Abstract
Background
Research demonstrates strong associations between adverse childhood experiences (ACEs) and non-medical prescription opioid use (NMPO), but pathways are not understood, hindering prevention and treatment responses.
Methods
We assessed hypothesized mediators of the association between ACEs and NMPO in a nationally-representative U.S. sample. National Longitudinal Study of Adolescent to Adult Health data (N=12,288) yielded an ordinal exposure comprising nine ACEs (neglect; emotional, physical, sexual abuse; parental incarceration and binge drinking; witnessed, threatened with, experienced violence) and a binary lifetime NMPO outcome. Nine potential mediators measured in adolescence and/or adulthood included depression, anxiety, suicidality, delinquency, impulsivity, and risk-taking. We estimated adjusted odds ratios (AOR) and 95% confidence intervals (CI) for sex-stratified associations of: ACEs and mediators; mediators and NMPO; and ACEs and NMPO adjusting for mediators individually and simultaneously.
Results
All associations of ACEs and mediators were statistically significant and similar by sex. All mediators had statistically significant associations with NMPO (except one depression measurement for each sex). Delinquency was strongly associated with ACEs and NMPO and was the strongest individual mediator. Every ACE increase was associated with increased NMPO odds of 32% for males and 27% for females. Adjusting for all mediators, odds of NMPO were attenuated partially for males [AOR=1.18 (95% CI:1.07, 1.31)] and somewhat more for females [AOR=1.11 (95% CI:1.00, 1.25)].
Conclusions
Internalizing and externalizing factors partially explained the pathway from ACEs to NMPO. Substance abuse may be more difficult to treat with co-occurring psychopathologies and maladaptive behaviors, highlighting the need to address trauma early in life.
Keywords: Adverse childhood experiences, prescription opioid misuse, adolescent health, mental health, delinquency
1. Introduction
The opioid epidemic in the United States is well-documented, and by many metrics, worsening. Drug overdose is now the leading cause of death from unintentional injury, and most involve opioids (Rudd). Evidence is emerging that most people who use illicit opioids such as heroin first misused prescription opioids (Mateu-Gelabert et al., 2015; Surratt et al., 2017; Lankenau et al., 2012; Cerda et al., 2015; Banergee et al., 2016); therefore, transition to more addictive and potent opioids and high-risk behaviors such as injection amplify this public health crisis. High prevalence of non-medical prescription opioid (NMPO) use among young people (SAMHSA, 2015; Maxwell, 2015) highlights both the imperative to understand risk factors for initiation and the opportunity to strengthen prevention efforts and mitigate morbidity and mortality by intervening early in life.
Limited but compelling research demonstrates a strong association between adverse childhood experiences (ACEs) and NMPO use (Quinn et al., 2016; Lawson et al., 2013; McCauley et al., 2010; Conroy et al., 2009; Sansone et al., 2009). While there was a recent call for substance abuse prevention and treatment programs to reflect the needs of those with a history of trauma (Press et al., 2017), the pathways from trauma to NMPO are not yet understood, hindering the ability to formulate optimal programmatic responses. Neuroscience suggests that ACEs may lead to physiological processes that disrupt early development of the central nervous system, diminish ability to cope with emotions (Perry and Pollard, 1998), and lead to impaired emotional and behavioral self-regulation over the life course (Dunn et al., 2017; van der Kolk et al., 1991). Individuals may self-medicate with substances to cope with the dysregulated stress response (Dworkin et al, 2017; McHugh et al., 2017; Khantzian, 1985).
Hypotheses about potential pathways from trauma to NMPO use are informed by extant research on the relationships between: 1. trauma and internalizing and externalizing factors; and 2. internalizing and externalizing factors and substance misuse. “Internalizing problems are inner-directed, and refer to problems that generate unease, tension, and suffering in the individual…and group together syndromes such as depression, anxiety, social isolation, or somatic complaints.” (Forns, Abad, and Kirchner, 2011). “Externalizing problems are outer-directed and generate discomfort and conflict in other people and imply disregard of social norms…and group together syndromes such as aggressiveness and delinquency or rule-breaking behavior…” (Forns). Early life trauma is associated throughout the life course with depressive disorders, anxiety disorders, post-traumatic stress disorder (PTSD), and suicidality (Khoury et al., 2010; Felitti et al., 1998; Weber et al., 2008; de Venter et al., 2013; Dube et al., 2001; Mirhashim et al., 2017) and delinquency, risk taking, sensation seeking, and impulsivity (Cannon et al., 2016; Felitti et al., 1998; Bornovalova et al., 2008; Dube et al., 2001; MacMillan et al., 2001; Mirhashim et al., 2017). In turn, internalizing and externalizing disorders are associated with a broad range of substance use outcomes, including opioid misuse (Khoury et al., 2010; Dube et al., 2002; Dube et al., 2003; Edlund et al., 2015; Feldstein and Miller, 2006; Crews and Boettiger, 2009).
Since limited research has examined the influence of ACEs on NMPO use, very few studies have investigated mediators of the relationship with NMPO use explicitly. A study of 84 individuals with a history of ACEs and heroin or NMPO use found emotional abuse, but not other forms, to be associated with PTSD, PTSD to be associated with opioid misuse (Mirhashem et al., 2017). Another small study found the association of ACEs and alcohol, cocaine or opioid dependence) to be partially mediated by mood and anxiety disorders, but externalizing factors were not assessed (Douglas et al., 2010). A study of women found that in middle adulthood, PTSD, stressful life events, and delinquent and criminal behavior were independent mediators of the relationship between ACE and substance misuse, but when assessed together, only stressful life events for substance use problems and only PTSD for illicit drug use remained mediators (White and Widom, 2008). Studies suggest differences in mediators and their effects between females and males (Dube et al., 2001; MacMillan et al., 2001; Khoury et al., 2010), highlighting a need to further explore the role of sex given hypothesized sex differences in internalizing and externalizing sequelae of trauma and coping strategies.
