Abstract
Introduction
There is room for innovation in medical education regarding HIV and modern biomedical preventive strategies such as pre-exposure prophylaxis (PrEP). Previously described undergraduate medical curricular modules address care for HIV patients but do not include PrEP. A graduate medical curriculum concerning HIV has also been described but misses the opportunity for early introduction of HIV risk prevention, an element of primary preventive care. The guiding framework described here provides one mechanism to begin addressing this gap and fosters interprofessional collaboration among students through community engagement.
Methods
We assembled a team of 11 first-year students (medical, physician assistant, podiatry, pharmacy, and health care psychology). The team collaborated to create a training module about HIV risk and PrEP access in Lake County, Illinois. A biopsychosocial perspective on HIV risk and PrEP was employed as the guiding framework. The student team presented the module to care teams at the Lake County Health Department and to the university campus through interactive workshops.
Results
Participating students completed a self-reflection instrument. Responses were positive in terms of student enjoyment and attainment of new knowledge regarding HIV risk and PrEP. Students also self-reported competency in a selected group of Interprofessional Education Collaborative competencies. Narrative responses were analyzed for context.
Discussion
Student responses suggest that this activity is effective in providing education about HIV risk and PrEP. The framework is novel in that it requires research and modification at each site of implementation. Furthermore, as an extracurricular element, its implementation is flexible.
Keywords: Interprofessional Education, Population Health, HIV, Cultural Competence, Diversity, Health Equity, Access to Care, Pre-Exposure Prophylaxis, PrEP, Community Engagement, LGBTQ+, Service Learning
Educational Objectives
By the end of this activity, learners will be able to:
-
1.
Discuss the rationale for prescribing pre-exposure prophylaxis (PrEP) and medical requirements for monitoring a patient taking PrEP.
-
2.
Analyze the connections between social determinants and HIV risk for a specific community.
-
3.
Contrast the disparities in HIV diagnosis to access to PrEP for a specific community using national- and local-level data.
-
4.
Relate financial and administrative barriers to PrEP access to disparities in HIV diagnosis at the national and local levels.
-
5.
Relate social and cultural factors to HIV stigma and PrEP access at the national and local levels.
-
6.
Develop case studies that describe HIV risk factors and PrEP access barriers for a unique community.
-
7.
Confront stereotypes about HIV diagnosis and provision of care to patients at risk for HIV.
-
8.
Examine the role of interprofessional collaboration in preventive HIV care.
Introduction
The human immunodeficiency virus (HIV) remains a significant and disparate public health concern in the United States. In 2017, nearly 40,000 new diagnoses were reported.1 New diagnoses of HIV occur disproportionately among racial minority communities, specifically black and Latino patients, and among men who have sex with men.1,2 Pre-exposure prophylaxis (PrEP) is a once-daily regimen of two antiretroviral drugs: emtricitabine/tenofovir disoproxil fumarate (TDF/FTC), marketed as Truvada (Gilead Sciences, Foster City, CA). Presently, TDF/FTC is the only regimen that is approved by the US Food and Drug Administration (FDA) for use as PrEP. With regular dosing, PrEP is over 90% effective at preventing HIV transmission.3–5 TDF/FTC also has a well-documented safety profile with minor side effects.6,7
Despite receiving FDA approval in 2012, uptake of PrEP in patients at risk for HIV has been slow, with disparities again most pronounced in prescription rates to minority patients.8–10 One reported explanation for the slow uptake of PrEP is inadequate health care provider awareness.11–13 This gap in education likely stems from professional training, which offers limited content regarding HIV risk factors and prevention strategies.14 Gaps in education also exist in the knowledge medical students have regarding other sexually transmitted infections (STIs).14,15 This is a symptom of a larger issue in medical and health professions education: lack of content overall regarding sexual health, including that of lesbian, gay, bisexual, transgender, and queer (LGBTQ+) patients, a community with an intimate historical connection to HIV.16–21
