Abstract
The aim of the present study was to explore the expression levels of tumor suppressor candidate 3 (TUSC3) in human clear cell renal cell carcinoma (ccRCC) and its clinical value. Immunohistochemical staining, western blotting and reverse transcription-quantitative polymerase chain reaction were used to detect TUSC3 expression in paracancerous normal tissues and ccRCC tissues. The tissues were derived from the pathological specimens of 54 patients with ccRCC. Additionally, associations among TUSC3 expression and histological grade and clinicopathological staging of ccRCC were investigated. The results of these comparisons revealed that TUSC3 expression in ccRCC tissues was significantly lower than that in paracancerous tissues (P<0.05). TUSC3 expression in the high differentiation group was higher than that in the median and low differentiation groups (P<0.05). Expression levels of TUSC3 in stage I and II tissues were higher than those in stage III and IV tissues (P<0.05). The expression levels of TUSC3 in the lymph node metastasis group were lower than those in the non-lymph node metastasis group (P<0.05). In conclusion, the expression levels of TUSC3 in human ccRCC tissues were downregulated compared with those found in normal human renal tissue, and TUSC3 may inhibit the progression of ccRCC. Furthermore, the TUSC3 gene may be used as a promising tumor marker for the early diagnosis and prognosis of ccRCC.
Keywords: tumor suppressor candidate 3, renal cell carcinoma, clinicopathological staging
Introduction
Clear cell renal cell carcinoma (ccRCC) is the third most common adult genitourinary cancer, accounting for ~3% of all malignancies, with ~209,000 newly diagnosed cases and 14,970 cases of ccRCC-associated mortality worldwide in 2017 (1–3). ccRCC exhibits radiotherapy and chemotherapy resistance, but surgical tumor resection is an effective treatment strategy for ccRCC at present (4–6). However, there are certain limitations to the surgical resection treatments (7,8). Following surgery, 25–30% of patients with ccRCC exhibit distant metastasis occurrence and 40% of patients with ccRCC exhibit local recurrence (2,9). The prognosis of ccRCC is unfavorable and hard to predict due to the complicated biological behavior and unclear molecular mechanism of ccRCC (10). In summary, a novel method for early detection and advanced treatment strategies for ccRCC are urgently required.
Tumor suppressor candidate 3 (TUSC3) is considered to be a promising anti-oncogene (11). TUSC3 expression has been demonstrated to be downregulated in various malignant tumors with a poor prognosis, including prostate cancer, colorectal cancer and pancreatic carcinoma (12–15). TUSC3 is a homolog of the yeast Ost3p subunit of the oligosaccharyltransferase (OST) complex, which promotes N-linked glycation of proteins in the endoplasmic reticulum (16). Peng et al (17) reported that the autophagy of human non-small cell lung cancer cells may be induced by TUSC3 via the activation of the Wnt/β-catenin signaling pathway. An experiment conducted by Liu et al (18) suggested that the proliferation and migration of breast cancer cells were inhibited by the upregulation of TUSC3 expression. Although TUSC3 has been identified to be crucial for tumorigenesis, TUSC3 expression in ccRCC and its clinical significance remain unclear. The purpose of the present study was to compare the expression levels of TUSC3 in ccRCC and normal renal tissues, and to assess the prognostic value of TUSC3 expression in patients with ccRCC.
Materials and methods
Clinical specimens
Surgical specimens were obtained from 54 patients with ccRCC during a nephrectomy at Jingzhou Central Hospital (Jingzhou, China) between September 2014 and January 2017. The mean age of the 54 patients was 61.5±6.2 years (range, 48–76 years). A total of 20 patients were female and 34 were male. The present study was approved by the Institutional Ethics Committee of Jingzhou Central Hospital. All patients provided relevant clinical information and written informed consent. Half of each specimen was preserved by fixation using 4% paraformaldehyde at room temperature for 1–2 weeks, followed by routine paraffin embedding. The remaining half of each sample was preserved in liquid nitrogen at −196°C. All specimens were identified to be ccRCC tissues or normal tissues by histological identification, and tumor stage and grade were evaluated according to the American Joint Committee on Cancer guidelines (19).
Cell lines and cell culture
The human renal proximal tubular epithelial HKC8 cell line, human ccRCC A498, 786-O and OS-RC-2 cell lines, and the papillary renal cell carcinoma ACHN cell line (Type Culture Collection of the Chinese Academy of Sciences, Shanghai, China; cat. nos. GNHu12, TCHu158, TCHu186, TCHu40 and TCHu199) were cultured at 37°C with 5% CO2 in Dulbecco's modified Eagle's medium (Thermo Fisher Scientific, Inc., Waltham, MA, USA), supplemented with 10% fetal bovine serum (ScienCell Research Laboratories, Inc., San Diego, CA, USA), 0.1 mg/ml streptomycin and 100 U/ml penicillin. The medium was replaced every 24 h.
