Abstract
Background
Magnesium is an essential mineral required for regulation of body temperature, nucleic acid and protein synthesis and in maintaining nerve and muscle cell electrical potentials. Many women, especially those from disadvantaged backgrounds, have low intakes of magnesium. Magnesium supplementation during pregnancy may be able to reduce fetal growth restriction and pre‐eclampsia, and increase birthweight.
Objectives
To assess the effects of magnesium supplementation during pregnancy on maternal, neonatal/infant and paediatric outcomes.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (31 March 2013).
Selection criteria
Randomised and quasi‐randomised trials assessing the effects of dietary magnesium supplementation during pregnancy were included. The primary outcomes were perinatal mortality (including stillbirth and neonatal death prior to hospital discharge), small‐for‐gestational age, maternal mortality and pre‐eclampsia.
Data collection and analysis
Two review authors independently assessed study eligibility, extracted data and assessed the risk of bias of included studies.
Main results
Ten trials involving 9090 women and their babies were included; one trial had a cluster design (with randomisation by study centre). All 10 trials randomly allocated women to either an oral magnesium supplement or a control group; in eight trials a placebo was used, and in two trials no treatment was given to the control group. In the 10 included trials, the compositions of the magnesium supplements, gestational ages at commencement, and doses administered varied, including: magnesium oxide, 1000 mg daily from ≤ four months post‐conception (one trial); magnesium citrate, 365 mg daily from ≤ 18 weeks until hospitalisation after 38 weeks (one trial), and 340 mg daily from nine to 27 weeks' gestation (one trial); magnesium gluconate, 2 to 3 g from 28 weeks' gestation until birth (one trial), and 4 g daily from 23 weeks' gestation (one trial); magnesium aspartate, 15 mmol daily (three trials, commencing from either six to 21 weeks' gestation until birth, ≤ 16 weeks' gestation until birth, or < 12 weeks until birth), or 365 mg daily from 13 to 24 weeks until birth (one trial); and magnesium stearate, 128 mg elemental magnesium from 10 to 35 weeks until birth (one trial).
In the analysis of all trials, oral magnesium supplementation compared to no magnesium was associated with no significant difference in perinatal mortality (stillbirth and neonatal death prior to discharge) (risk ratio (RR) 1.10; 95% confidence interval (CI) 0.72 to 1.67; five trials, 5903 infants), small‐for‐gestational age (RR 0.76; 95% CI 0.54 to 1.07; three trials, 1291 infants), or pre‐eclampsia (RR 0.87; 95% CI 0.58 to 1.32; three trials, 1042 women). None of the included trials reported on maternal mortality.
Considering secondary outcomes, while no increased risk of stillbirth was observed, a possible increased risk of neonatal death prior to hospital discharge was shown for infants born to mothers who had received magnesium (RR 2.21; 95% CI 1.02 to 4.75; four trials, 5373 infants). One trial contributed over 70% of the participants to the analysis for this outcome; the trial authors suggested that the large number of severe congenital anomalies in the supplemented group (unlikely attributable to magnesium) and the deaths of two sets of twins (with birthweights < 750 g) in the supplemented group likely accounted for the increased risk of death observed, and thus this result should be interpreted with caution. Furthermore, when the deaths due to severe congenital abnormalities in this trial were excluded from the meta‐analysis, no increased risk of neonatal death was seen for the magnesium supplemented group. Magnesium supplementation was associated with significantly fewer babies with an Apgar score less than seven at five minutes (RR 0.34; 95% CI 0.15 to 0.80; four trials, 1083 infants), with meconium‐stained liquor (RR 0.79; 95% CI 0.63 to 0.99; one trial, 4082 infants), late fetal heart decelerations (RR 0.68; 95% CI 0.53 to 0.88; one trial, 4082 infants), and mild hypoxic‐ischaemic encephalopathy (RR 0.38; 95% CI 0.15 to 0.98; one trial, 4082 infants). Women receiving magnesium were significantly less likely to require hospitalisation during pregnancy (RR 0.65, 95% CI 0.48 to 0.86; three trials, 1158 women).
Of the 10 trials included in the review, only two were judged to be of high quality overall. When an analysis was restricted to these two trials none of the review's primary outcomes (perinatal mortality, small‐for‐gestational age, pre‐eclampsia) were significantly different between the magnesium supplemented and control groups.
Authors' conclusions
There is not enough high‐quality evidence to show that dietary magnesium supplementation during pregnancy is beneficial.
Plain language summary
There is not enough high quality evidence to show that dietary magnesium supplementation during pregnancy is beneficial
Many women, especially those from disadvantaged backgrounds, have intakes of magnesium below recommended levels. Magnesium supplementation during pregnancy may be able to reduce growth restriction of the fetus and pre‐eclampsia (high blood pressure and protein in the urine during pregnancy), and increase birthweight. This review aimed to assess the effects of magnesium supplementation during pregnancy on maternal, neonatal and paediatric outcomes.
We included 10 randomised trials involving 9090 women and their babies in this review. These trials were of a low to moderate quality overall. No difference in the risk of perinatal mortality (stillbirth and death of babies prior to hospital discharge) was found when we compared the group of babies born to mothers who received magnesium during their pregnancy and the group of babies born to mothers who did not receive magnesium. Magnesium supplementation did not reduce the risk of babies being born small for their gestational age, and did not reduce the risk of pre‐eclampsia for the mothers.
We found no convincing evidence that magnesium supplementation during pregnancy is beneficial.
Background
Magnesium is one of the essential minerals needed by humans in relatively large amounts. Magnesium works with many enzymes to regulate body temperature, synthesise nucleic acids and proteins as well as maintaining electrical potentials in nerves and muscle membranes. Magnesium also has an important role in modulating vasomotor tone and cardiac excitability. Magnesium occurs widely in many foods; dairy products, breads and cereals, legumes, vegetables and meats are all good sources. It is therefore not surprising that frank magnesium deficiency has never been reported to occur in healthy individuals who eat varied diets. However, processing of the above foods can lead to marked depletion of magnesium. Common causes of magnesium deficiency include inadequate dietary intake or gastrointestinal absorption, increased losses through the gastrointestinal or renal systems and increased requirement for magnesium, such as in pregnancy.
A study measuring serum magnesium during low‐risk pregnancies reported that both ionised and total serum magnesium were significantly reduced after the 18th week of gestation compared to measurements prior to this time (Arikan 1999). Dietary intake studies during pregnancy consistently demonstrate that many women, especially those from disadvantaged backgrounds, have intakes of magnesium below recommended levels (Inst Med 1990). In a retrospective study of medical records, Conradt 1984 reported that magnesium supplementation during pregnancy was associated with a reduced risk of fetal growth retardation and pre‐eclampsia. A later cross‐sectional study of dietary intake towards the end of the first trimester of pregnancy reported that higher magnesium intake was associated with increased birthweight (Doyle 1989). Stimulated by these encouraging preliminary reports, several randomised clinical trials have been undertaken to evaluate the potential benefits of magnesium supplementation during pregnancy on maternal and infant outcomes.
Why it is important to do this review
This review updates a previously published Cochrane review on magnesium supplementation during pregnancy (Makrides 2001). In this previous version of the review, magnesium supplementation was shown to be associated with a lower frequency of preterm birth, low birthweight and small‐for‐gestational age when compared with placebo. However, of the seven trials included in this previous version, only one was judged to be of high quality. Thus the review authors concluded that there was not enough high‐quality evidence to show that dietary magnesium supplementation during pregnancy is beneficial.
It is important to assess whether magnesium supplementation during pregnancy has benefits for mothers and their infants without causing harm. We believe this review could provide information about the potential for magnesium supplementation to improve neonatal/infant outcomes such as weight and growth and improve maternal outcomes such as pre‐eclampsia, without causing adverse effects for women and their babies.
Objectives
To assess the effects of magnesium supplementation during pregnancy on maternal, neonatal/infant and paediatric outcomes, using the best available evidence.
Methods
Criteria for considering studies for this review
Types of studies
All published, unpublished and ongoing randomised, quasi‐randomised trials or cluster‐randomised trials of dietary magnesium supplementation during pregnancy. For the purpose of this review, a dietary supplement was defined as a product taken by mouth that contains a "dietary ingredient" intended to supplement the diet (US FDA 2009).
Types of participants
Women with normal or high‐risk pregnancies.
Types of interventions
We included studies where magnesium was administered orally at any time during the antenatal period, regardless of dose. We excluded where magnesium was administered intravenously/intramuscularly.
Types of outcome measures
Primary outcomes
Infant
Perinatal mortality (including stillbirth and neonatal death prior to hospital discharge)
Small‐for‐gestational age
Maternal
Maternal mortality
Pre‐eclampsia
Secondary outcomes
Infant
Stillbirth
Neonatal death prior to hospital discharge
Miscarriage
Gestational age at birth
Preterm birth at less than 37 weeks
Birthweight and low birthweight
Admission to a neonatal intensive care unit
Long‐term infant outcomes (disability at paediatric follow‐up)
Infant outcomes not pre‐specified in the original protocol
Low Apgar score at one or five minutes
Late fetal heart decelerations
Meconium‐stained liquor and meconium aspiration
Breech presentation
Placental abruption
Placental weight
Hypoxic ischaemic encephalopathy (HIE) and neonatal encephalopathy
Congenital abnormalities
Maternal
Maternal acceptance of treatment
Side effects of therapy (grouped as gastrointestinal and non‐gastrointestinal)
Systolic and diastolic blood pressure
Pregnancy‐induced hypertension
Eclampsia
Need for maternal hospitalisation
Antepartum and postpartum haemorrhage
Length of labour
The methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirht Group.
Search methods for identification of studies
Electronic searches
For the search strategy used to identify trials included in the previous version of this review (Other published versions of this review), see Appendix 1.
For this update, we contacted the Trials Search Co‐ordinator to search the Cochrane Pregnancy and Childbirth Group’s Trials Register (31 March 2013).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
weekly searches of Embase;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and Embase, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
We did not apply any language restrictions.
Data collection and analysis
For the methods used when assessing the trials identified in a previous version of this review (Other published versions of this review), see Appendix 1.
For the most recent update we used the following methods when assessing the trials identified by the search.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies we identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted a third person.
Data extraction and management
We designed a form to extract data. For eligible studies, at least two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted a third person. We entered data into Review Manager software (RevMan 2012) and checked for accuracy.
When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details. When articles were not written in English, every attempt was made to obtain translations to ensure accurate data extraction and analysis.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreement by discussion or by involving a third author.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the methods used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the methods as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation sequence and determined whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study, the methods, if any, used to blind study participants and personnel from knowledge of which intervention a participant received. We considered studies to be at a low risk of bias if they were blinded, or if we judged that the lack of blinding would be unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported or was supplied by the trial authors, we included the missing data in the analyses which we undertook.
We assessed the methods as:
low risk of bias (e.g. where there was no missing data or where reasons for missing data were balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; 'as treated' analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting bias (checking for reporting bias)
We described for each included study how the possibility of selective outcome reporting bias was examined by us and what we found.
We assessed the methods as:
low risk of bias (where it was clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review had been reported);
high risk of bias (where not all the study’s pre‐specified outcomes had been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other sources of bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias. We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals
Continuous data
For continuous data, we used the mean difference when outcomes were measured in the same way between trials. We planned to use the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
We have included one cluster‐randomised trial (Hungary 1988) in the analyses along with individually‐randomised trials. We have adjusted its sample size and event rates using the methods described in the Cochrane Handbook and a conservative estimate of the intracluster correlation co‐efficient (ICC) (0.02) in the primary analysis (Higgins 2011) (Table 1). As estimates of ICCs for mortality outcomes have been shown to be lower than for other perinatal outcomes, we also carried out a sensitivity analysis to investigate the effect of varying the ICC (using a range of ICCs from 0.0002 to 0.02) for the outcomes perinatal mortality, stillbirth, and neonatal death prior to discharge.
1. The original data and adjusted data for dichotomous data of the cluster‐randomised trial.
| Outcomes | Intervention (original data) | Control (original data) | Intervention (adjusted data)1 | Control (original data)1 | ||||
| Total number | Event number | Total number | Event number | Total number | Event number | Total number | Event number | |
| Perinatal mortality | 6 | 400 | 5 | 396 | 3 | 174 | 2 | 172 |
| Small‐for‐gestational age < 10th percentile | 33 | 400 | 59 | 396 | 14 | 174 | 26 | 172 |
| Stillbirth | 3 | 400 | 3 | 396 | 1 | 174 | 1 | 172 |
| Neonatal death prior to discharge | 3 | 400 | 2 | 396 | 1 | 174 | 1 | 172 |
| Miscarriage (< 20 weeks' gestation) | 28 | 428 | 32 | 428 | 12 | 186 | 14 | 186 |
| Preterm birth < 37 weeks' gestation | 33 | 400 | 54 | 396 | 14 | 174 | 23 | 172 |
| Low birthweight | 18 | 400 | 31 | 396 | 8 | 174 | 13 | 172 |
| Maternal side effects | 140 | 400 | 156 | 396 | 61 | 174 | 68 | 172 |
1. Adjusted data = n / design effect, where:
- design effect = 1 + (M ‐ 1) x ICC = 2.3
- M = average cluster size = (total number of intervention + total number of control randomised)/(cluster number of intervention + cluster number of control) = 66
- ICC = intracluster correlation co‐efficient = 0.02
We acknowledged heterogeneity in the randomisation unit and performed a subgroup analysis to investigate the effects of the randomisation unit.
Dealing with missing data
For included studies, we noted levels of attrition. We planned to explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analyses.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses, and all participants were analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either the Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
In future updates of this review, if there are 10 or more studies in the meta‐analysis, we plan to investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2012). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar. If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or where substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average range of possible treatment effects and we have discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we would not have combined trials.
Where we have used random‐effects analyses, we have presented the results as the average treatment effect with its 95% confidence interval, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
If we had identified substantial heterogeneity, we planned to investigate it using subgroup analyses and sensitivity analyses. We planned to consider whether an overall summary was meaningful, and if it was, used random‐effects analysis to produce it.
Maternal characteristics and characteristics of the intervention may affect health outcomes.
We planned to carry out the following subgroup analyses.
