Abstract
Aims
Our goals were to compare the effect of adding fentanyl to midazolam in a double-blinded, randomized, placebo-controlled trial and determine if fentanyl enhances sedation, increases adverse events or effects time of the procedure or discharge.
Methods
Patients 18 to 65 years scheduled for outpatient upper endoscopy were eligible for the study. Patients were randomized to receive either 100 mcg/2 mL of Fentanyl or 2 mL of placebo IV with a double-blinded protocol. All patients received 2 mg of intravenous midazolam initially. Additional midazolam could be given to achieve adequate sedation.
Results
There were 68 patients randomized to the Fentanyl group and 69 patients to the placebo group. The mean dose of midazolam was 4.0 mg for the Fentanyl group and 5.2 mg for placebo group (P=0.003). Both endoscopist and nurse independently rated sedation to be better in the fentanyl group (P=0001). The patient did not perceive any difference in sedation (P=0.4). Procedure time was significantly shorter in the Fentanyl group (8.5 versus 11.1 minutes, P=0.001), with no difference in the discharge time. There was significantly less retching observed in patients in the fentanyl group (P<0.001). There were no major complications.
Conclusions
Endoscopists and nurses found adding fentanyl significantly improved sedation, led to a shorter procedure time, and allowed for less midazolam to be used per case. It did not affect the patient experience of sedation and was safe. Fentanyl use for routine outpatient upper endoscopy should be considered as a safe option to improve procedural sedation.
NCT:01514695 (www.clinicaltrials.gov)
Accepted as an abstract for the Canadian Digestive Diseases Week meeting in February 2014.
Keywords: Clinical trial, Endoscopy, Fentanyl, Quality, Sedation
Upper gastrointestinal (GI) endoscopy is a valuable diagnostic and therapeutic procedure considered safe in most patients. However, some patients experience discomfort from air insufflation in the stomach and unpleasantness due to gagging during the procedure. Sedation has been shown to improve success in performing endoscopies and improve patient satisfaction (1–3). Conscious sedation with a benzodiazepine (sedative) and opioid narcotic analgesia are used routinely in Canada for a variety of procedures to improve patient and physician satisfaction without compromising safety (4).
There is a lack of consensus about choice of sedative use in upper GI endoscopy as discussed in meta-analysis and guidelines (5–7). Some endoscopists use midazolam (benzodiazepine) or narcotics alone, but many use midazolam in combination with a narcotic (either meperidine or fentanyl) (8–11). Fentanyl was a better tolerated drug compared with meperidine in studies of patients undergoing colonoscopy (12). Studies with meperidine added to midazolam suggested a benefit in endoscopist satisfaction (13–15). A single study investigated the use fentanyl in addition to midazolam for upper GI endoscopy, but this study was small, not randomized, and not blinded (16). The results suggested that patients did not find a difference in the procedure adding fentanyl, but endoscopists found the procedure easier.
Optimizing sedation is important for the endoscopist to complete the examination with ease and for the patient to be comfortable during the procedure. Many patients have significant anxiety, which can be mitigated by sedation and provide a more pleasant endoscopy experience. However, there are potential risks of over-sedation with narcotics including aspiration, transient hypoxemia and airway obstruction, especially for those patients with significant systemic illness (17). Most sedation is administered at the discretion of the endoscopist to maintain ease of performing the procedure.
PURPOSE
The purpose of this study was to perform a large, double-blinded, placebo-controlled, randomized clinical trial to assess if adding fentanyl to midazolam provides further benefit for patient perceived satisfaction, endoscopist satisfaction, and nurse satisfaction during routine upper endoscopy without significant adverse effects.
METHODS
The study was approved by the hospital research ethics board at St. Joseph’s Healthcare Hamilton and McMaster University. Recruitment occurred from March to December of 2012.