Immunohistochemistry
Immunohistochemical staining was used to evaluate the expression levels of TUSC3. The tissues were cut into 4-µm thick sections. Endogenous peroxidase activity was inhibited with 3% hydrogen peroxide at 37°C for 10 min. Subsequently, the sections were incubated in normal horse serum (1:50) in Tris-buffered saline (TBS) for 30 min at 37°C. Next, rabbit polyclonal anti-TUSC3 antibody (1:1,000; cat. no. ab77600; Abcam, Cambridge, MA, USA) was applied, followed by overnight incubation at 4°C. The sections were washed with PBS three times. Subsequently, the sections were incubated with horseradish peroxidase-conjugated secondary antibody (1:2,000; cat. no. SA00001-9; ProteinTech Group, Inc., Chicago, IL, USA) for 30 min at 20°C. The sections were incubated with the color reagent 3,3′-diaminobenzidine for 2 min at 20°C. Tissues were observed under a light microscope (magnification, ×400) and images were captured. The integrated optical density (IOD) was calculated from five random fields of view per slide using Image-Pro Plus software version 5.0 (Media Cybernetics, Inc., Rockville, MD, USA), and the IOD was presented as the mean value of three detections for each sample.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Extraction of total RNA from clinical specimens and cancer cells was performed using the TRIzol® RNA Reagent kit (Takara Bio, Inc., Otsu, Japan). RT of RNA into cDNA was conducted using the Applied Biosystems SYBR Green mix kit (cat. no. 163795-75-3; Shanghai Aladdin Biochemical Company, Shanghai, China), according to the manufacturer's protocol. The primer sequences for TUSC3 and GAPDH are shown in Table I. A total of 5 µl DNA Marker was used, and 1.5% agarose gel electrophoresis was performed using 5 µl RT-PCR product. GAPDH was used as an endogenous reference gene to analyze the relative gene expression levels. The thermocycling conditions were as follows: One cycle of 95°C for 3 min, followed by 35 cycles of 95°C for 5 sec, 58°C for 30 sec and 72°C for 30 sec. The expression levels were analyzed according to the 2−ΔΔCq method (20). All experiments were performed in triplicate. The appearance of a single peak in the melting curve implicated the specificity of the PCR products.
Table I.
Primers used for reverse transcription-quantitative polymerase chain reaction analysis of mRNA levels.
| Gene | Primer sequence (5′-3′) |
|---|---|
| TUSC3 | F: GGCTCAGTTTGTGGCAGAATC |
| R: CATCGCCTTTCGAAGTTGCT | |
| GAPDH | F: CTCGCTTCGGCAGCACA |
| R: AACGCTTCACGAATTTGCGT |
TUSC3, tumor suppressor candidate 3.
Western blotting
HKC8, A498, 786-O, OS-RC-2 and ACHN cells were lysed using a Total Protein Extraction kit (Wuhan Goodbio Technology Co., Ltd., Wuhan, China), according to the manufacturer's protocol. Protein concentrations were assessed using a Bicinchoninic Acid assay prior to loading the samples. Briefly, 40 µg/lane total protein from each sample was separated by 10% SDS-PAGE and transferred to a nitrocellulose membrane. The membranes were blocked for 2 h at room temperature with 5% milk dissolved in TBS containing 0.05% Tween-20 (TBST)), and incubated with the primary polyclonal antibodies anti-TUSC3 (1:500; cat. no. ab77600; Abcam) and anti-β-actin (1:500; cat. no. SA00001-9; ProteinTech Group Inc.), at 4°C overnight. Subsequently, the membranes were washed three times with TBST, and incubated with horseradish peroxidase-conjugated secondary antibodies (1:1,000; cat. no. SA00001-9; ProteinTech Group, Inc.) in 5% non-fat milk at room temperature for 1 h. Following three washes with TBST, the membranes were developed with enhanced chemiluminescence western blotting detection kit (EMD Millipore, Billerica, MA, USA), Expression of TUSC3 protein in each group was semi-quantified using ImageJ software (National Institutes of Health, Bethesda, MD) and Image Pro Plus v6.0 software (Media Cybernetics, Inc.).
Statistical analysis
Experiments were repeated at least three times. All data are presented as the mean ± standard deviation and were analyzed using SPSS v11.0 (SPSS, Inc., Chicago, IL, USA). Differences in values and percentages among groups were compared using a paired t-test, χ2 test, Fisher's exact test or one-way analysis of variance followed by Dunnett's multiple comparison test, respectively. Survival length was calculated from the date of surgery to the date of mortality or last follow-up. Survival curves and univariate analysis were estimated using the Kaplan-Meier method and the log-rank test. Parameters that demonstrated a statistically significant effect on overall survival in the univariate analysis were included in a Cox multivariate proportional hazards regression model. P<0.05 was considered to indicate a statistically significant difference.