Composition of magnesium supplement (i.e. magnesium citrate versus magnesium aspartate versus other)
Dose of magnesium (i.e. high versus low)
Gestational age at commencement of supplementation (i.e. commencement at < 28 weeks versus ≥ 28 weeks)
Normal versus high‐risk women
However, we were not able to conduct subgroup analyses based on the gestational age at commencement of supplementation or on the inclusion of normal versus high‐risk women, as only one trial administered magnesium after 28 weeks' gestation and included high‐risk women (China 1997), and this trial did not report on any of the review's primary outcomes. We were not able to conduct a subgroup analysis based on dose in this update.
We restricted subgroup analyses to primary outcomes.
We assessed subgroup differences by interaction tests available within RevMan (RevMan 2012). We have reported the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
We carried out a sensitivity analysis to explore the effects of trial quality assessed by allocation concealment and sequence generation, by omitting studies rated as 'high risk of bias' and 'unclear' for these components. We restricted this to the primary outcomes.
Results
Description of studies
SeeCharacteristics of included studies; Characteristics of excluded studies and Characteristics of ongoing studies.
Results of the search
The updated search of the Cochrane Pregnancy and Childbirth Group’s Trials Register identified 22 new reports relating to 14 studies.
We have included three new trials (Hungary 1979; Italy 1994; South Africa 2007), and have excluded nine studies (Denmark 1990; Denmark 1991; Detroit 1999; India 2012; ISRCTN03989660; NCT01709968; Norway 2008; Sweden 1987; Sweden 1995).
Two trials are currently ongoing, assessing magnesium supplementation in the second trimester of pregnancy for overweight individuals (NCT01510665) and magnesium citrate for the prevention of increased blood pressure during the final weeks of pregnancy (ISRCTN98365455) (seeCharacteristics of ongoing studies for further details).
We previously included seven trials in this review (Angola 1992; Austria 1997; China 1997; Hungary 1988; Memphis 1989; Mississippi 1992; Zurich 1988). We have therefore included a total of 10 trials (Angola 1992; Austria 1997; China 1997; Hungary 1979; Hungary 1988; Italy 1994; Memphis 1989; Mississippi 1992; South Africa 2007; Zurich 1988), and excluded a total of nine studies from this review.
Included studies
For full details seeCharacteristics of included studies.
Five studies were conducted in Europe (Austria 1997; Hungary 1979; Hungary 1988; Italy 1994; Zurich 1988), two in America (Memphis 1989; Mississippi 1992), two in Africa (Angola 1992; South Africa 2007), and one in Asia (China 1997).
Participants
A total of 9090 women and their babies were included in the 10 trials; four trials had sample sizes of less than 150 women (Angola 1992; China 1997; Italy 1994; Mississippi 1992), and the South Africa 2007 trial randomised 4476 women.
In six trials both primiparous and multiparous women were included (Angola 1992; Austria 1997; Hungary 1988; Mississippi 1992; South Africa 2007; Zurich 1988) while in three trials, only primiparous women were included (China 1997; Italy 1994; Memphis 1989); this was not clearly specified in Hungary 1979.
Women were recruited at various stages in their pregnancies into the included trials. In the Angola 1992 trial, designed for the prevention of pre‐eclampsia, women were recruited at any stage during their first four months of pregnancy, whereas in China 1997, also designed for the prevention of pregnancy‐induced hypertension, normal and high‐risk women were recruited from 22 weeks' gestation. Women with low‐risk pregnancies were recruited into the Austria 1997 trial before their 18th week of pregnancy, for the prevention of preterm labour; in the Mississippi 1992 trial however, women with risk factors for preterm birth were recruited at a mean gestational age at entry between 23 and 24 weeks. In Hungary 1988 and South Africa 2007, women were recruited at their first antenatal clinic/appointment (in South Africa 2007 the gestational age of women varied from 10 to 35 weeks, with a mean of 21 weeks). In Memphis 1989 women were recruited from between 13 and 24 weeks' gestation, whereas in Italy 1994 and Zurich 1988, women were included at no later than 12 and 16 weeks respectively.
Interventions and comparisons
In the 10 included trials, the composition of the magnesium supplements, gestational ages at commencement of supplementation, and doses administered varied. In eight of the trials a placebo supplement (Angola 1992; China 1997; Hungary 1988; Italy 1994; Mississippi 1992; South Africa 2007) or active control (aspartic acid) (Memphis 1989; Zurich 1988) was used; in two trials, no treatment was given to the control group (Austria 1997; Hungary 1979).
Magnesium oxide: in one trial (Angola 1992) women were given two tablets daily of magnesium oxide 500 mg (1000 mg total daily) beginning from no later than four months post‐conception.
Magnesium citrate: in two trials, women received magnesium citrate tablets (Austria 1997; Hungary 1979). Women in Austria 1997 were given 365 mg of magnesium citrate daily from no later than 18 weeks' gestation until hospitalisation after 38 weeks, whereas women in Hungary 1979 received 340 mg of magnesium citrate daily, either before nine weeks' gestation, or from nine to 27 weeks' gestation.
Magnesium gluconate: women in two trials received magnesium gluconate (China 1997; Mississippi 1992). In China 1997 women received 2 g of magnesium gluconate daily from 28 weeks' gestation to 30 weeks; they then received 3 g daily from 30 weeks until delivery. In Mississippi 1992 women received two 500 mg tablets of magnesium gluconate four times daily (4 g daily total, 215 mg elemental magnesium) from 23 weeks' gestation.
Magnesium aspartate: in four trials, women received magnesium aspartate. In Hungary 1988, Italy 1994 and Zurich 1988 women received 15 mmol of magnesium aspartate daily. In Hungary 1988 women received a tablet of 5 mmol three times per day from six to 21 weeks' gestation until birth, whereas in Zurich 1988 women received six tablets daily from no later than 16 weeks' gestation until birth. In Italy 1994 supplementation commenced before 12 weeks' gestation. In Memphis 1989 women received six tablets of magnesium aspartate hydrochloride per day (each containing 60.8 mg elemental magnesium: 365 mg daily) from between 13 to 24 weeks until birth.
Magnesium stearate: in South Africa 2007 women received two 'slow‐release' magnesium tablets daily (64 mg elemental magnesium per tablet) from the time of enrolment (10 to 35 weeks; mean: 21 weeks) until birth.
Outcomes
All of the 10 included trials focused on perinatal outcomes for women and/or their babies (Angola 1992; Austria 1997; China 1997; Hungary 1979; Hungary 1988; Italy 1994; Memphis 1989; Mississippi 1992; South Africa 2007; Zurich 1988). None of the included studies reported on any longer‐term outcomes for the infants.
Excluded studies
Four studies were excluded as intravenous magnesium sulphate was administered as part of the intervention (Denmark 1990; Denmark 1991; Detroit 1999; India 2012). Four further trials were excluded (ISRCTN03989660; NCT01709968; Norway 2008; Sweden 1995), as they assessed the effects of oral magnesium supplementation on pregnancy‐related leg cramps and therefore have been (or are likely to be) considered for inclusion in the relevant Cochrane review (Garrison 2012). One further trial (Sweden 1987) did not assess magnesium, rather assessed calcium and vitamin C for pregnant women with leg cramps.
SeeCharacteristics of excluded studies for further details.
Risk of bias in included studies
We judged the trials to have a moderate risk of bias overall. See Figure 1 and Figure 2.
1.
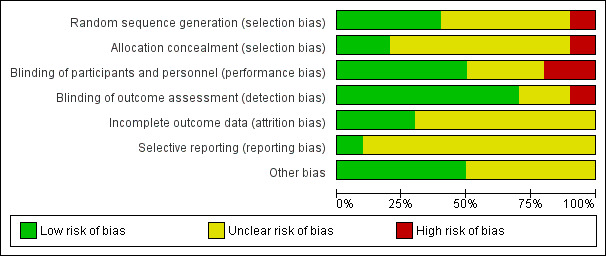
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
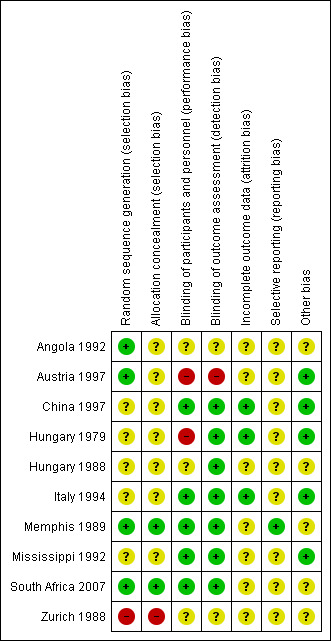
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Four of the 10 trials used adequate methods to generate a random sequence (Angola 1992; Austria 1997; Memphis 1989; South Africa 2007). Angola 1992 used a table of random numbers; in Austria 1997, Memphis 1989 and South Africa 2007 a computer‐generated randomisation list was used. For five trials, the methods used for random sequence generation were unclear (China 1997; Hungary 1979; Hungary 1988; Italy 1994; Mississippi 1992), and in one trial, allocation was based on the participants' date of birth (Zurich 1988).
Only two trials were judged to have adequate methods to conceal allocation (Memphis 1989; South Africa 2007). In Memphis 1989 allocation was performed through the hospital pharmacy; in South Africa 2007 research assistants not involved in the care of the women issued consecutive numbers to each participant. For the remaining seven trials, the risk of selection bias due to inadequate allocation concealment was judged as unclear (Angola 1992; Austria 1997; China 1997; Hungary 1979; Hungary 1988; Italy 1994; Mississippi 1992).
Blinding
A placebo was used in six of the 10 trials (Angola 1992; China 1997; Hungary 1988; Italy 1994; Mississippi 1992; South Africa 2007); in Memphis 1989 and Zurich 1988 women in the control group received tablets containing aspartic acid. Blinding of participants, personnel and outcome assessors was judged to be adequate in five of these eight trials (China 1997; Italy 1994; Memphis 1989; Mississippi 1992; South Africa 2007). In Angola 1992 whilst a placebo was used, the placebo and magnesium oxide tablets were distributed in different quantities to the women, and it was unclear if the tablets were identical in appearance; thus the risk of performance and detection bias were judged as unclear. In Hungary 1988 the success of blinding of participants and personnel was also judged as unclear, as while a placebo was used, it was unclear whether this was identical in appearance to the magnesium aspartate tablets, and the leader of the study was able to identify of the composition of the tablets by identification marks.
In Zurich 1988, while the study was described as "double‐blind" and a placebo was used, allocation was based on the participants' date of birth, and thus it was unclear as to whether blinding would have been successfully achieved for personnel, participants and outcome assessors.
Austria 1997 was judged to be at a high risk of performance and detection bias with no blinding of participants, personnel or outcome assessors. In Hungary 1979, while no placebo was used, the translation of the manuscript detailed blind outcome assessment.
Incomplete outcome data
Three of the nine trials were judged to be at a low risk of attrition bias, with no or minimal post‐randomisation exclusions or attrition (China 1997; Hungary 1979; Italy 1994). The remaining seven trials were judged to be at an unclear risk of attrition bias (Angola 1992; Austria 1997; Hungary 1988; Memphis 1989; Mississippi 1992; South Africa 2007; Zurich 1988).
In Angola 1992 post‐randomisation exclusions were not reported. In Austria 1997, 7.5% of women (25 from the treatment group (9.7%) and 15 (5.7%) from the control group) were excluded for a variety of reasons including lack of compliance and gastro‐intestinal problems with supplementation. In Hungary 1988, while only 7/507 and 5/490 women were excluded from the placebo and magnesium groups initially (1.2% total), a further 104/500 (20.8%) were excluded from the placebo group and 85/485 (17.5%) from the magnesium group for a number of reasons including loss to follow‐up. In the Memphis 1989 trial, 11/200 (5.5%) women from the placebo group and 15/200 (7.5%) from the treatment group were excluded as they never started medication. In South Africa 2007, 190 women were excluded post‐randomisation, and a further 204 were lost to follow‐up (394/4476) and it was not possible to determine to which groups these women were randomised. Similarly in Mississippi 1992, it was not possible to ascertain from which group(s) the seven (13%) excluded women were originally assigned. Finally in Zurich 1988, the total number of women in each group were not reported in results tables, and it was thus difficult to determine exclusions or attrition; the manuscript detailed that "For various reasons such as refusal to take further tablets, delivery in other hospitals or abortion, some data were not available for analysis".
Selective reporting
Only one trial was judged to be at a low risk of selective reporting, with data reported for all pre‐specified and/or expected outcomes (Memphis 1989). For the remaining nine trials, the risk of reporting bias was judged to be unclear (Angola 1992; Austria 1997; China 1997; Hungary 1979; Hungary 1988; Italy 1994; Mississippi 1992; South Africa 2007; Zurich 1988), with for example, no pre‐specification of outcomes, important or expected outcomes not reported, or outcome data reported in such a way that it could not be included in a meta‐analysis.
Other potential sources of bias
Five of the trials were judged to be at a low risk of other potential of bias, with no obvious sources of bias identified (Austria 1997; China 1997; Hungary 1979; Italy 1994; Mississippi 1992). For the other trials, this was unclear, for example, with high non‐compliance (Hungary 1988; South Africa 2007).
Effects of interventions
Magnesium supplementation versus no magnesium
Primary outcomes
Infant outcomes
Magnesium supplementation compared with no magnesium supplementation was associated with no significant difference in the risk of perinatal mortality (risk ratio (RR) 1.10; 95% confidence interval (CI) 0.72 to 1.67; five trials, 5903 infants) (Analysis 1.1), or small‐for‐gestational age (RR 0.76; 95% CI 0.54 to 1.07; three trials; 1291 infants; I² = 7%) (Analysis 1.2). For the outcome perinatal mortality, data from the Austria 1997 and Memphis 1989 trials have been included in the meta‐analysis; it should be noted, however, that Austria 1997 only reported on stillbirths (and did not report on neonatal deaths), and Memphis 1989 only reported on neonatal deaths (and did not report on stillbirths). Considering the outcome small‐for‐gestational age, the definition provided in Hungary 1988 and Zurich 1988 was birthweight below the 10th percentile for gestational age; in Memphis 1989, no definition was provided.