Inclusion and Exclusion Criteria
All patients 18 to 65 years scheduled for routine outpatient upper endoscopy by a gastroenterologist at St. Joseph’s Healthcare Hamilton were eligible for the study, provided they could give consent. Patients were approached by a research staff to participate when they registered for their endoscopy, and no incentive was offered for participating. Exclusion criteria included mental incompetency, pregnancy, weight <55 kg, emergent procedures, known hypersensitivity or allergy to fentanyl or midazolam, chronic use of benzodiazepines or opioids, patients known a priori to require therapeutic interventions in conjunction with their EGD (e.g., dilation, Argon Plasma Coagulation, or esophageal variceal ligation) and patients with major cardiorespiratory comorbidities, sleep apnea, liver cirrhosis, or renal failure. Patients could refuse to participate at any time by verbalizing to any staff member their wish to withdraw consent. All data was to be analyzed.
Randomization, Allocation, and Blinding
A computer-generated, two-group randomization table was prepared by the inpatient pharmacy. Identical syringes of Fentanyl or placebo (saline solution) were assembled by the pharmacy, and allocation was concealed to any of the patients, research or clinical staff. The drugs were allocated to patients by nurses once a patient was consented in the endoscopy unit. As both the fentanyl and saline syringes were identical, blinding was preserved throughout the study, and the research team was only informed of the contents of the syringes after study completion.
Drug Dose and Administration
A dose of 100 mcg of Fentanyl intravenously was chosen as the study drug. This is routinely used as a standard dose in patients undergoing endoscopy and is high enough to distinguish whether it has an additive effect to midazolam.
After an initial 2 mg dose of intravenous Midazolam, patients were immediately given a 100 mcg dose of intravenous fentanyl or an identical syringe of placebo. The combination of drugs is within a safe range for patients weighing more than 55 kg to receive (18). Additional Midazolam was titrated as needed in 1 mg increments for deeper sedation at the discretion of the endoscopist, but no further fentanyl could be given. Topical xylocaine could be administered in the oropharynx at the discretion of the endoscopist.
Procedure details
All procedures were completed by a gastroenterologist or senior gastroenterology resident under direct supervision by a gastroenterologist. There were eight gastroenterologists who participated with a minimum of three years of experience in endoscopy.
All patients’ heart rates, blood pressures and oxygen saturations were monitored during the procedure and in recovery until ready for discharge. All patients were given 2 L oxygen by nasal cannula at the beginning of procedure; this is standard protocol in the endoscopy unit.
Sample size calculation
We estimated a difference of 20% in the overall satisfaction between a better score (e.g., excellent or good) to a poor score (e.g., fair or difficult or very difficult) in the Fentanyl group compared with the placebo group and assume that the Fentanyl group would have 90% of patients with a better score. Using a two-sided alpha of 0.05 and a power of 80%, the number in each arm required is 72 patients. Assuming a 5% missing data rate, the number of patients we aimed to recruit was 75 per arm.
Primary outcomes include endoscopist, nurse and patient satisfaction with sedation reported independently after the procedure on a five-point visual Likert scale, with one as extremely satisfied and five as extremely dissatisfied. Secondary outcomes included significant retching that persisted after intubation, presence of adverse events, time of procedure, and time to discharge after procedure. We also contacted patients up to 48 hours after the procedure by telephone and asked their willingness to repeat the procedure. Any adverse events were recorded, including change in vitals or episodic desaturation in oxygen.
RESULTS
During the study period, 283 patients were screened to be eligible, and 139 were recruited in the study. The most common reasons for exclusion were that the patient was not interested (n=58), had major comorbidities (n=26), required no sedation (n=20), had chronic opiate or benzodiazapine use (n=19), did not specify (n=10), could not provide consent to the study (n=9), and weighed less than 55 kg (n=2). Two patients withdrew after being randomized: one refused to participate after she consented, and the other’s procedure was cancelled by the endoscopist.
