Abstract
Iatrogenic pudendal nerve and groin complications have been reported to occur at rates up to 4.3%. While many of these complications are transient, the hip preservation community is in search of a safe postless distraction technique. Currently available postless distraction tables are expensive, require the surgeon to adopt a different technique, and have a high disposable fee. We present our technique for postless distraction using a standard table and a pink pad positioning device. Using our technique, we have demonstrated safe and cost-effective post-free distraction.
As the frequency of hip arthroscopy and preservation procedures continues to rise, recent evidence suggests that complication rates are significantly underreported.1 Groin-related complications of pudendal nerve palsy, impotence, and scrotal and labial tears have been reported, and the current reported incidence of pudendal nerve traction–related palsy is up to 4.3%.1, 2 Authors and companies have developed techniques and tables to achieve postless distraction to avoid such complications.3, 4, 5 Acquiring a new table can incur a substantial cost. The current proprietary Stryker postless distraction table can add a cost of up to $80,000 and then incur a disposable fee of up to $500 per case. It also requires the surgeon to adapt to a new patient position and technique.
In today's medical environment where cost conscientiousness is necessary, the ability to achieve postless distraction without incurring substantial cost or increased risk to the patient is paramount. The pink pad positioning device, developed and sold by Xodus Medical, was initially used in pilot studies for a postless distraction table for hip arthroscopy.3 This pink pad was abandoned as Stryker developed its own pad for a post-free distraction table on the Guardian table. Stryker's current post-free table requires adopting a new technique for arthroscopy. We present our technique for hip arthroscopy using this pink pad positioning device on current hip distraction tables. Our group has developed a cost-effective means to modify our current hip arthroscopy distractors to achieve postless distraction. Our method has a cost around $100 and uses the standard hip arthroscopy table to allow surgeons to continue their standard technique.
Methods
The current hip distraction beds, Hana table, Smith & Nephew distractor, ProFx table, and Arthrex distractor, can all be modified for this technique. The table is placed in the standard position per surgeon preference in the operative suite, and the pink pad (Xodus Medical) is fixed to the bed (Fig 1, Fig 2, Fig 3, Fig 4). The Velcro straps are applied around the Bucky arms on the bed for the Hana table and around the lower end of the operative table for the Smith & Nephew attachment (Figs. 1 and 2). For the Hana table, the pink pad covers the entire padded portion of the bed, and with the Smith & Nephew attachment it is important to position the pink pad as distal as possible and the patient as proximal as possible to maximize patient contact with the pink pad (Video 1). The patient is anesthetized on the gurney, and boots are applied in the standard fashion. The patient is transferred to the operative bed with a draw sheet under the patient. The C-arm is brought in from the contralateral side. An anteroposterior (AP) image is taken centering on the ischium, and the projection is rotated so the ischium is parallel to the inferior aspect of the screen image. The fluoroscopy unit is then advanced to take an AP image of the operative hip. The patient is placed as far proximal on the bed to maximize pink pad-patient contact while maintaining a clear fluoroscopic AP image of the hip (Fig. 5). The patient is then moved cephalad or caudad so an unobstructed view of the operative hip is achieved. An important note is that the patient needs to be lifted up off the mat to move cephalad or caudad and cannot be slid up or down on the pad. To facilitate this, the draw sheet should cover the majority of the pink pad, used to lift and move the patient, and be removed after the patient is positioned (Fig. 6). Once the appropriate position is obtained, the patient is secured to the bed with a safety strap, the feet are placed in the traction spars, and boots are secured in place (Figs. 7 and 8). The patient's legs are positioned per the surgeon's standard technique. The operative table is adjusted to achieve 0° to 15° of Trendelenburg, pending surgeon preference (Fig. 7). The operative field is then prepped and draped in a sterile fashion. The C-arm is then brought in, and an AP image is taken centering on the ischium; the projection is rotated so the ischium is parallel to the inferior aspect of the screen image. The fluoroscopy unit is then advanced to take an AP image of the operative hip. A spinal needle is then placed into the hip joint, and an air or normal saline arthrogram is performed with 30 to 90 mL of air or fluid, depending on surgeon preference. Adequate distension is confirmed radiographically when the femoral head subluxates laterally and distally, confirming disruption of hip suction seal (Figs. 9 and 10). Once a fluid or air arthrogram is obtained, the hip is then distracted to the surgeon's standard hip arthroscopy preference for approach for safe access. Arthroscopy is then performed per the surgeon's standard technique.
