Abstract
Background
Wait times for gastroenterologists in Canada continue to exceed recommended targets. Electronic consultation (eConsult) may reduce the need for face-to-face gastroenterologist visits.
Objective
The goal of this study was to identify the cases submitted to gastroenterologists though the Champlain BASE™ (Building Access to Specialists through eConsultation) eConsult service and explore their impact on primary care physicians’ (PCPs) courses of action.
Methods
Gastroenterology cases submitted between June 2013 and January 2015 were categorized using a modification of the International Classification for Primary Care (ICPC-2) taxonomy. Question type (e.g., diagnosis or management) was classified using a validated taxonomy.
Results
Of the 121 gastroenterology consults reviewed, 33% were related to hepatology, 23% to GI symptoms, and 13% to specific luminal diseases. Among hepatology eConsults (n=40), 47% pertained to abnormal liver function testing. Overall, 51% of eConsults were related to diagnosis, 30% to management, 9% to drug treatments and 7% to procedures. PCPs received a reply within a median of 2.9 days. Only 25% of cases resulted in a face-to-face referral.
Conclusions
The eConsult service provided timely, highly regarded advice from gastroenterologists directly to PCPs and often eliminated the need for a face-to-face consultation. An evaluation of the most commonly-posed questions could inform future continuing medical education activities for PCPs.
Keywords: Access to care, eConsult, Wait times
INTRODUCTION
Access to specialty care remains a challenge in Canada, where patients frequently face long wait times for specialist appointments. Primary care providers (PCPs) often cite gastroenterology as a high-demand specialty,(1, 2) and consequently, wait times for gastroenterologist appointments regularly exceed recommended benchmarks, which range from two weeks to two months depending on the condition.(3) New solutions are needed to improve access to advice from gastroenterologists for patients in a time frame supported by existing guidelines.
Virtual consultations such as telemedicine (where the provider connects to a patient remotely) and eConsult (where the referring provider ask a patient-specific question to a specialist through a secure server) have been demonstrated to reduce the need for patients to attend an in-person specialist visit.(1, 2) Within gastroenterology, telemedicine has been used primarily for patients with hepatitis C and inflammatory bowel disorders.(4, 5) There is one report from the Mayo Clinic that reported on gastroenterology eConsults occurring within the organization. They demonstrated that, of the 901 eConsults submitted, only 160 required a face-to-face visit.(2) Providers have noted that eConsults have an added benefit beyond reducing the number of patient visits by serving as an educational tool for PCPs, as the answers they receive can inform the care they provide for other patients and lead to discussions with peers about similar cases.(6) Building capacity within primary care on common referral scenarios can help reduce the number of referrals to subspecialty services, thus increasing time for more urgent consultations and sicker patients.(7)
The objective of this study was to 1) describe the utilization and impact of gastroenterology eConsults submitted through the Champlain BASE™ (Building Access to Specialists through eConsultation) eConsult service and 2) determine the types of questions most commonly asked by PCPs.
METHODS
Study design
We conducted a cross-sectional study of all eConsult cases submitted to gastroenterologists between June 2013 and January 2015. The University of Ottawa Research Ethics Board provided full approval for this study.
Setting
The Champlain BASE™ eConsult service is based in the Champlain Local Health Integration Network (LHIN), a health region in eastern Ontario. The Champlain LHIN has a population of 1.2 million, roughly half of which resides in the region’s main metropolitan centre (Ottawa) and half in the surrounding communities and rural areas up to two hours away by car.
