INTRODUCTION
Patients with microvillous inclusion disease (MVID) are at risk for development of cholestatic liver disease. We report a case of a parenteral nutrition (PN)-dependent patient with MVID and intractable pruritus managed with a fish oil-based lipid emulsion (FOLE).
PRESENTATION OF THE CASE
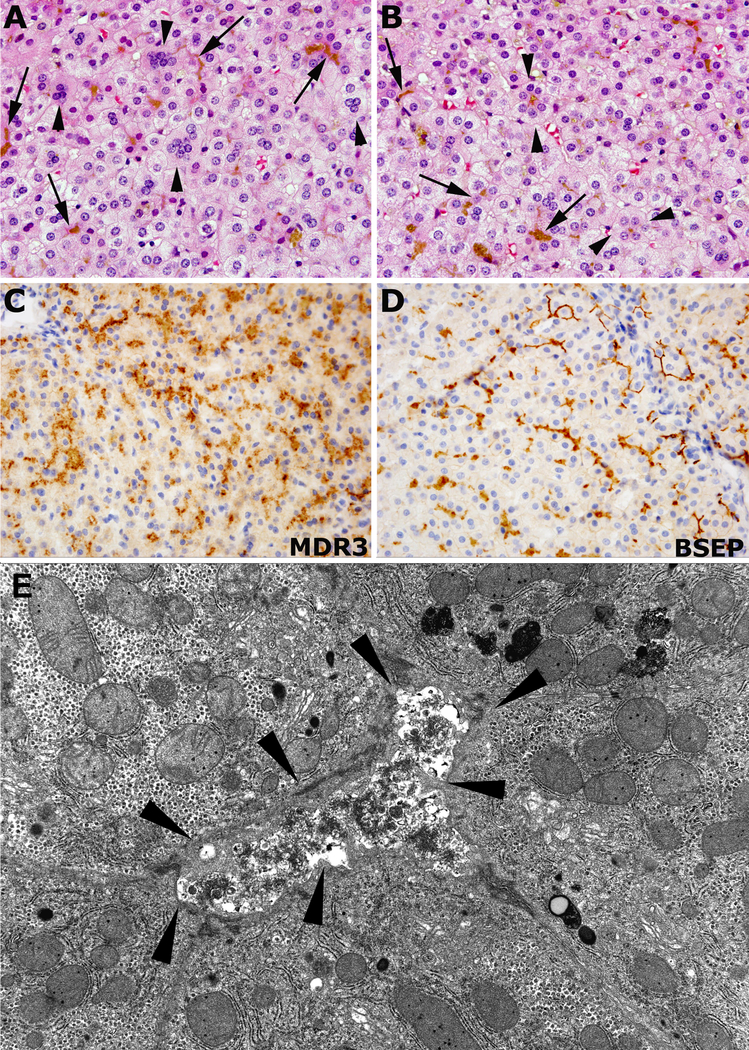
A PN-dependent 3-year-old male with MVID presented with a history of worsening jaundice and severe pruritus. He was managed at an outside institution with low dose soybean oil-based lipid emulsion (SOLE) Intralipid® (Fresenius-Kabi, Uppsala, Sweden) at 0.2 g/kg/day as a strategy to prevent PN-associated liver disease (PNALD). At 11 months of age he complained of significant pruritus without dermatologic findings. Ursodiol and diphenhydramine were administered with partial resolution. Bile acids (BA) levels at the time were elevated and returned to normal after cholestyramine therapy was started at age 2 (Table 1). A liver biopsy demonstrated cholestasis with isolated bile duct loss but no inflammation or fibrosis. Bile salt export pump staining was consistent with canalicular changes typically seen in MVID (Figure 1) (2).
Table 1.
