Abstract
Tumour necrosis factor α (TNF-α) and p38 mitogen-activated protein kinase (p38MAPK) serve an important role in regulating tumour cell apoptosis. However, a limited number of studies have investigated the predictive value of both TNF-α and p38MAPK in hepatocellular carcinoma (HCC). An integrated bioinformatics analysis was initially performed using two datasets available from the Oncomine™ database to determine the association between TNF-α and/or p38MAPK expression and prognosis of patients with HCC. Subsequently, TNF-α and p38MAPK expression in tissue samples from 83 patients with HCC classified as T1N0M0, using the Tumour-Node-Metastasis (TNM) staging system, was investigated using immunohistochemistry. The associations between clinicopathological characteristics and different TNF-α and p38MAPK expression levels in HCC were investigated using the χ2 test. Kaplan-Meier and Cox univariate/multivariate survival analyses were performed to explore the predictive significance of TNF-α and/or p38MAPK expression in patients with HCC. Using the Oncomine™ database, it was revealed that TNF-α and/or p38MAPK expression was not significantly associated with overall survival (OS) or disease-free survival (DFS) rates; however, TNF-α and p38MAPK expression levels were positively associated (P<0.05), and high p38MAPK expression was significantly associated with low aspartate aminotransferase levels (P<0.05). Compared with low expression levels of TNF-α and p38MAPK together, high expression of TNF-α alone, p38MAPK alone and TNF-α and p38MAPK together were significantly associated with improved OS and DFS rates (P<0.05). Additionally, multivariate Cox regression models suggested that high expression levels of TNF-α alone, p38MAPK alone, or TNF-α and p38MAPK together in the HCC microenvironment were independent predictive factors for OS and DFS rates (P<0.05). Patients with T1N0M0 HCC with high TNF-α and/or p38MAPK expression had a significantly lower risk of recurrence and mortality compared with patients with low TNF-α and p38MAPK expression. Consequently, TNF-α and p38MAPK could serve as predictive biomarkers or potential therapeutic targets for T1N0M0 HCC treatment.
Keywords: hepatocellular carcinoma, tumour necrosis factor α, p38 mitogen-activated protein kinase, bioinformatics, immunohistochemistry, prognosis
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignant tumour types worldwide and has the highest incidence rates of all types of cancer (1). In general, HCC development is silent and is, therefore, usually diagnosed only when it reaches the late stage of disease (2,3). Although HCC treatment has made marked progress with the development of modern medical science and technology, there are a limited number of effective treatment options. Surgical resection and liver transplantation remain the first choices for treating HCC (4). The 5-year survival rate following hepatectomy can reach 50–70% (5–7), but >70% of patients with HCC following surgery will have tumour recurrence (8). Therefore, identifying effective predictors of recurrence and metastasis following HCC surgery is important for guiding postoperative treatment and improving patient prognosis.
In previous years, tumour necrosis factor-α (TNF-α), interleukin (IL)-6, IL-17, IL-10 and other cytokines associated with inflammation or immunity have received extensive attention. These cytokines can promote and/or inhibit tumour development (9), and they are important for evaluating the risk of recurrence and long-term survival following HCC surgery. Among these, TNF-α is a pro-inflammatory cytokine that has a variety of biological activities and is produced primarily by macrophages and monocytes (10). TNF-α serves an important role in tumour development and progression. Moore et al (11) reported that TNF-α serves a role in promoting skin cancer development; however, Joseph et al (12) identified that TNF-α can cause damage to tumour vascular endothelial cells, resulting in blood vessel rupture, dysfunction or thrombosis. Effects such as these can block local blood flow to the tumour tissue and cause haemorrhage or hypoxic necrosis. These conflicting studies suggest that the role of TNF-α in tumours needs to be investigated further. Nevertheless, the conclusion that TNF-α is associated with tumorigenesis, development, recurrence and metastasis is consistent.
The mitogen-activated protein kinase (MAPK) family is an important signal transduction system in cells. This family includes extracellular signal regulated protein kinase, p38MAPK and c-Jun N-terminal kinase (13). The p38MAPK signalling pathway is an important part of the MAPK cascade and leads to different biological functions by mediating signal transduction (14). There is evidence that TNF-α can activate MAPK kinase kinase (MAPKKK) and ultimately activate p38MAPK and induce apoptosis (15). Furthermore, Meldrum et al (16) reported that p38MAPK can induce apoptosis by increasing TNF-α expression. In addition, Valladares et al (17) revealed that p38MAPK-mediated TNF-α induced apoptosis and cell cycle arrest in rat embryonic brown adipose tissue. The aforementioned studies indicate that TNF-α and p38MAPK are involved in apoptosis regulation and possibly tumour inhibition. TNF-α induces apoptosis by activating p38MAPK, and p38MAPK enhances TNF-α expression to induce apoptosis, which constitutes a positive feedback pathway.
The present study used an integrated bioinformatics analysis based on two datasets available from the Oncomine™ database (www.oncomine.org) to determine the association between TNF-α and/or p38MAPK expression and prognosis in HCC samples. TNF-α and p38MAPK expression was investigated in patients with HCC, alongside the associations between TNF-α and p38MAPK expression and clinicopathological characteristics and prognosis.