1.1. Analysis.
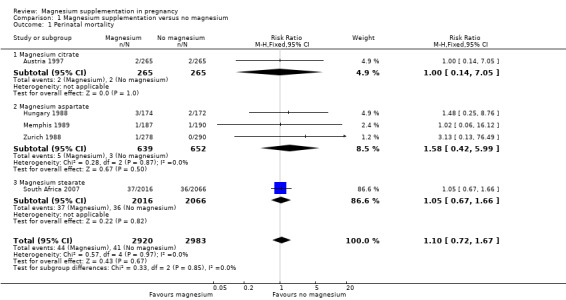
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 1 Perinatal mortality.
1.2. Analysis.
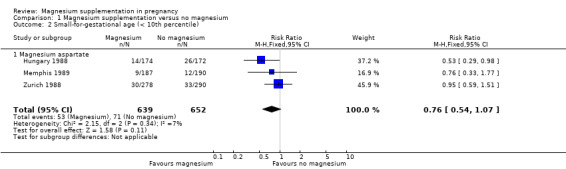
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 2 Small‐for‐gestational age (< 10th percentile).
Maternal outcomes
The effect of magnesium supplementation on maternal death was not reported by any of the included studies. No significant difference in pre‐eclampsia was observed between the magnesium supplemented and control groups (RR 0.87; 95% CI 0.58 to 1.32; three trials, 1042 women) (Analysis 1.3). The definitions for the three trials reporting on pre‐eclampsia varied: in Memphis 1989 pre‐eclampsia was defined as "a systolic blood pressure reading of ≥ 140 mm Hg, diastolic blood pressure of ≥ 90 mm Hg on two occasions at least 6 hours apart with or without proteinuria, or both"; however in Angola 1992, the definition was "the simultaneous occurrence of the clinical triad of hypertension, edema, and proteinuria at any time during the course of pregnancy"; with hypertension defined as "A rise in systolic BP greater than 30 mm Hg and/or a rise in diastolic BP greater than 15 mm Hg"; proteinuria defined as "Protein greater than one determine by test tape" and oedema defined as "Visible fluid accumulation in the ankles and feet; indentation produced by pressure applied by the thumb over the anterior surface of the tibia." In Zurich 1988, the definition was not clear.
1.3. Analysis.
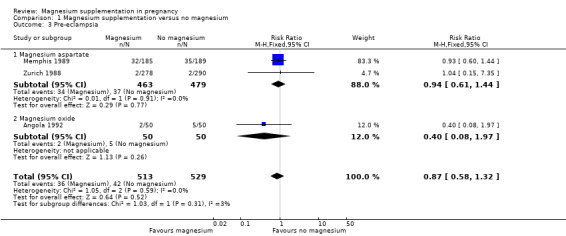
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 3 Pre‐eclampsia.
No statistical heterogeneity was observed in the meta‐analyses for the primary outcomes (I² = 0%), excluding small‐for‐gestational age, where the I² has been reported above.
Secondary outcomes
Infant outcomes
Magnesium supplementation compared with no magnesium supplementation was associated with no significant difference in the risk of stillbirth (risk ratio (RR) 0.73; 95% confidence interval (CI) 0.43 to 1.25; four trials, 5526 infants) (Analysis 1.4), however, a possible increased risk of neonatal death prior to discharge was seen for the group of infants whose mothers had received magnesium supplementation (RR 2.21; 95% CI 1.02 to 4.75; four trials, 5373 infants) (P = 0.04) (Analysis 1.5). The South Africa 2007 trial contributed the majority of participants (more than 70%) to this outcome, with 17 infant deaths occurring in the magnesium supplemented group and seven in the control group. The authors of the South Africa 2007 trial suggested that the large number of severe congenital anomalies in the supplemented group (accounting for seven of the 17 deaths) and the deaths of two sets of twins (with birthweights of less than 750 g) in the supplemented group likely accounted for the increased risk of death observed with magnesium supplementation, and thus this result should be interpreted with caution. When we excluded the seven deaths due to "congential abnormalities incompatible with life" from the meta‐analysis for this outcome, reassuringly, no increased risk of neonatal death was seen for the magnesium supplemented group (RR 1.45; 95% CI 0.63 to 3.32; four trials, 5373 infants) (Analysis 1.5).
1.4. Analysis.
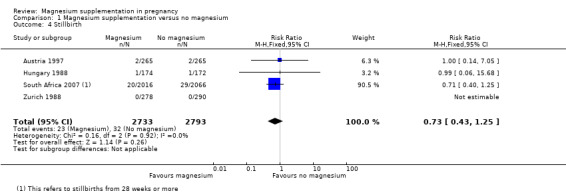
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 4 Stillbirth.
1.5. Analysis.
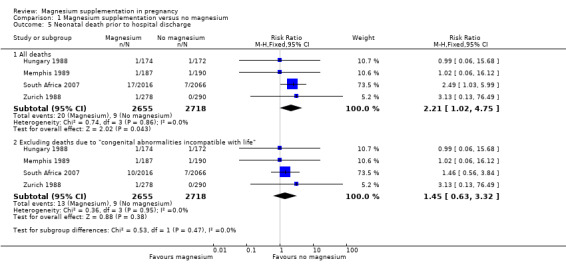
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 5 Neonatal death prior to hospital discharge.
There was no significant difference between the magnesium supplemented group and the control group for the outcome miscarriage (average RR 0.85; 95% CI 0.49 to 1.49; six trials, 3704 women) (Analysis 1.6). As we identified moderate statistical heterogeneity for this outcome (Tau² = 0.19; I² = 44%) a random‐effects model was used. It is possible that the differing types of magnesium supplement (and the differing regimens for administration used) across the six included trials (Austria 1997; Hungary 1979; Hungary 1988; Italy 1994; Memphis 1989; Zurich 1988) contributed to this moderate level of heterogeneity. Similarly, no significant differences between the magnesium supplemented group and the control group were observed for the outcomes gestational age at birth (mean difference (MD) 0.06 weeks; 95% CI ‐0.07 to 0.20; five trials; 5564 women) (Analysis 1.7) and preterm birth (average RR 0.89; 95% CI 0.69 to 1.14; seven trials; 5981 women; Tau² = 0.04; I² = 37%) (Analysis 1.8).
1.6. Analysis.
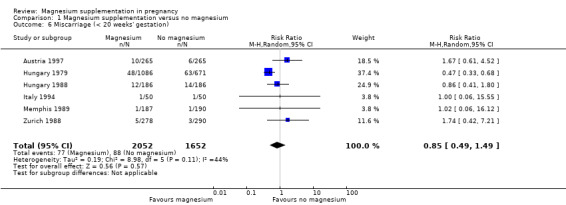
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 6 Miscarriage (< 20 weeks' gestation).
1.7. Analysis.
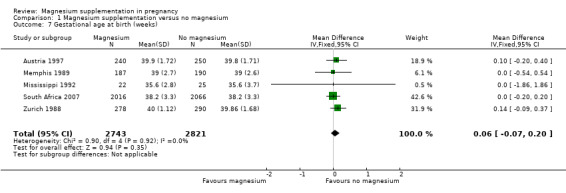
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 7 Gestational age at birth (weeks).
1.8. Analysis.
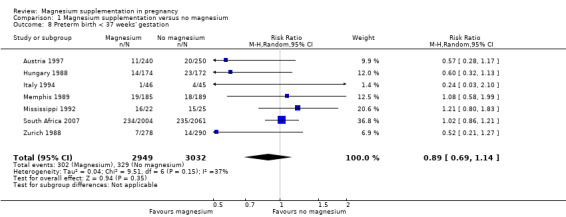
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 8 Preterm birth < 37 weeks' gestation.
Five trials reported on low birthweight infants of less than 2500 g and revealed no significant difference in the incidence of low birthweight with magnesium supplementation (RR 0.95; 95% CI 0.83 to 1.09; 5577 infants) (Analysis 1.9). One trial (Zurich 1988) reported data relating to very low birthweight infants (less than 1500 g), with no observed effect of maternal magnesium supplementation (RR 0.52; 95% CI 0.13 to 2.07). No difference in mean birthweight between the two groups was observed (MD 22.21 g; 95% CI ‐27.23 to 71.65; five trials, 5564 infants) (Analysis 1.10). As we identified moderate statistical heterogeneity for this outcome (Tau² = 1138.34; I² = 38%) a random‐effects model was used.
1.9. Analysis.
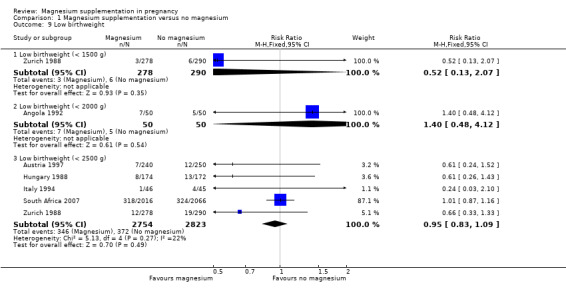
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 9 Low birthweight.
1.10. Analysis.
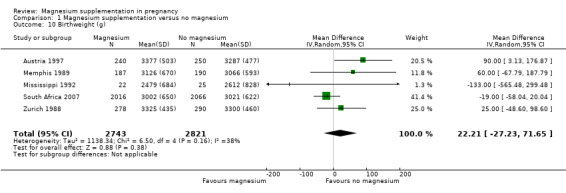
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 10 Birthweight (g).
Magnesium supplementation was not shown to be associated with a difference in admission to the neonatal intensive care unit (RR 0.74; 95% CI 0.50 to 1.11; three trials, 1435 infants) (Analysis 1.11).
1.11. Analysis.
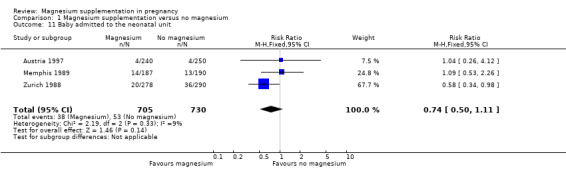
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 11 Baby admitted to the neonatal unit.
Disability at paediatric follow‐up was not reported by any of the included trials.
Non pre‐specified infant outcomes
We have reported data on a number of outcomes relating to neonatal morbidity that were not pre‐specified in the original review protocol, but that we considered to be clinically relevant and important to include in this update.
Magnesium supplementation was not shown to be associated with any differences considering the outcomes of a one‐minute Apgar score less than five (RR 0.83; 95% CI 0.41 to 1.67; one trial, 377 infants) (Analysis 1.12), meconium aspiration (RR 0.63; 95% CI 0.32 to 1.26; one trial, 4082 infants) (Analysis 1.15), breech presentation (RR 1.25; 95% CI 0.81 to 1.92; one trial, 4082 infants) (Analysis 1.16), placental abruption (RR 0.96; 95% CI 0.48 to 1.94; one trial, 4082 infants) (Analysis 1.17), placental weight (MD ‐0.01 g; 95% CI ‐22.16 to 22.14; two trials, 4459 infants; Tau² = 113.95; I² = 36%) (Analysis 1.18), any hypoxic ischaemic encephalopathy (HIE) (RR 0.70; 95% CI 0.36 to 1.34; one trial, 4082 infants), moderate HIE (RR 1.02; 05% CI 0.26 to 4.09; one trial, 4082 infants), severe HIE (RR 2.56; 95% CI 0.50 to 13.19; one trial, 4082 infants) (Analysis 1.19), or significant congenital abnormalities (RR 2.05; 95% CI 0.77 to 5.45; one trial, 4082 infants) (Analysis 1.20).
1.12. Analysis.
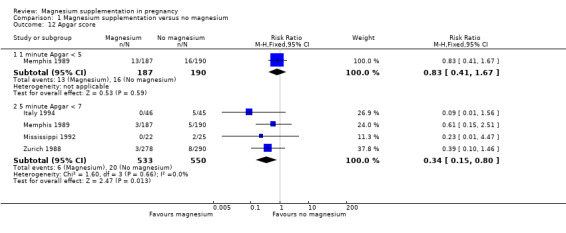
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 12 Apgar score.
1.15. Analysis.
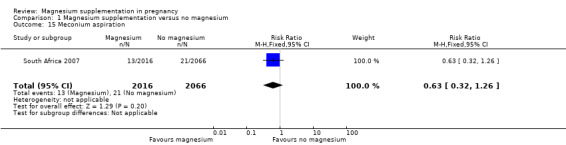
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 15 Meconium aspiration.
1.16. Analysis.
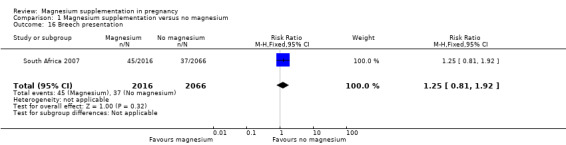
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 16 Breech presentation.
1.17. Analysis.
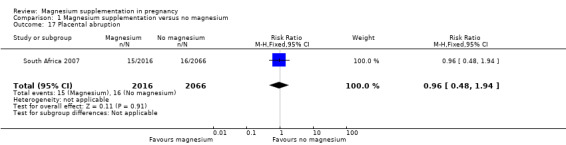
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 17 Placental abruption.
1.18. Analysis.
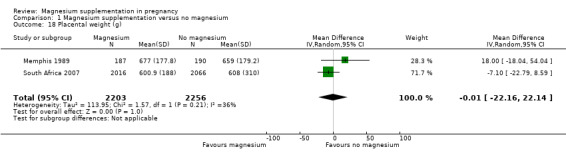
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 18 Placental weight (g).
1.19. Analysis.
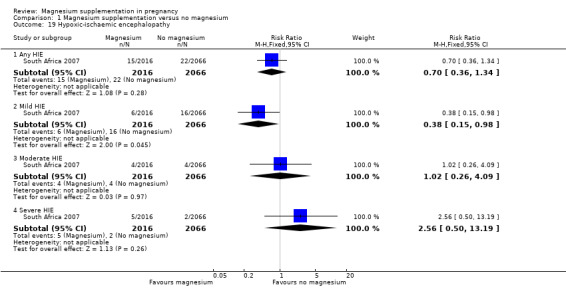
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 19 Hypoxic‐ischaemic encephalopathy.
1.20. Analysis.
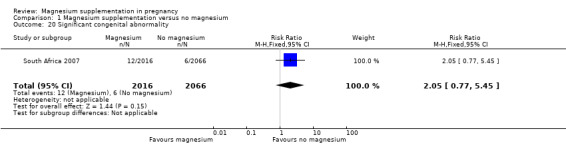
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 20 Significant congenital abnormality.