Results
TUSC3 expression in clinical specimens
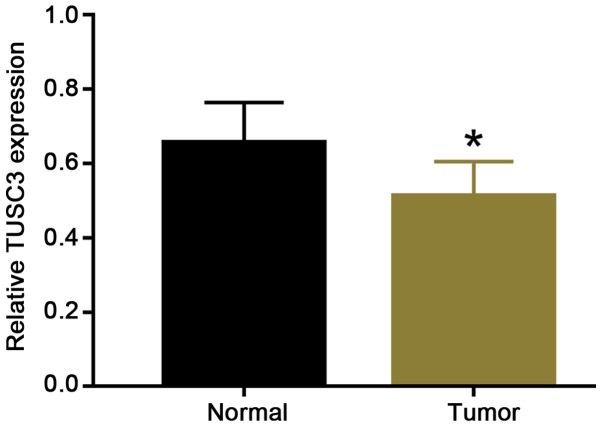
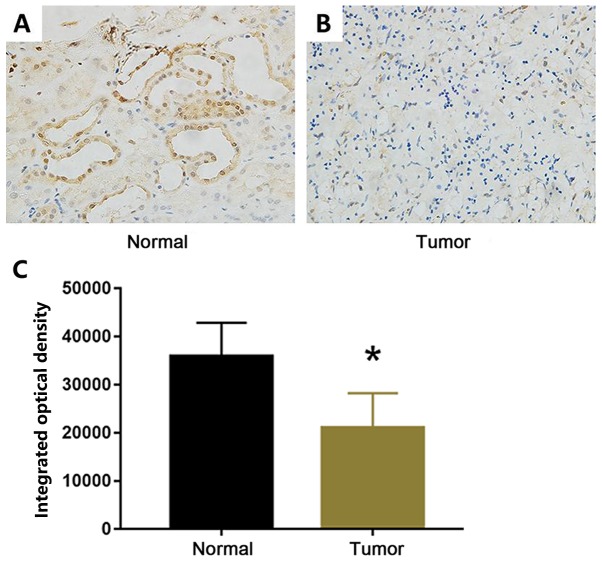
To clarify whether TUSC3 expression is associated with ccRCC progression, carcinoma tissues and adjacent non-neoplastic parenchyma were analyzed using RT-qPCR and immunohistochemical staining. The RT-qPCR data revealed that the relative expression of TUSC3 in adjacent normal tissues was 0.657±0.101 and the relative expression of TUSC3 in ccRCC tissues was 0.512±0.087. Therefore, compared with that in adjacent normal tissues, TUSC3 expression was significantly reduced in ccRCC tissues (Fig. 1). The mean (0.5845) of the relative expression of TUSC3 in tissues of all paired samples was used as a cut-off to determine high and low expression groups. In 54 paired specimens from patients with ccRCC, 35.2% of tissues exhibited high expression of TUSC3, and 64.8% of tissues exhibited low expression of TUSC3 (Table II). TUSC3 expression in adjacent normal tissues was distinctly higher than that in ccRCC tissues (P=0.007; Table II). As shown in Fig. 2, TUSC3 expression levels were decreased in tumor tissues compared with those in adjacent normal tissues. In tumor tissues, TUSC3 was expressed in the cytoplasm and nucleus of renal epithelial cells of proximal and distal tubules (Fig. 2). Furthermore, tumor stage and grade were classified according to the Tumor-Node-Metastasis (TNM) staging system of the American Joint Committee on Cancer guidelines (19) (Table III). TUSC3 levels were significantly associated with primary tumor size (P=0.030), tumor thrombus (P=0.044), clinical tumor stage (P=0.039), regional lymph node involvement (P=0.040), distant metastasis (P=0.044), TNM stage (P=0.039) and nuclear grade (P=0.021). TUSC3 expression in tumor tissues was significantly decreased in higher TNM stages. These results indicated that TUSC3 expression was closely associated with ccRCC progression.
Figure 1.
Reverse transcription-quantitative polymerase chain reaction analysis of TUSC3 expression in human clear cell renal cell carcinoma tissues from 54 patients. *P<0.05 vs. normal. TUSC3, tumor suppressor candidate 3.
Table II.
Expression levels of TUSC3 in ccRCC and adjacent tissues.
| TUSC3 expression | |||
|---|---|---|---|
| Tissues | n | Low, n (%) | High, n (%) |
| ccRCC | 54 | 35 (64.8) | 19 (35.2) |
| Adjacent normal tissues | 54 | 21 (38.9) | 33 (61.1) |
| χ2 | 7.269 | ||
| P-value | 0.007a | ||
P-value was calculated using a χ2 test.
Statistically significant. ccRCC, clear cell renal cell carcinoma; TUSC3, tumor suppressor candidate 3.
Figure 2.
Immunohistochemical analysis of TUSC3 expression. (A and B) Immunohistochemical staining of TUSC3 in normal kidney tissues and clear cell renal cell carcinoma tissues (magnification, ×400). (C) Quantitative analysis of immunohistochemical images. *P<0.01 vs. normal. TUSC3, tumor suppressor candidate 3.
Table III.
Clinicopathological characteristics of 54 patients with clear cell renal cell carcinoma and their association with TUSC3 expression.