Materials and methods
Oncomine™ database
Oncomine™ is a bioinformatics database with an abundance of collected and standardized DNA microarray data. As an analysis platform, Oncomine™ facilitates functional discovery using genome-wide expression analyses (18,19). The present study used the Oncomine™ database to collect data on TNF-α and p38 gene abundance values and HCC prognosis. By searching ‘Gene: TNF (Search: TNF-alpha) or MAPK14 (Search: p38)’; ‘Cancer Type: Hepatocellular Carcinoma’; and ‘Clinical Outcome: Survival Status or Recurrence Status’ and setting ‘P-value: <0.0001’; ‘Fold Change: 2’; and ‘Gene rank: = top 10%’, two datasets were obtained: Guichard Liver and Guichard Liver 2. A total of 74 samples in the Guichard Liver dataset had complete follow-up data, whereas 25 samples in the Guichard Liver 2 dataset had complete follow-up data. More importantly, none of these data had detailed Tumour-Node-Metastasis (TNM) staging (20). The data were divided into high and low TNF-α- and p38MAPK-expression groups on the basis of the median of the abundance values. SPSS software (version 19.0; IBM Corp., Armonk, NY, USA) was used to perform the survival analysis.
Patient information
Paraffin-embedded specimens that had been surgically removed from 83 patients with HCC between January 2000 and December 2012 at the Department of Hepatobiliary and Pancreatic Surgery of The Affiliated Hospital of Qingdao University (Qingdao, China) were retrospectively collected. The patients included 67 males and 16 females with a mean age of 55.8 years (range, 31–83 years). The inclusion criteria were as follows: i) Postoperative pathological diagnosis of HCC, and ii) T1N0M0 stage. The exclusion criteria were as follows: i) Anticancer treatment prior to surgery, ii) serious complications or death within 30 days following surgery or iii) unavailable follow-up information. The study was approved by the Ethics Committee of The Affiliated Hospital of Qingdao University. Written informed consent was obtained from all patients.
Immunohistochemistry
Immunuohistochemistry (IHC)was performed as described previously (21). Briefly, paraffin-embedded specimens obtained from patients with HCC were cut into 4-µm-thick sections. Paraffin was removed with xylene (Shanghai Macklin Biochemical Co., Ltd., Shanghai, China) for 15 min and the sections were rehydrated through a graded alcohol series (anhydrous ethanol I, 5 min; anhydrous ethanol II, 5 min; 95% ethanol, 3 min; 90% ethanol, 3 min; 80% ethanol, 2 min; and 70% ethanol, 2 min) (Shanghai Macklin Biochemical Co., Ltd.). Following antigen retrieval with citrate buffer (10 mM, pH 6.0), endogenous peroxidase activity was blocked with 3% hydrogen peroxide for 10 min. Subsequently, the paraffin slides were stained with anti-TNF-α (1:100 dilution; catalogue no. Ab6671; Abcam, Cambridge, MA, USA) or anti-p38 (1:50 dilution; catalogue no. Ab197348; Abcam) primary antibodies at 4°C overnight. The MaxVision kit (Fuzhou Maixin Biotech Co., Ltd., Fujian, China) was used to detect primary antibodies, and the colour was developed using 3,3′-diaminobenzidine chromogen substrate. The slides were counterstained with haematoxylin for 1 min, cleared in water and mounted with neutral balsam.
IHC evaluation
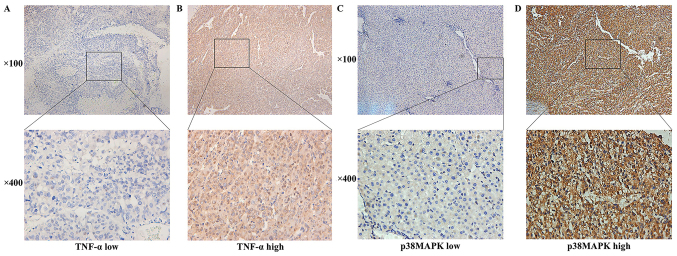
As described previously (21), two pathologists at the Affiliated Hospital of Qingdao University (Qingdao, China) who had been blinded to the clinical data interpreted the results simultaneously. Under a light microscope, markedly stained cells exhibited brown staining in the cytoplasm. Overall, 10 fields were observed under high magnification (magnification, ×400), and the degree of immunostaining was reviewed and scored according to the intensity of staining and the percentage of immunoreactive cells. Staining intensity was graded according to the following criteria: Cells without staining were scored as 0, whereas that stained light yellow, yellowish brown and brown were scored as 1, 2 and 3 points, respectively. The extent of immunoreactivity was graded as follows: <5%, ≥5%, ≥26%, ≥51% and ≥75% were scored as 0, 1, 2, 3 and 4 points, respectively. The two scores were summed, and a total score of ≤4 represented low expression, whereas >4 represented high expression. All patients were divided into high- and low-expression groups according to the IHC score results. Patients with high expression levels of both TNF-α and p38MAPK were included in the high-expression group, whereas those with low expression of both TNF-α and p38MAPK were included in the low-expression group. Patients with high TNF-α and low p38MAPK expression and patients with low TNF-α and high p38MAPK expression were included in the TNF-α high-expression group and the p38MAPK high-expression group, respectively. Representative images are presented in Fig. 1.
Figure 1.
