Abstract
Background
In patients with myocardial infarction (MI), reduced kidney function is recognized as an important predictor of poor prognosis, but the impact of albuminuria, a representative measure of kidney damage, has not been extensively evaluated.
Methods and Results
In the SCREAM (Stockholm Creatinine Measurements) project (2006–2012), we identified 2469 patients with incident MI with dipstick proteinuria measured within a year before MI (427 patients also had urine albumin to creatinine ratio [ACR] measured concurrently) and obtained estimates for ACR with multiple imputation in participants with data solely on dipstick proteinuria. We quantified the association of ACR with the post‐MI composite and individual outcomes of all‐cause mortality, cardiovascular mortality, recurrent MI, ischemic stroke, or heart failure using Cox models and then evaluated the improvement in C statistic. During a median follow‐up of 1.0 year after MI, 1607 participants (65.1%) developed the post‐MI composite outcome. Higher ACR levels were independently associated with all outcomes except for ischemic stroke. Per 8‐fold higher ACR (eg, 40 versus 5 mg/g), the hazard ratio of composite outcome was 1.21 (95% CI, 1.08–1.35). The addition of the ACR improved the C statistic of the post‐MI composite by 0.040 (95% CI, 0.030–0.051). Largely similar results were obtained regardless of diabetic status and when ACR or dipstick was separately analyzed without imputation.
Conclusions
In patients with MI, albuminuria was a potent predictor of subsequent outcomes, suggesting the importance of paying attention to the information on albuminuria, in addition to kidney function, in this high‐risk population.
Keywords: albuminuria, chronic kidney disease, myocardial infarction, prognosis
Subject Categories: Cardiovascular Disease, Secondary Prevention
Clinical Perspective
What Is New?
Albuminuria, a marker of kidney damage, is associated with adverse outcomes in patients with myocardial infarction independently of kidney function.
Albuminuria improves risk prediction beyond conventional risk factors among patients with myocardial infarction.
What Are the Clinical Implications?
Our results suggest that healthcare providers should pay attention to the information on albuminuria in addition to kidney function in patients with myocardial infarction.
Since testing for albuminuria is recommended in several clinical scenarios (eg, diabetes mellitus and hypertension), data on albuminuria may be readily available for risk classification in some patients with myocardial infarction.
Introduction
Reduced kidney function has been recognized as a potent predictor of poor prognosis among patients with myocardial infarction (MI).1, 2, 3, 4, 5 Indeed, several risk prediction tools or clinical guidelines for this patient group incorporate a measure of kidney function (eg, estimated glomerular filtration rate [eGFR] based on creatinine, creatinine clearance, or blood urea nitrogen).6, 7, 8, 9, 10, 11, 12, 13, 14 On the other hand, there are limited data regarding the prognostic value of albuminuria, the other key measure of chronic kidney disease representing kidney damage, in patients with MI. Several studies explored this clinical question but have some caveats such as short‐term prognosis (eg, 1‐month or in‐hospital mortality),15, 16 only mortality outcomes, small sample size (<500 participants),15, 17, 18, 19, 20, 21, 22 and selected study populations from clinical trials.23, 24 Also, only a few studies formally tested risk prediction improvement by adding albuminuria among patients with MI.15, 18, 19, 24 These are important caveats since the current international clinical guideline emphasizes characterizing chronic kidney disease according to both eGFR and albuminuria.25 Therefore, we quantified the association of albuminuria with fatal and nonfatal cardiovascular outcomes in patients with MI from a Swedish population‐based cohort and evaluated risk prediction improvement by adding albuminuria to conventional predictors.
Methods
Study materials are available to other researchers for collaborative projects. Requests should be sent to the SCREAM (Stockholm Creatinine Measurements) steering committee group (contact: juan.jesus.carrero@ki.se).
Study Population
The SCREAM project is a repository of laboratory data of individuals accessing health care in the region of Stockholm. SCREAM includes 1 118 507 Stockholm citizens older than 18 years who had serum creatinine measured at least once between 2006 and 2012.26 In SCREAM, we identified 23 674 individuals who developed MI during follow‐up based on International Classification of Disease, Tenth Revision (ICD‐10) diagnostic codes (I21). Of these patients with MI, 21 303 had information on serum creatinine within a year before hospitalized MI. Of these individuals, 2469 patients had data on dipstick proteinuria within a year before the index MI (427 patients also had data on urine albumin to creatinine ratio [ACR]). An additional 724 patients had data only on ACR in this time frame. As anticipated, most patients with only data on ACR had diabetes mellitus (72.2%), although the prevalence of diabetes mellitus in all index MI cases was 22.0% (Table S1). In contrast, patients with dipstick proteinuria data had much closer characteristics (eg, the prevalence of diabetes mellitus was 32.0%) to the overall patients with index MI. To obtain inferences for ACR (the albuminuria measure recommended in clinical guidelines25) not restricted to patients with diabetes mellitus, we primarily analyzed 2469 patients with data on dipstick proteinuria within a year before index MI, and obtained 2042 estimates for ACR with multiple imputation (83%), as subsequently detailed (Figure S1). As secondary analysis, we analyzed dipstick proteinuria data in 2469 patients and ACR data in 1151 patients without multiple imputation. The regional institutional review board and the Swedish National Board of Welfare approved the study for use of deidentified data. The study complies with the Declaration of Helsinki and was performed in accordance with the local legislation.
Albuminuria
We used ACR and dipstick data clinically measured in SCREAM.27, 28 Urine creatinine measurement was standardized to isotope dilution mass spectrometry standards. Dipstick proteinuria was assessed by an automated urine analyzer and was recorded as <30, 30 to 100, 101 to 300, and >300 mg/dL.
Covariates
We considered predictors included in the Thrombolysis In Myocardial Infarction Risk Score for Secondary Prevention (TRS2°P) for recent patients with MI as conventional predictors and adjusted for them.12 Specifically, TRS2°P included 9 factors of age, heart failure, hypertension, diabetes mellitus, stroke, coronary artery bypass graft, peripheral artery disease, eGFR, and smoking status.29 However, since our study did not have information on smoking status, we used the remaining 8 predictors as covariates. A history of clinical conditions in TRS2°P was based on ICD‐10 diagnostic codes and Nordic Medico‐Statistical Committee classification (Table S2). eGFR was based on the creatinine‐based Chronic Kidney Disease Epidemiology Collaboration equation.