We hypothesize that childhood trauma’s impact on psychological health throughout life leads to NMPO initiation to manage long-term sequelae. This analysis examines the roles of potential mediators of the relationship of ACEs and lifetime NMPO use with data from The National Longitudinal Study of Adolescent to Adult Health (Add Health) described at http://www.cpc.unc.edu/projects/addhealth (accessed October 18, 2017). We contribute to knowledge of drivers of the opioid epidemic in several ways: 1) This mediation analysis builds on findings of a strong dose-response relationship between childhood trauma load and initiation of NMPO use in emerging and early adulthood in this nationally-representative sample (Quinn et al., 2016); 2) We examine potential internalizing and externalizing factors not measured in other nationally-representative studies; 3) The main exposure is informed by a comprehensive perspective of childhood adversity that includes nine types of abuse, household dysfunction, and violence and allows us to estimate the cumulative effect of multiple types of experiences; and 4) We explore sex differences in important mediators. Results may be used to refine evidence-based prevention and treatment strategies for addressing NMPO use early in life and interrupting the transition to initiation and injection of illicit opioids.
2. Material and Methods
2.1. Study population and design
We analyzed Add Health data from a U.S. nationally-representative, stratified, random survey sample of 20,745 middle and high school students. Retention was high -- approximately 80% across the waves of data collection -- and analyses indicate that the magnitude of bias due to attrition is small, especially when appropriate sample weights are used (Harris, 2013, Carolina Population Center). Our analytic sample, described elsewhere in detail (Quinn et al., 2016), included 12,228 participants in the restricted-use dataset who had sample weights at Waves I, III and IV, representing adolescence (11-21 years), emerging adulthood (18-28 years), and adulthood (24-34 years) in our analyses. We characterized the relationships between number of ACEs and lifetime NMPO use, first adjusting for sociodemographic covariates and then adjusting for internalizing and externalizing factors in adolescence and adulthood to identify factors that may mediate the pathway from ACEs to NMPO use. We stratified all analyses by sex.
2.2. Variables
2.2.1. ACE exposures
Using Waves I, III and IV data, we created nine dichotomous measures of self-reported (except parent-reported binge drinking) adverse experiences occurring before age 18, defined as: neglect (left alone when adult should have been present and/or basic needs unmet ≥six times); emotional abuse (caregiver said hurtful things feelings or made child feel unloved ≥six times); physical abuse (slapped, hit, kicked, or thrown by caregiver ≥six times); sexual abuse (caregiver touched child or forced child to touch him/her in sexual way); parental incarceration (parent/parent figure spent time in jail or prison); witnessed violence (saw shooting or stabbing); threatened with violence (knife or gun on pulled on child); experienced violence (child shot or cut/stabbed); and parental binge drinking (≥five drinks on one occasion in past month). We summed the nine traumas to create an ordinal ACE score with a range of 0 to 4 or more ACEs (due to sparse data in the higher range). Analyses included only cases with no missing data for all nine ACEs (n=9,569). We conducted sensitivity analyses in prior work to compare associations of ACEs and NMPO (Quinn et al., 2016) as well as other drug use (e.g., marijuana and cocaine) (Scheidell et al., 2017) in this subsample with those in the full sample and found no meaningful differences that would change our interpretation of the associations; therefore, we continue to present conservative estimates for only the sample with complete ACE data.
2.2.2. NMPO use outcome
We used data from the Wave IV survey question, “Have you ever taken any prescription drugs that were not prescribed for you, taken prescription drugs in larger amounts than prescribed, more often than prescribed, for longer periods than prescribed, or taken prescription drugs that you took only for the feeling or experience they caused?” and coded all respondents reporting having ever used “pain killers or opioids such as Vicodin, Oxycontin, Percocet, Demerol, Percodan, or Tylenol with codeine” in the follow-up question as lifetime NMPO use.
2.2.3. Sociodemographic covariates
Adjusted models included self-report data to control for: ordinal age at Wave I; race/ethnicity (non-Hispanic white (referent), non-Hispanic black, Hispanic, other) at Wave I; and a proxy measure of poverty defined as concern about paying bills at Wave I (parent-reported, yes vs. no). Poverty at Wave III and educational attainment at Wave IV were not significantly associated with NMPO and were excluded. We stratified all analyses by male or female sex reported at Wave I.
2.2.4. Potential mediators
We evaluated nine variables hypothesized to be influenced by the experience of trauma and to increase risk of opioid initiation. All were created from self-report data and coded as binary variables with the referent group reflecting the absence of the mediator or the more optimal psychological health level. We hereafter refer to two groups of mediators as “internalizing” and “externalizing” factors.
We assessed five potential internalizing factors as mediators. Depressive symptoms were measured at Waves I, III, and IV using 9 items common across Waves from the CES-D (Center for Epidemiologic Studies-Depression) scale with a range of 0 to 27 representing the experience or feeling never or rarely to most or all of the time during the past week. The depression variables were coded as high (>=10) vs. low (<10). Anxiety symptoms comprised seven Wave I questions about experiences during the past year (upset stomach, cold sweats, dizziness, trouble sleeping, trouble relaxing, moodiness, and fearfulness). We used the 75th percentile cutoff of 1 to create a variable reflecting any anxiety symptom vs. none. Suicidality was from a Wave III yes or no question: “During the past 12 months, have you ever seriously thought about committing suicide?”
Four potential externalizing factors mediators were defined as follows. We created delinquency variables for Waves I and III from 7 items (stole <$50, stole>$50, damaged property, burglarized, sold drugs, used or threatened someone with a weapon, participated in a group fight), with one or more considered delinquent (vs. none) as used in previous research (Aalsma et al., 2010). Risk taking was a Wave III attitudinal question, “Do you agree or disagree that you like to take risks?” with answers coded as strongly agree or agree vs. neither or disagree or strongly disagree. Six items representing impulsivity at Wave III had the preface, “How true do you think the following is of you?” and the 5 response choices included not, a little, somewhat, pretty, and very true. Items included: 1. I often try new things just for fun or thrills, even if most people think they are a waste of time; 2. I can usually get people to believe me, even when what I’m saying isn’t quite true.3. I like it when people can do whatever they want, without strict rules and regulations; 4. I often follow my instincts, without thinking through all the details; 5. I can do a good job of “stretching the truth” when I’m talking to people; 6. I change my interest a lot, because my attention often shifts to something else. The higher level of impulsivity for each item included the two highest levels of agreement. Six items were summed, and the final variable used a cutoff of two (75th percentile) to dichotomize respondents as high vs. low impulsivity.