Magnesium supplementation was, however, shown to reduce the risk of a five‐minute Apgar score less than seven (RR 0.34; 05% CI 0.15 to 0.80; four trials, 1083 infants) (Analysis 1.12). Significant reductions in late fetal heart rate decelerations (RR 0.68; 95% CI 0.53 to 0.88) (Analysis 1.13), meconium‐stained liquor (RR 0.79; 95% CI 0.63 to 0.99) (Analysis 1.14), and mild HIE (RR 0.38; 95% CI 0.15 to 0.98) (Analysis 1.19) were also observed with magnesium supplementation in one trial of 4082 infants (South Africa 2007).
1.13. Analysis.
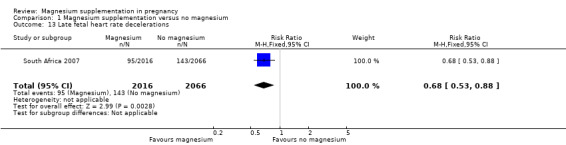
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 13 Late fetal heart rate decelerations.
1.14. Analysis.
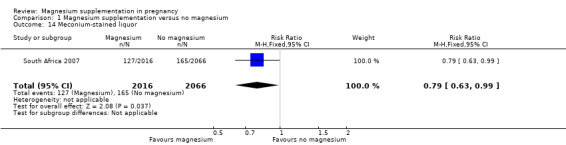
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 14 Meconium‐stained liquor.
Maternal outcomes
There were no data available from any of the trials relating to maternal acceptance of treatment. Of the five trials reporting maternal side effects of treatment (Hungary 1988; Italy 1994; Memphis 1989; Mississippi 1992; Zurich 1988), four reported on gastro‐intestinal symptoms and found no significant difference between the magnesium supplemented group and control group (RR 0.88; 95% CI 0.69 to 1.12; 1388 women) (Analysis 1.21). The Mississippi 1992 trial reported that no women in either group had any side effects.
1.21. Analysis.
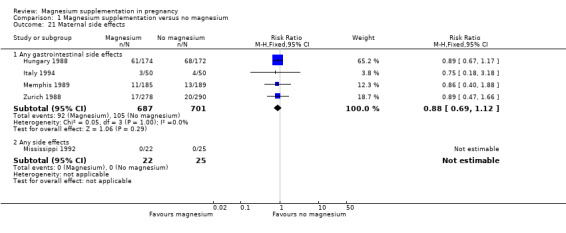
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 21 Maternal side effects.
Magnesium supplementation was associated with a significantly higher systolic blood pressure near birth (MD 1.00 mm Hg; 95% CI 0.03 to 1.97; three trials, 1432 women) (Analysis 1.22), however no significant differences in diastolic blood pressure (MD 0.23 mm Hg; 95% CI ‐0.67 to 1.13; three trials, 1432 women) (Analysis 1.23), or pregnancy‐induced hypertension (average RR 0.39; 95% CI 0.11 to 1.41; three trials, 4284 women) (Analysis 1.24) were observed between groups. Substantial statistical heterogeneity was observed for the outcome pregnancy‐induced hypertension (Tau² = 0.98; I² = 77%), and thus a random‐effects model was used. It is possible that the differing types of magnesium supplement (and the differing regimens for administration used) across the three included trials, or variation between trials in the definitions used for this outcome contributed to this level of heterogeneity (with only the Angola 1992 trial providing a clear definition: a rise in systolic blood pressure > 30 mm Hg and/or a rise in diastolic blood pressure > 15 mm Hg during the course of the pregnancy). Furthermore, the Angola 1992 and China 1997 trials, which showed benefit for the outcome pregnancy‐induced hypertension with magnesium supplementation, were of comparatively small sample sizes (150 and 102 women respectively), and judged to be of a lower quality than the South Africa 2007 trial, of 4476 women, which did not show a difference between groups.
1.22. Analysis.
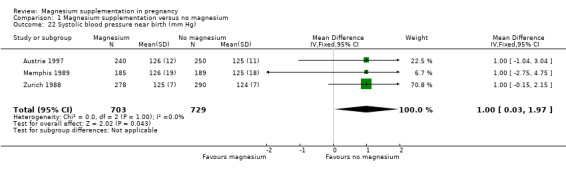
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 22 Systolic blood pressure near birth (mm Hg).
1.23. Analysis.
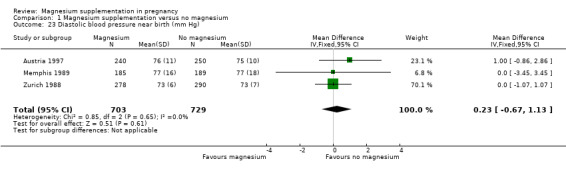
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 23 Diastolic blood pressure near birth (mm Hg).
1.24. Analysis.
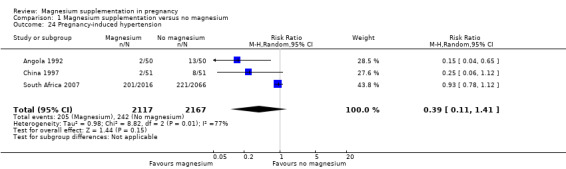
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 24 Pregnancy‐induced hypertension.
Three trials assessed the need for maternal hospitalisation and demonstrated a reduced need with magnesium supplementation compared with no treatment (RR 0.65; 95% CI 0.48 to 0.86; 1158 women) (Analysis 1.26). No difference between magnesium supplementation and no treatment was shown for the outcomes eclampsia (RR 0.14; 95% CI 0.01 to 2.70; one trial, 100 women) (Analysis 1.25), length of labour (MD ‐0.00 hours; 95% CI ‐0.50 to 0.50; two trials, 4650 women) (Analysis 1.28) or antepartum haemorrhage (average RR 0.53; 95% CI 0.09 to 3.15; two trials. 942 women) (Analysis 1.27). It is possible that the Zurich 1988 trial's low quality (being quasi‐randomised, with unclear blinding) contributed to the substantial statistical heterogeneity observed for the outcome antepartum haemorrhage (Tau² = 1.12; I² = 67%).
1.26. Analysis.
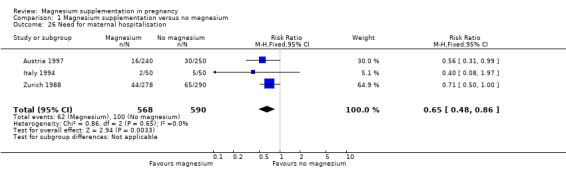
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 26 Need for maternal hospitalisation.
1.25. Analysis.
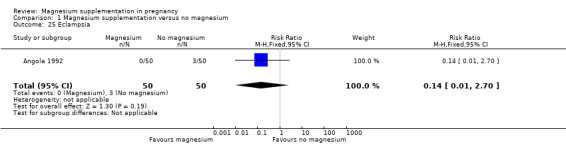
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 25 Eclampsia.
1.28. Analysis.
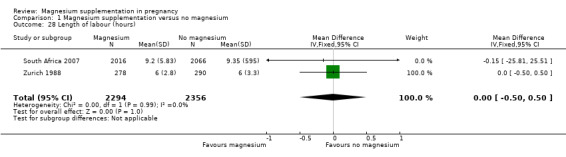
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 28 Length of labour (hours).
1.27. Analysis.
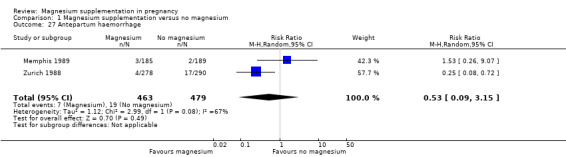
Comparison 1 Magnesium supplementation versus no magnesium, Outcome 27 Antepartum haemorrhage.
The incidence of postpartum haemorrhage was not reported by the included studies.
Subgroup analysis based on type of magnesium supplement
Subgroup analysis based on the type of magnesium supplement used, revealed no subgroup differences for the outcome perinatal mortality (Chi² = 0.33; P = 0.85; I² = 0%) (Analysis 1.1). We were not able to perform a subgroup analysis for small‐for‐gestational age, as all the trials that reported on this outcome used magnesium aspartate (Analysis 1.2).
Similarly, subgroup analysis based on the type of magnesium supplement used revealed no subgroup differences for pre‐eclampsia (Chi² = 1.03; P = 0.31; I² = 3.1%) (Analysis 1.3).
Subgroup analysis based on study design
Subgroup analysis based on the study designed used (cluster‐randomised versus individually‐randomised), revealed no subgroup differences for the primary outcomes, perinatal mortality (Chi² = 0.12; P = 0.73; I² = 0%) (Analysis 2.1), and small‐for‐gestational age (Chi² = 1.93; P = 0.16; I² = 48.3%) (Analysis 2.2). We were not able to perform a subgroup analysis for pre‐eclampsia, as the three trials that reported on this outcome were all individually‐randomised.
2.1. Analysis.
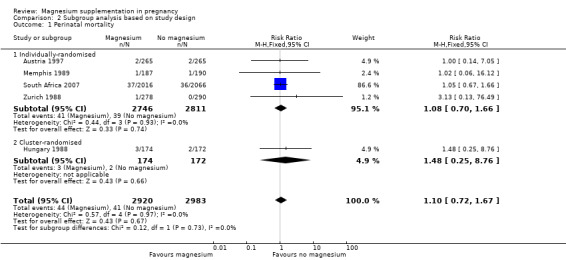
Comparison 2 Subgroup analysis based on study design, Outcome 1 Perinatal mortality.
2.2. Analysis.
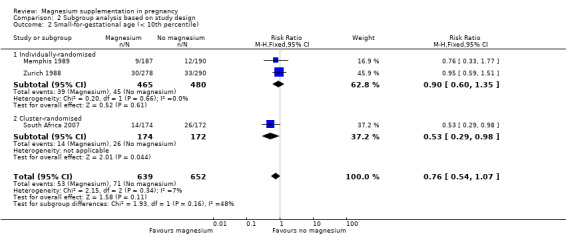
Comparison 2 Subgroup analysis based on study design, Outcome 2 Small‐for‐gestational age (< 10th percentile).
Sensitivity analysis ‐ varying the ICC for the cluster‐randomised trial
We conducted a sensitivity analysis using less conservative estimates of the ICC for mortality outcomes (0.0002, 0.002) (less conservative when considering the ICC of 0.02 used throughout the main analysis). Although selecting less conservative ICC values (assuming less clustering and thereby increasing the weight of the one included cluster‐randomised trial (Hungary 1988)) narrowed the confidence intervals slightly, overall this did not have a serious impact on the findings (Analysis 3.1; Analysis 3.2; Analysis 3.3).
3.1. Analysis.
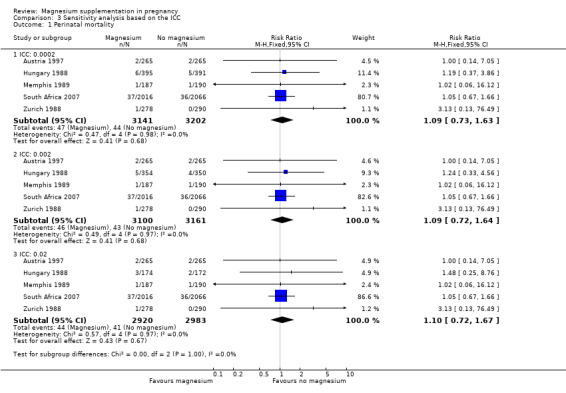
Comparison 3 Sensitivity analysis based on the ICC, Outcome 1 Perinatal mortality.
3.2. Analysis.
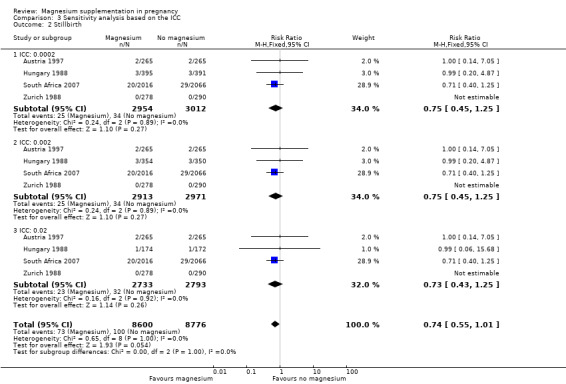
Comparison 3 Sensitivity analysis based on the ICC, Outcome 2 Stillbirth.
3.3. Analysis.
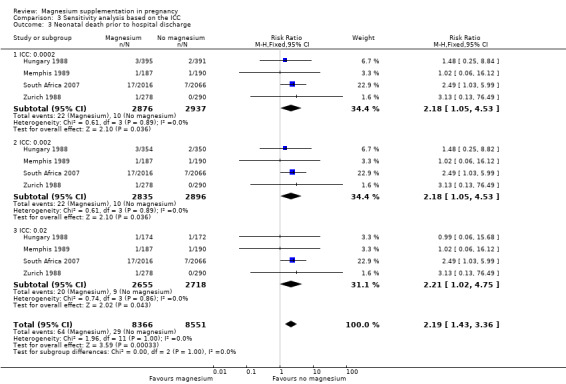
Comparison 3 Sensitivity analysis based on the ICC, Outcome 3 Neonatal death prior to hospital discharge.
Sensitivity analysis by quality rating
Only two trials had an allocation concealment and sequence generation rating of 'low risk of bias' (Memphis 1989; South Africa 2007). The sensitivity analysis excluded trials with an allocation concealment and/or sequence generation rating of 'unclear' or 'high risk of bias.' Among the 'high quality studies' there were no significant differences between the magnesium supplemented group and control group for the outcomes perinatal mortality (RR 1.05; 95% CI 0.67 to 1.65; two trials, 4459 infants) (Analysis 4.1) small‐for‐gestational age (RR 0.76; 95% CI 0.33 to 1.77; one trial, 377 infants) (Analysis 4.2) or pre‐eclampsia (RR 0.93; 95% CI 0.60 to 1.44; one trial, 374 women) (Analysis 4.3), as in the main analysis.
4.1. Analysis.
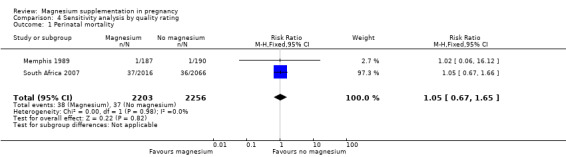
Comparison 4 Sensitivity analysis by quality rating, Outcome 1 Perinatal mortality.