Based on the presence and absence of those clinical diagnoses as well as age 75 years and older and eGFR <60 mL/min per 1.73 m2, we calculated TRS2°P ranging from 0 to 8. A TRS2°P of 0, 1 to 2, and ≥3 was defined as low, intermediate, and high risk, respectively.12 Information on drug dispensation was derived from the Swedish Dispensed Drug registry (Table S2). We considered any dispensation of aspirin, thienopyridine, ß‐blockers, angiotensin‐converting enzyme inhibitors, angiotensin II receptor blockers, and statins within 6 months before index MI or within 14 days after discharge date of index MI to be active use of these drugs at index MI.
Outcomes
The adverse health outcomes of interest were all‐cause mortality, cardiovascular mortality, recurrent MI, ischemic stroke, and heart failure. We considered a composite of those outcomes as the primary outcome but secondarily evaluated each outcome individually. All‐cause mortality and cardiovascular mortality were determined by linkage to vital status in the Swedish Population Registry. Cardiovascular mortality included deaths with MI, heart failure, stroke, or sudden cardiac death as the primary cause of death. We identified recurrent MI based on ICD‐10 codes I22 (subsequent ST‐segment elevation and non–ST‐segment–elevation MI within 4 weeks of a previous MI) within 28 days and I21 (ST‐segment elevation and non–ST‐segment–elevation MI) after 28 days after index MI, ischemic stroke based on I63 (cerebral infarction), and heart failure based on I50 (heart failure). The follow‐up period was from index MI until December 31, 2012, and participants were censored at the end of follow‐up (or death not related to an individual outcome of interest [eg, noncardiovascular mortality for the analysis of cardiovascular mortality]).
Statistical Analysis
To assess albuminuria as a continuous variable, we obtained estimates for log‐transformed ACR with multiple imputation in participants with data solely on dipstick proteinuria based on multivariate imputation using chained equation using age, heart failure, hypertension, diabetes mellitus, stroke, coronary artery bypass graft, peripheral artery disease, eGFR, dipstick proteinuria, composite outcome, and follow‐up time for 20 cycles.30 Descriptive statistics are presented as mean and SD for continuous variables or percentage for categorical variables across 4 categories of measured or average imputed values of ACR (<10, 10–29, 30–299, and ≥300 mg/g). Subsequently, we quantified the association of log‐ACR with adverse outcomes after adjusting for TRS2°P predictors using Cox proportional hazards models. To visualize the shape of association with composite and individual adverse outcomes, log‐ACR was modeled with its linear spline terms and 3 knots at 10, 30, and 300 mg/g (5 mg/g as a reference).31, 32
We conducted several sensitivity analyses to evaluate the robustness of our findings. First, we assessed potential interactions by diabetes mellitus. Statistical interaction between ACR and diabetes mellitus was assessed by a likelihood ratio test comparing models with and without their product terms. Also, to avoid the possible confounding by medications, we further adjusted for aspirin, thienopyridine, ß‐blockers, angiotensin‐converting enzyme inhibitors, angiotensin II receptor blockers, and statins. Third, to consider MI severity, we repeated the main analysis after excluding those who died within 14 days after MI.
To assess the predictive value of ACR beyond conventional predictors, we first estimated 1‐year cumulative incidence of composite outcome according to ACR ≥30 mg/g versus <30 mg/g within low, intermediate, and high risk categories determined by TRS2°P as noted above. To formally assess whether the addition of ACR to conventional predictors improves risk prediction of adverse outcomes, we estimated the difference in Harrell's C statistics33 and categorical net reclassification improvement (NRI)34 for 1‐year risk of adverse outcomes by contrasting 2 models incorporating predictors in TRS2°P with ACR versus without ACR. Based on the cumulative incidence of the composite adverse outcome in our data, 1‐year risks of 20% and 40%, roughly corresponding to average 1‐year risk in low‐ to intermediate‐risk and intermediate‐ to high‐risk categories, were used as thresholds for categorical NRI. For individual outcomes, we restricted the analysis of categorical NRI to major individual outcomes in this study, namely all‐cause mortality, cardiovascular mortality, and heart failure, and applied a half of the aforementioned thresholds, namely 1‐year risk of 10% and 20%. In addition, to evaluate calibration, we plotted predicted and observed risk based on decile of 1‐year risk and calculated a modified Hosmer‐Lemeshow chi‐square statistic.33 Observed risk was estimated using the Kaplan–Meier method based on coefficients from multiple imputation Cox models and average imputed values of ACR in relevant patients.35
Finally, we repeated our analyses described above in our primary study population based on data of dipstick proteinuria without multiple imputation. We used dipstick proteinuria categories (<30, 30–100, 100–300, and >300 mg/dL), with <30 mg/dL as a reference. Similarly, we repeated the analysis among 1151 participants with measured ACR data within a year before MI, without multiple imputation. All analyses were performed using Stata statistical software version 14 (StataCorp). All statistical tests were 2‐sided and statistical significance was determined as P<0.05.
Results
Participants' Characteristics
Among 2469 patients with MI and an available measure of proteinuria, the mean age of the study participants was 65 years (SD, 12 years), and 53% were men. The mean eGFR was 61 mL/min per 1.73 m2, and the prevalence of positive dipstick proteinuria (30–100, 101–300, and ≥300 mg/dL) was 32%. The baseline characteristics of our study population by ACR levels are shown in Table 1. Compared with those with lower ACR levels, individuals with higher ACR levels were more likely to be older, male, and have comorbidities (heart failure, hypertension, diabetes mellitus, stroke, coronary artery bypass graft, and peripheral artery disease). As anticipated, they were also more likely to have lower eGFR and higher dipstick proteinuria. Regarding cardiovascular medications, patients with higher ACR values were less likely to receive antiplatelets (aspirin and thienopyridine) and statins but were more likely to take angiotensin‐converting enzyme inhibitors or angiotensin II receptor blockers. No clear patterns were recognized for β‐blockers across ACR categories.