2.3. Analytical strategy
We used survey procedures in SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA) to account for the complex survey sample design and logistic regression to explore the main association of number of ACEs and lifetime NMPO by estimating unadjusted (OR) and adjusted odds ratios (AOR) and 95% confidence intervals (CI) for NMPO (ever vs. never). We conducted bivariable analyses to identify sociodemographic covariates for adjustment by estimating ORs for the association between each potential covariate and NMPO in the full sample (results not shown). If the sociodemographic variable had a statistically significant association at the p=0.05 level with NMPO use, we included it in stratified analyses.
We based our mediation analysis on the causal steps approach (Baron and Kenny, 1986) to identify mediators and assess their contributions to the relationship between number ACEs and NMPO use. Recent work has expanded this classic strategy by incorporating the counterfactual framework and allowance for non-linear models (Robins et al., 1992; Van der Weele and Vansteelandt, 2009, 2010). We first estimated the sex-stratified associations of ACE score, unadjusted and adjusted only for sociodemographic covariates, with each of nine hypothesized mediators. We then estimated the ORs and AORs for each potential mediator’s relationship with NMPO use, again in sex-stratified models. In the mediation models, we included all potential mediators that were significantly associated with both ACE score and NMPO use and sociodemographics. We examined correlation coefficients and alphas for all mediator relationships to ensure that highly correlated variables were not simultaneously included.
The total effect is represented by the estimate from the model including only number of ACEs and sociodemographics (no mediators) to predict NMPO use, which is then compared with mediation model results to estimate the direct effect, the portion of the total effect not due to the mediator. We conducted a series of multivariable logistic regressions to estimate the AOR for the ACE and NMPO association when each mediator was included singly (adjusted only for sociodemographics). The male and female mediation models each assessed eight mediators, though a different mediator was omitted for each sex based on not satisfying the a priori criteria (aforementioned steps 1 and 2) for a potential mediator. Final models included eight mediators each for females and males, also adjusted for sociodemographics.
We evaluated the strength of the association between number of ACEs and NMPO use by the magnitude of the AOR and the width of the CI. In this manner, we compared AORs across the models to evaluate their relative importance as mediators from ACEs to NMPO.
3. Results
3.1. Sociodemographic covariates
Bivariable associations of sociodemographics and NMPO use show that for males, only race/ethnicity was a strong predictor of NMPO; non-Hispanic blacks and Hispanics had 82% and 55% lower odds of NMPO, respectively, than non-Hispanic whites. Similarly, for females, all three race/ethnicity groups had much lower odds of NMPO relative to non-Hispanic whites. For females only, poverty was a strong predictor; those in the higher poverty group had 83% higher odds of NMPO. Though the associations were not statistically significant, for both sexes, odds of NMPO use were lower with increasing age (Table 1). All three variables were included in multivariable models since they were predictive in the non-stratified sample.
Table 1.
Associations of sociodemographic covariates and hypothesized mediators with lifetime non-medical prescription opioid (NMPO) use, by sex (N=12,274)
| Odds of NMPO use (referent=never used) | ||||||
|---|---|---|---|---|---|---|
| Males (N=5,596) | Females (N=6,678) | |||||
| Percent NMPO | OR (95% CI) | AOR (95% CI)* | Percent NMPO | OR (95% CI) | AOR (95% CI)* | |
| Total sample | 17.91 | NA | NA | 12.29 | NA | NA |
| Sociodemographic covariates | ||||||
| Race/ethnicity | ||||||
| White non-Hispanic | 22.07 | -- | 15.34 | -- | ||
| Black non-Hispanic | 4.71 | 0.18 (0.12, 0.26) | NA | 3.38 | 0.19 (0.13, 0.30) | NA |
| Hispanic | 11.39 | 0.45 (0.33, 0.64) | 8.79 | 0.53 (0.36, 0.80) | ||
| Other | 19.67 | 0.87 (0.59, 1.27) | 9.50 | 0.58 (0.37, 0.90) | ||
| Age (Wave I) | ||||||
| 11-13 | 19.28 | -- | 13.57 | -- | ||
| 14-16 | 19.07 | 0.99 (0.72, 1.35) | NA | 14.56 | 1.09 (0.72, 1.64) | NA |
| 17-18 | 16.60 | 0.83 (0.60, 1.15) | 9.18 | 0.64 (0.41, 1.02) | ||
| 19-21 | 14.18 | 0.69 (0.42, 1.15) | 7.66 | 0.53 (0.78, 1.01) | ||
| Poverty (Wave III) | ||||||
| Yes | 20.58 | 1.20 (0.90, 1.60) | NA | 18.49 | 1.83 (1.43, 2.34) | NA |
| No | 17.72 | -- | 11.06 | -- | ||
| Internalizing factors | ||||||
| Depression (Wave I) | ||||||
| High | 22.84 | 1.41 (1.06, 1.89) | 1.53 (1.14, 2.07) | 13.48 | 1.14 (0.92, 1.42) | 1.19 (0.95, 1.50) |
| Low | 17.33 | -- | -- | 12.00 | -- | -- |
| Depression (Wave III) | ||||||
| High | 19.99 | 1.15 (0.84, 1.59) | 1.20 (0.86, 1.66) | 18.85 | 1.83 (1.42, 2.37) | 1.90 (1.47, 2.46) |
| Low | 17.82 | -- | -- | 11.24 | -- | -- |
| Depression (Wave IV) | ||||||
| High | 22.26 | 1.36 (1.04, 1.78) | 1.56 (1.20, 2.04) | 19.84 | 2.05 (1.63, 2.58) | 2.09 (1.63, 2.68) |
| Low | 17.36 | -- | -- | 10.77 | -- | -- |
| Anxiety (Wave I) | ||||||
| High | 23.52 | 1.62 (1.30, 2.03) | 1.59 (1.27, 2.00) | 15.33 | 1.55 (1.24, 1.93) | 1.42 (1.14, 1.78) |
| Low | 15.93 | -- | -- | 10.48 | -- | -- |
| Suicidality (Wave III) | ||||||
| Yes | 32.16 | 2.36 (1.74, 3.20) | 2.10 (1.54, 2.87) | 29.87 | 3.45 (2.56, 4.66) | 3.15 (2.31, 4.29) |
| No | 16.75 | -- | -- | 10.99 | -- | -- |
| Externalizing factors | ||||||
| Risk taking (Wave III) | ||||||
| Yes | 14.43 | 1.48 (1.21, 1.82) | 1.43 (1.17, 1.74) | 19.75 | 1.44 (1.20, 1.72) | 1.42 (1.18, 1.72) |
| No | 10.51 | -- | -- | 14.23 | -- | -- |
| Impulsivity (Wave III) | ||||||