The champlain BASE™ eConsult service
The Champlain BASE™ eConsult service, established in 2010, uses a secure web-based platform through which PCPs (family physician or nurse practitioner) can submit a patient-specific clinical question to over 100 different specialty services. Gastroenterology was added to the service June 2013.(8) PCPs can attach supplementary investigations such as laboratory or imaging results that may be relevant to the question asked. The specialist receives notification of the pending case via email and has seven days to respond following the initial email notification. The specialist responds through the same secure web-based platform by providing clinical advice, requesting further information or recommending a face-to-face consultation. This dialogue continues until the PCP closes the case. In order to close a case, the PCP must complete a brief survey assessing the case’s outcome and perceived value for the patient and PCP (Figure 1). Specialists are remunerated at $200 CAD per hour prorated to their self-reported time spent answering the case. We calculated the costs paid to the specialist for eConsults and compared those to payment for a face-to-face referral based on the current Ontario fee schedule ($157 per consult seen).
Figure 1.
Closeout survey administered upon completion of each eConsult.
Data collection and analysis
The eConsult service automatically collects utilization data for each case, including PCP type (family doctor versus nurse practitioner), patient age and gender, specialty referred to, and specialist self-reported response time. Additionally, the service saves a complete log of all exchanges between PCPs and specialists, with timestamps indicating when each exchange was sent. PCP feedback is collected via the mandatory closeout survey. All data were exported into an Excel database for analysis.
We identified all cases submitted to gastroenterology during the study period. All cases were received and responded to by a single gastroenterologist at our institution who has been in practice for over 10 years. Descriptive analyses were used to quantify the most common clinical topics and question types. All cases between June 2013 and January 2015 were reviewed retrospectively for gastroenterology content using a predefined list of clinical diagnoses, which was generated by consensus using a modification of the International Classification for Primary Care (ICPC-2) taxonomy. Each question was also classified by the type of question (e.g., diagnosis or management) using a validated taxonomy.(9) To ensure agreement on categorization, the first 20 eConsults were coded by the resident (SC) and reviewed with the specialist (NS). Any disagreements were resolved through re-reviewing and discussing the eConsult in detail. To examine eConsult’s impact on referral behaviour, we collected PCPs’ responses to the mandatory closeout survey for all gastroenterology cases.
RESULTS
Between June 24, 2013 (when GI was added as an eConsult specialty) and January 31, 2015, 1264 cases were completed through the Champlain BASE™ service, of which 184 (14.5%) were directed to gastroenterology. A subset of 100 to 120 cases was deemed sufficient for the analysis, and as such, 121 cases were coded.
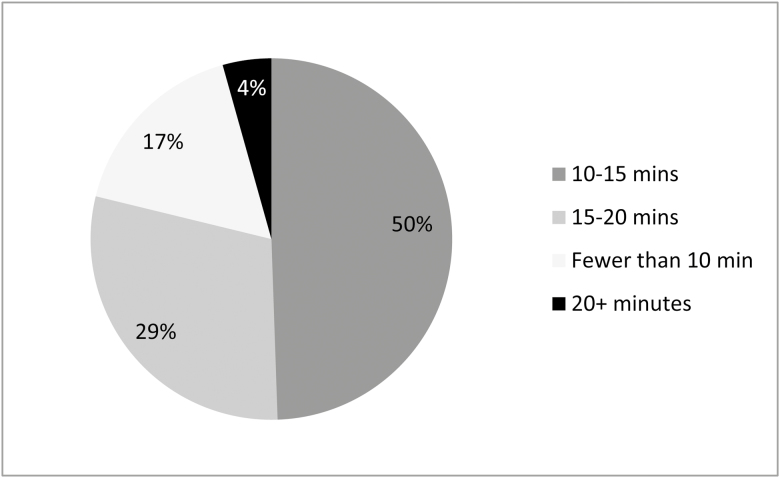
Of the 121 cases included in the study, 113 (93%) were completed by family physicians and 8 (7%) by nurse practitioners. PCPs received a reply within a median of 2.9 days. The time the gastroenterologist self-reported for completing the case was less than 10 minutes in 16 (8%) cases, 10–15 minutes in 60 (50%) cases, 15–20 minutes in 41 (34%) cases and over 20 minutes in 4 (3%) of cases (Figure 2). The average specialist payment was $54.53 per consult.
Figure 2.