Table 1.
Baseline Characteristics by Urine ACRa Categories (N=2469)
| ACR, mg/g | ||||
|---|---|---|---|---|
| <10 (n=302) | 10 to 29 (n=1033) | 30 to 299 (n=873) | ≥300 (n=261) | |
| Demographic | ||||
| Age, y | 59.0 (12.8) | 64.7 (12.1) | 68.1 (10.8) | 64.2 (11.3) |
| Men, % | 56.3 | 47.8 | 55.6 | 64.8 |
| Comorbidities, % | ||||
| Heart failure | 18.9 | 30.2 | 41.6 | 52.5 |
| Hypertension | 31.5 | 64.4 | 75.8 | 85.8 |
| Diabetes mellitus | 20.9 | 26.0 | 37.0 | 51.7 |
| Prior stroke | 4.3 | 10.7 | 17.2 | 19.9 |
| Coronary artery bypass graft | 1.0 | 2.2 | 4.4 | 5.4 |
| Peripheral artery disease | 2.3 | 4.7 | 19.4 | 23.0 |
| Kidney measures | ||||
| eGFR, mL/min per 1.73 m2 | 85.6 (19.8) | 75.4 (23.3) | 54.9 (26.6) | 35.8 (25.8) |
| eGFR <60 mL/min per 1.73 m2, % | 7.6 | 23.7 | 62.3 | 85.8 |
| Dipstick proteinuria, mg/dL, % | ||||
| <30 | 97.0 | 95.3 | 44.7 | 2.3 |
| 30 to 100 | 2.0 | 4.2 | 35.7 | 3.8 |
| 101 to 300 | 1.0 | 0.5 | 18.7 | 36.8 |
| >300 | 0.0 | 0.1 | 0.9 | 57.1 |
| ACR | 7.6 (1.8) | 18.1 (5.5) | 87.5 (65.5) | 1636.6 (1879.9) |
| Medication useb | ||||
| Aspirin | 85.8 | 79.7 | 75.6 | 77.4 |
| Thienopyridine | 62.3 | 50.9 | 40.9 | 37.6 |
| ß‐Blocker | 80.8 | 80.0 | 74.9 | 81.2 |
| ACEI or ARB | 58.9 | 65.2 | 65.5 | 71.7 |
| Statin | 75.5 | 64.3 | 54.8 | 56.7 |
Values for categorical variables are given as percentages and values for continuous variables are given as means (SDs). ACEI indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; eGFR, estimated glomerular filtration rate.
Average of imputed values for patients without measured albumin to creatinine ratio (ACR).
Within 6 months before index myocardial infarction or within 14 days after discharge date of index myocardial infarction.
Albuminuria and Adverse Outcomes After Index MI
Over a maximum follow‐up of 8 years (median follow‐up of 1.0 [interquartile interval, 0.1–3.1] years), 1607 participants with index MI developed at least 1 of the outcomes of interest (1223 all‐cause deaths including 569 cardiovascular deaths, 794 heart failure cases, 396 recurrent MI cases, and 168 ischemic stroke cases). The adjusted hazard ratio of adverse outcomes after incident MI increased largely linearly along with higher levels of log‐ACR (Figure 1). As compared with the reference ACR of 5 mg/g, adjusted hazard ratio exceeded 1.5 at an ACR level of 30.4 mg/g. The adjusted hazard ratio at ACR 400 mg/g in the range of severe albuminuria was 1.77 (95% CI, 1.49–2.09).
Figure 1.
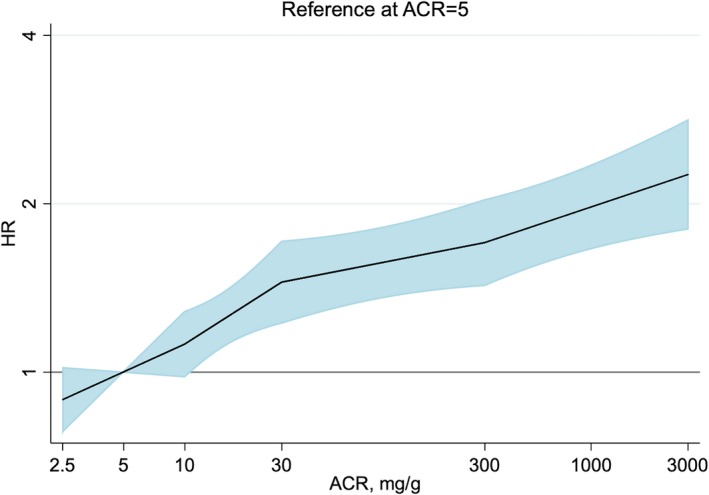
Adjusted hazard ratios of composite outcome after index myocardial infarction by linear splines of urine albumin to creatinine ratio (ACR) with 3 knots (10, 30, and 300 mg/g) in each imputation data set (N=2469).
Given this largely linear relationship, we modeled log‐ACR as a linear term for subsequent analyses. Per 8‐fold increment in ACR, the hazard ratio was 1.21 (95% CI, 1.08–1.35) for the primary composite outcome (Table 2, second left column). When we examined individual outcomes separately, a higher level of ACR was similarly associated with all outcomes, although the association with ischemic stroke did not reach statistical significance. The associations were largely the same after further adjusting for medication use (Table 2, second right column) or excluding patients who died within 14 days after MI (Table 2, right column). There was no evidence of effect modification by diabetes mellitus (Table S3).
Table 2.