| High | 22.22 | 1.97 (1.59, 2.46) | 1.87 (1.49, 2.35) | 17.16 | 1.90 (1.60, 2.26) | 1.81 (1.52, 2.17) |
| Low | 12.64 | -- | -- | 9.83 | -- | -- |
| Delinquency (Wave I) | ||||||
| High | 32.32 | 2.03 (1.65, 2.50) | 2.09 (1.69, 2.58) | 24.30 | 2.38 (1.95, 2.91) | 2.39 (1.95, 2.93) |
| Low | 13.04 | -- | -- | 11.57 | -- | -- |
| Delinquency (Wave III) | ||||||
| High | 24.30 | 2.45 (2.02, 2.98) | 2.46 (2.00, 3.02) | 22.23 | 2.21 (1.79, 2,72) | 2.16 (1.75, 2.68) |
| Low | 11.57 | -- | -- | 12.64 | -- | -- |
OR: odds ratio; AOR: adjusted odds ratio; CI: confidence interval; NA: not applicable
Adjusted for age, race/ethnicity, and poverty
3.2. Associations of ACEs and mediators
Prevalence of nine mediators differed by sex, with females having higher prevalence of the higher mediator category for the depression and anxiety symptoms while males had higher prevalence for risk taking, impulsivity, and delinquency. Suicidality prevalence was similar by sex. Nonetheless, the unadjusted and adjusted associations of ACEs with all mediators were statistically significant and of similar strength for males and females. For all three depression mediators, every increase of one ACE was associated with 30-38% increased odds of being in the high depression group for both sexes. The associations for anxiety and suicidality were slightly stronger for females than males, and while these two mediators had similarly strong associations for males, the suicidality association for females was somewhat higher. Associations for risk taking and impulsivity were nearly identical by sex; every increase in ACE number was associated with about 10% increased odds of risk taking and 20% increased odds of impulsivity. For males and females, delinquency in adolescence had the strongest associations with ACEs of all mediators; ACE score was associated with 57% and 49% increased odds of delinquency, respectively. For males and females, ACE’s predictive strength for delinquency in emerging adulthood was considerably weaker than delinquency in adolescence [AOR males=1.26(95% CI:1.16, 1.36)], [AOR females=1.20(95% CI:1.12, 1.29)].
3.3. Associations of hypothesized mediators and NMPO use
While males had higher prevalence of lifetime NMPO use (18%) than females (12%), all mediators had statistically significant associations with NMPO use in unadjusted and adjusted models for males and females, and the strength of association was similar by sex in most cases (Table2). The notable exception is depression; Wave III depression for males and Wave I for females were not predictive of NMPO. These results are somewhat surprising given that Wave III depression was associated with 83% higher odds for females and Wave I depression was associated with 55% higher odds for males in adjusted models. Wave IV depression was associated with 56% increased odds for males and more than twice the odds of NMPO for females. Anxiety was associated with roughly 50% higher odds of NMPO for both sexes. Suicidality had the strongest association with NMPO; males had more than twice the odds and females more than three times the odds of NMPO. Risk taking was a moderately strong predictor, associated with more than 40% increased odds for both sexes, while impulsivity was a stronger predictor, associated with 87% and 81% increased odds for males and females, respectively. Delinquency was a very strong predictor of NMPO for both sexes at both Waves I and III, associated with more than twice the odds of NMPO. For males, the association measured by the Wave III variable in emerging adulthood [AOR=2.46(95% CO:2.00, 3.02)] was about 18% higher than for the adolescence measure. Conversely, for females, delinquency in emerging adulthood was associated with about a 10% decrease in odds relative to the association in adolescence [AOR=2.39(95% CI:1.95, 2.93)].
Table 2.
Associations of childhood adverse experiences and hypothesized mediators, by sex (N=9,569)
| Odds of high level of mediator associated with every increase of 1 trauma versus no/low level of mediator | ||||||
|---|---|---|---|---|---|---|
| Males (N=4,295) | Females (N=5,274) | |||||
| % high level of mediator | OR (95% CI) | AOR (95% CI)* | % high level of mediator | OR (95% CI) | AOR (95% CI)* | |
| Internalizing factors | ||||||
| Depression (Wave I) | 12.38 | 1.43 (1.28, 1.60) | 1.38 (1.24, 1.55) | 21.76 | 1.42 (1.31, 1.54) | 1.38 (1.28, 1.49) |
| Depression (Wave III) | 8.19 | 1.35 (1.20, 1.51) | 1.32 (1.17, 1.49) | 14.19 | 1.44 (1.33, 1.54) | 1.37 (1.28, 1.47) |
| Depression (Wave IV) | 11.45 | 1.34 (1.22, 1.47) | 1.30 (1.17, 1.44) | 16.93 | 1.43 (1.32, 1.54) | 1.36 (1.25, 1.48) |
| Anxiety (Wave I) | 26.15 | 1.27 (1.18, 1.37) | 1.28 (1.19, 1.38) | 37.65 | 1.38 (1.30, 1.47) | 1.38 (1.30, 1.47) |
| Suicidality (Wave III) | 6.34 | 1.27 (1.23, 1.42) | 1.27 (1.13, 1.44) | 7.06 | 1.48 (1.32, 1.67) | 1.47 (1.30, 1.66) |
| Externalizing factors | ||||||
| Risk taking (Wave III) | 19.75 | 1.09 (1.02, 1.78) | 1.10 (1.02, 1.19) | 14.23 | 1.10 (1.04, 1.16) | 1.10 (1.04, 1.17) |
| Impulsivity (Wave III) | 54.88 | 1.20 (1.11, 1.29) | 1.21 (1.13, 1.31) | 33.71 | 1.24 (1.17, 1.32) | 1.22 (1.15, 1.30) |
| Delinquency (Wave I) | 48.26 | 1.57 (1.45, 1.70) | 1.57 (1.45, 1.70) | 32.98 | 1.52 (1.42, 1.62) | 1.49 (1.39, 1.59) |
| Delinquency (Wave III) | 50.18 | 1.25 (1.15, 1.36) | 1.26 (1.16, 1.36) | 29.62 | 1.23 (1.15, 1.32) | 1.20 (1.12, 1.29) |
OR: odds ratio; AOR: adjusted odds ratio; CI: confidence interval
Adjusted for age, race/ethnicity, and poverty
3.4. Multivariable models to identify mediators of ACE’s association with NMPO use
Correlation coefficients among the mediators were low (0.01 to 0.22) for almost all variables. Wave I depression and anxiety (alpha=0.35) and Waves III and IV depression (alpha=0.25) were moderately correlated; however, based on null associations with NMPO use, depression at Wave I (for females) and Wave III (for males) were omitted, resulting in eight mediators in each final model.