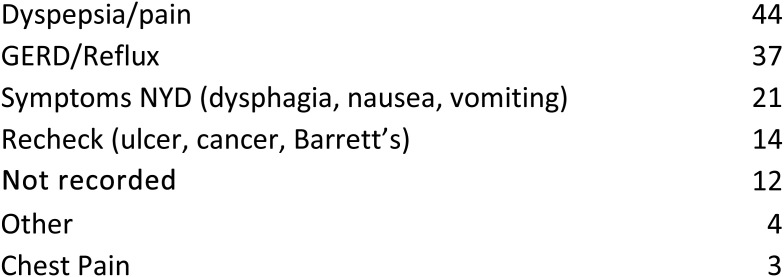
The mean age was 45 years, and 39.6% were male. The mean patient weight was 77.7 kg. Most patients were American Society of Anesthesiology (ASA) class one (85%). The most common indications for upper endoscopy were to investigate dyspepsia/epigastric pain (n=44), Gastro Esophageal Reflux Disease (GERD)/Reflux (n=37), and upper GI symptoms NYD (n=21) (see Figure 1).
Figure 1.
Indications for upper endoscopy
Of the 137 patients analyzed, 68 were allocated in the Fentanyl group, with 69 in the placebo group. The baseline characteristics were similar for both groups (see Table 1).
Table 1.
Baseline characteristics
| Fentanyl N=68 |
Placebo N=69 |
|
|---|---|---|
| Age (years) | 44.9 | 45.7 |
| Males (%) | 0.46 | 0.35 |
| Weight (kg) | 78.0 | 77.9 |
| ASA 1 | 62 | 56 |
| ASA 2 | 5 | 12 |
| ASA 3 | 1 | 0 |
| Midazolam dose (mg) | 4.0 | 5.2 |
| Xylocaine given, n | 48 | 54 |
Before the procedure, 48 patients in the fentanyl group and 54 patients in the placebo group received topical xylocaine (P=0.30). The mean dose of midazolam given to the fentanyl group was 4.0 mg compared with 5.2 mg given to the placebo group, and this difference was statistically significant, with P=0.003.
The primary outcome was a significant improvement in independently reported endoscopist and nurse satisfaction with the fentanyl group compared with the placebo group (1.4 versus 2.5 P =< 0.01). However, there was no difference in the patient satisfaction in the fentayl group compared with the placebo group (1.3 versus 1.5, P=0.4, see Table 2).
Table 2.
Primary and secondary outcomes
| Fentanyl (n=68) | Placebo (n=69) | P-value | |
|---|---|---|---|
| Patient satisfaction, mean 1–5* | 1.3 | 1.5 | P=0.4 |
| MD satisfaction, mean 1–5* | 1.4 | 2.5 | P<0.001 |
| Nurse satisfaction, mean 1–5* | 1.4 | 2.5 | P<0.001 |
| Significant Retching, n | 3 | 34 | P<0.001 |
| Willing to repeat, n, % | 60, 100 | 56, 100 | n/a |
| Procedure time, minutes | 8.5 | 11.1 | P=0.001 |
| Discharge time, minutes | 35.6 | 37.2 | P=0.54 |
(* 1–5 where 1 is extremely satisfied, and 5 is extremely dissatisfied)
Significant retching during the procedure was seen more often in the placebo group (34 of 69) compared with the fentanyl group (3 of 68) (P<0.01).
The time of procedure in the fentanyl group was 8.5 minutes compared with 11.1 minutes in the placebo group, and this difference was statistically significant (P=0.001). The time to discharge after the procedure in the fentanyl group was 35.6 minutes compared with 37.2 minutes in the placebo group, and this was not statistically significant (P=0.54).
There were no major adverse events. We recorded three transient drops in oxygen saturation <90% (all in the Fentanyl group), and two minor complications (both in placebo group), with 1 patient vomiting and another reporting nausea.
The patients’ willingness to repeat the procedure was confirmed by telephone in 116 patients (60 in the fentanyl group and 56 in the placebo group). All patients reported a willingness to repeat the procedure if necessary.
