PubMed] [Google Scholar]
- 41.Holm I., Oiestad B.E., Risberg M.A., Aune A.K. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38:448–454. doi: 10.1177/0363546509350301. [DOI] [PubMed] [Google Scholar]
- 42.Oiestad B.E., Holm I., Engebretsen L., Risberg M.A. The association between radiographic knee osteoarthritis and knee symptoms, function and quality of life 10-15 years after anterior cruciate ligament reconstruction. Br J Sports Med. 2011;45:583–588. doi: 10.1136/bjsm.2010.073130. [DOI] [PubMed] [Google Scholar]
- 43.Song E.K., Seon J.K., Yim J.H., Woo S.H., Seo H.Y., Lee K.B. Progression of osteoarthritis after double- and single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:2340–2346. doi: 10.1177/0363546513498998. [DOI] [PubMed] [Google Scholar]
- 44.Zhang Z., Gu B., Zhu W., Zhu L. Double-bundle versus single-bundle anterior cruciate ligament reconstructions: a prospective, randomized study with 2-year follow-up. Eur J orthop Surg Traumatol. 2014;24:559–565. doi: 10.1007/s00590-013-1221-2. [DOI] [PubMed] [Google Scholar]
- 45.Louboutin H., Debarge R., Richou J. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16:239–244. doi: 10.1016/j.knee.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 46.Snow M., Stanish W.D. Double-bundle acl reconstruction: how big is the learning curve? Knee Surg Sports Traumatol Arthrosc. 2010;18:1195–1200. doi: 10.1007/s00167-010-1062-z. [DOI] [PubMed] [Google Scholar]
- 47.Sernert N., Hansson E. Similar cost-utility for double- and single-bundle techniques in acl reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):634–647. doi: 10.1007/s00167-017-4725-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nunez M., Sastre S., Nunez E., Lozano L., Nicodemo C., Segur J.M. Health-related quality of life and direct costs in patients with anterior cruciate ligament injury: single-bundle versus double-bundle reconstruction in a low-demand cohort--a randomized trial with 2 years of follow-up. Arthroscopy. 2012;28:929–935. doi: 10.1016/j.arthro.2011.11.034. [DOI] [PubMed] [Google Scholar]