| TUSC3 expression | ||||
|---|---|---|---|---|
| Characteristics | n | Low, n (%) | High, n (%) | P-value |
| Age at surgery, years | 0.999 | |||
| <65 | 27 | 18 (66.6) | 9 (33.3) | |
| ≥65 | 27 | 17 (63.0) | 10 (37.0) | |
| Sex | 0.572 | |||
| Male | 34 | 21 (61.8) | 13 (38.2) | |
| Female | 20 | 14 (70.0) | 6 (30.0) | |
| Primary tumor size, cm | 0.030a | |||
| <7 | 38 | 21 (60.5) | 17 (39.5) | |
| ≥7 | 16 | 14 (87.5) | 2 (12.5) | |
| Tumor thrombus | 0.044a | |||
| None | 47 | 28 (59.6) | 19 (40.4) | |
| Level 0-IV | 7 | 7 (100.0) | 0 (0.0) | |
| Primary tumor classification | 0.039a | |||
| T1+T2 | 42 | 24 (57.1) | 18 (42.9) | |
| T3+T4 | 12 | 11 (91.7) | 1 (8.3) | |
| Regional lymph node involvement | 0.040a | |||
| N0 | 43 | 26 (60.5) | 17 (39.5) | |
| N1+N2 | 11 | 11 (100.0) | 0 (0.0) | |
| Distant metastasis | 0.044a | |||
| M0 | 47 | 28 (59.6) | 19 (40.4) | |
| M1 | 7 | 7 (100.0) | 0 (0.0) | |
| TNM stage | 0.039a | |||
| I+II | 42 | 24 (57.1) | 18 (42.9) | |
| III+IV | 12 | 11 (91.7) | 1 (8.3) | |
| Nuclear grade | 0.021a | |||
| 1+2 | 41 | 23 (56.1) | 18 (43.9) | |
| 3+4 | 13 | 12 (92.3) | 1 (7.7) | |
P-values were calculated using Fisher's exact test.
Considered statistically significant. TNM, Tumor-Node-Metastasis; TUSC3, tumor suppressor candidate 3.
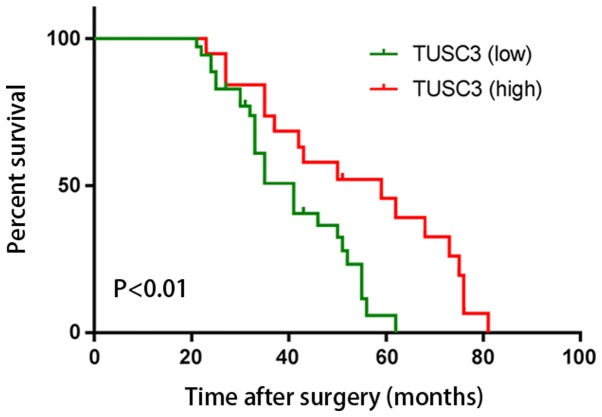
Association between TUSC3 expression and survival rate in patients
To the best of our knowledge, no study has demonstrated that the level of TUSC3 expression is a good predictor of survival in patients with ccRCC. In the present study, to determine the prognostic value of TUSC3, overall survival rates of 54 patients with ccRCC were explored using Kaplan-Meier survival curves. Postoperatively, patients with a high expression level of TUSC3 exhibited a higher overall survival rate compared with that of patients with a high expression level of TUSC3 (P<0.01; Fig. 3). This indicated that TUSC3 expression was a prognostic factor in patients with ccRCC. Cox univariate analysis revealed that primary tumor size (P=0.016), tumor thrombus (P=0.020), primary tumor classification (P=0.022), regional lymph node involvement (P=0.019), distant metastasis (P=0.026), TNM stage group (P=0.020), nuclear grade (P=0.015) and TUSC3 expression (P<0.001) were all significantly associated with overall survival (Table IV). Furthermore, Cox multivariate regression analysis suggested that primary tumor size (P=0.032), tumor thrombus (P=0.018), primary tumor classification (P=0.036), regional lymph node involvement (P=0.039), distant metastasis (P=0.044), TNM stage group (P=0.037), nuclear grade (P=0.012) and TUSC3 expression (P=0.015) were all independent prognostic factors for patients with ccRCC. These data indicated that low intratumoral TUSC3 expression may be used as a novel marker for ccRCC progression and a poor prognosis.
Figure 3.
Kaplan-Meier survival analysis of patients with clear cell renal cell carcinoma with high (n=19) and low (n=35) TUSC3 expression. TUSC3, tumor suppressor candidate 3.
Table IV.
Univariate and multivariate analyses of overall survival of patients with clear cell renal cell carcinoma.
| Overall survival | ||||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| Characteristics | HR (95% CI) | P-value | HR (95% CI) | P-value |
| Age at surgery (<65 years vs. ≥65 years) | 1.784 (1.077–3.531) | 0.062 | 1.580 (1.012–3.230) | 0.079 |
| Sex (male vs. female) | 0.728 (0.358–1.369) | 0.236 | 0.625 (0.310–1.158) | 0.291 |
| Primary tumor size (<7 cm vs. ≥7 cm) | 4.632 (2.653–6.758) | 0.016a | 5.220 (2.793–9.365) | 0.032a |
| Tumor thrombus (None vs. level 0-IV) | 9.458 (4.635–21.325) | 0.020a | 8.457 (3.656–17.632) | 0.018a |
| Primary tumor classification (T1+T2 vs. T3+T4) | 4.320 (2.542–9.326) | 0.022a | 4.550 (2.860–11.736) | 0.036a |
| Regional lymph node involvement (NX+N0 vs. N1+N2) | 7.236 (4.335–26.324) | 0.019a | 6.358 (3.886–23.656) | 0.039a |
| Distant metastasis (M0 vs. M1) | 8.873 (2.365–24.325) | 0.026a | 5.637 (1.875–17.639) | 0.044a |
| TNM stage (I+II vs. III+IV) | 3.369 (2.859–9.635) | 0.020a | 3.963 (3.582–12.362) | 0.037a |
| Nuclear grade (1+2 vs. 3+4) | 5.238 (3.596–11.387) | 0.015a | 4.698 (3.157–9.692) | 0.012a |
| TUSC3 expression (low vs. high) | 0.185 (0.102–3.112) | <0.001 | 0.326 (1.786–5.447) | 0.015a |
P<0.05. CI, confidence interval; HR, hazard ratio; TNM, Tumor-Node-Metastasis.