TNF-α and p38MAPK expression levels detected using immunohistochemistry. (A) Low expression and (B) high expression of TNF-α in the hepatocellular carcinoma microenvironment (magnification, ×100 and ×400). (C) Low expression and (D) high expression of p38MAPK in the hepatocellular carcinoma microenvironment (magnification, ×100 and ×400). TNF-α, tumour necrosis factor-α; p38MAPK, p38 mitogen-activated protein kinase.
Statistical analysis
All statistical analyses were performed using SPSS software (version 19.0; IBM Corp.). The χ2 test, continuous correction χ2 test or Fisher's exact test was used to analyse the association between TNF-α or p38MAPK expression and the clinicopathological characteristics. The association between TNF-α and p38MAPK expression was determined by Pearson's contingency analysis. The data were censored at the last follow-up (March 2017) for patients without recurrence, metastases or mortality. Disease-free survival (DFS) and overall survival (OS) rates were assessed using Kaplan-Meier curves. The log-rank test was used to compare TNF-α and/or p38MAPK expression with recurrence and survival. The Cox proportional hazards model was used to screen variables for unilateral and multivariate analyses of HCC prognosis. A two-tailed P<0.05 was considered to indicate a statistically significant difference.
Results
TNF-α/p38MAPK expression in HCC and clinicopathological characteristics
By reference to the Oncomine™ database, TNF-α and p38MAPK exhibited high expression rates in the HCC samples. TNF-α and p38MAPK were positively expressed in 50.51 (50/99) and 50.51% (50/99) of the samples, respectively.
In the T1N0M0 HCC tissues, TNF-α and p38MAPK were distributed in a diffuse manner and were present primarily in the cytoplasm of the tumour cells (Fig. 1). TNF-α and p38MAPK were highly expressed in the HCC microenvironment. TNF-α and p38MAPK were positively expressed in 62.65 (52/83) and 69.88% (58/83) of the samples, respectively.
The association between TNF-α/p38MAPK expression in the HCC microenvironment and various clinicopathological characteristics of the patients with HCC were analysed using the χ2 test as presented in Table I. High p38MAPK expression in the HCC microenvironment was significantly associated with low aspartate aminotransferase (AST) levels (P=0.026; Table I). However, no significant associations were observed between TNF-α or p38MAPK expression and the other clinicopathological features. Pearson's contingency analysis indicated a positive association between TNF-α and p38MAPK expression (r=0.253; P=0.021; Table II).
Table I.
Association between TNF-α/p38MAPK expression and clinicopathological characteristics.
| TNF-α | p38MAPK | ||||||
|---|---|---|---|---|---|---|---|
| Parameter | n (%) | High | Low | P-value | High | Low | P-value |
| Sex | 0.989a | 0.846b | |||||
| Male | 67 (80.7) | 42 | 25 | 46 | 21 | ||
| Female | 16 (19.3) | 10 | 6 | 12 | 4 | ||
| Age, years | 0.803a | 0.567a | |||||
| <50 | 20 (24.1) | 13 | 7 | 15 | 5 | ||
| ≥50 | 63 (75.9) | 39 | 24 | 43 | 20 | ||
| Alcohol abuse | 0.835a | 0.268a | |||||
| Yes | 23 (27.7) | 14 | 9 | 14 | 9 | ||
| No | 60 (72.3) | 38 | 22 | 44 | 16 | ||
| HBV infection | 0.919b | 0.169b | |||||
| Yes | 74 (89.2) | 47 | 27 | 54 | 20 | ||
| No | 9 (10.8) | 5 | 4 | 4 | 5 | ||
| TBIL level, µmol/l | 0.684b | 1.000b | |||||
| ≤22 | 72 (86.7) | 44 | 28 | 50 | 22 | ||
| >22 | 11 (13.3) | 8 | 3 | 8 | 3 | ||
| ALB level, g/l | 0.530b | 0.169b | |||||
| <35 | 9 (10.8) | 7 | 2 | 4 | 5 | ||
| ≥35 | 74 (89.2) | 45 | 29 | 54 | 20 | ||
| ALT level, U/l | 0.722a | 0.542b | |||||
| ≤60 | 68 (81.9) | 42 | 26 | 49 | 19 | ||
| >60 | 15 (18.1) | 10 | 5 | 9 | 6 | ||
| AST level, U/l | 0.803a | 0.026a | |||||
| ≤42 | 63 (75.9) | 39 | 24 | 48 | 15 | ||
| >42 | 20 (24.1) | 13 | 7 | 10 | 10 | ||
| PLT level, ×109 cells/l | 0.304a | 0.467b | |||||
| <100 | 19 (22.9) | 10 | 9 | 12 | 7 | ||
| ≥100 | 64 (77.1) | 42 | 22 | 46 | 18 | ||
| Liver cirrhosis | 1.000b | 0.871b | |||||
| Yes | 9 (10.8) | 6 | 3 | 7 | 2 | ||
| No | 74 (89.2) | 46 | 28 | 51 | 23 | ||
| AFP level, ng/l | 0.779a | 0.257a | |||||
| ≤400 | 63 (75.9) | 40 | 23 | 42 | 21 | ||
| >400 | 20 (24.1) | 12 | 8 | 16 | 4 | ||
| Child-Pugh grade | 1.000c | 0.301c | |||||
| A | 82 (98.8) | 51 | 31 | 58 | 24 | ||
| B | 1 (1.2) | 1 | 0 | 0 | 1 | ||
| Tumor size, cm | 0.363b | 0.231b | |||||
| ≤5 | 76 (91.6) | 46 | 30 | 55 | 21 | ||
| >5 | 7 (8.4) | 6 | 1 | 3 | 4 | ||
| Tumor margin, cm | 0.530b | 0.089b | |||||
| ≤2 | 74 (89.2) | 45 | 29 | 49 | 25 | ||
| >2 | 9 (10.8) | 7 | 2 | 9 | 0 | ||
| Pathological differentiation | 0.694b | 0.377b | |||||
| High | 8 (9.6) | 4 | 4 | 4 | 4 | ||
| Middle and low | 75 (90.4) | 48 | 27 | 54 | 21 | ||
| Microvascular tumor thrombus | 0.722a | 0.991b | |||||
| Yes | 15 (18.1) | 10 | 5 | 11 | 4 | ||
| No | 68 (81.9) | 42 | 26 | 47 | 21 | ||
| Capsule invasion | 0.470b | 1.000c | |||||
| Yes | 76 (91.6) | 49 | 27 | 53 | 23 | ||
| No | 7 (8.4) | 3 | 4 | 5 | 2 | ||
Pearson's χ2 test
Continuity correction by χ2 test
Fisher's exact test. TNF-α, tumor necrosis factor α; p38MAPK, p38 mitogen-activated protein kinase; HBV, hepatitis B virus; TBIL, total bilirubin; ALB, albumin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; PLT, platelet; AFP, α-fetoprotein.