Adjusted HRs (95% CIs) of Adverse Outcomes After Index MI by Continuous Urine ACR (N=2469)
| 8‐Fold ACR | Additionally Adjusting for Medicationsb | After Excluding Patients Who Died Within 14 Daysa | |
|---|---|---|---|
| Primary Analysisa | |||
| Composite outcomec | 1.21 (1.08–1.35) | 1.20 (1.08–1.34) | 1.26 (1.14–1.39) |
| All‐cause mortality | 1.22 (1.10–1.34) | 1.19 (1.08–1.31) | 1.29 (1.17–1.43) |
| Cardiovascular mortality | 1.21 (1.05–1.39) | 1.18 (1.02–1.36) | 1.35 (1.16–1.56) |
| Heart failure | 1.21 (1.06–1.38) | 1.22 (1.07–1.39) | 1.19 (1.05–1.36) |
| Recurrent MI | 1.23 (1.05–1.44) | 1.22 (1.05–1.43) | 1.24 (1.05–1.46) |
| Ischemic stroke | 1.19 (0.96–1.48) | 1.17 (0.94–1.45) | 1.17 (0.92–1.49) |
ACR indicates albumin to creatinine ratio; HR, hazard ratio.
Adjusted for age (continuous), heart failure, hypertension, diabetes mellitus, stroke, coronary artery bypass graft, peripheral artery disease, and estimated glomerular filtration rate (continuous).
Additionally adjusted for aspirin, thienopyridine, ß‐Blocker, angiotensin‐converting enzyme inhibitor or angiotensin II receptor blocker, and statin.
All‐cause mortality, cardiovascular mortality, heart failure, recurrent myocardial infarction (MI), or ischemic stroke.
Risk Classification and Prediction With ACR
In each category of low, intermediate, and high risk based on conventional risk factors, the 1‐year cumulative incidence of adverse outcomes was higher in patients with an ACR ≥30 mg/g than those with an ACR <30 mg/g, with particularly evident differences in the low‐ and intermediate‐risk categories (Figure 2). Patients with low risk and an ACR ≥30 mg/g had a higher risk than those with intermediate risk and an ACR <30 mg/g.
Figure 2.
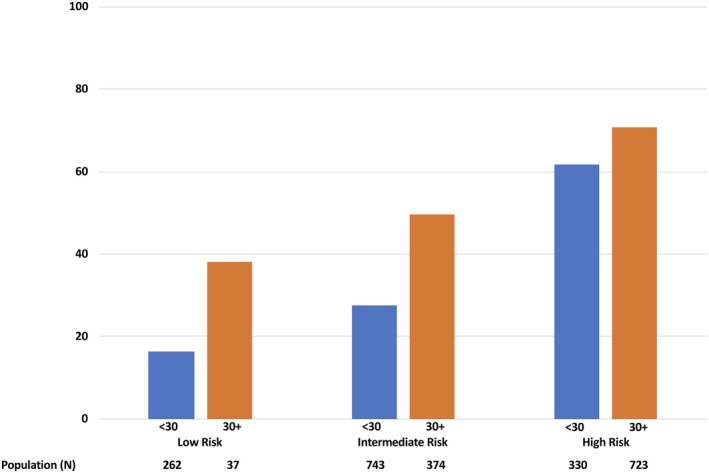
One‐year cumulative incidence (percentage) of the composite outcome after index myocardial infarction by predicted risk categories based on Thrombolysis In Myocardial Infarction Risk Score for Secondary Prevention and urine albumin to creatinine ratio categories.
The C statistic for the composite outcome based on TRS2°P predictors was 0.664 in our study. The addition of ACR significantly improved C statistic by 0.040 (95% CI, 0.030–0.051) to 0.705 (95% CI, 0.690–0.719) (Table 3). Similar results were seen for all individual outcomes except ischemic stroke. The C statistic for recurrent MI improved the most, by 0.084 (95% CI, 0.058–0.011) to 0.649 (95% CI, 0.615–0.683).
Table 3.
Prediction Statistics With the Addition of Urine ACR to Conventional Risk Factors
| C Statistic (95% CI) | Δ C Statistic (95% CI) | NRI, Categorical (95% CI)a | |
|---|---|---|---|
| Composite outcomeb | |||
| Conventional risk factors | 0.664 (0.649–0.680) | ||
| +ACR | 0.705 (0.690–0.719) | 0.040 (0.030–0.051) | 0.027 (0.010–0.044) |
| All‐cause mortality | |||
| Conventional risk factors | 0.694 (0.675–0.713) | ||
| +ACR | 0.725 (0.707–0.743) | 0.031 (0.023–0.039) | 0.023 (0.002–0.043) |
| Cardiovascular mortality | |||
| Conventional risk factors | 0.721 (0.700–0.744) | ||
| +ACR | 0.744 (0.722–0.767) | 0.023 (0.017–0.030) | 0.026 (−0.003 to 0.056) |
| Heart failure | |||
| Conventional risk factors | 0.701 (0.680–0.721) | ||
| +ACR | 0.734 (0.714–0.754) | 0.033 (0.020–0.047) | 0.012 (−0.010 to 0.034) |
| Recurrent MI | |||
| Conventional risk factors | 0.565 (0.530–0.600) | ||
| +ACR | 0.649 (0.615–0.683) | 0.084 (0.058–0.011) | ··· |
| Ischemic stroke | |||
| Conventional risk factors | 0.780 (0.736–0.824) | ||
| +ACR | 0.783 (0.740–0.826) | 0.003 (−0.002 to 0.008) | ··· |
ACR indicates albumin to creatinine ratio. All prediction statistics were based on 1‐year predicted risk. Conventional risk factors were age (continuous), heart failure, hypertension, diabetes mellitus, stroke, coronary artery bypass graft, peripheral artery disease, and estimated glomerular filtration rate (continuous). For individual outcomes, we restricted the analysis of categorical net reclassification improvement (NRI) to major individual outcomes, all‐cause mortality, cardiovascular mortality, and heart failure, because of a small number of events.
For composite outcome, the 1‐year risk of 20% and 40% were used as thresholds for categorical NRI. For individual outcomes, the 1‐year risk of 10% and 20% (a half of those thresholds) were used as thresholds for categorical NRI.
All‐cause mortality, cardiovascular mortality, heart failure, recurrent myocardial infarction (MI), or ischemic stroke.