4.2. Analysis.
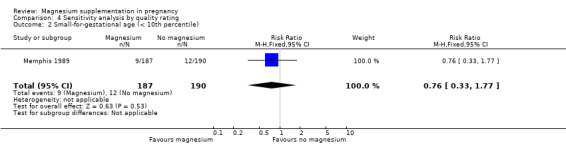
Comparison 4 Sensitivity analysis by quality rating, Outcome 2 Small‐for‐gestational age (< 10th percentile).
4.3. Analysis.
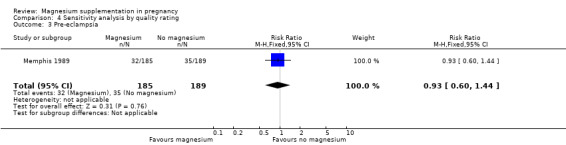
Comparison 4 Sensitivity analysis by quality rating, Outcome 3 Pre‐eclampsia.
Discussion
Summary of main results
The meta‐analysis of trials included in this review indicated no statistically significant effects of magnesium supplementation on the frequency of perinatal mortality or small‐for‐gestational age infants when compared with placebo or no treatment. Similarly, the results of this review indicated that magnesium supplementation during pregnancy had no significant effect on pre‐eclampsia; maternal deaths were not reported by the included trials.
For secondary outcomes, many of the included studies did not provide data, and where they did, mostly we did not detect differences between the magnesium supplemented and control groups. It is important to note that for some outcomes, the definitions used by individual trials were unclear and/or varied, such as for the outcomes pre‐eclampsia, small‐for‐gestational age and pregnancy‐induced hypertension. Some results did appear to show differences between the groups.
Magnesium supplementation was shown to result in fewer maternal hospitalisations during pregnancy; and while higher maternal systolic blood pressure near birth was shown for the magnesium supplemented group of women, this observed mean difference in blood pressure of 1 mm Hg is considered unlikely to be clinically significant. For both outcomes the Zurich 1988 trial significantly influenced the meta‐analysis; and as this trial was of low quality, being quasi‐randomised with women allocated according to their date of birth, and thus these findings should be interpreted with caution. While no significant difference between groups was shown for the outcome stillbirth, on meta‐analysis, a possible increased risk of neonatal death prior to discharge was observed for infants born to mothers who had received magnesium supplementation. It is important to highlight that only four of the 10 trials included in this review reported data to include in the meta‐analysis for this outcome. Furthermore, in the South Africa 2007 trial (which contributed over 70% of the participants to the analysis for this outcome), the trial authors documented a high number of severe congenital anomalies in the supplemented group (unlikely attributable to magnesium, as none of these seven infants had been exposed to magnesium prior to the 19th week of gestation) and the deaths of two sets of twins (with birthweights of less than 750 g) in the supplemented group. When the deaths due to "congenital abnormalities incompatible with life" (including thanatophoric dwarf, anencephaly, hypoplastic left heart, hypoplastic lungs, and multiple abnormalities) were excluded from the meta‐analysis for this outcome, reassuringly, no increased risk of neonatal death was seen for the magnesium supplemented group.
When only high‐quality trials were included in the analysis, there was no effect of magnesium supplementation on the frequency of perinatal mortality, small‐for‐gestational age, or pre‐eclampsia (Memphis 1989; South Africa 2007). One of the highest quality trials, Memphis 1989, of 400 women, demonstrated no effect of maternal magnesium supplementation on blood pressure, pre‐eclampsia or other pregnancy outcomes. The results of this trial may have however been influenced by the fact that all women (both magnesium supplemented and placebo groups) received a multivitamin and mineral preparation containing 100 mg of magnesium. For the outcomes small‐for‐gestational age and pre‐eclampsia, only the Memphis 1989 trial reported data for inclusion in the sensitivity analysis, and this study was underpowered to detect differences between groups for both of these outcomes, with considerable uncertainly about the treatment effects observed; unfortunately the South Africa 2007, of over 4000 women, did not report on small‐for‐gestational age or pre‐eclampsia.
The South Africa 2007 trial found no difference in meconium aspiration, breech presentation, placental abruption, congenital abnormalities, moderate or severe hypoxic ischaemic encephalopathy (HIE) and neonatal encephalopathy between the magnesium supplemented and placebo groups however it found that magnesium supplementation reduced the risk of late fetal heart decelerations, meconium‐stained liquor and mild HIE (South Africa 2007). These outcomes relating to infant morbidity were not pre‐specified in the original protocol for the review, and while the review authors believed their reporting in this update to be important, they acknowledge the potential for bias associated with the reporting of non pre‐specified review outcomes.
Quality of the evidence
There is a lack of high‐quality evidence assessing the use of magnesium supplementation during pregnancy. Only two trials were judged to be at a low risk of selection bias, with adequate methods to conceal allocation and to generate a random sequence (Memphis 1989; South Africa 2007); the remaining trials were largely judged to be at an unclear risk of selection bias. Only four of the 10 trials were judged at a low risk of both performance and detection bias (Italy 1994; Memphis 1989; Mississippi 1992; South Africa 2007), and for the Austria 1997 trial, the risk of performance and detection bias was judged as high, with no control/placebo treatment used. The majority of trials were judged at an unclear risk of attrition bias and reporting bias.
Potential biases in the review process
The evidence for this review is derived from trials identified through a detailed search process. It is possible (but unlikely) that additional trials assessing magnesium supplementation during pregnancy, have been published but not identified. It is also possible that other studies have been conducted but not published. Should such studies be identified, we will include them in future updates of this review.
Authors' conclusions
Implications for practice.
There is currently no evidence to support magnesium supplementation during pregnancy for improving maternal and neonatal/infant health outcomes. Until additional evidence from large, well‐designed randomised trials becomes available, current evidence is insufficient to make recommendations for routine clinical practice on the use of magnesium supplementation during pregnancy.
Implications for research.
In light of the limited current evidence, further randomised controlled trials may be warranted to determine whether supplementation with magnesium during pregnancy can improve maternal and neonatal/infant health outcomes. Such trials must be sufficiently powered, and well‐designed to allow important differences to be detected. Future research must consider relevant maternal and neonatal/infant outcomes (including reporting on maternal and perinatal mortality), as well as longer‐term paediatric outcomes (including disabilities). In addition to assessing effectiveness and safety, such trials may address specific considerations including timing of commencement of supplementation and dosage.
Feedback
Gelband, April 2000
Summary
Methods of the review: The largest trial in this review, Hungary 1998, was a cluster randomised trial with clinics as the unit of randomisation. The data appear to have been entered as though randomisation was by individual, without any adjustment for the cluster design. This is of particular concern as some results ware borderline for statistical significance, which might not be the case if the data were adjusted for cluster design.
[Summary of comments from Hellen Gelband, April 2000]
Reply
The review now includes two meta‐analyses, one including the Hungrian trial and one excluding the Hungarian trial. We preferred this approach to the total exclusion of the Hungarian trial because it is the largest trial included in the review. When the Hungarian trial is excluded from the meta‐analysis, three of six outcomes that were significantly different between treatment and placebo when all trials are included are no longer different. These outcomes are the frequency of preterm birth (< 37 weeks' gestation), the frequency of low birthweight and the frequency of small for gestational age. These findings are discussed in the review.
[Summary of response from Maria Makrides, Caroline Crowther and Simon Gates, June 2001]
Contributors
Hellen Gelband
What's new
| Date | Event | Description |
|---|---|---|
| 9 May 2019 | Amended | Edited Declarations of interest section. |
History
Protocol first published: Issue 1, 1998 Review first published: Issue 2, 1998
| Date | Event | Description |
|---|---|---|
| 3 September 2013 | New search has been performed | We have included three new trials (Hungary 1979; Italy 1994; South Africa 2007), and have excluded nine studies (Denmark 1990; Denmark 1991; Detroit 1999; India 2012; ISRCTN03989660; NCT01709968; Norway 2008; Sweden 1987; Sweden 1995). Two trials have been classified as ongoing (ISRCTN98365455; NCT01510665). |
| 3 September 2013 | New citation required and conclusions have changed | New evidence incorporated. In this update there is now some evidence of an effect for magnesium on the secondary outcomes of neonatal death prior to discharge, Apgar score less than seven at five minutes, meconium‐stained liquor, fetal heart rate deceleration and mild hypoxic ischaemic encephalopathy. There is now no evidence of an effect for magnesium supplementation on the primary outcome small‐for‐gestational age and secondary outcomes of preterm birth at less than 37 weeks, low birthweight and antepartum haemorrhage. |
| 11 September 2012 | New search has been performed | Contact details updated. |
| 1 October 2009 | Amended | Search updated. Fifteen reports added to Studies awaiting classification. |
| 17 September 2008 | Amended | Converted to new review format. |
| 24 July 2001 | New citation required and conclusions have changed | Substantive amendment. |
| 17 July 2001 | New search has been performed | Addition of primary paper of Austrian trial (Austria 1997), addition of Chinese trial (China 1997), additional meta‐analysis with the exclusion of Hungarian trial (Hungary 1988) based on comment/criticism. |
Acknowledgements
We thank Cordula Blank for translation of German papers, Emily Lemon and Esther Vitalis for the translations of a Hungarian papers, Wengxiong Chen and Sarah Dodd for translations of the Chinese paper and Louise Flanagan for the translation of the Austrian paper.
Marc JNC Keirse compiled an earlier version of this review published in the Oxford Database of Perinatal Trials.
We thank Lynn Hampson who performed the literature searches and Philippa Middleton who commented on all drafts.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team) and the Group's Statistical Adviser.
Appendices
Appendix 1. Methods used in the previous version of this review
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (June 2001). We updated this search on 1 October 2009 and added the results to Studies awaiting classification. The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
handsearches of 30 journals and the proceedings of major conferences
weekly current awareness alerts for a further 44 journals
plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL and MEDLINE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
In addition, we searched The Cochrane Controlled Trials Register using the terms: magnesium and pregnan* or pre‐eclamp* or pre eclamp* or preeclamp* or hypertens* or preterm or premature. The Controlled Trials Register was last searched in June 2001. We did not apply any language restrictions.
Data collection and analysis
Included trial data were processed as described in Clarke 2000. Trials under consideration were evaluated for inclusion and methodological quality, without consideration of their results. This was separately assessed by each author. Discrepancies were resolved by discussion. There was no blinding of authorship.
Quality scores for concealment of allocation were assigned to each trial, using the criteria described in Section 6 of the Cochrane Handbook (Clarke 2000). A = adequate, B = unclear, C = inadequate, D = not used.
In addition, quality scores were assigned to each trial for use of placebo, blinding of outcome assessment and completeness of follow‐up as follows:
Use of placebo: (A) placebo ‐ yes; (B) placebo attempted; (C) no placebo; (D) unclear.
For blinding of assessment of outcome: (A) Double‐blind, neither investigator nor participant knew or were likely to guess the allocated treatment. (B) Single‐blind, either the investigator or the participant knew the allocation. Or, the trial is described as double‐blind but side effects of one or other treatment mean that it is likely that for a significant proportion (</= 20%) of participants the allocation could be correctly identified. (C) No blinding, both investigator and participant knew (or were likely to guess) the allocated treatment. (D) Unclear.
Completeness of follow‐up: (A) < 3% of participants excluded; (B) 3% ‐ 9.9% of participants excluded; (C) 10% ‐ 19.9% of participants excluded; (D) 20% or more of participants excluded; (E) unclear.
Data were independently extracted by the two reviewers and double entered. Discrepancies were resolved by discussion. Whenever possible, unpublished data were sought from investigators.
All eligible trials were included in the initial analysis. Sensitivity analysis was planned to evaluate the effect of trial quality by including trials given quality scores of A for allocation concealment, use of placebo, and blinding of primary outcome assessment and an A or B score for completeness of follow‐up.
The meta‐analysis was conducted using a fixed‐effect model (Meta‐View 4.1). Summary statistics for dichotomous variables are reported as relative risk (RR) with 95% confidence intervals, while summary statistics for continuous variables are reported as weighted mean difference with 95% confidence intervals.