Fig 1.
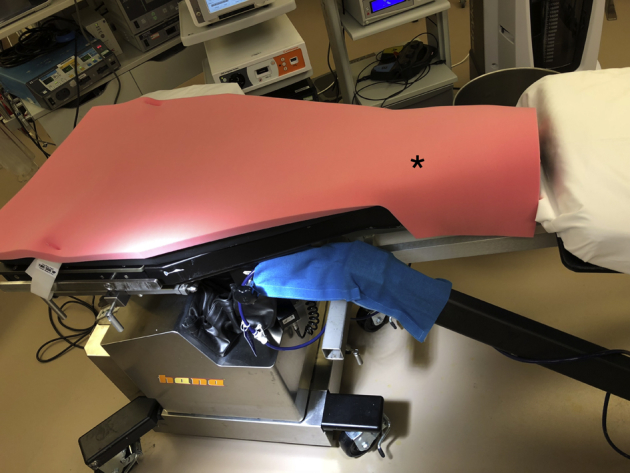
Custom pink pad for the Hana table secured to a Hana table. *Pink pad.
Fig 2.
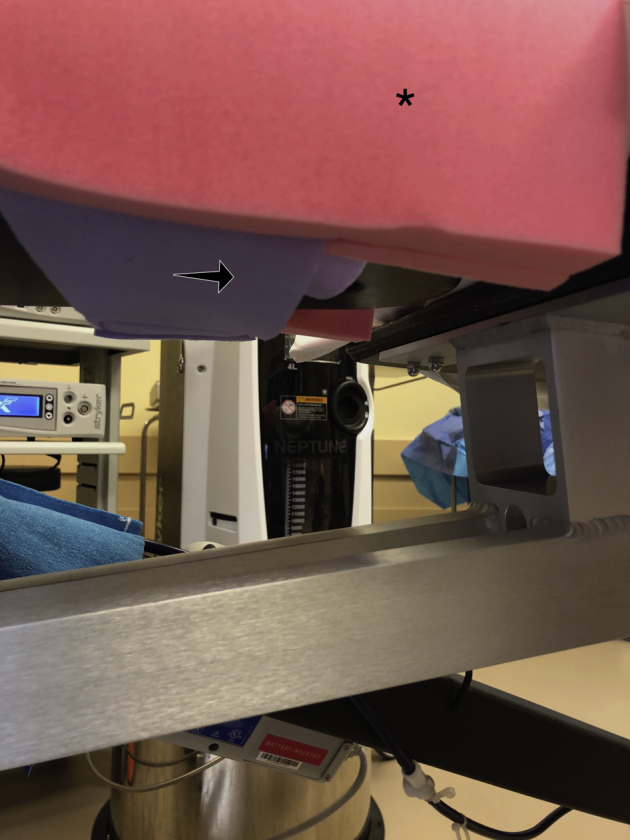
Image of the distal and posterior aspect of the secured pink pad on a Hana table. *Pink pad. The arrow indicates distally and posteriorly that the pink pad is secured with purple Velcro strap.
Fig 3.
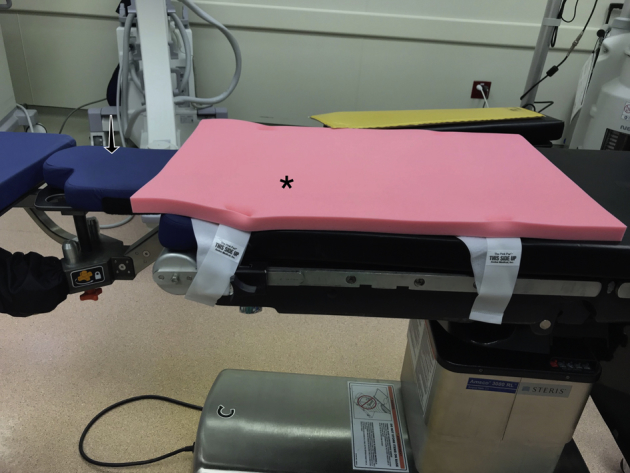
Image of the small pink pad positioning device fixed on the operative table with the Smith & Nephew distractor attached. The black arrow indicates the distractor, and the asterisk (*) indicates the pink pad attached to the bed distally.