The categorical NRI was positive for all outcomes tested, although statistical significance was seen only for the primary composite outcome and all‐cause mortality (Table 3). Regarding calibration, although some overestimation for all‐cause mortality and cardiovascular mortality were shown in a few top deciles, the calibration for composite outcome was reasonably good (Figure S2). When we excluded patients with MI who died within 14 days after MI, we observed similar improvement in C statistics and significantly positive categorical NRI for the composite outcome, all‐cause mortality, and cardiovascular mortality (Table S4).
Analysis Without Multiple Imputation
When we investigated data on dipstick proteinuria in the study population of 2469 patients without multiple imputation, in general, higher levels of dipstick proteinuria were similarly associated with adverse outcomes after MI (Table S5), with a dose‐response relationship seen in some, but not all, outcomes. For risk prediction, when we added dipstick proteinuria to conventional risk factors, although categorical NRI was not statistically positive, we observed significant improvement in C statistics for composite outcome, all‐cause and cardiovascular mortality, heart failure, and recurrent MI (Table S6).
When we analyzed 1151 patients with MI and measured ACR data within a year before MI without multiple imputation, we observed a dose‐response relationship between ACR and outcomes similar to the main analysis (Figure S3 and Tables S7 and S8). For risk prediction, the addition of ACR did not significantly improve C statistic from the model with conventional risk factors, whereas it significantly improved categorical NRI for composite outcome and heart failure (Table S9). We also converted dipstick proteinuria into ACR values based on a median ACR value of each dipstick proteinuria category in a previous study36 and confirmed a similar association between ACR and composite outcome after incident MI (Figure S4).
Discussion
Among patients with MI from a healthcare utilization cohort, we found that albuminuria was independently and potently associated with subsequent adverse outcomes including all‐cause mortality, cardiovascular mortality, heart failure, and recurrent MI. For example, compared with ACR 5 mg/g, ACR ≈30 mg/g (the threshold between normal and elevated albuminuria) conferred 50% higher risk of adverse outcomes in this high‐risk clinical population. The associations were largely consistent regardless of the presence versus the absence of diabetes mellitus and use of cardiovascular medications. We also confirmed that ACR significantly improved risk discrimination and classification of post‐MI adverse outcomes beyond conventional predictors, including eGFR. The reclassification appeared to be particularly evident when conventional predictors indicated low or intermediate risk (Figure 2). Although our main analysis implemented multiple imputation of ACR using data on dipstick proteinuria and other variables, we confirmed similar patterns in dipstick proteinuria and ACR without multiple imputation.
Several studies have investigated the association of albuminuria with adverse outcomes among patients with MI,15, 16, 17, 18, 19, 20, 21, 22 and a few showed improvement of risk prediction beyond known risk factors, including kidney function (eg, serum creatinine).15, 18, 19 However, as mentioned above, most previous studies had small sample sizes,15, 17, 18, 19, 20, 21, 22 followed up patients for relatively short periods, or focused on fatal outcomes.15, 16, 17, 18, 19, 20, 21 One study explored fatal and nonfatal outcomes (all‐cause mortality, MI, stroke, and heart failure) in >3000 patients with acute coronary syndrome (≈70% for MI and ≈30% unstable angina) over a median follow‐up of 2 years.23 However, in contrast to our study, this study showed that urine albumin concentration >300 μg/mL was only an independent predictor of all‐cause mortality. The difference with results from our study may be the result of study population characteristics since this previous study was based on data from a randomized clinical trial among selected patients for statin therapy versus placebo. Importantly, our study uniquely observed that albuminuria was an important predictor for prognosis after MI when adding to proposed stratification tools12 and improved risk prediction of major post‐MI fatal and nonfatal outcomes.
Since albuminuria has been shown to predict cardiovascular events in various settings,32, 37 our results in patients with MI may not be surprising. Although mechanisms linking albuminuria to poor prognosis in patients with MI are yet to be elucidated, albuminuria has been suggested to be an indicator of microvascular damage and endothelial dysfunction,38, 39 and these pathophysiological conditions are considered to play key roles in the development of atherosclerotic disease and heart failure.40
Our results have several clinical implications. While the recent international clinical guidelines of chronic kidney disease recommend25 that healthcare providers pay attention to the information on albuminuria in addition to eGFR, our results suggest that this recommendation should be applied to patients with recent MI as well. Although risk‐centered management is not yet widely recommended in patients with MI other than for the selection of urgent revascularization in non–ST‐segment–elevation MI,41 some investigators suggest the potential usefulness of this approach for intensive antiplatelet therapy.12 Also, the need for risk prediction in patients with MI has grown as novel, effective but expensive drugs such as PCSK9 inhibitors are developed for patients with MI.42 In this context, our results suggest the potential value of taking into account data on albuminuria. Importantly, testing for albuminuria is recommended in several clinical scenarios such as in patients with diabetes mellitus and hypertension,43, 44 and thus data on albuminuria may be readily available in some patients with MI (eg, 61% of all patients with MI in SCREAM had either diabetes mellitus or hypertension). Furthermore, to our knowledge, there are no established prediction tools including albuminuria for patients after MI. Therefore, it would be reasonable to develop prediction tools with albuminuria for a risk‐centered management of patients with MI.
Study Limitations
Our study has several limitations. First, because information on ACR was lacking in most patients with MI and we aimed to obtain most generalizable estimates for ACR, we applied multiple imputation in our primary analysis. Although multiple imputation can provide unbiased and valid results in general,45, 46 multiple imputation in the majority of participants can be concerning. Nonetheless, we confirmed similar results using data without multiple imputation. Second, although the use of a study population with dipstick data was to investigate relatively representative patients with MI in SCREAM, we recognize that patients with dipstick data did not fully represent the source patient population (eg, higher prevalence of diabetes mellitus). Third, the discrimination capacity in our study was not excellent (C statistic <0.7), but this is largely comparable to the C statistics shown for prediction tools for patients with MI such as TRS2°P.12, 41 Finally, the possibility of residual confounding was not avoidable. For example, as noted above, data on smoking, a predictor of TRS2°P, were lacking.