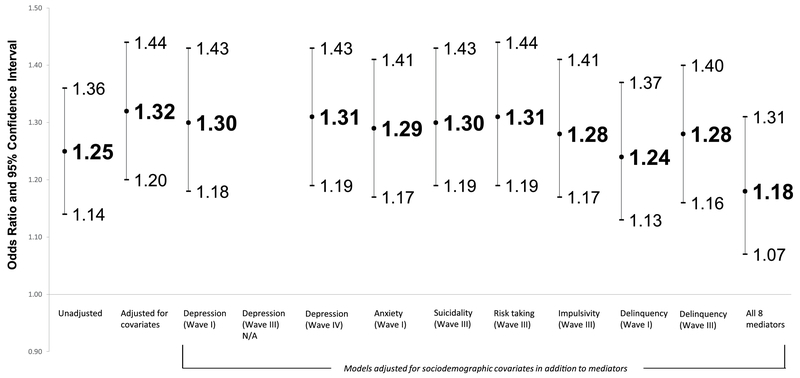
3.4.1. Males
Figure 1 shows the unadjusted and adjusted associations of ACE score and NMPO for males. The AOR adjusted for sociodemographics was 1.32(95% CI:1.14, 1.36). In eight individual mediator models, adjusted for sociodemographics and only a single mediator per model, mediation was relatively weak. The strongest mediator was delinquency at Wave I, which decreased the main association to 1.24(95% CI: 1.13,1.37), and the weakest mediators were Wave IV depression [AOR=1.31(95% CI:1.19, 1.43)] and risk taking [AOR=1.31(95% CI:1.19, 1.44)]. In the fully-adjusted model, the association of ACEs and NMPO was attenuated substantially [AOR=1.18(95% CI:1.07, 1.31)], suggesting that the mediators account for most but not all of the pathway from ACEs to NMPO.
Figure 1.
Associations of childhood trauma and non-medical prescription opioid use with and without adjustment for hypothesized mediators among MALES (N=4,295)
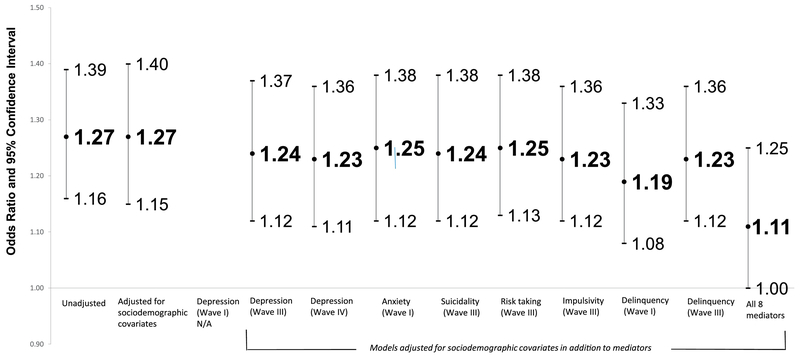
3.4.2. Females
Figure 2 shows the unadjusted and adjusted associations of ACEs and NMPO for females. The AOR adjusted only for sociodemographics is smaller than for males, 1.27(95% CI:1.15, 1.40). Among the eight individual mediator models, mediation was again relatively weak. The strongest mediator was delinquency at Wave I, as it was for males, which decreased the main association to 1.19(95% CI:1.08, 1.33). The weakest mediators were anxiety [AOR=1.23(95% CI:1.12, 1.38)] and as for males, risk taking [AOR=1.23 (95% CI: 1.13, 1.38)]. The final mediation model suggests somewhat stronger mediation for females and yielded a now nearly null association of ACE score and NMPO [AOR=1.11(95% CI:1.00, 1.25)].
Figure 2.
Associations of childhood trauma and non-medical prescription opioid use with and without adjustment for hypothesized mediators among FEMALES (N=5,274)
4. Discussion
This analysis made novel use of the Add Health dataset to advance our understanding of potential internalizing and externalizing factors that mediate the influence of trauma in childhood on NMPO use. Depression, anxiety, suicidality, delinquency, impulsivity, and risk-taking explained some, but not all, of the path from adversity to NMPO use. A history of even one ACE predicted moderately increased odds of multiple negative internalizing and externalizing factors. These results are aligned with numerous studies that have demonstrated that children exposed to trauma are more likely to have various types of psychiatric illness and more physical symptoms and to engage in more health-risk behaviors than their non-abused counterparts (Arnow, 2004).
Findings underscore calls to address undiagnosed, untreated psychological and behavioral issues among those with a history of trauma as a public health priority (Malvaso et al., 2015; Fox et al., 2015; Plotzker et al., 2007). Delinquency was a strong and consistent mediator across the adolescent and young adult life course. Early identification of and intervention among youth who commit delinquent acts or are at risk of initiating such behaviors may prevent development of antisocial tendencies and in turn addiction risk. The trauma-informed program TARGET (https://www.samhsa.gov/nctic/trauma-interventions, (accessed October 18, 2017) for youth in juvenile justice settings and at-risk youth in community settings aims to reduce trauma-related impacts on affect regulation by providing a skill set to youth and families to regulate extreme emotional states and encourage clear thinking in the context of stress (Ford and Hawke, 2012). We need rigorous program evaluation to understand the influence on downstream adverse outcomes such as adulthood NMPO use.