Specialists’ self-reported response times for eConsult cases.
Of the 121 gastroenterology consults reviewed, 33% were related to liver issues, 23% to gastrointestinal (GI) symptoms and 13% to specific luminal diseases (Table 1). Of the liver-related eConsults, 47% were specifically regarding abnormal liver enzyme tests. Imaging findings were also common, with 15% of cases for fatty liver and 10% for liver nodules. Among eConsults for GI symptoms, the most common questions regarded gastroesophageal reflux disease (30% of GI symptom questions) and abdominal pain (24%).
Table 1.
eConsults to GI specialists by question category (n=121)
| Category | N | % of Category |
|---|---|---|
| Hepatology (n = 40) | ||
| Liver Abnormal LFTs NOS | 23 | 58% |
| Hepatomegaly | 1 | 3% |
| Fatty Liver | 6 | 15% |
| Liver Cirrhosis | 1 | 3% |
| Haemachromatosis | 1 | 3% |
| Low Ceruloplasmin | 1 | 3% |
| Hepatitis B | 1 | 3% |
| Hepatitis C | 2 | 5% |
| Liver nodule/Lesion | 4 | 10% |
| Luminal GI (n = 26) | ||
| Celiac disease/gluten sensitivity | 7 | 27% |
| IBD | 2 | 8% |
| Barrett’s Esophagus | 1 | 4% |
| Esophageal Disease | 1 | 4% |
| Recurrent Bowel Obstruction | 1 | 4% |
| H. Pylori | 5 | 19% |
| Anal Fissure/Perianal Abscess | 1 | 4% |
| IBS | 6 | 23% |
| Colonic Polyps/Colorectal Cancer | 1 | 4% |
| GI Cancer | 1 | 4% |
| GI Symptoms (n = 33) | ||
| Gastroesophageal reflux disease Abdominal | 10 | 30% |
| pain/Cramps | 8 | 24% |
| Chronic Diarrhoea | 5 | 15% |
| Constipation | 2 | 6% |
| Rectal/Anal Pain | 3 | 9% |
| Fecal Incontinence | 1 | 3% |
| Belching | 1 | 3% |
| Easy Gagging | 1 | 3% |
| Weight gain | 1 | 3% |
| Dyspepsia/Indigestion | 1 | 3% |
| Procedures (n = 9) | ||
| Screening Colonoscopy | 7 | 78% |
| Colonoscopy | 1 | 11% |
| PEG | 1 | 11% |
| Other (n = 7) | ||
| Gallbladder polyps | 2 | 29% |
| Pancreatic disease | 1 | 14% |
| Zinc Deficiency | 1 | 14% |
| Periumbilical Ecchymoses | 1 | 14% |
| Use of NSAID in post = gastric bypass | 1 | 14% |
| Anaemia | 1 | 14% |
Question type related to diagnosis in 51% of cases, management of a disease/symptoms in 30%, drug treatments in 9%, and procedures in 7%. Of the procedural-related questions, the majority (78%) were regarding colonoscopy.
Based on the end of consult survey, PCPs reported the service as high or very high quality for them and their patient in 97% of cases. The eConsult changed the clinical course of many patients, with PCPs identifying that in 80 (66%) of cases, the PCP identified that they received advice for a new or additional course of action. There was significant impact on PCP intention to refer the patient for a face-to-face referral.
In 51 (42%) cases, a referral was originally contemplated, but ultimately avoided. In 31 (26%) cases, a referral was not originally contemplated and was still not needed. Overall, 68% of all completed cases did not require a face-to-face visit. In 32 (26%) cases, a referral was originally contemplated and was still needed, but the PCP perceived that eConsult would lead to a more effective specialist visit. In 4 (3%) cases, a referral was not originally contemplated, but eConsult process resulted in a referral being initiated. The total cost of specialist payment for eConsult was $6599. The cost for face-to-face visits if eConsult was not available would have been $13,031 (83 patients at $157 each) compared with $5495 (36 patient at $157 each) after an eConsult. Thus, the overall cost with eConsult and subsequent face-to-face visits was $12,094, compared with anticipated $13,031 if eConsult was not available. We did not calculate costs to the patient or other indirect costs.