Fig 4.

Custom pink pad developed specifically for the Smith & Nephew distractor. A draw sheet, indicated by arrow, is placed on the pad for patient transfer. *Custom designed pad for the Smith & Nephew distractor.
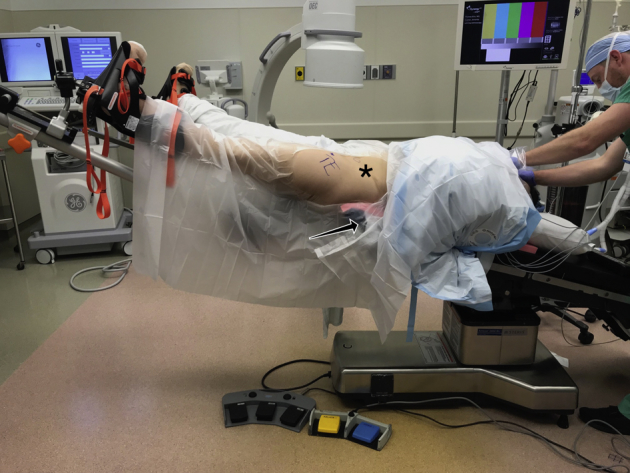
Fig 5.

Patient is in the supine position on the Hana table for revision left hip arthroscopy (arrow). The image intensifier (*) is brought in from the contralateral side to verify proper positioning of the operative left hip prior to draw sheet removal and placement in the spars. *C-arm image intensifier. The black arrow indicates the operative left hip.
Fig 6.

Patient positioning on the Hana table. The patient is in the supine position on a Hana table for revision left hip arthroscopy. Patient is moved proximally, the draw sheet is removed, and the C-arm used to have a clear anteroposterior x-ray of the operative hip. The draw sheet is removed to maximize the contact between the patient and the pink pad, arrow. *Left hip. The black arrow indicates the contact between the patient and the pink pad.
Fig 7.
Final patient positioning using the Smith & Nephew distractor for post-free distraction with the pink pad positioning device. Patient is in the supine position for left hip arthroscopy, the contralateral leg is abducted, and the bed is in 15° of Trendelenburg. * Left hip. The black arrow shows the pink pad positioning device.
Fig 8.

Patient is in the supine position for left hip arthroscopy with periacetabular osteotomy. The bed is in 5° of Trendelenburg, legs are adducted, and the draw sheet has been removed for maximum patient contact with the pink pad (black arrow). *Left operative hip. The black dot represents the adducted leg positioning. The black arrow indicates the post-free distraction with the pink pad positioning device.
Fig 9.

Patient is positioned using a Smith & Nephew distractor for left hip primary arthroscopy. Once prepped and draped, an arthrogram, using air or saline, is performed to aid in achieving post-free distraction of the hip. The black star indicates the left hip. The black arrow indicates the spinal needle used to perform the arthrogram.
Fig 10.