Liver function tests and fatty acid values before and after initiation of fish oil-based lipid emulsion monotherapy.
| 30m Pre-FOLE | 18m Pre-FOLE | 1d Pre- FOLE | 1w Post-FOLE | 1m Post-FOLE | 3m Post-FOLE | 5m Post-FOLE | 7m Post-FOLE | 1y Post-FOLE | |
|---|---|---|---|---|---|---|---|---|---|
| Total bilirubin (mg/dl) | 1.7 | 0.3 | 10.5 | 9.4 | 4.9 | 1 | 0.8 | 0.6 | 0.4 |
| Direct bilirubin (mg/dl) | 1.1 | 0.1 | 7.8 | 6.1 | 3 | 0.2 | 0.2 | 0.1 | <0.2 |
| Serum bile acids (μmol/L) | 108 | 13 | 211 | 15 | |||||
| AST (U/L) | 65 | 40 | 197 | 70 | 101 | 119 | 41 | 41 | 54 |
| ALT (U/L) | 104 | 47 | 355 | 117 | 154 | 143 | 51 | 56 | 46 |
| GGT (U/L) | 10 | 7 | 8 | 14 | 31 | 20 | 14 | 15 | 14 |
| Alkaline phosphatase (U/L) | 716 | 552 | 521 | 525 | 217 | 219 | 254 | 227 | 130 |
| Alpha-linolenic acid (nmol/ml) | 11 | 95 | 71 | 94 | 47 | 20 | 23 | 21 | 27 |
| Linoleic acid (nmol/ml) | 571 | 1458 | 2548 | 2847 | 1690 | 744 | 659 | 618 | 569 |
| Eicosapentaenoic acid (nmol/ml) | 108 | 23 | 33 | 1155 | 1144 | 508 | 755 | 730 | 1294 |
| Docosahexaenoic acid (nmol/ml) | 68 | 100 | 349 | 2027 | 1432 | 541 | 748 | 695 | 1224 |
| Arachidonic acid (nmol/ml) | 641 | 494 | 970 | 1032 | 520 | 242 | 209 | 229 | 255 |
| Total ω-3 fatty acids (nmol/ml) | 0.1 | 0.22 | 0.45 | 3.28 | 2.62 | 1.07 | 1.53 | 1.45 | 2.54 |
| Total ω-6 fatty acids (nmol/ml) | 1.4 | 2.1 | 3.7 | 4 | 2.2 | 1 | 0.9 | 0.9 | 0.8 |
| ω-6:ω-3 ratio | 14 | 9.55 | 8.22 | 1.22 | 0.84 | 0.93 | 0.59 | 0.62 | 0.31 |
| Triene:Tetraene ratio | 0.097 | 0.113 | 0.029 | 0.011 | 0.008 | 0.004 | 0.005 | 0.009 | 0.008 |
Abbreviations: AST – aspartate aminotransferase; ALT – alanine aminotransferase; GGT – gamma-glutamyl transferase; FOLE – fish oil-based lipid emulsion.
Figure 1.
Representative images of core needle liver biopsies stained with hematoxylin and eosin, and immunohistochemistry performed at our institution. Diffuse hepatocellular damage with loss of the radial orientation of hepatocellular trabecules, multinucleated giant cells (arrowheads in A) and pseudoacinar transformation of hepatocytes (between arrowheads in B), and cytoplasmic and canalicular cholestasis (arrows in A and B). MDR3 (C) and BSEP (D) immunohistochemistry showing thickened and granular reactivity along the canaliculi (in brown color). Representative image of the ultrastructure of the core needle liver biopsy performed at outside institution showing a distended canaliculus (between arrowheads), with luminal osmophilic granular bile and microvillous effacement (E). Abbreviations: BSEP – bile salt export pump.
At 3 years of age the pruritus became severe leading to significant disruptions in his quality of life. Additional failed medications included rifampicin, hydroxyzine, and naltrexone. Over the following weeks he developed worsening jaundice and rising bilirubin levels. The patient was transferred to our institution where treatment with the FOLE Omegaven® (Fresenius Kabi, Bad Homburg, Germany) at 1 g/kg/day was initiated for presumed PNALD. There was no family history of liver disease. He appeared ill with scleral icterus, jaundiced skin with multiple excoriations, and fragile gray-colored hair. There were no signs of portal hypertension. Laboratory studies demonstrated direct hyperbilirubinemia with transaminitis and elevated BA (Table 1). An abdominal ultrasound revealed a normal liver size and no bile duct dilatation. A core needle liver biopsy was suggestive of PNALD (Figure 1).