A number of educational modules that focus on HIV and LGBTQ+ health care have been reported. A recently published case-based learning module covers the pathophysiology of HIV infection but does not mention prevention or psychosocial factors associated with HIV.22 Other case-based modules focus on a single patient in a general sense23 rather than exploring the diversity of patients at risk for HIV.24,25 Other modules that are HIV specific are designed for resident physicians or fellows, missing the opportunity to introduce this information to medical students.26,27 Discussion of HIV risk at a general national level also misses local-level data, which are important in influencing care decisions on a day-to-day basis.28 LGBTQ+ health training materials have been developed as well but do not include a specific focus on HIV and PrEP.29,30 Finally, these examples are all course based rather than service based, missing the centrality of community focus in HIV risk and PrEP access.31–33
The project presented here describes the process for organizing a team of health professions graduate students who collaborate to create a community-specific training module about HIV risk and PrEP access. Faculty members act as facilitators and guide the process as students research HIV risk and the current state of PrEP use in their community. Dissemination of this information occurs through interactive workshops hosted by members of the student team for their campus, community health care providers, and volunteer organizations. The purpose of this initiative is twofold: to educate both current and future practitioners about using PrEP for HIV prevention.
This educational summary report and the appendices are meant to guide replication of this project at other institutions by providing example materials and a framework for customizing them to create a community-specific training module about HIV risk and PrEP access. To that effect, assembling the community-specific training module is a learning experience for the student team that conducts the process and for any additional students who attend the workshops that result from the customized training materials.
Methods
The target audience of this activity was first- or second-year medical and health professions graduate students. Ideally, this activity would be implemented at a medical school with other professional graduate education programs. A student-run clinic would also be an asset.
Our interprofessional student team was recruited from a Foundations of Interprofessional Practice course for all first-year students in graduate-level clinical programs at Rosalind Franklin University of Medicine and Science (RFUMS). The program was announced to the class, and students were invited to attend an information session. In total, 11 students participated. Students represented disciplines of medicine, podiatry, physician assistant, pharmacy, health care administration, and health care psychology. Prior knowledge regarding HIV or PrEP was not required for participation. Faculty were also recruited to serve as facilitators throughout the process and represented both basic and clinical sciences. It may be beneficial for faculty to have prior knowledge of PrEP or HIV care and HIV risk within the community. Faculty facilitators ensured that the information contained in the training module was accurate and attended workshops to answer questions and provide feedback.
Logistically, the requirements for this activity were minimal. The student team required meeting space for preparatory meetings. Students could also make the decision to conduct all collaboration virtually. Costs associated with this activity were also minimal, including only the cost of printing materials for workshops. Students each contributed approximately 4 hours of work researching and compiling their portions of the training module. Additional time was required for presentation of the training module through workshops, as described below.
Creating the Training Module
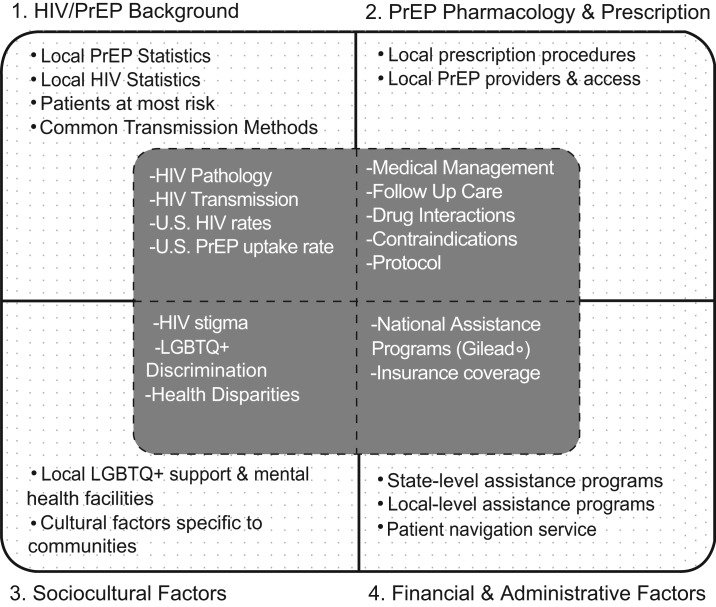
The RFUMS student team created a community-specific training module about HIV risk and PrEP access in Lake County, Illinois. The training module contained four domains of information: HIV and PrEP background, PrEP pharmacology and prescription, sociocultural factors, and financial and administrative factors. Within each domain, two levels of information were included: national and local (Figure 1). This method provided education that oriented attendees to HIV incidence and PrEP uptake in terms of the national landscape while also making the information presented actionable and relevant to the specific community attendees served in Lake County.