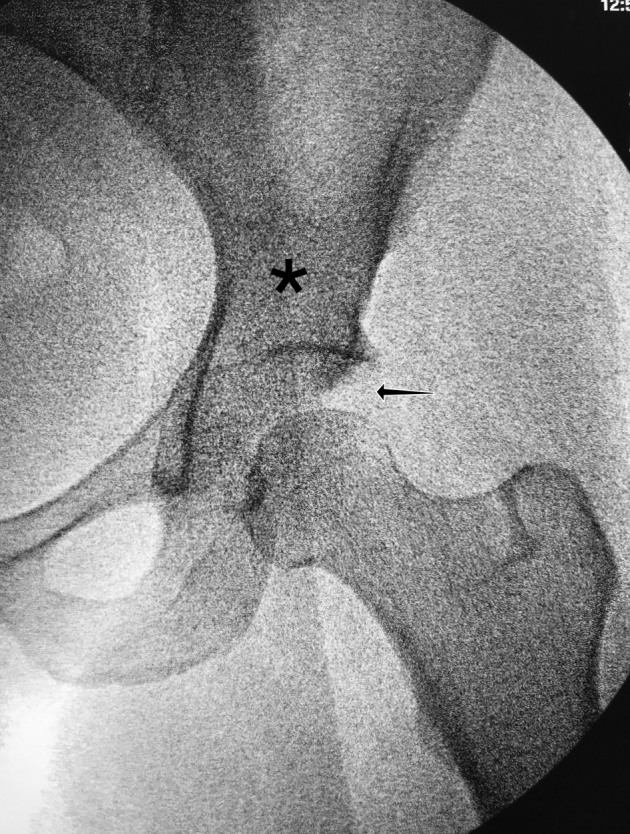
The patient is in the supine position for left hip arthroscopy using a Smith & Nephew hip distractor. Distraction is achieved using the pink pad for postless entry for hip arthroscopy. *Left hip. The black arrow indicates appropriate distraction achieved with the pink pad positioning device.
Hip access is obtained with standard anterolateral portal, and midaccessory and distal anterior lateral portals are used depending on surgeon preference. Central compartment evaluation, acetabular rim trimming, and labral repair are performed per surgeon preference. The traction is then released, and the bed is taken out of any Trendelenburg. The peripheral compartment is accessed using the surgeon's standard technique.6, 7, 8
Discussion
With the evolution and rapid growth of hip arthroscopy, attention needs to be paid to the iatrogenic groin injuries caused during the procedure. While many of these injuries are transient, they are completely avoidable by adopting a postless arthroscopic technique. Postless distraction, while a novel technique, is being marketed with a high cost for new proprietary bed attachments. The pink pad technique presented here allows for post-free distraction at the cost of most disposable large perineal pads on the market.
Pudendal nerve palsy as well as scrotal and labial skin damage are devastating iatrogenic complications of using a perineal post. Current published options for postless distraction add a significant cost in an already overburdened system and require the hip arthroscopist to adapt to a new table, new leg position, and new technique. Our technique offers surgeons the comfort of using their current technique with the caveat that Trendelenburg may be necessary in select patients.
While considering the risks and limitations of this technique to achieve safe distraction, the surgeon should keep in mind the following to avoid complications. Lighter patients, less than 120 pounds, may require greater degrees of Trendelenburg to achieve distraction. Upon distraction, the friction generated between the pad and skin may cause an anterior tilt to the pelvis and effect a lumbar lordosis. This does not occur while using a perineal post, and surgeons adopting our technique should be cognizant of this. If an increase in lordosis is observed, the buttocks and lumbosacral spine need to be adjusted to ensure a normal AP pelvis on x-ray and reduce the lumbosacral stress. Lastly, the patient cannot slide up and down on the bed. To adjust the position, the patient must be lifted completely off the pad to translate the patient up and down. The friction of the pad is too great to slide the patient and the pad will tear. In conclusion, the pink pad positioning device is an alternative method for achieving postless distraction and prospective studies are underway to further evaluate the utility (Tables 1 and 2).
Table 1.
Pearls and Pitfalls for Postless Distraction
| Step | Pearl | Pitfall |
|---|---|---|
| Fixation of the pad to the table. |
|
|
| Transfer of the patient. |
|
|
| C-arm image to ensure proper position. |
|
|
| Removal of the draw sheet. |
|
|
Table 2.