Most other hypothesized mediators, though associated with ACEs and with NMPO use, were found to weakly mediate the ACE-NMPO relationship when assessed individually. In models adjusting for potential mediators simultaneously, the association was fully attenuated among females and partially attenuated among males, suggesting internalizing and externalizing factors work in tandem. Addressing any one factor would likely not be sufficient to interrupt a trajectory of risk that leads to NMPO use. Partial attenuation of the ACE-NMPO use association among males highlights the need for qualitative and quantitative research to identify the paths linking trauma to NMPO use risk. This is particularly important given the higher NMPO prevalence observed among males in these nationally-representative data and our emerging understanding of the role of NMPO in the trajectory to heroin use.
Additional noteworthy sex differences emerged. The final sex-stratified mediation models contained nearly identical mediator variables since all but one variable each for females and males met criteria in the first steps of the causal approach. It appears, however, that the relationship between trauma and depression differs over the life course by sex. The relationship is stronger for males in adolescence and weaker in adulthood than for females. On the other hand, delinquency was an important mediator for both sexes across both adulthood waves, in conflict with historical conceptualizations that young males are more likely than females to develop externalizing factors and practice maladaptive behaviors in response to adversity. Better understanding of internalizing versus externalizing symptoms and sex-related coping strategies, and their timing in the developmental process, must inform interventions for trauma-exposed individuals.
We observed a strong relationship between number of different ACEs and lifetime NMPO use among males and females, consistent with our previous analyses exploring a dose-response relationship in this nationally-representative population (Quinn et al., 2016), and other studies suggesting that the trauma load during stress-sensitive childhood negatively affects well-being (Kaysen et al.; 2009, Khoury et al., 2010; Neuner et al., 2004; Weber et al., 2008). Every increase of one ACE was associated with 32% higher odds of NMPO use for males and 24% for females. The prevalence of illicit drug use is high among adolescents and young adults, in part due to easy availability and experimentation in the course of normal development (SAMHSA). The possibility that youth exposed to acute and chronic adversity face additional risk of drug initiation underscores the urgency of understanding pathways.
Harmful prescribing of opioids has been a primary prevention focus of the epidemic, but understanding upstream risk factors and pathways is critical to weighing potential harms and benefits of prescription opioids. Evidence-based programs such as Seeking Safety that mitigate trauma’s effects by promoting coping skills and self-care can be instrumental in identification and treatment of mental health problems. Given the strong relationships between trauma and psychological issues and between psychological issues and NMPO use, we must prioritize integrating behavioral health and prevention interventions.
We note the following limitations. We used three waves of data from a longitudinal cohort study spanning almost 25 years. The majority of mediators represented emerging adulthood, and therefore likely occurred after childhood events, but we cannot ascertain the exact or relative timing of ACEs, mediators, or lifetime NMPO use. Prevalence of lifetime NMPO use among high school seniors in the U.S. was low, about 6-7%, in 1994-95 when the cohort of our analysis were adolescents, according to Monitoring the Future data (McCabe, et al., 2017)). The mean age at initiation of NMPO was 16.8 years in a study of opioid users aged 18-29 in New York City; age at initiation in the general population is likely much higher (Mateu-Gelebert, et al., 2015). Most NMPO use was likely to have occurred in emerging or early adulthood in our sample and therefore after exposure to most ACEs. This analysis represents an advance relative to cross-sectional studies. We acknowledge the challenges of collecting accurate self-report data on sensitive topics such as childhood events, illicit drug use, and psychological and behavioral factors.
The causal approach of examining change in estimates to infer mediation requires several assumptions that are often unmet. Direct effect estimates may be biased because of unmeasured confounding of the mediator-outcome relationship (Kaufman and Cooper, 2001); challenges inherent in measuring complex psychological factors likely caused residual confounding. Relatively low NMPO prevalence suggests that OR estimates are good approximations of risk ratios; however, the non-collapsibility of ORs warrants caution in comparing estimates for males and females (Valeri and Van der Weele, 2013 ).
4.1. Conclusion
Diverse internalizing and externalizing factors partially explained the path from childhood adversity to NMPO use. Since substance abuse is more difficult to treat with co-occurring psychopathologies and maladaptive behaviors, it is crucial to address childhood trauma early and focus on prevention of harmful sequelae. Expanding our knowledge of mediators from the psychological realm into relationship factors, neighborhood influences, and additional social determinants is important for comprehensive prevention and treatment efforts. Further, understanding mediators that promote the transition from prescription opioids to more potent opioids and risky drug-related behaviors is necessary to more effectively address the ongoing epidemics of opioid misuse and overdose.
Highlights.
Every increase of one ACE was associated with 32% higher odds of NMPO use for males and 24% for females.
Depression, anxiety, suicidality, delinquency, impulsivity, and risk-taking explained some, but not all, of the path from ACEs to NMPO use, with these mediators collectively attenuating the relationship somewhat more for females.
Delinquency was a strong and consistent mediator for both sexes in emerging adulthood and adulthood.
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due to Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis. We also acknowledge non-funding support from The Center for Drug Use and HIV/HCV Research (CDUHR) grant P30DA011041.
Role of funding source
This work was supported by National Institute on Drug Abuse (NIDA) study R01DA036414: Longitudinal Study of Trauma, HIV Risk, and Criminal Justice Involvement and T32 DA007233B: Behavioral Sciences Training in Drug Abuse Research Program, NYU Rory Meyers College of Nursing. These sponsors had no involvement in study design; in collection, analysis, or interpretation of data; in the writing of the report; and in the decision to submit the report for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors declare no conflict of interest.