Data and analyses
Comparison 1. Magnesium supplementation versus no magnesium.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Perinatal mortality | 5 | 5903 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.72, 1.67] |
| 1.1 Magnesium citrate | 1 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 7.05] |
| 1.2 Magnesium aspartate | 3 | 1291 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.42, 5.99] |
| 1.3 Magnesium stearate | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.67, 1.66] |
| 2 Small‐for‐gestational age (< 10th percentile) | 3 | 1291 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.54, 1.07] |
| 2.1 Magnesium aspartate | 3 | 1291 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.54, 1.07] |
| 3 Pre‐eclampsia | 3 | 1042 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.58, 1.32] |
| 3.1 Magnesium aspartate | 2 | 942 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.61, 1.44] |
| 3.2 Magnesium oxide | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.97] |
| 4 Stillbirth | 4 | 5526 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.43, 1.25] |
| 5 Neonatal death prior to hospital discharge | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 All deaths | 4 | 5373 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [1.02, 4.75] |
| 5.2 Excluding deaths due to "congenital abnormalities incompatible with life" | 4 | 5373 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.63, 3.32] |
| 6 Miscarriage (< 20 weeks' gestation) | 6 | 3704 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.49, 1.49] |
| 7 Gestational age at birth (weeks) | 5 | 5564 | Mean Difference (IV, Fixed, 95% CI) | 0.06 [‐0.07, 0.20] |
| 8 Preterm birth < 37 weeks' gestation | 7 | 5981 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.69, 1.14] |
| 9 Low birthweight | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Low birthweight (< 1500 g) | 1 | 568 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.13, 2.07] |
| 9.2 Low birthweight (< 2000 g) | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.4 [0.48, 4.12] |
| 9.3 Low birthweight (< 2500 g) | 5 | 5577 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.83, 1.09] |
| 10 Birthweight (g) | 5 | 5564 | Mean Difference (IV, Random, 95% CI) | 22.21 [‐27.23, 71.65] |
| 11 Baby admitted to the neonatal unit | 3 | 1435 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.50, 1.11] |
| 12 Apgar score | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 1 minute Apgar < 5 | 1 | 377 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.41, 1.67] |
| 12.2 5 minute Apgar < 7 | 4 | 1083 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.15, 0.80] |
| 13 Late fetal heart rate decelerations | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.53, 0.88] |
| 14 Meconium‐stained liquor | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.63, 0.99] |
| 15 Meconium aspiration | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.32, 1.26] |
| 16 Breech presentation | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.81, 1.92] |
| 17 Placental abruption | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.48, 1.94] |
| 18 Placental weight (g) | 2 | 4459 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐22.16, 22.14] |
| 19 Hypoxic‐ischaemic encephalopathy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Any HIE | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.36, 1.34] |
| 19.2 Mild HIE | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.15, 0.98] |
| 19.3 Moderate HIE | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.26, 4.09] |
| 19.4 Severe HIE | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.56 [0.50, 13.19] |
| 20 Significant congenital abnormality | 1 | 4082 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.77, 5.45] |
| 21 Maternal side effects | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 Any gastrointestinal side effects | 4 | 1388 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.69, 1.12] |
| 21.2 Any side effects | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Systolic blood pressure near birth (mm Hg) | 3 | 1432 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [0.03, 1.97] |
| 23 Diastolic blood pressure near birth (mm Hg) | 3 | 1432 | Mean Difference (IV, Fixed, 95% CI) | 0.23 [‐0.67, 1.13] |
| 24 Pregnancy‐induced hypertension | 3 | 4284 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.11, 1.41] |
| 25 Eclampsia | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.70] |
| 26 Need for maternal hospitalisation | 3 | 1158 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.48, 0.86] |
| 27 Antepartum haemorrhage | 2 | 942 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.09, 3.15] |
| 28 Length of labour (hours) | 2 | 4650 | Mean Difference (IV, Fixed, 95% CI) | ‐0.00 [‐0.50, 0.50] |
Comparison 2. Subgroup analysis based on study design.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Perinatal mortality | 5 | 5903 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.72, 1.67] |
| 1.1 Individually‐randomised | 4 | 5557 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.70, 1.66] |
| 1.2 Cluster‐randomised | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.25, 8.76] |
| 2 Small‐for‐gestational age (< 10th percentile) | 3 | 1291 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.54, 1.07] |
| 2.1 Individually‐randomised | 2 | 945 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.60, 1.35] |
| 2.2 Cluster‐randomised | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.29, 0.98] |
Comparison 3. Sensitivity analysis based on the ICC.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Perinatal mortality | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 ICC: 0.0002 | 5 | 6343 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.73, 1.63] |
| 1.2 ICC: 0.002 | 5 | 6261 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.72, 1.64] |
| 1.3 ICC: 0.02 | 5 | 5903 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.72, 1.67] |
| 2 Stillbirth | 4 | 17376 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.55, 1.01] |
| 2.1 ICC: 0.0002 | 4 | 5966 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.45, 1.25] |
| 2.2 ICC: 0.002 | 4 | 5884 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.45, 1.25] |
| 2.3 ICC: 0.02 | 4 | 5526 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.43, 1.25] |
| 3 Neonatal death prior to hospital discharge | 4 | 16917 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.19 [1.43, 3.36] |
| 3.1 ICC: 0.0002 | 4 | 5813 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [1.05, 4.53] |
| 3.2 ICC: 0.002 | 4 | 5731 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [1.05, 4.53] |
| 3.3 ICC: 0.02 | 4 | 5373 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [1.02, 4.75] |
Comparison 4. Sensitivity analysis by quality rating.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Perinatal mortality | 2 | 4459 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.67, 1.65] |
| 2 Small‐for‐gestational age (< 10th percentile) | 1 | 377 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.33, 1.77] |
| 3 Pre‐eclampsia | 1 | 374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.60, 1.44] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Angola 1992.
| Methods | Randomised controlled trial. | |
| Participants | 150 women completed the study; 100 women from the placebo and magnesium oxide groups (50 from another treatment group). Setting: Maternidade Central de Luanda, Angola from 1986 to 1987. Inclusion criteria: “150 women were selected from a population of similar ethnic background and socio‐economic status.” Women were primiparous and multiparous, aged 14 to 40 years, and had to be in the first 4 months of pregnancy to be eligible. Exclusion criteria: none detailed. Whilst not specified, the trial was designed for the prevention of pre‐eclampsia, thus it was assumed that no woman had pre‐eclampsia at randomisation. Other: considering the 150 women: 67% had a history of malaria or fever of unknown origin; 77% had a history of anaemia; 34% personal or family history of sickle cell trait or disease. |
|
| Interventions | There were 3 study groups; for the purpose of the review 2 groups were considered. Treatment group (n = 50) Women received 60 tablets per month or 2 per day (500 mg magnesium oxide). Control group (n = 50) Women received 240 placebo capsules at the start of the study period (8 per day) containing olive oil without vitamin E. |
|
| Outcomes | Adverse effects of supplements; weight gain between the 1st and 3rd trimesters; pregnancy‐associated hypertension (increase in systolic blood pressure > 30 mmHg and/or increase in diastolic blood pressure > 15 mmHg); oedema; proteinuria; pre‐eclampsia (hypertension, oedema and proteinuria); severe pre‐eclampsia with 1 or 2 convulsions; babies’ condition (after 24 hours: skin colour, heart rate, respiratory effort and muscle tone); birthweight (> 3000 g; < 2000 g). | |
| Notes | The trial was designed for the prevention of pre‐eclampsia. There was no sample size calculation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised using a table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not detailed. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The trial was described as "partially double‐blinded" with the magnesium oxide tablets having a different appearance to the oil‐containing capsules. The code of the capsules was not known to the manufacturer until the end of the treatment period. Women in groups 1 (placebo) and 2 (primrose oil and fish oil) received 240 capsules at the beginning of the supplementation period (eight per day), whereas women in group 3 (magnesium) received 60 tablets per month (2 per day). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding of outcome assessment not detailed; however considered unlikely to have been effective in view of the differing interventions. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Post‐randomisation exclusions not stated. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes were not pre‐specified in the methods, and for some outcomes such as adverse effects only P values were reported (with no event values per group reported). |
| Other bias | Unclear risk | The placebo group had significantly better dietary intake than the treatment group and the magnesium oxide group had poor pregnancy weight gain at baseline. |
Austria 1997.
| Methods | Randomised controlled trial. | |
| Participants | 530 women were randomised. Setting: Obstetric and Gynaecological University Clinic, Graz, Austria from 1993 to 1996. Inclusion criteria: women with “non‐risk” pregnancies, recruited before their 18th week of pregnancy. Exclusion criteria: women with serious pre‐existing conditions, IVF, multiple pregnancy, uterine abnormalities, historical tendency towards preterm labour, hypertensive pregnancy‐related illness were excluded. |
|
| Interventions |
Treatment group (n = 265) Women were given oral magnesium citrate supplements (365 mg (15 mmol) once daily) from recruitment (< 18 weeks' gestation) until hospitalisation from 38 weeks due to contractions or rupture of membranes. Control group (n = 265) No placebo supplement was used. |
|
| Outcomes | Threatened preterm labour (and cervical changes before 37 weeks); hospitalisation due to threatened preterm labour; duration of hospitalisation; use of cerclage, pessaries, parental tocolysis; spontaneous delivery; caesarean section; forceps birth; gestational age at birth; premature rupture of membranes; administration of oxytocin; birthweight; birth length; preterm birth (< 37 weeks); birthweight < 2500 g; admission to the neonatal intensive care unit. Additional outcomes reported in text included: Apgar score; umbilical arterial and venous pH; rate of infections requiring treatment (maternal); pregnancy induced hypertension. | |
| Notes | No sample size calculation presented. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation according to a computer‐generated randomisation list. |
| Allocation concealment (selection bias) | Unclear risk | Not detailed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7.5% (40/530) post‐randomisation exclusions. 25 women from the treatment group and 15 women from the control group were excluded due to lack of adherence, termination of pregnancy, GI problems with supplementation, controls treated with magnesium for cramps, spontaneous abortion, intrauterine fetal death, missed abortion. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to determine (from translation). |
| Other bias | Low risk | There was no significant difference between the magnesium and control groups at baseline. No other obvious risk of bias sources identified. |
China 1997.
| Methods | Randomised controlled trial. | |
| Participants | 102 women were included. Setting: The Third Hospital of Beijing Medical University, Beijing from 1994 to 1996. Inclusion criteria: first time mothers with singleton pregnancies. Exclusion criteria: women with heart or kidney problems, with high blood pressure or a history of diabetes were excluded. There were 50 women with normal pregnancies and 52 with high‐risk pregnancies (normal pregnancies: 28 women in control group, 22 women in treatment group; high‐risk pregnancies: 23 women in control group, 29 women in treatment group). Other: women were aged between 24 and 35 years and at 22 and 41 weeks' gestation. |
|
| Interventions |
Treatment group (for high‐ and low‐risk pregnancies) (n = 51) Women were given 2 g per day magnesium gluconate from 28 weeks' gestation to 30 weeks and then 3 g per day magnesium gluconate from 30 weeks until delivery. Control group (for high‐ and low‐risk pregnancies) (n = 51) Women received the same regimen as the treatment group, but of a placebo. |
|
| Outcomes | Pregnancy‐induced hypertension; 6‐keto‐PGF1α, TXB2, 6‐keto/TXB2 ratio; serum magnesium. | |
| Notes | No sample size calculation presented. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Random allocation" ‐ method not stated. Separate randomisation for high‐risk and low‐risk pregnancies. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo used. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment (from translation). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No post‐randomisation exclusions. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to determine (from translation). |
| Other bias | Low risk | No other obvious risk of bias evident. |
Hungary 1979.
| Methods | Randomised controlled trial. | |
| Participants | 1763 women were randomised. Setting: Hungary. Inclusion criteria: pregnant women. No further details provided. |
|
| Interventions |
Treatment group 1 (group II) (n = 407) Women received a magnesium supplement from the 4th to the 9th week of pregnancy. Treatment group 2 (group III) (n = 682) Women received a magnesium supplement from weeks 10 to 27 of their pregnancy. Control group (group I) (n = 674) Women received no magnesium supplementation. The preparation of magnesium citrate used contained 16 mg per g of magnesium citrate. |
|
| Outcomes | Miscarriage. | |
| Notes | No sample size calculation presented. An additional paper presents further data relating to women included in this trial. The outcomes reported included: duration of gestation; infant weight (and birthweight < 2500 g; > 3000 g); infant size measurements and head circumference. This paper concluded that magnesium supplementation increased the duration of gestation, birthweight, length at birth and head circumference, however we were unable to extract the data to include in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not stated; quote "By randomisation, 3 groups were determined". |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo was used. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment (from translation). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Post‐randomisation exclusion of 6 women (0.3%) because they moved away from the area where the study was being conducted (placebo group: 3 women; magnesium < 9th week group: 1 woman; magnesium between 10 to 27 weeks: 2 women). |
| Selective reporting (reporting bias) | Unclear risk | Miscarriage was the only outcome presented. |
| Other bias | Low risk | No other bias reported. |
Hungary 1988.
| Methods | Cluster‐randomised controlled trial. | |
| Participants | 997 women were enrolled. Setting: 15 pregnancy clinics run by the city of Szeged, the Medical Faculty of Szeged University, and the Obstetrics and Gynaecology ward of the Municipal Hospital of Szeged from 1984 to 1985. Inclusion criteria: women with singleton pregnancies. Exclusions: multiple pregnancies. |
|
| Interventions |
Treatment group (n = 490; 485 treated) Women received 1 tablet of 5 mmol magnesium aspartate 3 times per day (15 mmol per day). The tablets were chewable. Control group (n = 507; 500 treated) Women received placebo tablets (the content of the tablets were not reported). Treatment began between 6 to 21 weeks and lasted until birth. |
|
| Outcomes | Perinatal mortality (antenatal, during delivery, postnatal)/miscarriage; preterm birth (< 285 days); duration of gestation; birthweight percentiles (e.g. < 10th percentile); low birthweight (< 2500 g); EPH gestosis. | |
| Notes | No sample size calculation presented. We were unable to include the data relating to "EPH gestosis" as this was reported for 1321 women in the magnesium group and 1089 in the placebo group according to the translation, which was considered incorrect given that this far exceed the total number of women in the trial. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation by centre ‐ 8 "magnesium" centres, 7 placebo centres. Method not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | A placebo was used however the composition of placebo not reported. Only the leader of the study knew the composition of the magnesium/placebo tablet bottles – there were identification marks on the tablets known to the leader of the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment (as per translations). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7/507 (1.4%) women from the placebo group and 5/490 (1.0%) from the magnesium group were excluded initially (in total 12/997 (1.2%) were excluded). 4 were not pregnant, 7 were multiple pregnancies and 1 pregnancy was terminated due to anencephaly. A further 104/500 (20.8%) women were excluded from the placebo group and 85/485 (17.5%) women were excluded from the magnesium group. 189/985 (19.2%) women were excluded in total due to miscarriage, death of the infant prior to discharge or loss to follow‐up. No significant difference was found in exclusions between the magnesium and placebo groups. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to determine (from translation). |
| Other bias | Unclear risk | High non‐adherence rate. Difficult to determine other bias due to translation. |
Italy 1994.
| Methods | Randomised controlled trial. | |
| Participants | 100 women were included. Setting: Italy. Inclusion criteria: primigravidas, of not more than 12 weeks' gestation (aged 18 to 28 years old). |
|
| Interventions |
Treatment group (n = 50) Women received 15 mmol magnesium hydrochlorate aspartate. Control group (n = 50) Women received a placebo. |
|
| Outcomes | Arterial pressure; maternal weight gain; hospitalisation rate; duration of pregnancy; premature labour; 5‐minute Apgar index; birthweight (< 2500 g); mean length; cranial circumference; placental weight; serum magnesium concentration/magnesaemia. Side effects and miscarriage were reported (as these women were subsequently excluded). | |
| Notes | Sample size calculation was not performed. It was presumed that participants were randomised equally to the treatment and control groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “A double‐blind protocol was used and... each was assigned a code number on the basis of which she received tablets.” No detail provided re: the generation of the random sequence. |
| Allocation concealment (selection bias) | Unclear risk | As above, no further detail provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Only the chemist knew the association between the code number and the treatment/placebo group. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blind outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Post‐randomisation exclusion due to side effects of the treatment or miscarriage (4 in placebo and 3 in treatment group due to side effects such as diarrhoea, nausea, emesis; 1 in placebo and 1 in treatment group due to miscarriage). |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not clearly pre‐specified in the methods. Mean duration of pregnancy and birth length were reported with no standard deviations/errors. |
| Other bias | Low risk | No other obvious source of bias identified. |
Memphis 1989.