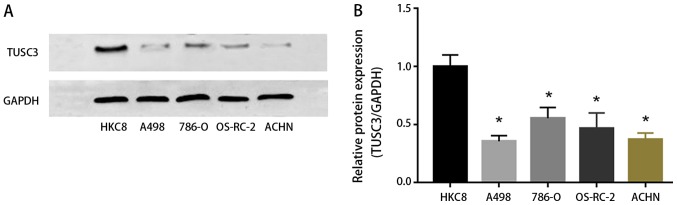
TUSC3 expression in ccRCC cells
To explore the influence of TUSC3 on RCC cell lines (A498, 786-O, OS-RC-2 and ACHN), expression levels of TUSC3 were detected by western blotting. Compared with the control group (HKC8 cells), A498, 786-O, OS-RC-2 and ACHN cells exhibited lower protein expression levels of TUSC3 (P<0.05; Fig. 4). This supported our in vivo data demonstrating that TUSC3 expression inhibits ccRCC tumorigenesis.
Figure 4.
TUSC3 expression was downregulated in clear cell renal cell carcinoma cells. (A and B) Western blot analysis of TUSC3 relative to GAPDH for HKC8, A498, 786-O, OS-RC-2 and ACHN cells. *P<0.01 vs. HKC8. TUSC3, tumor suppressor candidate 3.
Discussion
ccRCC accounts for 2–3% of adult tumors, representing 90% of renal malignancies (21,22). Despite the development of diagnostic techniques in recent years, ~30% of patients with ccRCC are diagnosed with metastases at the first diagnosis, and 30–40% of patients exhibit localized ccRCC recurrence and metastasis following surgical resection (23,24). Surgery is the most common primary therapeutic method for ccRCC; however, ccRCC cannot be treated completely by radical surgery. Recent studies have focused on the possibility of combining modalities for improving the therapeutic value of existing standard therapies, including chemotherapy and radiotherapy (25,26); however, ccRCC is not sensitive to radiotherapy and chemotherapy. Patients with ccRCC continue to have extremely poor outcomes (27,28). The genesis and progression of ccRCC involve various factors, including carcinogenic substances and environmental factors (29,30). The mortality rate of patients with metastatic ccRCC is high, although novel targeted therapies have been developed. Therefore, determining prognostic markers to more accurately select patients with ccRCC with poor survival is becoming increasingly important.
TUSC3, also known as N33, is a gene segment with a length of ~349,435 bp that is composed of 11 exons (31). The OST complex, which is a component of the endoplasmic reticulum, promotes N-linked glycation of proteins during the protein folding process (32,33). The human OST complex is composed of seven elements, including OST complex subunit 4, dolichyl-diphosphooligosaccharide protein glycosyltransferase non-catalytic subunit, defender against cell death 1, ribophorin I, ribophorin II, STT3 oligosaccharyltransferase complex catalytic subunit A or STT3 oligosaccharyltransferase complex catalytic subunit B, TUSC3/N33 and magnesium transporter 1 (16,34). TUSC3 has been demonstrated to exert various biological functions in human learning and memory processes, and its mechanism is associated with the alteration of the magnesium ion transport system (35). Numerous studies have demonstrated that TUSC3 is mainly expressed in the epithelium of the liver, lung, placenta, prostate, ovary, colon, testis and adipose tissues (13,18,36–40). TUSC3 was identified as a potential anti-oncogene when it was first identified in the 1990s, and deletion of TUSC3 expression is associated with the malignant transformation of cells (37). A large number of studies reported that the carcinogenesis of pancreatic, gastric, ovarian and prostate cancer may be associated with the mutation or deletion of TUSC3 (11,41,42). Furthermore, the loss of TUSC3 expression may result in an increase in cancer cell growth, migration and invasion (43,44).