Figure 1. Structural framework of the educational module designed in this project. The four domains of information to be captured are delineated. At the core is the general information for each domain that is to be included. In the gray sections surrounding the core are the areas for customization based on the specific community and its population, needs, and resource availability. PrEP, pre-exposure prophylaxis.
The attached facilitator's guide (Appendix A) was for use by faculty facilitators and students. It guided the process of adapting the training module materials for a specific community of interest. The process for adapting and implementing the training module described here is ready for immediate implementation at medical schools using the template materials, including case studies (Appendices B and C) and the workshop presentation (Appendix D). The four sections of material contained in the template training module are described below.
HIV and PrEP background: This domain of the module focused on presenting basic foundational information about HIV biology and epidemiology. This included HIV transmission methods, the pathological mechanisms of the HIV virus, and symptoms of acute HIV infection. Distributions of new HIV diagnoses by race, gender, geography, and lifestyle factor were also presented. Locally, transmission rates within Lake County were presented, with special mention of the demographics of the communities surrounding RFUMS.
PrEP pharmacology and prescription: This domain outlined the rationale for prescribing PrEP and the patient populations specifically indicated for PrEP. The prerequisite medical tests required for prescription of TDF/FTC and the follow-up care required to safely maintain therapy were described. Contraindications for PrEP were specified, including a brief description of the pharmacologic mechanism of action of TDF/FTC and medication interactions. Local information consisted of resources directly from the Lake County Health Department (LCHD) and included information for specific individuals to be contacted if providers or their staff had further questions about department-specific PrEP prescription practices.
Sociocultural factors: Here, HIV risk factors and PrEP access were discussed with societal context. A brief history of HIV stigma, particularly that relating to gay men, was included. This was offered as context for the perceived and actual barriers that patients face and that contribute to disparities in PrEP uptake. Health disparities for LGBTQ+ individuals were also presented. Students also identified specific cultural representations of Lake County, informed through conversations with community members. This highlighted the communities and environment of Lake County and how these factors related to PrEP access and follow-up care retention.
Financial and administrative factors: This domain provided practical information about the administrative and insurance requirements for access to PrEP. Specifically, this involved national financial assistance programs, including the co-pay assistance program administered by the TDF/FTC manufacturer. A short discussion about the national health insurance coverage landscape for PrEP was also included. Local information was the most critical here, as most financial assistance for PrEP access occurs at the local and state levels. We discussed Illinois Medicaid coverage of PrEP and 340B medication pricing for eligible health care facilities. Resources specifically available to practitioners were given as well to provide direct information about the experts within their health care system if they had questions about a patient's eligibility for PrEP or departmental-level policies for financial assistance applications and patient navigation.
Case Studies
Case studies were the central instructional tool of the workshops included in this activity. The student team consulted with community advocates to determine examples of common patients newly diagnosed with HIV in Lake County. No identifying patient information was given, only general trends in patient and social characteristics associated with HIV risk and subsequent diagnosis. The student team wrote case studies of fictional patients with sociodemographic factors that mirrored patients in Lake County who had been newly diagnosed with HIV. Each case included details from all four training module content domains to emphasize the intersectionality that multiple factors have in the continuum of HIV prevention. The cases designed during our implementation of this training in Lake County are described below for context and to assist adaptation of this training module for subsequent implementation. Using case studies as an instructional tool allows flexibility in that risk factors included in case studies designed by student teams in other geographical locations can be changed to reflect the local community and resources.