| Methods | Randomised controlled trial. | |
| Participants | 400 women were randomised. Setting: prenatal clinics in Memphis, USA. Inclusion criteria: normotensive primigravid women (enrolled at 13 to 24 weeks' gestation). Exclusion criteria: women with medical and obstetric complications, and those > 24 weeks' gestation at the time of the first prenatal visit were excluded. |
|
| Interventions |
Treatment group (n = 200) Women received 6 tablets of magnesium‐aspartate hydrochloride per day (each containing 60.8 mg of elemental magnesium: 365 mg/day) from 13 to 24 weeks until birth. Control group (n = 200) Women received identically appearing aspartic acid tablets. All women: received prenatal vitamins containing 200 mg of elemental calcium and 100 mg of elemental magnesium per day. |
|
| Outcomes | Maternal blood pressure; pre‐eclampsia (mild or severe); preterm labour (with or without preterm prelabour rupture of membranes); post‐term pregnancy; gestational age at birth; birthweight; placental weight; Apgar scores; admission to special care nursery; small‐for‐gestational age. | |
| Notes | Sample size calculation performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation chart using a randomisation schedule. |
| Allocation concealment (selection bias) | Low risk | Allocation by pharmacy. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The control treatment matched the magnesium aspartate hydrochloride tablets. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 11/200 (5.5%) of women excluded from the placebo group and 15/200 (7.5%) of women excluded from the treatment group because they never started the medication (6.5% total post‐randomisation exclusions). |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Unclear risk | 14 women in the placebo group and 11 in the treatment group stopped taking the tablets prior to the commencement of the third trimester. The remaining women took approximately 90% of the tablets. Reasons for ceasing the medication included gastrointestinal symptoms and trouble swallowing the tablets. There was no difference in the incidence of side effects between the placebo and treatment groups. |
Mississippi 1992.
| Methods | Randomised controlled trial. | |
| Participants | 54 women were randomised. Setting: Mississippi, USA. Inclusion criteria: women with risk factors for preterm delivery. |
|
| Interventions |
Treatment group (n = 27) Women received 2 500 mg tablets of magnesium gluconate 4 times daily (4 g daily, 215 mg elemental magnesium). Control group (n = 27) Women received 2 placebo tablets, 4 times daily. The tablets had the same physical appearance. If preterm labour occurred: the study medication was discontinued and the woman was treated with standard tocolytic therapy (magnesium sulphate). |
|
| Outcomes | Preterm labour; gestational age at birth; birthweight; major adverse effects; Apgar score < 7 at 5 minutes; serum magnesium concentrations. | |
| Notes | Composition of placebo not reported. No sample size calculation performed. After the study begun 31 consecutive women (16 in the treatment group; 15 in the placebo group) received home uterine ambulatory monitoring for 1 hour twice daily. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly selected ‐ methods not given. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The healthcare providers were blinded to the treatment allocation. Placebo used had identical appearance to the magnesium tablets. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Assuming equal randomisation into the treatment and placebo groups, 2/27 (7.4%) women were excluded from the placebo group and 5/27 (18.5%) women were excluded from the treatment group (13% women excluded in total). This assumption had to be made as the original report did not report which group the women who were excluded were assigned to. 7 women were excluded – 4 moved away, 2 experienced an early pregnancy loss, and 1 “violated protocol”. |
| Selective reporting (reporting bias) | Unclear risk | Not all reported outcomes were clearly pre‐specified in methods. |
| Other bias | Low risk | No other obvious sources of bias identified. Risk factors for preterm birth and other baseline characteristics were comparable between groups. |
South Africa 2007.
| Methods | Randomised controlled trial. | |
| Participants | 4476 women were randomised into the study. Setting: Midwife Obstetric Unit in Guguletu and its referral hospitals, South Africa. Inclusion criteria: women presenting to the above unit. (Black pregnant women of low socio‐economic status.) Exclusion criteria: women with a multiple pregnancy. |
|
| Interventions |
Treatment group (n = 2016) Women were given slow‐release magnesium stearate tablets (64 mg elemental magnesium). Control group (n = 2066) Women were given indistinguishable placebo tablets containing lactose sugar. All women: received the tablets from the time of enrolment until delivery. Both tablets were cherry‐red, biconvex, enteric‐coated and of similar‐size. The tablets were packed into brown glass bottles with similar labels (A or B). Only the manufacturer knew the contents. Women received a bottle of 60 tablets and were instructed to swallow 2 whole tablets with water each morning (not to be chewed or sucked). |
|
| Outcomes |
Pre‐specified: hypoxic ischaemic encephalopathy classified by altered muscle tone and consciousness; bulging anterior fontanelle; inadequate suck reflex; haematuria and ultrasound signs of cerebral oedema with compression of the ventricles as assessed by the hospital's neonatologists; low Apgar scores (≤ 4 at 1 minute; ≤ 6 at 5 minutes); fetal heart rate abnormalities scored from cardiotocograph tracings; meconium aspiration pneumonia diagnosed by respiratory distress from birth and radiological evidence as assess by the hospital's neonatologists; term stillbirth. Other outcome data reported relating to delivery and infant characteristics: adverse effects from tablets; discontinuation of tablets due to discomfort; red blood cell magnesium; additional antenatal assessment or treatment in hospital; labour (including spontaneous onset, need for induction – and use of oxytocin/prostaglandin gel/other); duration of labour; labour complications; mode of birth (normal vaginal; caesarean); live‐births; neonatal deaths (and reasons); birthweight; placental weight; gestational age at birth; head circumference; premature birth; birthweight < 2500 g; congenital abnormalities |
|
| Notes | Sample size calculation: 4372 pregnant women would be needed to have 80% power for a 50% reduction in hypoxic ischaemic encephalopathy. However, a 2% dropout rate was also allowed for, therefore 4459 women were required. Authors attributed the higher mortality rate of preterm infants in the supplemented group to the deaths of 2 sets of twins of less than 750 g at birth. * Trial authors were contacted and responded 31/08/2013 regarding the numbers of neonatal deaths in each group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation sequence was provided by the Medical Research Council from computer‐generated random numbers linked to the letters A and B. |
| Allocation concealment (selection bias) | Low risk | “Simple randomisation was conducted by the research assistants who issued consecutive numbers to each participant.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Nurses and medical staff were unaware of the participants' status. Bottles of tablets were marked A or B and only the manufacturer knew the contents of the bottles. The placebo tablets used appeared identical to the magnesium tablets. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 8.8% post‐randomisation exclusions. 204 women lost to follow‐up. 190 women excluded post‐randomisation. The analysis was not performed on women lost to follow‐up or those excluded post‐randomisation. It is also difficult to determine which group the excluded women were randomised to. |
| Selective reporting (reporting bias) | Unclear risk | While pre‐specified/expected outcomes were reported, the reporting of outcome data related to stillbirths and neonatal deaths in the manuscript was unclear, and further with no access to a trial protocol, it is not possible to confidently assess selective reporting. In the text it suggests that there were 16 treatment group and 7 control group neonatal deaths, however the table indicated that there were 17 treatment group and 7 control group neonatal deaths. Trial authors were contacted and were able to confirm the numbers of neonatal deaths per group (17 and 7). In regards to stillbirths, only the values for stillbirth at greater than 28 weeks and at term were provided by group allocation. |
| Other bias | Unclear risk | The authors reported poor adherence (one‐quarter of women on average took all the prescribed tablets). |
Zurich 1988.
| Methods | Quasi‐randomised controlled trial. | |
| Participants | 568 women were randomised. Setting: Outpatients clinic at the Department of Obstetrics, University of Zurich, from 1983 to 1985. Inclusion criteria: women with normal and high‐risk pregnancies, at no later than 16 weeks' gestation. |
|
| Interventions |
Treatment group (n = 278) Women received 15 mmol of magnesium aspartate‐hydrochloride daily from ≤ 16 weeks' gestation until delivery. Control group (n = 290) Women received a control tablet containing 13.5 mmol of aspartic acid per day. No detail of the appearance/taste of these tablets being similar to the treatment tablets. The doses were divided into 6 tablets to be taken daily. |
|
| Outcomes | Adverse effects; miscarriage; maternal weight increase; blood pressure; oedema; hospitalisation (and indication for hospitalisation); median gestation; preterm birth; duration of the first and second stage of labour; operative birth; placental weight; infant weight; low birthweight; infant length; head circumference; neonatal acid‐base values; admission to the neonatal intensive care unit; perinatal death; low Apgar score (≤ 7). | |
| Notes | Sample size was determined by the duration of the study’s recruitment period (2 years). Groups were comparable at baseline. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Allocation was based on the women's date of birth. |
| Allocation concealment (selection bias) | High risk | Women with even birth date given magnesium‐aspartate‐hydrochloride, women with odd birth date given aspartic acid. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The study was described as “double‐blind” with the use of a placebo; however allocation was based on the women's date of birth, and thus it is unclear as to whether blinding would have been successfully achieved for women and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The study was described as “double‐blind” with the use of a placebo; however allocation was based on the women's date of birth, and thus it is unclear as to whether blinding would have been successfully achieved for outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Actual group values (total number per group) are not reported in the outcome data tables, and thus it is difficult to determine the exclusions and attrition and where there is missing data; quote “For various reasons such as refusal to take further tablets, delivery in other hospitals or abortion, some data were not available for analysis." |
| Selective reporting (reporting bias) | Unclear risk | Outcome data reported for a range of important outcomes – these however were not pre‐specified in the methods, and it is therefore difficult to assess selective reporting. |
| Other bias | Unclear risk | No other obvious sources of bias identified. |
EPH: edema, proteinuria, hypertension GI: gastrointestinal IVF: in vitro fertilisation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Denmark 1990 | This trial compared light and electron microscope changes in the placenta and umbilical cord of 28 women with pregnancy‐induced hypertension randomised to intravenous and oral magnesium sulphate or placebo. This trial may be considered for inclusion in a future update of the Duley 2010 Cochrane review. |
| Denmark 1991 | This trial recruited 58 women with pregnancy‐induced hypertension to determine effects of intravenous and oral magnesium versus placebo on maternal blood pressure. This study may be considered for inclusion in a future update of the Duley 2010 Cochrane review. |
| Detroit 1999 | This trial assessed the effects of intravenous magnesium sulphate on fetal heart rate parameters. |
| India 2012 | This randomised trial recruited 48 women with gestational age greater than 34 weeks with mild pre‐eclampsia or gestational hypertension and randomly assigned them to receive either intravenous magnesium sulphate or placebo, to assess the effects on fetal umbilical artery and middle cerebral artery blood flow. This trial may be considered for inclusion in a future update of the Duley 2010 Cochrane review. |
| ISRCTN03989660 | This study will assess the effects of oral magnesium supplementation on pregnancy‐related leg cramps, which is the focus of another relevant Cochrane review (Garrison 2012). |
| NCT01709968 | This study will assess the effects of oral magnesium supplementation on pregnancy‐related leg cramps, which is the focus of another relevant Cochrane review (Garrison 2012). |
| Norway 2008 | This study examined the effects of oral magnesium supplementation on pregnancy‐related leg cramps and has been assessed in the relevant Cochrane review (Garrison 2012). |
| Sweden 1987 | This randomised controlled trial randomised 60 pregnant women to either calcium or ascorbic acid (1 g twice daily) as treatment for leg cramps. There was no magnesium arm in this trial. |
| Sweden 1995 | This study examined the effects of oral magnesium supplementation on pregnancy‐related leg cramps and has been assessed in the relevant Cochrane review (Garrison 2012). |
Characteristics of ongoing studies [ordered by study ID]
ISRCTN98365455.
| Trial name or title | Acid‐base balance and blood pressure during pregnancy: a double‐blinded randomised controlled trial. |
| Methods | Randomised controlled trial. |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention group: magnesium citrate powder (Diasporal), 12 mmol magnesium daily, taken at week 25 of pregnancy until delivery.
Control group: no supplements. Blood pressure and proteinuria will be measured routinely in all pregnancies. |
| Outcomes | Primary outcome measure(s): blood pressure increase during final weeks of pregnancy. Secondary outcome measure(s): symptoms of pre‐eclampsia during final weeks of pregnancy. |
| Starting date | October 2010. |
| Contact information | Professor Ragnar Rylander, Sodra Alvsaborg’s Hospital, Sweden. envhealth@biofact.se. |
| Notes | Estimated enrolment: 60 women. |
NCT01510665.
| Trial name or title | Magnesium supplementation in the second trimester of pregnancy for overweight individuals. |
| Methods | Randomised, double‐blind, controlled trial. |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention group: magnesium citrate dietary supplement (300 mg elemental magnesium daily dose) given week 13 to week 28 (2 pills daily). Control group: identical appearing pill with inactive ingredients given week 13 to week 28 (2 pills daily). |
| Outcomes | Primary outcome measure(s): change in maternal biomarkers during pregnancy up to 28 weeks; neonatal birthweight/height; change in maternal biomarkers in pregnancy in the third trimester. Secondary outcome measure(s): macrosomia, preterm birth, head circumference, and Apgar score; endothelial progenitor cell presence in cord blood, and DNA expression from the placental tissue; gestational diabetes, hypertension, proteinuria, shoulder dystocia, caesarean section, weight gain. |
| Starting date | January 2012. |
| Contact information | Dr Simin Liu, University of California, Los Angeles. |
| Notes | Estimated enrolment: 60 women. |
BMI: body mass index HgbA1C: glycated haemoglobin
Differences between protocol and review
We have updated the methods for this review update.
We have specified that the intervention could be commenced at any time during pregnancy (rather than prior to the 25th week of pregnancy as previously specified), and we planned to assess variation according to gestation of commencement by a pre‐specified subgroup analysis, as detailed in the methods.
We have specified that cluster‐randomised trials are eligible for inclusion.
We have separated the review's outcomes into primary and secondary outcomes, and have detailed in this update a number of non pre‐specified infant outcomes for which we have reported data, as they were considered to be clinically relevant and important for inclusion in this review.