Advantages, Disadvantages, and Limitations of the Pink Pad Technique
| Advantages | Disadvantages | Limitations |
|---|---|---|
| Eliminates post-related complications. | Lighter patients (<∼120 pounds) may require greater degrees of Trendelenburg to achieve distraction. | Surgeon bias toward a perineal post. |
| Less early postoperative pain (fewer opioids, better early recovery). | Possible anterior tilt of the pelvis with increased lumbar lordosis. | Learning curve that surgeons need to invest in. |
| Strong distraction force, using gravity and friction— as strong, if not stronger than with use of perineal post, especially with heavier patients, tight stiff hips. | Cannot slide patient up or down the bed; must lift the patient completely off the pad and translate up/down. The friction between pad and patient is too great to permit sliding. | |
| Permits greater range of motion for arthroscopic and fluoroscopic dynamic examination to assess osseous corrections and possible locations of impingement. | ||
| Pad can be used on your normal operating room table without buying a completely new table and distractor legs. | ||
| Learning curve for positioning is 1 to 5 cases. | ||
| Inexpensive single-use item with small size easy for local operating room storage. | ||
| Permits central compartment traction-dependent work with less concern for time (surgeon learning curve, teaching trainees and fellow surgeons, more complicated lengthier cases [large posterolateral pincer, protrusio, complete labral reconstruction]). |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.K. receives support from Arthroscopy. T.E. receives support from Acute Innovations, Medacta, and Stryker. B.L. receives support from Biom'up. J.H. receives support from Smith and Nephew, SLACK, Össur, NIA Magellan, Frontiers in Surgery, DePuy, Arthroscopy Association of North America, Arthroscopy, American Orthopaedic Society for Sports Medicine, American Journal of Orthopedics, and AAOS. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Left hip revision arthroscopy using postless distraction achieved with the use of the pink pad positioning device. Patient is in the supine position, and the Hana table is used. Hip arthroscopy was performed using the anterolateral, mid-anterolateral, and distal anterolateral portals. Patient underwent revision arthroscopy with labral reconstruction using a fascia lata allograft, revision femoral neck osteoplasty, and capsular plication.
References
- 1.Habib A., Haldane C.E., Ekhtiari S. Pudendal nerve injury is a relatively common but transient complication of hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2018;26:969–975. doi: 10.1007/s00167-017-4783-4. [DOI] [PubMed] [Google Scholar]
- 2.Nwachukwu B.U., McFeely E.D., Nasreddine A.Y., Krcik J.A., Frank J., Kocher M.S. Complications of hip arthroscopy in children and adolescents. J Pediatr Orthop. 2011;31:227–231. doi: 10.1097/BPO.0b013e31820cadc5. [DOI] [PubMed] [Google Scholar]
- 3.Mei-Dan O., McConkey M.O., Young D.A. Hip arthroscopy distraction without the use of a perineal post: Prospective study. Orthopedics. 2013;36:e1–e5. doi: 10.3928/01477447-20121217-10. [DOI] [PubMed] [Google Scholar]
- 4.Merrell G., Medvecky M., Daigneault J., Jokl P. Hip arthroscopy without a perineal post: A safer technique for hip distraction. Arthroscopy. 2007;23:107.e101–107.e103. doi: 10.1016/j.arthro.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Mei-Dan O., Kraeutler M.J., Garabekyan T., Goodrich J.A., Young D.A. Hip distraction without a perineal post: A prospective study of 1000 hip arthroscopy cases. Am J Sports Med. 2018;46:632–641. doi: 10.1177/0363546517741704. [DOI] [PubMed] [Google Scholar]
- 6.Federer A.E., Karas V., Nho S., Coleman S.H., Mather R.C., 3rd Capsular suspension technique for hip arthroscopy. Arthrosc Tech. 2015;4:e317–e322. doi: 10.1016/j.eats.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kollmorgen R., Mather R. Current concepts in labral repair and refixation: Anatomical approach to labral management. Am J Orthop (Belle Mead, NJ) 2017;46:42–48. [PubMed] [Google Scholar]
- 8.Suslak A.G., Mather R.C., 3rd, Kelly B.T., Nho S.J. Improved arthroscopic visualization of peripheral compartment. Arthrosc Tech. 2012;1:e57–e62. doi: 10.1016/j.eats.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Left hip revision arthroscopy using postless distraction achieved with the use of the pink pad positioning device. Patient is in the supine position, and the Hana table is used. Hip arthroscopy was performed using the anterolateral, mid-anterolateral, and distal anterolateral portals. Patient underwent revision arthroscopy with labral reconstruction using a fascia lata allograft, revision femoral neck osteoplasty, and capsular plication.