Case study 1: This case described AS, a male patient who was an immigrant to the United States from a country where homosexuality was illegal (Appendix B). His history was presented in the context of a routine physical examination. He was sexually active in a monogamous relationship. He carried private insurance through his university, but his policy had a high medication co-pay. Follow-up questions explored whether AS was a candidate for PrEP and, if so, what additional resources were available to make PrEP affordable, plus the additional medical services that he might need. The recommended answers are provided in the case studies facilitator guide (Appendix C).
Case study 2: This case described ZH, a patient who visited a health department clinic routinely for STIs (Appendix B). The patient gave sparse details about use of protection, but recent HIV testing was negative. ZH was insured by a managed Medicaid product in Illinois. Follow-up prompts probed into what counseling would be appropriate for ZH and why PrEP was appropriate for this patient, pending the appropriate medical testing. The recommended answers are provided in the case studies facilitator guide (Appendix C).
Case study 3: This case described KJ, a female injection drug user who exchanged sex for heroin (Appendix B). The patient indicated that her drug dealers might not provide her with drugs if she requested they use a condom. Implicit within this case was the risk for HIV transmission through needle sharing. KJ was homeless and often slept on the couches of her drug dealers or other friends in the community. This case was included to introduce a patient who was medically and socially complex and to explore the degree to which social factors would influence the use of PrEP for HIV prevention. Follow-up questions required consideration of these factors and what the role of the health care provider could be in helping KJ regain control over her situation (Appendix C).
Case study 4: This case described JB, a man who presented to a primary care physician complaining of penile discharge (Appendix B). He admitted to having unprotected anal sex with men, unbeknownst to his wife. JB was HIV negative at the time of the visit. His wife carried their insurance through her employer. A number of complexities were involved in this case; the follow-up questions reflected this. Discussion covered the delicate nature of this patient's situation and the role of the health care professional in counseling about ways to reduce HIV/STI risk (Appendix C).
Case study 5: This case described TW, a man who suffered an accidental needlestick while at work (Appendix B). He was sexually active with one female partner and was asymptomatic at the time of the visit. TW was otherwise healthy. The case of TW was included to differentiate between PrEP and post-exposure prophylaxis (PEP). PEP is a full-dose antiretroviral regimen of three antiretroviral drugs given to individuals believed to have been exposed to HIV and is taken for only a limited time to prevent a potential HIV infection. The follow-up questions were meant to help distinguish PrEP and PEP (Appendix C).
Community Workshops
Groups of four to six students from the larger student team held workshops for multidisciplinary care teams at LCHD clinics. Workshops were interactive, consisting of a presentation of the didactic information and discussions of the case studies. As the case studies were designed to mirror patients frequently seen by the LCHD, there were ample opportunities for discussion between students and practitioners about the realities of preventing HIV in vulnerable populations. Six workshops were hosted by the student team.
The student team also partnered with the student-run Interprofessional Community Clinic (ICC) at RFUMS. The ICC provided free care to uninsured patients in Lake County. The interprofessional student team collaborated with the ICC to provide the training module materials to clinic volunteers and hosted two on-campus workshops for all students and faculty at RFUMS. All workshops were completed in approximately 75 minutes. A PowerPoint presentation (Appendix D) was used to present the didactic material, and paper copies of the case studies were provided to attendees. A sample workshop agenda is provided in the facilitator's guide (Appendix A). Faculty facilitators were present at all workshops and gave feedback on student presentations and small-group discussions. The facilitators were also there to answer questions from workshop attendees if needed.