Conclusions
Albuminuria is an independent and a potent predictor of adverse outcomes among patients with MI. Indeed, albuminuria improves risk prediction among patients with MI beyond conventional predictors, including eGFR. Particularly since the measurement of albuminuria is recommended in diabetes mellitus and hypertension and most patients with MI have at least 1 of these conditions, our results reinforce the importance of considering albuminuria, in addition to eGFR, for risk classification among patients with MI.
Sources of Funding
The SCREAM project has obtained financial support from the Stockholm County Council, the regional agreement on medical training and clinical research between the Stockholm County Council and Karolinska Institutet, the Swedish Medical Research Council (Vetenskapsrådet), Martin Rind's, and Westman's Foundations.
Disclosures
None.
Supporting information
Table S1. Baseline Characteristics by Sample
Table S2. Definition of Covariates
Table S3. Adjusted HRs (95% CIs)* of Adverse Outcomes After Index MI by Continuous ACR and Diabetes Mellitus Status
Table S4. Model Performance Measures With the Addition of ACR to TRS2°P Variables After Excluding Patients Who Died Within 14 Days After Hospitalization for MI
Table S5. Crude Incidence Rate (Per 100 Person‐Years) and Adjusted HRs (95% CIs)* of Adverse Outcomes After Index MI by Dipstick Proteinuria (N=2469)
Table S6. Model Performance Measures With the Addition of Dipstick Proteinuria to Conventional Risk Factors
Table S7. Adjusted HRs (95% CIs)* of Adverse Outcomes After Index MI by Continuous Urine ACR Among Patients With ACR Data (N=1151)
Table S8. Crude Incidence Rate (100 Person‐Years) and Adjusted HRs (95% CIs)* of Adverse Outcome After Index MI by Urine ACR Among Patients With ACR Data (N=1151)
Table S9. Model Performance Measures With the Addition of ACR to Conventional Risk Factors Among Patients With ACR Data (N=1151)
Figure S1. Study population.
Figure S2. One‐year probability of adverse outcomes by decile of 1‐year risk with the addition of urine albumin to creatinine ratio (ACR) to conventional risk factors.
Figure S3. Adjusted hazard ratios (HRs) of composite outcome after index myocardial infarction (MI) by linear splines of urine albumin to creatinine ratio (ACR) with 3 knots (10, 30, and 300 mg/g) in patients with ACR data.
Figure S4. Adjusted hazard ratios (HRs) of composite outcome after index myocardial infarction (MI) by linear splines of converted urine albumin to creatinine ratio (ACR) with 3 knots (10, 30, and 300 mg/g).
(J Am Heart Assoc. 2019;8:e010546 DOI: 10.1161/JAHA.118.010546.)
Preliminary results of this work were presented at the American Heart Association Scientific Sessions, November 11 to 15, 2017, in Anaheim, CA.
References
- 1. Al Suwaidi J, Reddan DN, Williams K, Pieper KS, Harrington RA, Califf RM, Granger CB, Ohman EM, Holmes DR Jr; GUSTO‐IIb, GUSTO‐III, PURSUIT. Global Use of Strategies to Open Occluded Coronary Arteries. Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy; PARAGON‐A Investigators. Platelet IIb/IIIa Antagonism for the Reduction of Acute coronary syndrome events in a Global Organization Network . Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation. 2002;106:974–980. [DOI] [PubMed] [Google Scholar]
- 2. Santopinto JJ, Fox KA, Goldberg RJ, Budaj A, Pinero G, Avezum A, Gulba D, Esteban J, Gore JM, Johnson J, Gurfinkel EP; GRACE Investigators . Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the global registry of acute coronary events (GRACE). Heart. 2003;89:1003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fox KA, Antman EM, Montalescot G, Agewall S, SomaRaju B, Verheugt FW, Lopez‐Sendon J, Hod H, Murphy SA, Braunwald E. The impact of renal dysfunction on outcomes in the ExTRACT‐TIMI 25 trial. J Am Coll Cardiol. 2007;49:2249–2255. [DOI] [PubMed] [Google Scholar]
- 4. Shiraishi J, Kohno Y, Nakamura T, Yanagiuchi T, Hashimoto S, Ito D, Kimura M, Matsui A, Yokoi H, Arihara M, Hyogo M, Shima T, Sawada T, Matoba S, Yamada H, Matsumuro A, Shirayama T, Kitamura M, Furukawa K; AMI‐Kyoto Multi‐Center Risk Study Group . Prognostic impact of chronic kidney disease and anemia at admission on in‐hospital outcomes after primary percutaneous coronary intervention for acute myocardial infarction. Int Heart J. 2014;55:301–306. [DOI] [PubMed] [Google Scholar]
- 5. Lau JK, Anastasius MO, Hyun KK, Dabin B, Coverdale S, Ferry C, Hung J, Antonis P, Chew DP, Aliprandi‐Costa B, Cass A, Brieger DB. Evidence‐based care in a population with chronic kidney disease and acute coronary syndrome. Findings from the Australian Cooperative National Registry of Acute Coronary Care, Guideline Adherence and Clinical Events (CONCORDANCE). Am Heart J. 2015;170:566–572.e1. [DOI] [PubMed] [Google Scholar]
- 6. Normand ST, Glickman ME, Sharma RG, McNeil BJ. Using admission characteristics to predict short‐term mortality from myocardial infarction in elderly patients. Results from the Cooperative Cardiovascular Project. JAMA. 1996;275:1322–1328. [PubMed] [Google Scholar]
- 7. Jacobs DR Jr, Kroenke C, Crow R, Deshpande M, Gu DF, Gatewood L, Blackburn H. PREDICT: a simple risk score for clinical severity and long‐term prognosis after hospitalization for acute myocardial infarction or unstable angina: the Minnesota heart survey. Circulation. 1999;100:599–607. [DOI] [PubMed] [Google Scholar]
- 8. Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG, Flather MD, Fox KA; Global Registry of Acute Coronary Events Investigators . Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. [DOI] [PubMed] [Google Scholar]
- 9. Halkin A, Singh M, Nikolsky E, Grines CL, Tcheng JE, Garcia E, Cox DA, Turco M, Stuckey TD, Na Y, Lansky AJ, Gersh BJ, O'Neill WW, Mehran R, Stone GW. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. J Am Coll Cardiol. 2005;45:1397–1405. [DOI] [PubMed] [Google Scholar]
- 10. Lee JH, Park HS, Chae SC, Cho Y, Yang DH, Jeong MH, Kim YJ, Kim KS, Hur SH, Seong IW, Hong TJ, Cho MC, Kim CJ, Jun JE, Park WH; Korea Acute Myocardial Infarction Registry Investigators . Predictors of six‐month major adverse cardiac events in 30‐day survivors after acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry). Am J Cardiol. 2009;104:182–189. [DOI] [PubMed] [Google Scholar]