DISCUSSION
This study demonstrated that adding fentanyl to routine outpatient upper endoscopy may provide several advantages to using midazolam alone. To our knowledge, this is the first double-blinded, placebo-controlled trial adding fentanyl to midazolam in upper endoscopy and shows that the quality of the procedure is likely better. This conclusion is based on significantly less retching during the procedure and independent nurse and physician assessment of the procedure as being better in terms of satisfaction of sedation.
Adding fentanyl for sedation also significantly shortened the procedure time by two and a half minutes, which is over 20% faster. This benefit may be counter intuitive to traditional thinking in quality of endoscopy because longer procedures are thought to be correlated with better exams; however, in routine upper endoscopy, a shorter procedure time could be associated with a better exam if the patient is not moving or retching. Moreover, shorter and smoother endoscopy procedures will help keep endoscopy units on schedule and make the turnaround time for procedures easier.
Not surprisingly, adding fentanyl resulted in significantly less midazolam use during the procedure, which may be beneficial to patients because midazolam is a longer acting sedative and could be associated with more side effects like persistent nausea and fatigue.
Fentanyl did not show any major side effects. There were 3 incidences of transient oxygen desaturations. Regular use of oxygen support during the procedure with 2 L by nasal pronged likely masked some of the side effects of respiratory depression. A CO2 monitor would have been a useful tool for measuring respiratory effect, but this was not available to us.
Some of the limitations of our study include the small size of the study, but our target population based on power calculations was met. Most of the patients were females, and most patients had dyspepsia or GERD, suggesting a possible selection bias. We excluded high risk patients, and there was only one patient who was ASA class three in the entire study. It is possible that higher risk patients may not tolerate as much sedation and be prone to sedation-related complications. It is possible the study group was identified by the endoscopist, despite blinding and allocation concealment, as the dose of midazolam was higher in the placebo group.
The only caveat to consider is that patients do not feel any different whether they receive fentanyl or not. The lack of difference from a patient perspective is worth noting. Even though significant retching is experienced by patients in the midazolam/placebo group, the amnestic effect of the sedative provides a good experience for most patients, and one they would be willing to repeat whether fentanyl is added or not.
In summary, this study demonstrated that adding fentanyl to midazolam for sedation in outpatient upper endoscopy provided superior sedation. There was a statistically significant benefit from reduced retching and satisfaction of the endoscopist and nurse caring for the patient, and this may permit a higher quality procedure in a shorter time. However, the patient’s perception is no different after the procedure, nor is it any different when asked if they are willing to repeat the procedure up to 48 hours later. Although using fentanyl did not show major side effects or complications, caution must be taken in patients with advanced age or major comorbidities and with patients undergoing emergent procedures, as these patients were not included in the study.
ACKNOWLEDGEMENTS
The authors wish to thank Jody Hannah, Dr. Raffaela Profiti, Linda Gandy and the endoscopy staff at St. Joseph’s Healthcare Hamilton for their clinical support, Christine Wallace and the pharmacy staff at St. Joseph’s Healthcare for their technical support, and Lisa Balogh-Melanson, Atif Nehvi, Shoaib Ahmad and Dr. Tahseen Rahman for their logistical support. Special thanks to Dr. Paul Moayyedi for mentorship and the Division of Gastroenterology at McMaster University for funding support.