Table II.
Association between the expression of TNF-α and p38MAPK.
| TNF-α | Pearson's contingency | |||
|---|---|---|---|---|
| p38MAPK | High | Low | Coefficient | P-value |
| High | 41 | 17 | 0.253 | 0.021 |
| Low | 11 | 14 | ||
TNF-α, tumor necrosis factor α; p38MAPK, p38 mitogen-activated protein kinase.
Survival analysis
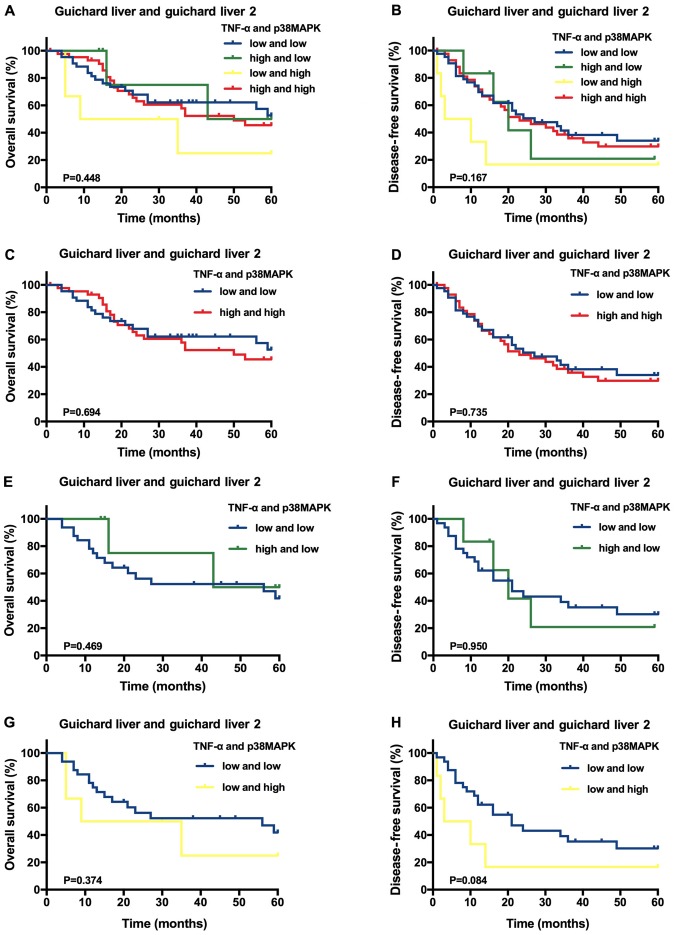
Using the Oncomine™ datasets, it was identified that the average follow-up time was 33.19±20.64 months (range, 1.0–60.0 months), and the 1-, 3- and 5-year OS rates were 83.84, 45.45 and 24.24%, respectively. The DFS rates at 1, 3 and 5 years were 70.00, 29.30 and 16.16%, respectively. A Kaplan-Meier analysis of 99 HCC samples indicated that, compared with the other expression categories, high TNF-α and p38MAPK expression levels were not significantly associated with higher OS or DFS rates (P>0.05; Fig. 2A and B). Furthermore, compared with HCC samples with low expression of both TNF-α and p38MAPK, the samples with high expression of either TNF-α or p38MAPK, as well as those with high expression of both TNF-α and p38MAPK, were not significantly associated with improved OS and DFS rates (P>0.05; Fig. 2C-H).
Figure 2.
Predictive value of TNF-α and/or p38MAPK expression in the Oncomine™ database hepatocellular carcinoma samples. Kaplan-Meier overall survival and disease-free survival analysis of the different samples stratified according to the specific expression category: (A and B) both high vs. all others, (C and D) both high vs. both low, (E and F) TNF-α high vs. both low, (G and H) p38MAPK high vs. both low. TNF-α, tumour necrosis factor-α; p38MAPK, p38 mitogen-activated protein kinases.