In the present study, TUSC3 protein was identified to be downregulated in human ccRCC tissues, and its expression was significantly associated with clinical stage and lymph node metastasis. Patients with ccRCC with low expression of TUSC3 exhibited a higher TNM stage, and TUSC3 was a prognostic factor for the overall postoperative survival of patients. Numerous studies have demonstrated the anticancer properties of TUSC3 (11,13,42,44); however, the precise molecular mechanism of the function of TUSC3 in the development of tumor remains poorly understood. The sequence of the chromosomal band 8p22, where TUSC3 is located, has been revealed to be lost in human prostate cancer (45). Subsequent studies indicated that the proliferation, migration and invasion of prostate and ovarian cancer cells can be increased due to decreased TUSC3 expression (40,46). A previous study demonstrated that TUSC3 expression is downregulated in higher grades of ovarian cancer (46). Subsequently, a study explored the molecular mechanism of TUSC3 in ovarian cancer, which revealed that the hypermethylation of the TUSC3 promoter could lead to low expression of TUSC3, and the methylation of promoter is a prognostic indicator of patients with cancer (37). The present study explored TUSC3 expression in ccRCC specimens and its association with TNM staging and overall survival of patients with ccRCC, and demonstrated that immunohistochemical staining for TUSC3 served an important role in the prediction of ccRCC progression. Furthermore, the data suggested that low expression of TUSC3 in ccRCC cells was associated with the poor prognosis of patients, revealing that TUSC3 expression may be associated with the progression of ccRCC. In addition, the functions and biological mechanisms of TUSC3 are currently being elucidated (33). N-linked glycosylation of proteins serves an important role in protein synthesis, suggesting that TUSC3 may block tumor progression by transforming the glycosylation reaction in various types of carcinoma (33). Dysfunction of TUSC3 may result in improper protein glycosylation, potentially leading to disorders of cellular biological function (42). The present study revealed that TUSC3 expression may inhibit tumor progression in patients with ccRCC, and TUSC3 may serve as a biomarker to identify tumor progression and the prognosis of patients with ccRCC.
There were several limitations to the present study. One was the relatively small sample size. Second, the biomarker role of TUSC3 was only tested in ccRCC cell lines and a papillary renal cell carcinoma cell line, thus further verification in other types of RCC cell lines is required. Third, the present study did not investigate the antitumor mechanism of TUSC3 in ccRCC.
In conclusion, the present study demonstrated that TUSC3 is associated with the progression of ccRCC and the prognosis of patients with ccRCC. However, the antitumor mechanism of TUSC3 in ccRCC requires further investigation.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
JJZ conceived, designed and supervised the study. YJY drafted the manuscript. YJY and ZJC conducted the experiment. YXL contributed to statistical analysis. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the Institutional Ethics Committee of Jingzhou Central Hospital, Jingzhou, China. All patients enrolled in the present study signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Barata PC, Rini BI. Treatment of renal cell carcinoma: Current status and future directions. CA Cancer J Clin. 2017;67:507–524. doi: 10.3322/caac.21411. [DOI] [PubMed] [Google Scholar]
- 4.Cavaliere C, D'Aniello C, Pepa CD, Pisconti S, Berretta M, Facchini G. Current and emerging treatments for metastatic renal cell carcinoma. Curr Cancer Drug Targets. 2018;18:468–479. doi: 10.2174/1568009617666170209094030. [DOI] [PubMed] [Google Scholar]
- 5.Miao D, Margolis CA, Gao W, Voss MH, Li W, Martini DJ, Norton C, Bossé D, Wankowicz SM, Cullen D, et al. Genomic correlates of response to immune checkpoint therapies in clear cell renal cell carcinoma. Science. 2018;359:801–806. doi: 10.1126/science.aan5951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhai W, Ma J, Zhu R, Xu C, Zhang J, Chen Y, Chen Z, Gong D, Zheng J, Chen C, et al. MiR-532-5p suppresses renal cancer cell proliferation by disrupting the ETS1-mediated positive feedback loop with the KRAS-NAP1L1/P-ERK axis. Br J Cancer. 2018;119:591–604. doi: 10.1038/s41416-018-0196-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu KG, Gupta S, Goel S. Immunotherapy: Incorporation in the evolving paradigm of renal cancer management and future prospects. Oncotarget. 2017;8:17313–17327. doi: 10.18632/oncotarget.14388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Du Y, Pahernik S, Hadaschik B, Teber D, Duensing S, Jäger D, Hohenfellner M, Grüllich C. Survival and prognostic factors of patients with renal cell cancer with bone metastasis in the era of targeted therapy: A single-institution analysis. Urol Oncol. 2016;34:433.e1–e8. doi: 10.1016/j.urolonc.2016.05.017. [DOI] [PubMed] [Google Scholar]