Contributions of authors
For this update DC and EB assessed the new studies for inclusion, performed data extraction and assessed the risk of bias for included trials. EB and DC drafted the changes to the text and prepared subsequent drafts. MM and CAC contributed to the subsequent drafts and the final version.
MM and CAC developed the original protocol, extracted data and wrote the previous versions of this review.
Sources of support
Internal sources
ARCH, Robinson Institute, The University of Adelaide, Australia.
Women's & Children's Health Research Institute, Adelaide, Australia.
External sources
National Health and Medical Research Council, Australia.
Commonwealth Department of Health and Ageing, Australia.
Declarations of interest
Maria Makrides ‐ has received advisory board payments from Nestle Nutrition Insitute, Fonterra,and Nutricia/Danone. These advisory boards were related to clinical nutrition in paediatric settings (and therefore not related to the topic under review). The Nestle Nutrition Institute advisory board was only focused on education and training aspects and there were no discussions relating to products. All the honoraria associated with these boards were paid to Maria Makrides' institution and used to fund continuing education and travel for students, early and mid‐career researchers.
Danielle Crosby ‐ none known
Emily Shepherd ‐ none known
Caroline Crowther ‐ none known
Edited (no change to conclusions)
References
References to studies included in this review
Angola 1992 {published data only}
- D'Almeida A, Carter JP, Antol A, Prost C. Effects of a combination of evening primrose oil (gamma linolenic acid) and fish oil (eicosapentaenoic + docosahexaenoic acid) versus magnesium, and placebo in preventing pre‐eclampsia. Women and Health 1992;19:117‐31. [DOI] [PubMed] [Google Scholar]
Austria 1997 {published data only}
- Arikan G, Gucer F, Scholl W, Weiss PAM. Preterm labour during oral magnesium supplementation in uncomplicated pregnancies [Fruhgeburtlichkeit unter oraler magnesium substitution bei unkomplizierten schwangerschaften: eine randomisiert kontrolliert klinische studie]. Geburtshilfe und Frauenheilkunde 1997;57:491‐5. [Google Scholar]
- Arikan G, Panzitt T, Gaucer F, Boritsch J, Trojovski A, Haeusler MCH. Oral magnesium supplementation and the prevention of preterm labor. American Journal of Obstetrics and Gynaecology 1997;176:(1Pt2):S45. [Google Scholar]
China 1997 {published data only}
- Li S, Tian H. Oral low‐dose magnesium gluconate preventing pregnancy induced hypertension (translation). Chunh‐Hua‐Fu‐Chan‐Ko‐Tsa‐Chih [Chinese Journal of Obstetrics and Gynaecology] 1997;32:613‐5. [PubMed] [Google Scholar]
Hungary 1979 {published data only}
- Balazs M, Kuti V, Morvay F, Varenka Zs, Szekely A, Szucs M. New data on the relationship between magnesium intake and the quality of pregnancy [Données nouvelles sur les relations entre l'apport alimentaire en magnésium et la qualité de la grossesse]. Revue Française d'Endocrinologie Clinique, Nutrition, et Métabolisme 1980;21(6):525‐7. [Google Scholar]
- Balazs M, Morvai F, Szekely Z, Miklos Szucs, Varenka Z, Kuti V. Miscarriage and magnesium intake [Avortment spontané et apport en magnésium de la ration alimentaire]. Revue Française d'Endocrinologie Clinique, Nutrition, et Métabolisme 1979;20(6):525‐9. [Google Scholar]
Hungary 1988 {published data only}
- Kovacs L, Molnar BG, Huhn E, Bodis L. Magnesium substitution in pregnancy. A prospective, randomized double‐blind study [Magnesium substitution in der Schwangerschaft: eine prospektive, randomisierte doppelblindstudie]. Geburtshilfe und Frauenheilkunde 1988;48:595‐600. [PubMed] [Google Scholar]
- Kovacs L, Molnar GB, Huhn E, Bodis L. Magnesium substitution during pregnancy. A prospective randomised, double blind, clinical trial. Magyar Noorvosok Lapja 1988;51:9‐14. [Google Scholar]
Italy 1994 {published data only}
- Zarcone R, Cardone G, Bellini P. Role of magnesium in pregnancy. Panminerva Medica 1994;36:168‐70. [PubMed] [Google Scholar]
Memphis 1989 {published data only}
- Sibai BM, Villar MA, Bary E. Magnesium supplementation during pregnancy: a double‐blind randomized controlled clinical trial. American Journal of Obstetrics and Gynaecology 1989;161:115‐9. [DOI] [PubMed] [Google Scholar]
Mississippi 1992 {published data only}
- Martin RW, McColgin SW, Perry KG, McCaul JF, Hess LW, Martin JN, et al. Oral magnesium and the prevention of preterm labor in a high‐risk group of patients. Proceedings of 10th Annual Meeting of Society of Perinatal Obstetricians, Houston, Texas, USA. 1990:181.
- Martin RW, Perry KG, Hess LW, Martin JN, Morrison JC. Oral magnesium and the prevention of preterm labor in a high‐risk group of patients. American Journal of Obstetrics and Gynaecology 1992;166:144‐7. [DOI] [PubMed] [Google Scholar]
South Africa 2007 {published data only}
- Fawcus S, Harrison V, Jordaan E. The prevention of neonatal encephalopathy: could magnesium supplementation during pregnancy play a role? [abstract]. 31st British International Congress of Obstetrics and Gynaecology. London, UK, 2007 July 4‐6:102.
- Harrison V, Fawcus S, Jordaan E. Magnesium supplementation and perinatal hypoxia: outcome of a parallel group randomised trial in pregnancy. British Journal of Obstetrics and Gynaecology 2007;114:994‐1002. [DOI] [PubMed] [Google Scholar]
Zurich 1988 {published data only}
- Jaspers V, Spatling L, Fallenstein F, Quakernack K. Magnesium, calcium, haemoglobin, haematocrit, oestriol and HPL following magnesium substitution [supplementation] during pregnancy [Magnesium, kalzium, hamoglobin, hamatokrit, ostriol und HPL unter magnesium substitution in der schwangerschaft]. Geburtshilfe und Frauenheilkunde 1990;50:628‐33. [DOI] [PubMed] [Google Scholar]
- Spatling L. Magnesium supplementation in pregnancy in pregnancy: a double‐blind study. Proceedings of International Symposium on Advances in the Prevention of Low Birthweight, Cape Cod, Massachusetts, USA. 1988:197‐201.
- Spatling L, Spatling G. Magnesium supplementation in pregnancy. A double‐blind study. British Journal of Obstetrics and Gynaecology 1988;95:120‐5. [PubMed] [Google Scholar]
- Vetter K, Spaetling L. Magnesium substitution in pregnancy a double‐blind study [Magnesium substitution in der schwangerschaft eine doppelblindstudie]. Archives of Gynaecology 1986;239:176‐7. [Google Scholar]
References to studies excluded from this review
Denmark 1990 {published data only}
- Rudnicki M, Junge J, Frolich A, Ornvold K, Fischer‐Rasmussen W. Magnesium supplement in pregnancy‐induced hypertension A clinicopathological study. Acta Pathologica, Microbiologica, et Immunologica Scandinavica 1990;98:1123‐7. [DOI] [PubMed] [Google Scholar]
Denmark 1991 {published data only}
- Rudnicki M, Frølich A, Fischer‐Rasmussen W. Magnesium supplement in pregnancy‐induced hypertension: effects on maternal and neonatal magnesium and calcium homeostasis. Mineral and Electrolyte Metabolism 1991;17(6):399‐403. [PubMed] [Google Scholar]
Detroit 1999 {published data only}
- Hallak M, Martinez‐Poyer J, Brish L, Poole‐Bryant K, Mammen EF, Sorokin Y. Magnesium sulfate impairs platelet function in normal pregnant women. American Journal of Obstetrics and Gynecology 1999;180(1 Pt 2):S142. [Google Scholar]
- Hallak M, Martinez‐Poyer J, Kruger M, Hassan S, Blackwell S, Sorokin Y. The effect of magnesium sulfate on fetal heart rate parameters: A randomized, placebo‐controlled trial. American Journal of Obstetrics and Gynecology 1999;181(5):1122‐7. [DOI] [PubMed] [Google Scholar]
- Hallak M, Martinez‐Poyer J, Kruger ML, Hassan S, Blackwell SC, Sorokin Y. Magnesium sulfate effect on fetal heart rate (FHR) parameters: A randomized, placebo controlled trial. American Journal of Obstetrics and Gynecology 1999;180(1 Pt 2):S155. [DOI] [PubMed] [Google Scholar]
- Hallak M, Martinez‐Poyer J, Kruger ML, King M, Russell E, Sorokin Y. Magnesium sulfate transiently increases fetal breathing movements but not body movements. American Journal of Obstetrics and Gynecology 1999;180(1 Pt 2):S155. [Google Scholar]
- Martinez‐Poyer J, Hallak M, King M, Kruger M, Sorokin Y. Magnesium sulfate increases impedance to flow in the fetal systemic circulation but has no effect on the cerebral circulation. American Journal of Obstetrics and Gynecology 1999;180(1 Pt 2):S114. [Google Scholar]
- Martinez‐Poyer J, Hallak M, Russell E, Poole‐Bryant K, Sorokin Y. Magnesium sulfate prolongs ventricular repolarisation in normal gravidas: A randomised, double‐blind, placebo controlled study. American Journal of Obstetrics and Gynecology 1999;180(1 Pt 2):S142. [Google Scholar]
India 2012 {published data only}
- Dasgupta S, Ghosh D, Seal SL, Kamilya G, Karmakar M, Saha D. Randomized controlled study comparing effect of magnesium sulfate with placebo on fetal umbilical artery and middle cerebral artery blood flow in mild preeclampsia at ≥ 34 weeks gestational age. Journal of Obstetrics and Gynaecology Research 2012;38(5):763‐71. [DOI] [PubMed] [Google Scholar]
ISRCTN03989660 {published data only}
- ISRCTN03989660. A randomized, double‐blinded, placebo‐controlled trial of oral magnesium for relief in pregnancy‐induced leg cramps. http://www.controlled‐trials.com/ISRCTN03989660/ (accessed 7 February 2013).
NCT01709968 {published data only}
- NCT01709968. Magnesium oxide monohydrate for nocturnal leg cramps (mgnlc); a prospective, randomized, double blind, placebo controlled clinical trial. http://clinicaltrials.gov/ct2/show/NCT01709968 (accessed 7 February 2013).
Norway 2008 {published data only}
- Nygaard IH, Valbø A, Pethick SV, Bøhmer T. Does oral magnesium substitution relieve pregnancy‐induced leg cramps?. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2008;141(1):23‐6. [DOI] [PubMed] [Google Scholar]
Sweden 1987 {published data only}
- Hammar M, Berg G, Solheim F, Larsson L. Calcium and magnesium status in pregnant women. A comparison between treatment with calcium and vitamin C in pregnant women with leg cramps. International Journal of Vitamin and Nutrition Research 1987;57:179‐83. [PubMed] [Google Scholar]
Sweden 1995 {published data only}
- Dahle LO, Berg G, Hammar M, Hurtig M, Larsson L. The effect of oral magnesium substitution on pregnancy‐induced leg cramps. American Journal of Obstetrics and Gynecology 1995;173(1):175‐80. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN98365455 {published data only}
- ISRCTN98365455. Magnesium intervention during pregnancy. http://www.controlled‐trials.com/isrctn/pf/98365455 (accessed 25 August 2011).
NCT01510665 {published data only}
- NCT01510665. Magnesium supplementation in the second trimester of pregnancy to overweight and obese individuals. http://clinicaltrials.gov/ct2/show/NCT01510665 (accessed 7 February 2013).
Additional references
Arikan 1999
- Arikan GM, Panzitt T, Gücer F, Scholz HS, Reinisch S, Haas J, et al. Course of maternal serum magnesium levels in low‐risk gestations and in preterm labor and delivery. Fetal Diagnosis and Therapy 1999;14(6):332‐6. [DOI] [PubMed] [Google Scholar]
Conradt 1984
- Conradt A, Weidinger H, Algayer. On the role of magnesium in fetal hypotrophy, pregnancy induced hypertension and pre‐eclampsia. Magnesium Bulletin 1984;6:68‐76. [Google Scholar]
Doyle 1989
- Doyle W, Crawford MA, Wynn AH, Wynn SW. Maternal magnesium intake and pregnancy outcome. Magnesium Research 1989;2:205‐10. [PubMed] [Google Scholar]
Duley 2010
- Duley L, Gülmezoglu AM, Henderson‐Smart DJ, Chou D. Magnesium sulphate and other anticonvulsants for women with pre‐eclampsia. Cochrane Database of Systematic Reviews 2010, Issue 11. [DOI: 10.1002/14651858.CD000025.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Garrison 2012
- Garrison SR, Allan GM, Sekhon RK, Musini VM, Khan KM. Magnesium for skeletal muscle cramps. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD009402.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Inst Med 1990
- Subcommittee on Nutritional Status and Weight Gain During Pregnancy, Subcommittee on Dietary Intake and Nutrient Supplements During Pregnancy, Committee on Nutritional Status During Pregnancy and Lactation, Food, Nutrition Board. Institute of Medicine, National Academy of Sciences. Nutrition During Pregnancy. Washington DC: National Academy Press, 1990. [Google Scholar]
RevMan 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
US FDA 2009
- US Department of Health and Human Services: US FDA. Overview of dietary supplements: What is a dietary supplement?. http://www.fda.gov/Food/DietarySupplements/ConsumerInformation/ucm110417.htm#what 2009 [accessed 25 Aug 2011].
References to other published versions of this review
Keirse 1995
- Keirse MJNC. Routine magnesium supplementation in pregnancy. Pregnancy and Childbirth Module; The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM]. The Cochrane Collaboration; Oxford, 1995 [revised 16 June 1993], issue 2.
Makrides 1998
- Makrides M, Crowther CA. Magnesium supplementation in pregnancy. Cochrane Database of Systematic Reviews 1998, Issue 2. [DOI: 10.1002/14651858.CD000937] [DOI] [PubMed] [Google Scholar]
Makrides 2001
- Makrides M, Crowther CA. Magnesium supplementation in pregnancy. Cochrane Database of Systematic Reviews 2001, Issue 4. [DOI: 10.1002/14651858.CD000937] [DOI] [PubMed] [Google Scholar]