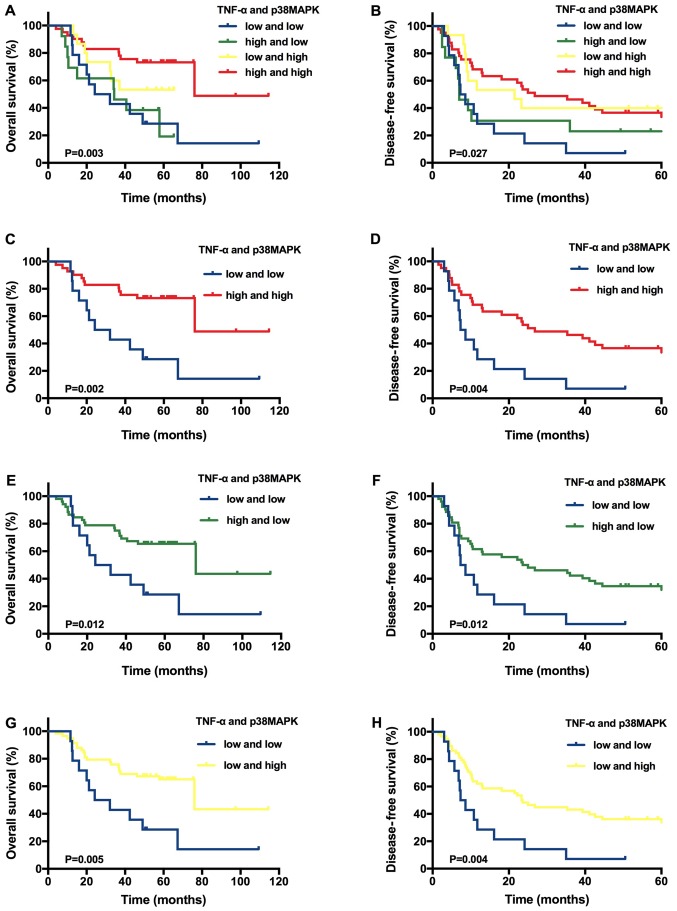
However, in the tissues from patients with T1N0M0 HCC, the average follow-up time was 44.85±24.11 months (range, 4.0–114.5 months), and the 1-, 3- and 5-year OS rates were 90.36, 66.27 and 31.33%, respectively. The DFS rates at 1, 3 and 5 years were 53.01, 36.14 and 19.28%, respectively. A Kaplan-Meier analysis of 83 patients with T1N0M0 HCC indicated significantly improved OS (P=0.003) and DFS (P=0.027) rates for the group with high levels of both TNF-α and p38MAPK expression compared with the other groups (Fig. 3A and 3B). On the basis of these results, another Kaplan-Meier analysis was performed using 83 patients with T1N0M0 HCC. Patients with high expression levels of both TNF-α and p38MAPK had higher OS (P=0.002) and DFS (P=0.004) rates compared with patients with low expression levels of both TNF-α and p38MAPK (Fig. 3C and D). Furthermore, the patients with high TNF-α expression alone had improved OS (P=0.012) and DFS (P=0.012) rates compared with patients with low expression levels of both TNF-α and p38MAPK (Fig. 3E and F). The patients with high p38MAPK expression alone had higher OS (P=0.005) and DFS (P=0.004) rates compared patients with low expression levels of both TNF-α and p38MAPK (Fig. 3G and H).
Figure 3.
Predictive value of TNF-α and/or p38MAPK expression in patients with T1N0M0 hepatocellular carcinoma. Kaplan-Meier overall survival and disease-free survival analysis of the different tissues stratified according to the specific expression category: (A and B) both high vs. all others, (C and D) both high vs. both low, (E and F) TNF-α high vs. both low, (G and H) p38MAPK high vs. both low. TNF-α, tumour necrosis factor-α; p38MAPK, p38 mitogen-activated protein kinase.
In addition, multiple univariate and multivariate Cox proportional hazards analyses were performed, including analyses of the high TNF-α only, high p38MAPK only, and high TNF-α and p38MAPK expression groups. The multivariate analysis of the TNF-α-expression group indicated that no hepatitis B virus infection (P=0.019), platelets ≥100×109 cells/l (P=0.031) and high TNF-α expression (P=0.0497) were independent predictive factors for an improved OS rate (Table III). Tumour size ≤5 cm (P=0.044), no microvascular tumour thrombus (P=0.010) and high TNF-α expression (P=0.005) also independently indicated an improved DFS rate (Table IV). Furthermore, the multivariate analysis of the p38MAPK-expression group identified that high p38MAPK expression (P=0.004) was an independent predictive factor for a higher OS rates (Table III). No microvascular tumour thrombus (P=0.031) and high p38MAPK expression (P=0.003) were independent predictive factors for a higher DFS rates (Table IV). In addition, the multivariate Cox regression model of the TNF-α and p38MAPK-expression group (both low vs. both high) revealed that no microvascular tumour thrombus (P=0.025 and P=0.011, respectively) and high TNF-α and p38MAPK expression (P=0.001 and P=0.002, respectively) were independent indicators for improved OS and DFS rates (Tables III and IV, respectively).
Table III.