- 9.Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356:125–134. doi: 10.1056/NEJMoa060655. [DOI] [PubMed] [Google Scholar]
- 10.Ridge CA, Pua BB, Madoff DC. Epidemiology and staging of renal cell carcinoma. Semin Intervent Radiol. 2014;31:3–8. doi: 10.1055/s-0033-1363837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vašíčková K, Horak P, Vaňhara P. TUSC3: Functional duality of a cancer gene. Cell Mol Life Sci. 2018;75:849–857. doi: 10.1007/s00018-017-2660-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fan X, Zhang X, Shen J, Zhao H, Yu X, Chen Y, Zhuang Z, Deng X, Feng H, Wang Y, Peng L. Decreased TUSC3 promotes pancreatic cancer proliferation, invasion and metastasis. PLoS One. 2016;11:e0149028. doi: 10.1371/journal.pone.0149028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu YF, Dong M. Expression of TUSC3 and its prognostic significance in colorectal cancer. Pathol Res Pract. 2018;214:1497–1503. doi: 10.1016/j.prp.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Birnbaum DJ, Adélaïde J, Mamessier E, Finetti P, Lagarde A, Monges G, Viret F, Gonçalvès A, Turrini O, Delpero JR, et al. Genome profiling of pancreatic adenocarcinoma. Genes Chromosomes Cancer. 2011;50:456–465. doi: 10.1002/gcc.20870. [DOI] [PubMed] [Google Scholar]
- 15.Arbieva ZH, Banerjee K, Kim SY, Edassery SL, Maniatis VS, Horrigan SK, Westbrook CA. High-resolution physical map and transcript identification of a prostate cancer deletion interval on 8p22. Genome Res. 2000;10:244–257. doi: 10.1101/gr.10.2.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohorko E, Glockshuber R, Aebi M. Oligosaccharyltrans-ferase: The central enzyme of N-linked protein glycosylation. J Inherit Metab Dis. 2011;34:869–878. doi: 10.1007/s10545-011-9337-1. [DOI] [PubMed] [Google Scholar]
- 17.Peng Y, Cao J, Yao XY, Wang JX, Zhong MZ, Gan PP, Li JH. TUSC3 induces autophagy in human non-small cell lung cancer cells through Wnt/beta-catenin signaling. Oncotarget. 2017;8:52960–52974. doi: 10.18632/oncotarget.17674. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 18.Liu K, Xie F, Gao A, Zhang R, Zhang L, Xiao Z, Hu Q, Huang W, Huang Q, Lin B, et al. SOX2 regulates multiple malignant processes of breast cancer development through the SOX2/miR-181a-5p, miR-30e-5p/TUSC3 axis. Mol Cancer. 2017;16:62. doi: 10.1186/s12943-017-0632-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amin MB, Edge SB, editors. AJCC cancer staging manual. Eighth. Switzerland: Springer; 2017. American Joint Committee on Cancer. [DOI] [Google Scholar]
- 20.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 21.Hirata H, Hinoda Y, Ueno K, Majid S, Saini S, Dahiya R. Role of secreted frizzled-related protein 3 in human renal cell carcinoma. Cancer Res. 2010;70:1896–1905. doi: 10.1158/1538-7445.AM10-2355. [DOI] [PubMed] [Google Scholar]
- 22.Tan X, Liu Y, Hou J, Cao G. Targeted therapies for renal cell carcinoma in Chinese patients: Focus on everolimus. Onco Targets Ther. 2015;8:313–321. doi: 10.2147/OTT.S64660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pei X, Li M, Zhan J, Yu Y, Wei X, Guan L, Aydin H, Elson P, Zhou M, He H, Zhang H. Enhanced IMP3 expression activates NF-κB pathway and promotes renal cell carcinoma progression. PLoS One. 2015;10:e0124338. doi: 10.1371/journal.pone.0124338. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Sanchez-Gastaldo A, Kempf E, González Del Alba A, Duran I. Systemic treatment of renal cell cancer: A comprehensive review. Cancer Treat Rev. 2017;60:77–89. doi: 10.1016/j.ctrv.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 25.Miao J, Wang L, Zhu M, Xiao W, Wu H, Di M, Huang Y, Huang S, Han F, Deng X, et al. Long-term survival and late toxicities of elderly nasopharyngeal carcinoma (NPC) patients treated by high-total- and fractionated-dose simultaneous modulated accelerated radiotherapy with or without chemotherapy. Oral Oncol. 2019;89:40–47. doi: 10.1016/j.oraloncology.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Zheng R, Lian S, Huang X, Guan G, Li X, Chi P, Xu B. The survival benefit of intensified full-dose XELOX chemotherapy concomitant to radiotherapy and then resting-period consolidation chemotherapy in locally advanced rectal cancer. J Cancer. 2019;10:730–736. doi: 10.7150/jca.28265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie J, Lin W, Huang L, Xu N, Xu A, Chen B, Watanabe M, Liu C, Huang P. Bufalin suppresses the proliferation and metastasis of renal cell carcinoma by inhibiting the PI3K/Akt/mTOR signaling pathway. Oncol Lett. 2018;16:3867–3873. doi: 10.3892/ol.2018.9111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandrasekar T, Klaassen Z, Goldberg H, Kulkarni GS, Hamilton RJ, Fleshner NE. Metastatic renal cell carcinoma: Patterns and predictors of metastases-A contemporary population-based series. Urol Oncol. 2017;35:661.e7–661.e14. doi: 10.1016/j.urolonc.2017.06.060. [DOI] [PubMed] [Google Scholar]