- 11. Kim HK, Jeong MH, Ahn Y, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, Cho MC, Kim CJ, Seung KB, Chung WS, Jang YS, Rha SW, Bae JH, Cho JG, Park SJ; other Korea Acute Myocardial Infarction Registry Investigators and Korea Acute Myocardial infarction Registry (KAMIR) Study Group of Korean Circulation Society . A new risk score system for the assessment of clinical outcomes in patients with non‐ST‐segment elevation myocardial infarction. Int J Cardiol. 2010;145:450–454. [DOI] [PubMed] [Google Scholar]
- 12. Bohula EA, Bonaca MP, Braunwald E, Aylward PE, Corbalan R, De Ferrari GM, He P, Lewis BS, Merlini PA, Murphy SA, Sabatine MS, Scirica BM, Morrow DA. Atherothrombotic risk stratification and the efficacy and safety of vorapaxar in patients with stable ischemic heart disease and previous myocardial infarction. Circulation. 2016;134:304–313. [DOI] [PubMed] [Google Scholar]
- 13. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli‐Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P; ESC Scientific Document Group . 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. [DOI] [PubMed] [Google Scholar]
- 14. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines . 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–e425. [DOI] [PubMed] [Google Scholar]
- 15. Schiele F, Meneveau N, Chopard R, Descotes‐Genon V, Oettinger J, Seronde MF, Briand F, Bernard Y, Ecarnot F, Bassand JP; Reseau de Cardiologie de Franche C . Prognostic value of albuminuria on 1‐month mortality in acute myocardial infarction. Am Heart J. 2009;157:327–333. [DOI] [PubMed] [Google Scholar]
- 16. Lekatsas I, Koulouris S, Triantafyllou K, Chrisanthopoulou G, Moutsatsou‐Ladikou P, Ioannidis G, Thalassinos N, Kalofoutis A, Anthopoulos L. Prognostic significance of microalbuminuria in non‐diabetic patients with acute myocardial infarction. Int J Cardiol. 2006;106:218–223. [DOI] [PubMed] [Google Scholar]
- 17. Berton G, Cordiano R, Palmieri R, Cucchini F, De Toni R, Palatini P. Microalbuminuria during acute myocardial infarction; a strong predictor for 1‐year mortality. Eur Heart J. 2001;22:1466–1475. [DOI] [PubMed] [Google Scholar]
- 18. Berton G, Cordiano R, Mazzuco S, Katz E, De Toni R, Palatini P. Albumin excretion in acute myocardial infarction: a guide for long‐term prognosis. Am Heart J. 2008;156:760–768. [DOI] [PubMed] [Google Scholar]
- 19. Berton G, Cordiano R, Palmieri R, Cavuto F, Buttazzi P, Palatini P. Comparison of C‐reactive protein and albumin excretion as prognostic markers for 10‐year mortality after myocardial infarction. Clin Cardiol. 2010;33:508–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Taskiran M, Iversen A, Klausen K, Jensen GB, Jensen JS. The association of microalbuminuria with mortality in patients with acute myocardial infarction. A ten‐year follow‐up study. Heart Int. 2010;5:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen JW, Wang YL, Li HW. Elevated admission microalbuminuria predicts poor myocardial blood flow and 6‐month mortality in ST‐segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. Clin Cardiol. 2012;35:219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Koulouris S, Lekatsas I, Karabinos I, Ioannidis G, Katostaras T, Kranidis A, Triantafillou K, Thalassinos N, Anthopoulos L. Microalbuminuria: a strong predictor of 3‐year adverse prognosis in nondiabetic patients with acute myocardial infarction. Am Heart J. 2005;149:840–845. [DOI] [PubMed] [Google Scholar]
- 23. Nazer B, Ray KK, Murphy SA, Gibson CM, Cannon CP. Urinary albumin concentration and long‐term cardiovascular risk in acute coronary syndrome patients: a PROVE IT‐TIMI 22 substudy. J Thromb Thrombolysis. 2013;36:233–239. [DOI] [PubMed] [Google Scholar]
- 24. Akerblom A, Clare RM, Lokhnygina Y, Wallentin L, Held C, Van de Werf F, Moliterno DJ, Patel UD, Leonardi S, Armstrong PW, Harrington RA, White HD, Aylward PE, Mahaffey KW, Tricoci P. Albuminuria and cardiovascular events in patients with acute coronary syndromes: results from the TRACER trial. Am Heart J. 2016;178:1–8. [DOI] [PubMed] [Google Scholar]
- 25. Kidney Disease: Improving Global O . KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. New York, NY: Nature Publishing Group; 2013. [Google Scholar]
- 26. Runesson B, Gasparini A, Qureshi AR, Norin O, Evans M, Barany P, Wettermark B, Elinder CG, Carrero JJ. The Stockholm CREAtinine Measurements (SCREAM) project: protocol overview and regional representativeness. Clin Kidney J. 2016;9:119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gasparini A, Evans M, Coresh J, Grams ME, Norin O, Qureshi AR, Runesson B, Barany P, Arnlov J, Jernberg T, Wettermark B, Elinder CG, Carrero JJ. Prevalence and recognition of chronic kidney disease in Stockholm healthcare. Nephrol Dial Transplant. 2016;31:2086–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carrero JJ, Grams ME, Sang Y, Arnlov J, Gasparini A, Matsushita K, Qureshi AR, Evans M, Barany P, Lindholm B, Ballew SH, Levey AS, Gansevoort RT, Elinder CG, Coresh J. Albuminuria changes are associated with subsequent risk of end‐stage renal disease and mortality. Kidney Int. 2017;91:244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD‐EPI (Chronic Kidney Disease Epidemiology Collaboration) . A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–694. [DOI] [PubMed] [Google Scholar]
- 31. Chronic Kidney Disease Prognosis C , Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT. Association of estimated glomerular filtration rate and albuminuria with all‐cause and cardiovascular mortality in general population cohorts: a collaborative meta‐analysis. Lancet. 2010;375:2073–2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Matsushita K, Coresh J, Sang Y, Chalmers J, Fox C, Guallar E, Jafar T, Jassal SK, Landman GW, Muntner P, Roderick P, Sairenchi T, Schottker B, Shankar A, Shlipak M, Tonelli M, Townend J, van Zuilen A, Yamagishi K, Yamashita K, Gansevoort R, Sarnak M, Warnock DG, Woodward M, Arnlov J; CKD Prognosis Consortium . Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta‐analysis of individual participant data. Lancet Diabetes Endocrinol. 2015;3:514–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. D'Agostino RB, Nam BH. Evaluation of the performance of survival analysis models: discrimination and calibration measures. 2003.