References
- Aalsma SC, Tong Y, Wiehe SE, Tu W, 2010. The impact of delinquency on young adult sexual risk behaviors and sexually transmitted infections. J. Adol. Health, 46 (1), 17–24. [DOI] [PubMed] [Google Scholar]
- Abad J, Forns M, 2008. Personality Profile for adolescents at risk for internalizing and externalizing problems. Psychol. Rep 103(1), 219–230. doi: 10.2466/Pr0.103.1.219-230 [DOI] [PubMed] [Google Scholar]
- Arnow BA, 2004. Relationships between childhood maltreatment, adult health and psychiatric outcomes, and medical utilization. J. Clin. Psychiatry. 65, 10–15. [PubMed] [Google Scholar]
- Banerjee G, Edelman EJ, Barry DT, Becker WC, Cerda M, Crystal S, Gaither JR, Gordon AJ, Gordon KS, Kerns RD, Martins SS, Fiellin DA, Marshall BDL, 2016. Non-medical use of prescription opioids is associated with heroin initiation among US veterans: a prospective cohort study. Addiction. 111(11), 2021–2031. doi: 10.1111/add.13491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA, 1986. The moderator mediator variable distinction in social psychological-research: conceptual, strategic, and tsatistical considerations. J. Pers. Soc. Psychol 51(6), 1173–1182. doi: 10.1037//0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gwadz MA, Kahler C, Aklin WM, Lejuez CW, 2008. Sensation seeking and risk-taking propensity as mediators in the relationship between childhood abuse and HIV-related risk behavior. Child Abuse Negl 32(1), 99–109. doi: 10.1016/j.chiabu.2007.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon Y, Davis G, Hsi A, Bochte A, 2016. Adverse childhood experiences in the New Mexico juvenile justice population. Retrieved from https://nmsc.unm.edu/reports/2016/adverse-childhood-experiences-in-the-new-mexico-juvenile-justice-population.pdf
- Center for Behavioral Health Statistics and Quality., 2015. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50). Retrieved from http://www.samhsa.gov/data/
- Cerda M, Santaella J, Marshall BDL, Kim JH, Martins SS, 2015. Nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: a national study. J. Pediatrics. 167(3), 605–12. doi: 10.1016/j.jpeds.2015.04.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy E, Degenhardt L, Mattick RP, Nelson EC, 2009. Child maltreatment as a risk factor for opioid dependence: comparison of family characteristics and type and severity of child maltreatment with a matched control group. Child Abuse Negl 33(6), 343–352. doi: 10.1016/j.chiabu.2008.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crews FT, Boettiger CA, 2009. Impulsivity, frontal lobes and risk for addiction. Pharmacology Biochem. Behav 93(3), 237–247. doi: 10.1016/j.pbb.2009.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Venter M, Demyttenaere K, Bruffaerts R, 2013. The relationship between adverse childhood experiences and mental health in adulthood. A systematic literature review. Tijdschrift Voor Psychiatrie. 55(4), 259–268. [PubMed] [Google Scholar]
- Douglas KR, Chan G, Gelernter J, Arias AJ, Anton RF, Weiss RD, Brady K, Poling J, Farrer L, Kranzler HR, 2010. Adverse childhood events as risk factors for substance dependence: Partial mediation by mood and anxiety disorders. Addict. Behav 35(1), 7–13. doi: 10.1016/j.addbeh.2009.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH, 2001. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span - findings from the adverse childhood experiences study. J. Am. Med. Assoc 286(24), 3089–3096. doi:DOI 10.1001/jama.286.24.3089 [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB, 2002. Adverse childhood experiences and personal alcohol abuse as an adult. Addict. Behav 27(5), 713–725. doi: 10.1016/S0306-4603(01)00204-0 [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF, 2003. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics. 111(3), 564–572. doi: 10.1542/peds.111.3.564 [DOI] [PubMed] [Google Scholar]
- Dunn EC, Nishimi K, Powers A, Bradley B, 2017. Is developmental timing of trauma exposure associated with depressive and post-traumatic stress disorder symptoms in adulthood? J. Psych. Res 84, 119–127. doi: 10.1016/j.jpsychires.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER, Ojalehto H, Bedard-Gilligan MA, Cadigan JM, Kaysen D, 2017. Social support predicts reductions in PTSD symptoms when substances are not used to cope: a longitudinal study of sexual assault survivors. J. Affect. Disord, 229, 135–140. doi: 10.1016/j.jad.2017.12.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Forman-Hoffman VL, Winder CR, Heller DC, Kroutil LA, Lipari RN, Colpe LJ, 2015. Opioid abuse and depression in adolescents: results from the National Survey on Drug Use and Health. Drug Alc. Depend 152, 131–138. doi: 10.1016/j.drugalcdep.2015.04.010 [DOI] [PubMed] [Google Scholar]
- Feldstein SW, Miller WR, 2006. Substance use and risk-taking among adolescents. J. Mental Health. 15(6), 633–643. [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS, 1998. Relationship of childhood abuse and household dysfunction to many of th leading causes of death in adults. The adverse childhood experiences (ACE) study. Am. J. Prev. Med 14(4), 245–258. doi:Doi 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Ford JD, Hawke J, 2012. Trauma affects regulation psychoeducation group and milieu intervention outcomes in juvenile detention facilities. J. Aggress. Maltreat. Trauma. 21(4):365–384. [Google Scholar]
- Forns M, Abad J, Kirchner T, 2011. Internalizing and externalizing problems In: Levesque RJR (eds) Encyclopedia of Adolescence. Springer, New York, NY. [Google Scholar]
- Fox BH, Perez N, Cass E, Baglivio MT, Epps N, 2015. Trauma changes everything: examining the relationship between adverse childhood experiences and serious, violent and chronic juvenile offenders. Child Abuse Negl 46, 163–173. doi: 10.1016/j.chiabu.2015.01.011 [DOI] [PubMed] [Google Scholar]
- Harris KM 2013. The Add Health Study: Design and Accomplishments. Carolina Population Center, The University of North Carolina at Chapel Hill, retrieved from: https://www.cpc.unc.edu/projects/addhealth/documentation/guides/DesignPaperWIIV.pdf [Google Scholar]
- Kaufman JS, Cooper RS, 2001. Commentary: Considerations for use of racial/ethnic classification in etiologic research. Am. J. Epidemiol 154(4), 291–298. doi:DOI 10.1093/aje/154.4.291 [DOI] [PubMed] [Google Scholar]
- Khantzian EJ, 1985. The self-medication hypothesis of addictive disorders - focus on heroin and cocaine dependence. Am. J. Psychiatry. 142(11), 1259–1264. [DOI] [PubMed] [Google Scholar]