The cholestasis and pruritus improved steadily beginning 2 weeks after FOLE initiation and completely resolved. The patient’s quality of life continued to improve. Jaundice resolved and BA and direct bilirubin levels normalized. The patient continued to do well after one year on FOLE without pruritus.
DISCUSSION
Many MYO5B gene mutations associated with MVID affect biliary function and present similarly to some types of progressive familial intrahepatic cholestasis with intermittent jaundice, pruritus, elevated serum BA and normal gamma-glutamyl transferase levels, as seen in this patient (1,2). Interestingly, he had pruritus for most of his life, even in the presence of normal liver enzymes and bilirubin.
The manifestation of liver disease in patients with the MYO5B mutation may be influenced by genetic, epigenetic, and/or environmental factors (3). Patients with MVID are thus predisposed to suffer from the hepatotoxic effects of SOLE. The inflammatory (or lack thereof) properties of omega-3 fatty acids (O3FA) in fish oil (FO) justify its efficacy in some inflammatory conditions. O3FA are precursors to leukotrienes and prostaglandins which are less pro-inflammatory than those derived from omega-6 fatty acids. The local shift in predominating polyunsaturated fatty acids alters the amount of leukotrienes and recruitment of inflammatory leukocytes to the skin. FO-supplemented animals have a higher “leukotriene inhibition potential” which affects the amounts of epidermal anti-inflammatory molecules (4).
FOLE therapy not only proved beneficial in the resolution of cholestasis, but also reduced the levels of BA and eradicated the pruritus. Similar to the efficacy of FOLE in treating PNALD, it seems likely that the resolution of symptoms for this case is multifactorial and we hypothesize that it was due to (1) resolution of cholestasis; (2) shift in epidermal inflammatory properties induced by O3FA present in FO; and (3) reduction in circulating pruritogenic BA. Properties of FOLE make it an option for treating intractable pruritus in patients with PNALD and MVID.
List of Abbreviations
- MVID
microvillous inclusion disease
- PN
parenteral nutrition
- FOLE
fish oil-based lipid emulsion
- SOLE
soybean oil-based lipid emulsion
- PNALD
parenteral nutrition-associated liver disease
- BA
bile acids
- O3FA
omega-3 fatty acids
- FO
fish oil
REFERENCES
- 1.Girard M, Lacaille F, Verkarre V, Mategot R, Feldmann G, Grodet A, et al. MYO5B and bile salt export pump contribute to cholestatic liver disorder in microvillous inclusion disease. Hepatology. 2014. July;60(1):301–10. [DOI] [PubMed] [Google Scholar]
- 2.Gonzales E, Taylor SA, Davit-Spraul A, Thébaut A, Thomassin N, Guettier C, et al. MYO5B mutations cause cholestasis with normal serum gamma-glutamyl transferase activity in children without microvillous inclusion disease. Hepatology. 2016;65(1):164–73. [DOI] [PubMed] [Google Scholar]
- 3.Qiu Y-L, Gong J-Y, Feng J-Y, Wang R-X, Han J, Liu T, et al. Defects in myosin VB are associated with a spectrum of previously undiagnosed low γ-glutamyltransferase cholestasis. Hepatology. 2017. May;65(5):1655–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller CC, Tang W, Ziboh VA, Fletcher MP. Dietary supplementation with ethyl ester concentrates of fish oil (n-3) and borage oil (n-6) polyunsaturated fatty acids induces epidermal generation of local putative anti-inflammatory metabolites. J Invest Dermatol. 1991. January;96(1):98–103. [DOI] [PubMed] [Google Scholar]