Evaluation
Upon completion of this project, all participating students were given the option to complete a self-reflection instrument (Appendix E). The first segment contained background questions to capture students' demographic information and perceptions of working on the project. These items were assessed using a Likert scale (1 = Not at All or Does Not Describe Me at All, 5 = Completely or Completely Describes Me). Core competencies from the Interprofessional Education Collaborative (IPEC) were also assessed by the self-reflection.34,35 Sixteen competencies were selected, four from each core area of competence identified by the IPEC: values and ethics, roles and responsibilities (RR), communication (CC), and teams and teamwork. IPEC competencies were phrased as statements beginning with “I am able to …” Students rated agreement with a statement using the same Likert scale. IPEC core competencies were selected as standard phrasing to assess the utility of this activity as a mechanism for promoting teamwork during education and future patient care, which has traditionally been difficult to measure.36 Responses were captured using an anonymous online form. The self-reflection instrument also contained nine free-response items designed to elicit reflection on the experience of participating on the team that designed the training module and the experience of presenting the information through workshops.
Workshop attendees completed a different postworkshop survey. This instrument was used to evaluate the effectiveness of the workshops and to capture demographic information about the attendees. This instrument also used a 5-point Likert scale (1 = Absolutely Not, 5 = Absolutely Yes).
Statistical Analysis
Descriptive statistics for the items on the student self-reflection instrument and the attendee postworkshop surveys were calculated. Mean responses on the postworkshop survey were compared between quasi groups of attendees grouped by professional discipline using one-way analysis of variance (ANOVA). Students' written reflections were extracted from the online form. Two reviewers (Samuel R. Bunting and Tamzin J. Batteson) independently coded the free-response question responses and debriefed to identify recurrent themes. All statistics were calculated using IBM SPSS Version 25.0 (Armonk, NY). This project received a quality improvement determination and was not subject to review by the Institutional Review Board of RFUMS.
Results
All participating students completed the self-reflection instrument (N = 11, 100% response rate). Before beginning this project, three (27%) of the participating students had prior knowledge of PrEP. The interprofessional student team comprised medical students (four), physician assistant students (one), pharmacy students (two), podiatry students (one), health care psychology students (one), and health care administration students (two).
Student Knowledge and Confidence
Mean scores for all items regarding self-reported confidence in discussing HIV risk and PrEP with patients and fellow providers were greater than 4.0 (Table 1). In line with the objectives of this project, the scores in response to the question “To what extent did this project increase your knowledge of PrEP?” indicated effectiveness (M = 4.8, SD = 0.4). Equally important was the question “Do you feel like you made a difference in the community?”, which also garnered high scores (M = 4.7, SD = 0.5).
Table 1. Mean Student Responses to Background Questions (N = 11).
| Question | M (SEM) |
|---|---|
| To what extent did this project … | |
| Increase your knowledge of PrEP? | 4.8 (0.1) |
| Increase your awareness of risk factors for HIV? | 4.2 (0.3) |
| Increase your confidence with discussing PrEP with a patient? | 4.8 (0.1) |
| Increase your confidence in your ability to identify a patient who is at risk for becoming HIV positive? | 5.0 (0.0) |
| Increase your confidence in your ability to speak about PrEP with other professionals? | 5.0 (0.0) |
| Give you a more informed perspective on the disparities LGBTQ+ patients face when accessing health care? | 4.7 (0.1) |
| Give you a more informed perspective on the disparities racial and ethnic minorities face when accessing health care? | 4.5 (0.3) |
| Help you confront stereotypes or biases regarding HIV care? | 4.4 (0.2) |
| Help you confront stereotypes or biases regarding LGBTQ+ patients? | 4.2 (0.3) |
| Appreciate the centrality of interprofessional collaboration to success in sexual health care? | 4.3 (0.3) |
| Make you feel you made a difference for the community? | 4.7 (0.1) |
Abbreviation: PrEP, pre-exposure prophylaxis.