Multivariate analysis of variables potentially associated with overall survival (Cox regression model).
| Variable | HR (95% CI) | P-value |
|---|---|---|
| TNF-α | ||
| HBV infection (no vs. yes) | 3.296 (1.212–8.967) | 0.019 |
| PLT level (<100 vs. ≥100×109 cells/l) | 0.417 (0.188–0.921) | 0.031 |
| TNF-α (both low vs. TNF-α high) | 0.461 (0.213–0.999) | 0.0497 |
| p38MAPK | ||
| p38MAPK (both low vs. p38MAPK high) | 0.332 (0.157–0.702) | 0.004 |
| TNF-α and p38MAPK | ||
| Microvascular tumor thrombus (no vs. yes) | 2.863 (1.141–7.185) | 0.025 |
| TNF-α and p38MAPK (both low vs. both high) | 0.251 (0.108–0.588) | 0.001 |
HR, hazard ratio; CI, confidence interval; TNF-α, tumor necrosis factor α; HBV, hepatitis B virus; PLT, platelet; p38MAPK, p38 mitogen-activated protein kinase.
Table IV.
Multivariate analysis of variables potentially associated with disease-free survival (Cox regression model).
| Variable | HR (95% CI) | P-value |
|---|---|---|
| TNF-α | ||
| Tumor size (≤5 cm vs. >5 cm) | 2.340 (1.022–5.356) | 0.044 |
| Microvascular tumor thrombus (no vs. yes) | 2.411 (1.235–4.707) | 0.010 |
| TNF-α (both low vs. TNF-α high) | 0.621 (0.444–0.869) | 0.005 |
| p38MAPK | ||
| Microvascular tumor thrombus (no vs. yes) | 2.057 (1.068–3.964) | 0.031 |
| p38MAPK (both low vs. p38MAPK high) | 0.372 (0.193–0.716) | 0.003 |
| TNF-α and p38MAPK | ||
| Microvascular tumor thrombus (no vs. yes) | 2.500 (1.230–5.079) | 0.011 |
| TNF-α and p38MAPK (both low vs. both high) | 0.337 (0.166–0.681) | 0.002 |
HR, hazard ratio; CI, confidence interval; TNF-α, tumor necrosis factor α; p38MAPK, p38 mitogen-activated protein kinase.
Discussion
In the present study, datasets from the Oncomine™ database were used to demonstrate that TNF-α and/or p38MAPK expression was not significantly associated with OS and DFS. However, there was no detailed TNM staging information in the Oncomine™ datasets; therefore, additional patients were screened according to their TNM stage and only patients with T1N0M0 HCC were selected. A positive association between TNF-α and p38MAPK expression in the HCC tumour microenvironment was revealed. p38MAPK expression was negatively associated with AST levels. In addition, OS and DFS rates were significantly improved in patients with T1N0M0 HCC with high expression levels of both TNF-α and p38MAPK in the tumour microenvironment compared with patients in the other groups. On the basis of these results, a pairwise comparison was conducted. It was revealed that the OS and DFS rates of patients with T1N0M0 HCC with high TNF-α and/or p38MAPK expression were improved compared with those of patients with low TNF-α and p38MAPK expression. In addition, a multivariate survival analysis indicated that high expression levels of TNF-α only or p38MAPK only, as well as both TNF-α and p38MAPK, in the T1N0M0 HCC microenvironment were independent predictive factors for OS and DFS rates.
TNF-α was identified in the 1970s as a cytokine secreted by immune cells that inhibits tumour cell growth and induces degenerative changes in tumours (22,23). There is evidence that TNF-α can promote p38MAPK signalling pathway activation (24,25). More notably, Sabio and Davis (26) indicated that MAPK activation by TNF-α can also increase TNF-α expression in target cells. These studies support the conclusion of the present study that TNF-α and p38MAPK are positively associated in the HCC tumour microenvironment (r=0.253; P=0.021). Additionally, Ichijo et al (15) indicated that TNF-α can induce apoptosis through activating p38MAPK, which may affect the prognosis of patients with cancer. Meldrum et al (16) also suggested that p38MAPK can induce apoptosis by enhancing TNF-α expression. Therefore, it can be hypothesized that TNF-α and p38MAPK are involved in apoptosis regulation and may thus have inhibitory effects on tumours. However, the mechanism through which TNF-α and p38MAPK induce apoptosis and further inhibit tumours remains unclear and requires further investigation.
It has been suggested that TNF-α released by host and tumour cells is an important factor in the initiation, proliferation, angiogenesis and metastasis of various types of cancer, and that it has a promoting effect on tumours (27,28). These suggestions were derived through investigation of the inhibitory effect of TNF-α on tumour cell apoptosis induced by nuclear factor-κB; however, the cytokine network in the body is a complex system. TNF-α does not exert its effects on tumours through a single pathway, but rather through multiple signal transductions. For example, Ichijo et al (15) and Donnahoo et al (29) identified that TNF-α can also promote apoptosis in tumour cells by interacting with p38MAPK. In the present study, the TNF-α/p38MAPK/TNF-α signalling pathway was investigated, which has not been widely studied to date. However, the current study has indicated that patients with T1N0M0 HCC with high TNF-α and/or p38MAPK expression had improved OS and DFS rates compared with the patients with low expression of both TNF-α and p38MAPK (P<0.05). In addition, a multivariate survival analysis revealed that high TNF-α and/or p38MAPK expression in the T1N0M0 HCC microenvironment was an independent predictive factor for OS and DFS (P<0.05). Therefore, to obtain improved OS and DFS rates, individualized treatment plans may be developed for patients with T1N0M0 HCC on the basis of postoperative TNF-α and p38MAPK expression levels. Then, according to the specific circumstances, a recombinant human TNF-α or p38MAPK activator could be injected into the liver of patients with T1N0M0 HCC. Van Horssen et al (30) identified that the topical use of TNF-α in combination with chemotherapeutic drugs can produce potent antitumour effects. However, relevant clinical trials should be designed to verify this treatment concept to further benefit patients with T1N0M0 HCC.