DISCUSSION
Given the increasing challenges gastroenterologists face in meeting benchmark wait times for care, eConsult offers an opportunity to reduce the number of face-to-face visits required.(3) Champlain BASE™ is the first eConsult service in Canada to include gastroenterology among its available specialties and has demonstrated the ability to provide PCPs and their patients with quick access to high-quality advice on gastroenterological issues, often without the need of a face-to-face visit with a specialist. While eConsult has the potential to reduce costs at a system level by avoiding unnecessary referrals, it can also have a positive economic impact on a patient level, since by avoiding unnecessary referrals, patients are able to avoid missing work or school or paying travel costs associated with specialist visits. These costs can be significant for patients in rural areas who must travel great distances for specialist care.(1, 10)
Healthcare providers have evaluated a number of different methods for reducing the need for face-to-face visits in gastroenterology. One such model involves allowing electronic communication between patients and gastroenterologists directly by connecting both parties via email or telephone, a situation most common for patients with chronic diseases who require regular follow-up with GI specialists.(11) Numerous studies have examined telephone consultations as an alternative to face-to-face consultations with gastroenterologists, noting that remote consultations improved overall quality of follow-up care, reduced nonattendance rates and shorter wait times for urgent appointments.(12–14) Although a number of studies have established eConsult’s ability to improve access, reduce need for face-to-face referrals, provide high levels of provider satisfaction and lower costs,(15, 16) there is only one study that specifically reports on gastroenterology eConsults. This study was conducted at the Mayo Clinic, where the referring and specialist providers’ access to the same EMR was established not to reduce wait times, but rather to improve efficiencies. Despite differences with the Champlain BASE™ model, the Mayo Clinic service demonstrated a similar savings in face-to-face referrals, with only 18% of the cases being converted to a face-to-face consultation. The most common clinical questions asked through the Mayo Clinic service were cancer screening, image interpretation, interpretation of lab results and procedure questions. The differences between the most common questions compared to our study may be due in part to the varying roles of PCPs in each system and to a restriction placed on ‘orderable’ eConsults through the Mayo Clinic electronic medical record.
While the Champlain BASE™ eConsult service was designed first and foremost to improve patients’ access to specialist advice, its ability to foster two-way communication between PCPs and specialists has had the unintentional benefit of supporting PCP learning. In a recent analysis of PCPs’ open text responses to the mandatory closeout survey, eConsult’s ability to serve as an educational tool emerged as a frequent theme.(6) Many PCPs noted that the advice they received from specialists was applicable to multiple cases and would likely improve their ability to treat future patients with similar conditions. Our findings suggest that such learning could reduce the need for gastroenterology referrals: one-third of the cases in our study were for hepatology concerns, the majority of which involved identification of abnormal liver enzymes, a process that could easily be carried out by the PCP without necessitating a face-to-face specialist referral. By identifying the most frequent questions PCPs pose to various specialties, eConsult could help guide future continuing medical education curricula and ensure PCPs are receiving education on topics relevant to their patients’ needs.
Our study is somewhat limited by the small sample size and focus on one geographical region. We have since expanded our eConsult service to different jurisdictions within Ontario and other provinces. We hope to be able to demonstrate more generalizability in future studies. It is too early to determine if the availability of an eConsult service will significantly impact wait times. We do not collect patient identifiers and thus cannot track individual patient outcomes. This is an important outcome which we will be studying in future projects. We are unable to compare our outcomes of traditional referrals.
CONCLUSIONS
The eConsult service provided timely, highly regarded advice from gastroenterologists directly to PCPs and often eliminated the need for a face-to-face consultation. With limited resources and access to gastroenterologists across Canada, eConsults provide a means to assist patient care provided by PCPs. Unnecessary referrals are avoided, which should result in reducing wait times for more urgent referrals. Commonly recurring questions can be used to inform planning of future continuing professional development events.