Scores for all 16 IPEC competency statements were positive as well (all > 4.0). In response to the statement “I am able to communicate the importance of teamwork in patient-centered care and population health programs and policies” (CC8), students self-reported a high degree of agreement (M = 4.8, SD = 0.4). In response to a related competency statement, “I express my knowledge and opinions to team members involved in patient care and population health improvement with confidence” (CC3), students also reported a high degree of agreement (M = 4.6, SD = 0.9). Similarly, self-reported responses to the statement “I am able to use unique and complementary abilities of all members of the team to optimize health and patient care” (RR9) were also positive (M = 4.8, SD = 0.4).
Student Satisfaction and Reflection
Overall, students learned “what PrEP was, how it can be used in the community, who can benefit from PrEP, how few providers knew about PrEP, and how much of an impact medical students can have on health care providers,” as reported in their self-reflections. Many of the reflections brought up a recurrent theme of learning about the “cultural barriers that are present in those that might benefit from the use of PrEP.” One student, who self-identified as a gay male, even stated that after learning about PrEP, he “instantly questioned why I not only wasn't offered [PrEP], but why I haven't heard much about it” from his own health care providers.
Even though HIV is not exclusively an LGBTQ+ health care concern, students were cognizant of the historical association between HIV and the LGBTQ+ community and “what impact that has on their health care access.” Students noted their sense of attending a “progressive school” but also that it became easy to “forget that there is a long history of bias that still has to be eradicated in many other places.”
Another overarching theme from the student reflections was perceived comfort in discussing sexual health with future patients. Students felt that they would “be able to take an appropriate sexual history and be better able to address the disparate aspects of LGBTQ+ health care.” Inclusion of sexual history for all patients was viewed as important because “if you ignore sexual history, you ignore risk factors that could lead to HIV infection or other sexually transmitted diseases.” Some students extended this recognition even further, reflecting that “having conversations about sexual health could open doors to getting patients in abusive relationships the proper resources” and that taking sexual history “could lead to opening up the conversation about other vaccines and safe practices.”
Community engagement and advocacy for LGBTQ+ health was another common thread of the student responses. One student described projects such as this one as “the reason I came to medical school.” The experience of offering workshops directly to health care providers working on the front lines of public health also gave students a sense of how their “contribution fell into the wider scheme of this topic,” and as a result, they “always felt motivated to work my hardest.” The design of case studies with the input of the community “put a face to the stories and words on the slides” and contributed to the sense of why it is important to “use cases based [on] patients with health disparities specific to the location we are living in” to make meaningful practice changes.
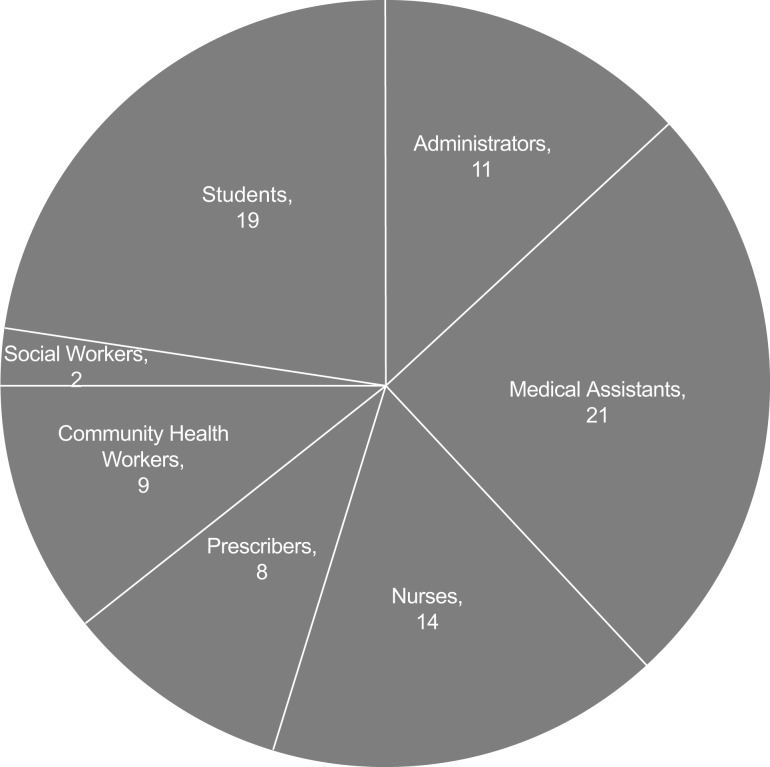
Workshop Attendee Knowledge and Confidence