In summary, the results of the present study have revealed a positive association between TNF-α and p38MAPK expression in the T1N0M0 HCC microenvironment. It was also identified that high TNF-α and/or p38MAPK expression is an independent predictive factor of OS and DFS rates and that patients with T1N0M0 HCC with high TNF-α and/or p38 MAPK expression have a favourable prognosis. TNF-α and p38MAPK could act as predictive biomarkers or potential therapeutic targets for treatment patients with T1N0M0 HCC. Importantly, the results from the present study indicate that patients with T1N0M0 HCC with low TNF-α and p38MAPK expression require more frequent follow-up observations. It should be noted that the present study is a single-centre study with a small sample size, and more conclusive results may be obtained by including more patients. In addition, the treatment for patients with T1N0M0 HCC with low TNF-α and p38MAPK expression also requires validation in future studies.
Acknowledgements
Not applicable.
Funding
The present study was supported by grants from the Science and Technology for People's Livelihood Project of Qingdao (no. 18-6-1-89-nsh), the Key Research and Development Plan of Shandong Province (no. 2018GSF118233) and the Science and Technology Plan of Qingdao City Shinan District (no. 2018-4-018-YY).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
BH, LW and SZ contributed to the study design. MZ and JH contributed to data analysis. HL and WH contributed to the collection of the tissue samples and patient data. MZ and JH wrote the manuscript. All authors have read and approved the final version of the manuscript.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of The Affiliated Hospital of Qingdao University. Written informed consent was obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Qin H, Du X, Zhang Y, Wang R. Platycodin D, a triterpenoid saponin from Platycodon grandiflorum, induces G2/M arrest and apoptosis in human hepatoma HepG2 cells by modulating the PI3K/Akt pathway. Tumor Biol. 2014;35:1267–1274. doi: 10.1007/s13277-013-1169-1. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;65:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.Josep ML. Hepatocellular carcinoma. Lancet (London, England) 2003;9399 doi: 10.1016/S0140-6736(03)14964-1. [DOI] [PubMed] [Google Scholar]
- 4.Carr BI. Hepatocellular carcinoma: Current management and future trends. Gastroenterology. 2004;127:S218–S224. doi: 10.1053/j.gastro.2004.09.036. [DOI] [PubMed] [Google Scholar]
- 5.Altekruse SF, McGlynn KA, Dickie LA, Kleiner DE. Hepatocellular carcinoma confirmation, treatment, and survival in surveillance, epidemiology, and end results registries, 1992–2008. Hepatology. 2012;55:476–482. doi: 10.1002/hep.24710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahbari NN, Mehrabi A, Mollberg NM, Müller SA, Koch M, Büchler MW, Weitz J. Hepatocellular carcinoma: Current management and perspectives for the future. Ann Surg. 2011;253:453–469. doi: 10.1097/SLA.0b013e31820d944f. [DOI] [PubMed] [Google Scholar]
- 7.Takayama T. Surgical treatment for hepatocellular carcinoma. Japanese J Clin Oncol. 2011;41:447–454. doi: 10.1093/jjco/hyr016. [DOI] [PubMed] [Google Scholar]
- 8.Poon RT. Prevention of recurrence after resection of hepatocellular carcinoma: A daunting challenge. Hepatology. 2011;54:757–759. doi: 10.1002/hep.24569. [DOI] [PubMed] [Google Scholar]
- 9.Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007;117:1175–1183. doi: 10.1172/JCI31537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caminero A, Comabella M, Montalban X. Tumor necrosis factor alpha (TNF-alpha), anti-TNF-alpha and demyelination revisited: An ongoing story. J Neuroimmunol. 2011;234:1–6. doi: 10.1016/j.jneuroim.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Moore RJ, Owens DM, Stamp G, Arnott C, Burke F, East N, Holdsworth H, Turner L, Rollins B, Pasparakis M, et al. Mice deficient in tumor necrosis factor-alpha are resistant to skin carcinogenesis. Nat Med. 1999;5:828–831. doi: 10.1038/10552. [DOI] [PubMed] [Google Scholar]
- 12.Joseph WR, Cao Z, Mountjoy KG, Marshall ES, Baguley BC, Ching LM. Stimulation of tumors to synthesize tumor necrosis factor-alpha in situ using 5,6-dimethylxanthenone-4-acetic acid: A novel approach to cancer therapy. Cancer Res. 1999;59:633–638. [PubMed] [Google Scholar]