Acknowledgements
This work was supported by the Royal College of Physicians and Surgeons of Canada, Department of Medicine University of Ottawa, Ontario Ministry of Health and Long-Term Care, The Ottawa Hospital Academic Medical Organization Innovation Fund, e-Health Ontario, and the Champlain Local Health Integration Network.
References
- 1. Kirsh S, Carey E, Aron DC et al. Impact of a national specialty e-consultation implementation project on access. Am J Managed Care 2015;21(12):e648–54. [PubMed] [Google Scholar]
- 2. North F, Uthke LD, Tulledge-Scheitel SM. Internal e-consultations in an integrated multispecialty practice: A retrospective review of use, content, and outcomes. J Telemed Telecare 2015;21(3):151–9. [DOI] [PubMed] [Google Scholar]
- 3. Leddin D, Bridges RJ, Morgan DG et al. Survey of access to gastroenterology in Canada: The SAGE wait times program. Can J Gastroenterol Hepatol 2010;24(1):20–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Siegel CA. Transforming gastroenterology care with telemedicine. Gastroenterol 2017;152(5):958–63. [DOI] [PubMed] [Google Scholar]
- 5. Aguas M, Del Hoyo J, Faubel R et al. Telemedicine in inflammatory bowel disease: Opportunity ahead. Inflamm Bowel Dis 2016;22(2):E4–5. [DOI] [PubMed] [Google Scholar]
- 6. Liddy C, Afkham A, Drosinis P et al. Impact and satisfaction with a new eConsult service: A mixed methods study of primary care providers. J Am Board Fam Med 2015;28(3):394–403. [DOI] [PubMed] [Google Scholar]
- 7. Mata-Roman L, del Olmo-Martinez L, Briso-Montiano R et al. Periodic gastroenterology and hepatology meetings with primary care. Reasons for consultation. Revista Espanloa De Enfermedades Digestivas 2013;105(9):521–8. [DOI] [PubMed] [Google Scholar]
- 8. Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-Consultation service across diverse specialties and primary care providers. Telemed J E Health 2013;19(10):733–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ely JW, Osheroff JA, Gorman PN et al. A taxonomy of generic clinical questions: Classification study. BMJ 2000;321(7258):429–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liddy C, Drosinis P, Deri Armstrong C et al. What are the cost savings associated with providing access to specialist care through the Champlain BASE eConsult service? A costing evaluation. BMJ Open 2016;6(6):e010920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Plener I, Hayward A, Saibil F. E-mail communication in the management of gastroenterology patients: A review. Can J Gastroenterol Hepatol 2014;28(3):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Akobeng AK, O’Leary N, Vail A et al. Telephone consultation as a substitute for routine out-patient face-to-face consultation for children with inflammatory bowel disease: Randomised controlled trial and economic evaluation. EBioMedicine 2015;2(9):1251–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gethins S, Robinson R, de Caestecker J et al. Impact of a nurseGêÆ led telephone clinic on quality of IBD care. Gastrointestinal Nursing 2007;5(1):34–9. [Google Scholar]
- 14. Miller L, Caton S, Lynch D. Telephone clinic improves quality of follow-up care for chronic bowel disease. Nursing Times 2001;98(31):36–8. [PubMed] [Google Scholar]
- 15. Liddy C, Drosinis P, Keely E. Electronic consultation systems: Worldwide prevalence and their impact on patient care: A systematic review. Fam Pract 2016;33(3):274–85. [DOI] [PubMed] [Google Scholar]
- 16. Vimalananda VG, Gupte G, Seraj SM et al. Electronic consultations (e-consults) to improve access to specialty care: A systematic review and narrative synthesis. J Telemed Telecare 2015;21(6):323–30. [DOI] [PMC free article] [PubMed] [Google Scholar]