A total of 107 people attended workshops both on campus and in the community at the LCHD, including students, nurses, medical assistants, social workers, community health workers, prescribers (physicians and advanced practice nurses), and administrators. Postworkshop surveys were returned by 84 attendees (Figure 2), yielding a response rate of 78.5%. Mean scores (all > 4.0) for items on the postworkshop survey indicated attendees felt confident in discussing HIV risk and PrEP with patients and in their knowledge of PrEP (Table 2). Specifically, workshop attendees indicated that they felt they had a comprehensive understanding of the rationale for prescribing PrEP (M = 4.7, SD = 0.5), of patients indicated for PrEP (M = 4.6, SD = 0.6), and of the social factors at play in access to PrEP for HIV prevention (M = 4.8, SD = 0.5). No mean responses differed significantly between groups of attendees (all ps > .05), as determined by ANOVA.
Figure 2. Graphical representation of professional disciplines of the individuals who attended the workshops hosted by the student team. The Prescribers category includes two nurse practitioners and six physicians.
Table 2. Mean Attendee Responses to Postworkshop Survey (N = 84).
| Item | M (SEM) |
|---|---|
| I feel I have a comprehensive understanding of the rationale for prescribing PrEP. | 4.7 (0.1) |
| I feel I have the skills necessary to identify a patient who may benefit from PrEP therapy. | 4.6 (0.1) |
| I feel comfortable in my understanding of the long-term requirements to maintain a PrEP prescription. | 4.6 (0.1) |
| I feel comfortable beginning a conversation with my patients that could benefit from PrEP. | 4.6 (0.1) |
| I have an understanding of the regulatory complications that may arise when prescribing PrEP to an eligible patient. | 4.4 (0.1) |
| I have an understanding of the potential pharmacological interactions of PrEP, and feel that I am comfortable in my ability to consider or in my ability to find more information concerning the medication interactions before writing a prescription for PrEP. | 4.3 (0.1) |
| I have a greater appreciation for the social factors that may contribute to or prohibit a patient from beginning PrEP therapy. | 4.8 (0.1) |
Abbreviation: PrEP, pre-exposure prophylaxis.
Discussion
Overall, the results from the RFUMS student team indicated a positive experience working on this project and increased self-reported knowledge about HIV risk factors, PrEP access, and interprofessional collaboration. Student-written reflections also demonstrated that students learned significantly from interactions with the Lake County community and their fellow teammates.
This activity provides one avenue for increasing content in medical education about HIV prevention and LGBTQ+ medical care. The materials provided here detail the framework for medical schools to guide the process of implementing this cocurricular project for creating a customized training module about HIV risk and PrEP access in their communities. This activity is designed for immediate replication at other schools that have an interest in providing education about HIV risk and PrEP access from both national and local perspectives.
Adaptation requires a student team to assemble a training module that addresses both of these issues from both national and local perspectives, using the template case studies and workshop presentation as a framework. This in turn requires mastery of the material sufficient to host workshops. Workshop attendees then provide an additional perspective on these issues through case discussion, drawing on personal and professional experiences, which creates a reciprocal learning experience. The training module presentation (Appendix D) and case studies (Appendices B and C) are examples for guidance to adapt this project and create a new, community-specific training module.