References
- 1. Abraham NS, Fallone CA, Mayrand S, et al. Sedation versus no sedation in the performance of diagnostic upper gastrointestinal endoscopy: A Canadian randomized controlled cost-outcome study. Am J Gastroenterol 2004;99(9):1692–9. [DOI] [PubMed] [Google Scholar]
- 2. Sachdeva A, Bhalla A, Sood A, et al. The effect of sedation during upper gastrointestinal endoscopy. Saudi J Gastroenterol 2010;16(4):280–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ciriza de los Ríos C, Fernández Eroles AL, García Menéndez L, et al. Sedation in upper gastrointestinal endoscopy. Analysis of tolerance, complications and cost-effectiveness. Gastroenterol Hepatol 2005;28(1):2–9. [DOI] [PubMed] [Google Scholar]
- 4. Baris S, Karakaya D, Aykent R, et al. Comparison of midazolam with or without fentanyl for conscious sedation and hemodynamics in coronary angiography. Can J Cardiol 2001;17(3):277–81. [PubMed] [Google Scholar]
- 5. McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc 2008;67(6):910–23. [DOI] [PubMed] [Google Scholar]
- 6. Thomson A, Andrew G, Jones DB. Optimal sedation for gastrointestinal endoscopy: Review and recommendations. J Gastroenterol Hepatol 2010;25(3):469–78. [DOI] [PubMed] [Google Scholar]
- 7. Cohen LB, Ladas SD, Vargo JJ, et al. Sedation in digestive endoscopy: The Athens international position statements. Aliment Pharmacol Ther 2010;32(3):425–42. [DOI] [PubMed] [Google Scholar]
- 8. Hsieh YH, Lin HJ, Hsieh JJ, et al. Meperidine as the single sedative agent during esophagogastroduodenoscopy, a double-blind, randomized, controlled study. J Gastroenterol Hepatol 2013;28(7):1167–73. [DOI] [PubMed] [Google Scholar]
- 9. Robertson DJ, Jacobs DP, Mackenzie TA, et al. Clinical trial: A randomized, study comparing meperidine (pethidine) and fentanyl in adult gastrointestinal endoscopy. Aliment Pharmacol Ther 2009;29(8):817–23 [DOI] [PubMed] [Google Scholar]
- 10. Cinar K, Yakut M, Ozden A. Sedation with midazolam versus midazolam plus meperidine for routine colonoscopy: A prospective, randomized, controlled study. Turk J Gastroenterol 2009;20(4):271–5. [DOI] [PubMed] [Google Scholar]
- 11. Wang F, Shen SR, Xiao DH, et al. Sedation, analgesia, and cardiorespiratory function in colonoscopy using midazolam combined with fentanyl or propofol. Int J Colorectal Dis 2011;26(6):703–8. [DOI] [PubMed] [Google Scholar]
- 12. Hayee B, Dunn J, Loganayagam A, et al. Midazolam with meperidine or fentanyl for colonoscopy: Results of a randomized trial. Gastrointest Endosc 2009;69(3 Pt 2):681–7. [DOI] [PubMed] [Google Scholar]
- 13. Ozel AM, Oncü K, Yazgan Y, et al. Comparison of the effects of intravenous midazolam alone and in combination with meperidine on hemodynamic and respiratory responses and on patient compliance during upper gastrointestinal endoscopy: A randomized, double-blind trial. Turk J Gastroenterol 2008;19(1):8–13. [PubMed] [Google Scholar]
- 14. Laluna L, Allen ML, Dimarino AJ Jr. The comparison of midazolam and topical lidocaine spray versus the combination of midazolam, meperidine, and topical lidocaine spray to sedate patients for upper endoscopy. Gastrointest Endosc 2001;53(3):289–93. [DOI] [PubMed] [Google Scholar]
- 15. Diab FH, King PD, Barthel JS, et al. Efficacy and safety of combined Meperidine and Midazolam for EGD sedation compared with Midazolam alone. Am J Gastroenterol 1996;91(6):1120–5. [PubMed] [Google Scholar]
- 16. Barriga J, Sachdev MS, Royall L, et al. Sedation for upper endoscopy: Comparison of midazolam versus fentanyl plus midazolam. South Med J 2008;101(4):362–6 [DOI] [PubMed] [Google Scholar]
- 17. Verschoore T, Vandecandelaere S, Vandecandelaere P, et al. Risk factors for complications and mortality related to endoscopic procedures in adults. Acta Gastroenterol Belg 2016;79(1):39–46. [PubMed] [Google Scholar]
- 18. Cohen LB, Ladas SD, Vargo JJ. et al. AGA Institute review of endoscopic sedation. Gastroenterology 2007; 133(2):675–701. [DOI] [PubMed] [Google Scholar]