- 29.Melkonian SC, Daniel CR, Ye Y, Tannir NM, Karam JA, Matin SF, Wood CG, Wu X. Gene-environment interaction of genome-wide association study-identified susceptibility loci and meat-cooking mutagens in the etiology of renal cell carcinoma. Cancer. 2016;122:108–115. doi: 10.1002/cncr.29543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deckers IA, van den Brandt PA, van Engeland M, van Schooten FJ, Godschalk RW, Keszei AP, Hogervorst JG, Schouten LJ. Potential role of gene-environment interactions in ion transport mechanisms in the etiology of renal cell cancer. Sci Rep. 2016;6:34262. doi: 10.1038/srep34262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang MJ, Xing LX, Cui M, Yang X, Shi JG, Li J, Zhang KJ, Zheng ZJ, Zhang FC, Li JL, Gao XC. Association of TUSC3 gene polymorphisms with non-syndromic mental retardation based on nuclear families in the Qinba mountain area of China. Genet Mol Res. 2015;14:5022–5030. doi: 10.4238/2015.May.12.5. [DOI] [PubMed] [Google Scholar]
- 32.Molinari F, Foulquier F, Tarpey PS, Morelle W, Boissel S, Teague J, Edkins S, Futreal PA, Stratton MR, Turner G, et al. Oligosaccharyltransferase-subunit mutations in nonsyndromic mental retardation. Am J Hum Genet. 2008;82:1150–1157. doi: 10.1016/j.ajhg.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohorko E, Owen RL, Malojčić G, Brozzo MS, Aebi M, Glockshuber R. Structural basis of substrate specificity of human oligosaccharyl transferase subunit N33/Tusc3 and its role in regulating protein N-glycosylation. Structure. 2014;22:590–601. doi: 10.1016/j.str.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Vandewynckel YP, Laukens D, Geerts A, Bogaerts E, Paridaens A, Verhelst X, Janssens S, Heindryckx F, Van Vlierberghe H. The paradox of the unfolded protein response in cancer. Anticancer Res. 2013;33:4683–4694. [PubMed] [Google Scholar]
- 35.Zhou H, Clapham DE. Mammalian MagT1 and TUSC3 are required for cellular magnesium uptake and vertebrate embryonic development. Proc Natl Acad Sci USA. 2009;106:15750–15755. doi: 10.1073/pnas.0908332106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.PLOS ONE. Staff: Correction: Decreased TUSC3 promotes pancreatic cancer proliferation, invasion and metastasis. PLoS One. 2016;11:e0151752. doi: 10.1371/journal.pone.0151752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pils D, Horak P, Vanhara P, Anees M, Petz M, Alfanz A, Gugerell A, Wittinger M, Gleiss A, Auner V, et al. Methylation status of TUSC3 is a prognostic factor in ovarian cancer. Cancer. 2013;119:946–954. doi: 10.1002/cncr.27850. [DOI] [PubMed] [Google Scholar]
- 38.Luo J, Zhu H, Jiang H, Cui Y, Wang M, Ni X, Ma C. The effects of aberrant expression of LncRNA DGCR5/miR-873-5p/TUSC3 in lung cancer cell progression. Cancer Med. 2018 doi: 10.1002/cam4.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Feng S, Zhai J, Lu D, Lin J, Dong X, Liu X, Wu H, Roden AC, Brandi G, Tavolari S, et al. TUSC3 accelerates cancer growth and induces epithelial-mesenchymal transition by upregulating claudin-1 in non-small-cell lung cancer cells. Exp Cell Res. 2018;373:44–56. doi: 10.1016/j.yexcr.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 40.Horak P, Tomasich E, Vaňhara P, Kratochvílová K, Anees M, Marhold M, Lemberger CE, Gerschpacher M, Horvat R, Sibilia M, et al. TUSC3 loss alters the ER stress response and accelerates prostate cancer growth in vivo. Sci Rep. 2014;4:3739. doi: 10.1038/srep03739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gu Y, Pei X, Ren Y, Cai K, Guo K, Chen J, Qin W, Lin M, Wang Q, Tang N, et al. Oncogenic function of TUSC3 in non-small cell lung cancer is associated with Hedgehog signalling pathway. Biochim Biophys Acta Mol Basis Dis. 2017;1863:1749–1760. doi: 10.1016/j.bbadis.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 42.Kratochvílová K, Horak P, Ešner M, Souček K, Pils D, Anees M, Tomasich E, Dráfi F, Jurtíková V, Hampl A, et al. Tumor suppressor candidate 3 (TUSC3) prevents the epithelial-to-mesenchymal transition and inhibits tumor growth by modulating the endoplasmic reticulum stress response in ovarian cancer cells. Int J Cancer. 2015;137:1330–1340. doi: 10.1002/ijc.29502. [DOI] [PubMed] [Google Scholar]
- 43.Duppel U, Woenckhaus M, Schulz C, Merk J, Dietmaier W. Quantitative detection of TUSC3 promoter methylation-a potential biomarker for prognosis in lung cancer. Oncol Lett. 2017;12:3004–3012. doi: 10.3892/ol.2016.4927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gu Y, Wang Q, Guo K, Qin W, Liao W, Wang S, Ding Y, Lin J. TUSC3 promotes colorectal cancer progression and epithelial-mesenchymal transition (EMT) through WNT/β-catenin and MAPK signalling. J Pathol. 2016;239:60–71. doi: 10.1002/path.4697. [DOI] [PubMed] [Google Scholar]
- 45.Bova GS, Carter BS, Bussemakers MJ, Emi M, Fujiwara Y, Kyprianou N, Jacobs SC, Robinson JC, Epstein JI, Walsh PC, et al. Homozygous deletion and frequent allelic loss of chromosome 8p22 loci in human prostate cancer. Cancer Res. 1973;53:3869–3873. [PubMed] [Google Scholar]
- 46.Vaňhara P, Horak P, Pils D, Anees M, Petz M, Gregor W, Zeillinger R, Krainer M. Loss of the oligosaccharyl transferase subunit TUSC3 promotes proliferation and migration of ovarian cancer cells. Int J Oncol. 2013;42:1383–1389. doi: 10.3892/ijo.2013.1824. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.