- Khoury L, Tang YL, Bradley B, Cubells JF, Ressler KJ, 2010. Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depress. Anxiety. 27(12), 1077–1086. doi: 10.1002/da.20751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankenau SE, Teti M, Silva K, Bloom JJ, Harocopos A, Treese M, 2012. Patterns of prescription drug misuse among young injection drug users. J. Urban Health. 89(6), 1004–1016. doi: 10.1007/s11524-012-9691-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson KM, Back SE, Hartwell KJ, Maria MMS, Brady KT, 2013. A comparison of trauma profiles among individuals with prescription opioid, nicotine, or cocaine dependence. Am. J. Addict 22(2), 127–131. doi: 10.1111/j.1521-0391.2013.00319.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, Duku EK, Walsh CA, Wong MY, Beardslee WR, 2001. Childhood abuse and lifetime psychopathology in a community sample. Am. J. Psychiatry, 158(11), 1878–1883. doi:DOI 10.1176/appi.ajp.158.11.1878 [DOI] [PubMed] [Google Scholar]
- Malvaso CG, Delfabbro P, Day A, 2015. The maltreatment-offending association: a systematic review of the methodological features of prospective and longitudinal studies. Trauma Violence Abuse. 19(1), 20–34. doi: 10.1177/1524838015620820 [DOI] [PubMed] [Google Scholar]
- Mateu-Gelabert P, Guarino H, Jessell L, Teper A, 2015. Injection and sexual HIV/HCV risk behaviors associated with nonmedical use of prescription opioids among young adults in New York City. J. Substance Abuse Treat 48(1), 13–20. doi: 10.1016/j.jsat.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell JC, 2015. The pain reliever and heroin epidemic in the United States: shifting winds in the perfect storm. J. Addict. Dis 34(2-3), 127–140. doi: 10.1080/10550887.2015.1059667 [DOI] [PubMed] [Google Scholar]
- McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ., 2017. Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976-2015. Pediatrics. 39(4); e20162387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley JL, Danielson CK, Amstadter AB, Ruggiero KJ, Resnick HS, Hanson RF, Smith DW, Saunders BE, Kilpatrick DG, 2010. The role of traumatic event history in non-medical use of prescription drugs among a nationally representative sample of US adolescents. J. Child Psychol. Psychiatry. 51(1), 84–93. doi: 10.1111/j.1469-7610.2009.02134.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Gratz KL, Tull MT, 2017. The role of anxiety sensitivity in reactivity to trauma cues in treatment-seeking adults with substance use disorders. Compr. Psychiatry, 78, 107–114. doi: 10.1016/j.comppsych.2017.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirhashem R, Allen HC, Adams ZW, van Stolk-Cooke K, Legrand A, Price M, 2017. The intervening role of urgency on the association between childhood maltreatment, PTSD, and substance-related problems. Addict. Behav 69, 98–103. doi: 10.1016/j.addbeh.2017.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuner F, Schauer M, Karunakara U, Klaschik C, Robert C, Elbert T, 2004. Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. Bmc Psychiatry. 4. doi: 10.1186/1471-244x-4-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry BD, Pollard R, 1998. Homeostasis, stress, trauma, and adaptation - A neurodevelopmental view of childhood trauma. Child Adol. Psychiatric Clin. North America, 7(1), 33–+. [PubMed] [Google Scholar]
- Plotzker RE, Metzger DS, Holmes WC, 2007. Childhood sexual and physical abuse histories, PTSD, depression, and HIV risk outcomes in women injection drug users: a potential mediating pathway. Am. J. Addictions, 16(6), 431–438. doi: 10.1080/10550490701643161 [DOI] [PubMed] [Google Scholar]
- Press D, Yoe J, Shern D, Najavits L, Covington S, Blanch A, 2017. Trauma-informed approaches need to be part of a comprehensive strategy for addressing the opioid epidemic. Retrieved from https://publichealth.gwu.edu/sites/default/files/downloads/Redstone-Center/CTIPP_OPB_final.pdf
- Quinn K, Boone L, Scheidell JD, Mateu-Gelabert P, McGorray SP, Beharie N, Cottler LB, Khan MR, 2016. The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug Alc. Depend 169, 190–198. doi: 10.1016/j.drugalcdep.2016.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins JM, Greenland S, 1992. Identifiability and exchangeability for direct and indirect effects. Epidemiol 3(2), 143–155. doi: 10.1097/00001648-199203000-00013 [DOI] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, Scholl L, 2016. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010-2015. Morb Mort Weekly Rep 65(50-51), 1445–1452. [DOI] [PubMed] [Google Scholar]
- Sansone RA, Whitecar P, Wiederman MW, 2009. The Prevalence of Childhood Trauma Among Those Seeking Buprenorphine Treatment. J. Addict. Dis 28(1), 64–67. doi: 10.1080/10550880802545101 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration., 2015. Trauma-Informed Approach and Trauma-Specific Interventions. Retrieved from https://www.samhsa.gov/nctic/trauma-interventions
- Surratt HL, Kurtz SP, Buttram M, Levi-Minzi MA, Pagano ME, Cicero TJ, 2017. Heroin use onset among nonmedical prescription opioid users in the club scene. Drug Alc. Depend 179, 131–138. doi: 10.1016/j.drugalcdep.2017.06.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valeri L, Van der Weele TJ, 2013. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol. Methods/ 18(2), 137–150. doi: 10.1037/a0031034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Kolk BA, Perry JC, Herman JL, 1991. Childhood Origins of Self-Destructive Behavior. Am. J. Psychiatry. 148(12), 1665–1671. [DOI] [PubMed] [Google Scholar]
- Van der Weele TJ, Vansteelandt S, 2009. Conceptual issues concerning mediation, interventions and composition. Stat. Interface, 2(4), 457–468. [Google Scholar]
- Van der Weele TJ, Vansteelandt S, 2010. Odds ratios for mediation analysis for a dichotomous outcome. Am. J. Epidemiol 172(12), 1339–1348. doi: 10.1093/aje/kwq332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber K, Rockstroh B, Borgelt J, Awiszus B, Popov T, Hoffmann K, Schonauer K, Watzl H, Propster K, 2008. Stress load during childhood affects psychopathology in psychiatric patients. Bmc Psychiatry. 8. doi: 10.1186/1471-244x-8-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Widom CS, 2008. Three potential mediators of the effects of child abuse and neglect on adulthood substance use among women. J. Stud. Alc. Drugs. 69(3), 337–347. doi:DOI 10.15288/jsad.2008.69.337 [DOI] [PubMed] [Google Scholar]