- 13.Mugami S, Dobkin-Bekman M, Rahamim-Ben Navi L, Naor Z. Differential roles of PKC isoforms (PKCs) in GnRH stimulation of MAPK phosphorylation in gonadotrope derived cells. Mol Cell Endocrinol. 2018;463:97–105. doi: 10.1016/j.mce.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Yokota T, Wang Y. p38 MAP kinases in the heart. Gene. 2016;575:369–376. doi: 10.1016/j.gene.2015.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ichijo H, Nishida E, Irie K, ten Dijke P, Saitoh M, Moriguchi T, Takagi M, Matsumoto K, Miyazono K, Gotoh Y. Induction of apoptosis by ASK1, a mammalian MAPKKK That activates SAPK/JNK and p38 signaling pathways. Science. 1997;275:90–94. doi: 10.1126/science.275.5296.90. [DOI] [PubMed] [Google Scholar]
- 16.Meldrum KK, Meldrum DR, Hile KL, Yerkes EB, Ayala A, Cain MP, Rink RC, Casale AJ, Kaefer MA. p38 MAPK mediates renal tubular cell TNF-alpha production and TNF-alpha-dependent apoptosis during simulated ischemia. Am J Physiol Cell physiol. 2001;281:C563–C570. doi: 10.1152/ajpcell.2001.281.2.C563. [DOI] [PubMed] [Google Scholar]
- 17.Valladares A, Alvarez AM, Ventura JJ, Roncero C, Benito M, Porras A. p38 mitogen-activated protein kinase mediates tumor necrosis factor-alpha-induced apoptosis in rat fetal brown adipocytes. Endocrinology. 2000;141:4383–4395. doi: 10.1210/endo.141.12.7843. [DOI] [PubMed] [Google Scholar]
- 18.Rhodes DR, Kalyana-Sundaram S, Mahavisno V, Varambally R, Yu J, Briggs BB, Barrette TR, Anstet MJ, Kincead-Beal C, Kulkarni P, et al. Oncomine 3.0: Genes, pathways, and networks in a collection of 18,000 cancer gene expression profiles. Neoplasia. 2007;9:166–180. doi: 10.1593/neo.07112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhodes DR, Yu J, Shanker K, Deshpande N, Varambally R, Ghosh D, Barrette T, Pandey A, Chinnaiyan AM. ONCOMINE: A cancer microarray database and integrated data-mining platform. Neoplasia. 2004;6:1–6. doi: 10.1016/S1476-5586(04)80047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamarajah SK, Frankel TL, Sonnenday C, Cho CS, Nathan H. Critical evaluation of the American joint commission on cancer (AJCC) 8th edition staging system for patients with hepatocellular carcinoma (HCC): A surveillance, epidemiology, end results (SEER) analysis. J Surg Oncol. 2018;117:644–650. doi: 10.1002/jso.24908. [DOI] [PubMed] [Google Scholar]
- 21.Zhang M, Zhang S, Yang Z, Hu J, Hu W, Sun P, Wu L, Han B. Association between the expression levels of IL-6 and IL-6R in the hepatocellular carcinoma microenvironment and postoperative recurrence. Oncol Lett. 2018;16:7158–7165. doi: 10.3892/ol.2018.9557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Green S, Dobrjansky A, Chiasson MA. Murine tumor necrosis-inducing factor: Purification and effects on myelomonocytic leukemia cells. J Natl Cancer Inst. 1982;68:997–1003. [PubMed] [Google Scholar]
- 23.Matthews N, Watkins JF. Tumor-Necrosis factor from the rabbit. I. Mode of action, specificity and physicochemical properties. Br J Cancer. 1978;38:302–309. doi: 10.1038/bjc.1978.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mose M, Kang Z, Raaby L, Iversen L, Johansen C. TNFα-and IL-17A-mediated S100A8 expression is regulated by p38 MAPK. Exp Dermatol. 2013;22:476–481. doi: 10.1111/exd.12187. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Wang W, Wang L, Wang X, Xia J. Regulatory mechanisms of interleukin-8 production induced by tumour necrosis factor-α in human hepatocellular carcinoma cells. J Cell Mol Med. 2012;16:496–506. doi: 10.1111/j.1582-4934.2011.01337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sabio G, Davis RJ. TNF and MAP kinase signaling pathways. Semin Immunol. 2014;26:237–245. doi: 10.1016/j.smim.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luo JL, Maeda S, Hsu LC, Yagita H, Karin M. Inhibition of NF-kappaB in cancer cells converts inflammation-induced tumor growth mediated by TNFalpha to TRAIL-mediated tumor regression. Cancer Cell. 2004;6:297–305. doi: 10.1016/j.ccr.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 28.Pikarsky E, Porat RM, Stein I, Abramovitch R, Amit S, Kasem S, Gutkovich-Pyest E, Urieli-Shoval S, Galun E, Ben-Neriah Y. NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature. 2004;431:461–466. doi: 10.1038/nature02924. [DOI] [PubMed] [Google Scholar]
- 29.Donnahoo KK, Shames BD, Harken AH, Meldrum DR. Review article: The role of tumor necrosis factor in renal ischemia-reperfusion injury. J Urol. 1999;162:196–203. doi: 10.1097/00005392-199907000-00068. [DOI] [PubMed] [Google Scholar]
- 30.van Horssen R, Ten Hagen TL, Eggermont AM. TNF-alpha in cancer treatment: Molecular insights, antitumor effects, and clinical utility. Oncologist. 2006;11:397–408. doi: 10.1634/theoncologist.11-4-397. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.