- 34. Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172; discussion 207–212. [DOI] [PubMed] [Google Scholar]
- 35. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. [DOI] [PubMed] [Google Scholar]
- 36. Konta T, Hao Z, Takasaki S, Abiko H, Ishikawa M, Takahashi T, Ikeda A, Ichikawa K, Kato T, Kawata S, Kubota I. Clinical utility of trace proteinuria for microalbuminuria screening in the general population. Clin Exp Nephrol. 2007;11:51–55. [DOI] [PubMed] [Google Scholar]
- 37. Mahmoodi BK, Matsushita K, Woodward M, Blankestijn PJ, Cirillo M, Ohkubo T, Rossing P, Sarnak MJ, Stengel B, Yamagishi K, Yamashita K, Zhang L, Coresh J, de Jong PE, Astor BC; Chronic Kidney Disease Prognosis Consortium . Associations of kidney disease measures with mortality and end‐stage renal disease in individuals with and without hypertension: a meta‐analysis. Lancet. 2012;380:1649–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kario K, Matsuo T, Kobayashi H, Matsuo M, Sakata T, Miyata T. Activation of tissue factor‐induced coagulation and endothelial cell dysfunction in non‐insulin‐dependent diabetic patients with microalbuminuria. Arterioscler Thromb Vasc Biol. 1995;15:1114–1120. [DOI] [PubMed] [Google Scholar]
- 39. Pedrinelli R, Giampietro O, Carmassi F, Melillo E, Dell'Omo G, Catapano G, Matteucci E, Talarico L, Morale M, De Negri F. Microalbuminuria and endothelial dysfunction in essential hypertension. Lancet. 1994;344:14–18. [DOI] [PubMed] [Google Scholar]
- 40. Moody WE, Edwards NC, Madhani M, Chue CD, Steeds RP, Ferro CJ, Townend JN. Endothelial dysfunction and cardiovascular disease in early‐stage chronic kidney disease: cause or association? Atherosclerosis. 2012;223:86–94. [DOI] [PubMed] [Google Scholar]
- 41. Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, Mautner B, Corbalan R, Radley D, Braunwald E. The TIMI risk score for unstable angina/non‐ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284:835–842. [DOI] [PubMed] [Google Scholar]
- 42. Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, Kuder JF, Wang H, Liu T, Wasserman SM, Sever PS, Pedersen TR; FOURIER Steering Committee and Investigators . Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–1722. [DOI] [PubMed] [Google Scholar]
- 43. American Diabetes A . 8. Cardiovascular disease and risk management. Diabetes Care. 2016;39(suppl 1):S60–S71. [DOI] [PubMed] [Google Scholar]
- 44. James PA, Oparil S, Carter BL, Cushman WC, Dennison‐Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 45. Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pedersen AB, Mikkelsen EM, Cronin‐Fenton D, Kristensen NR, Pham TM, Pedersen L, Petersen I. Missing data and multiple imputation in clinical epidemiological research. Clin Epidemiol. 2017;9:157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Baseline Characteristics by Sample
Table S2. Definition of Covariates
Table S3. Adjusted HRs (95% CIs)* of Adverse Outcomes After Index MI by Continuous ACR and Diabetes Mellitus Status
Table S4. Model Performance Measures With the Addition of ACR to TRS2°P Variables After Excluding Patients Who Died Within 14 Days After Hospitalization for MI
Table S5. Crude Incidence Rate (Per 100 Person‐Years) and Adjusted HRs (95% CIs)* of Adverse Outcomes After Index MI by Dipstick Proteinuria (N=2469)
Table S6. Model Performance Measures With the Addition of Dipstick Proteinuria to Conventional Risk Factors
Table S7. Adjusted HRs (95% CIs)* of Adverse Outcomes After Index MI by Continuous Urine ACR Among Patients With ACR Data (N=1151)
Table S8. Crude Incidence Rate (100 Person‐Years) and Adjusted HRs (95% CIs)* of Adverse Outcome After Index MI by Urine ACR Among Patients With ACR Data (N=1151)
Table S9. Model Performance Measures With the Addition of ACR to Conventional Risk Factors Among Patients With ACR Data (N=1151)
Figure S1. Study population.
Figure S2. One‐year probability of adverse outcomes by decile of 1‐year risk with the addition of urine albumin to creatinine ratio (ACR) to conventional risk factors.
Figure S3. Adjusted hazard ratios (HRs) of composite outcome after index myocardial infarction (MI) by linear splines of urine albumin to creatinine ratio (ACR) with 3 knots (10, 30, and 300 mg/g) in patients with ACR data.
Figure S4. Adjusted hazard ratios (HRs) of composite outcome after index myocardial infarction (MI) by linear splines of converted urine albumin to creatinine ratio (ACR) with 3 knots (10, 30, and 300 mg/g).