The application of this project to other medical schools and local communities is simplified in that it does not require dedicated classroom or instructional time. The activities required of the student team may be completed outside scheduled classes, and there is a great degree of flexibility within the student team workflow. One option would be to include the development of the training module as an element of an existing course. Another would be to offer students the opportunity to establish a team and earn required service-learning hours via creating a training module. The latter was the case in this pilot implementation, as all first-year students had to complete service-learning hours for a course requirement. Adaptation and implementation of the training module could also be implemented by a subcommittee of the executive board of a student-run clinic or similar community-outreach initiative.
The design of the project was centered around an interprofessional approach addressing Liaison Committee on Medical Education (LCME) standards 7.8 and 7.9, which focus on communication skills and interprofessional collaborative skills, respectively.37 Other elements of this activity, including the focus on cultural competence in providing HIV preventive care and its role as a potential barrier to PrEP access, encompass LCME standard 7.6, which describes cultural competence and health care disparities. Finally, if workshops are hosted for community health care venues, such as those at a local health department or other community health agency, this activity provides an opportunity to encompass LCME standard 6.6, which is related to service learning. As this activity is designed to be completed by a small group of students, it is best suited as one option within a larger program of service learning in order to provide structured opportunities for students interested in education and provision of community-based health care.
We acknowledge that the interprofessional composition of the student team may not be a possibility for institutions without multiple health professions academic programs. While having an interprofessional composition adds an additional layer of learning and skill building, lacking it should not deter institutions without multiple programs from adapting this training module. For institutions with only medical students, the process of researching HIV risk and PrEP access in their community and conveying this information is still beneficial. Regarding assessment, items relating to interprofessional collaboration should be omitted from the student postparticipation reflection instrument (Appendix E) if the team is uniprofessional.
A potential and significant barrier to successful adaptation and implementation of this training module may be garnering community and campus buy-in. Regarding community partners, those agencies that may be apt audiences for workshops should be carefully selected to ensure that the training reaches the practitioners most likely to benefit from it. We provided workshops to the public health department because each clinic had designated all-staff meeting time, a portion of which was reserved for our workshops. Agencies with this structure of dedicated meeting time may be promising avenues to explore for finding community partners willing to host workshops from the student team. On-campus workshops are also a valuable mechanism for disseminating the materials in the training module, especially if it is possible to schedule the workshop during an ongoing seminar series, such as grand rounds, as was the case here.
There are several limitations to the present assessment design of this project. The first is the lack of a pre-/postassessment comparison. The self-reflection instrument was given to students only after participating in the activity. Because this project ran over the course of several months, ensuring that any improvements were directly due to it would have been difficult. Academic activities, including some courses about infectious disease and some focused on interprofessional education and collaboration, occurred throughout the pilot implementation. These could have confounded results and would be difficult to correct for in analysis of the background questions and the IPEC competency self-ratings. For this reason, the self-reflection free-response items were analyzed to provide context for the numerical results. Finally, assessment was based solely on self-report of knowledge. As all students who participated in this project were in their preclinical years, there were no opportunities to observe and assess application of knowledge through patient encounters. Institutions that choose to adapt and replicate this training activity could explore the possibility of a more longitudinal assessment scheme. Students who participate in the project during their preclinical years may be given a follow-up survey in clinical years to determine whether any of the skills developed during the activity are used in subsequent patient interactions.
Another limitation is the small sample size (N = 11). This made statistical analysis beyond descriptive statistics difficult and also makes it difficult to generalize the findings. While the team size at the pilot university was small, plans are in development to replicate this project at a number of other health sciences universities in the United States. Replication with coordinated assessment using a standardized self-reflection instrument will increase the sample size and will also provide generalizable findings, as each implementation site will create a training module specific to its community, HIV risk factors, and barriers to PrEP access.
Appendices
A. PrEP Workshop Facilitator's Guide.pdf
B. Case Studies 1-5 - Participant Version.docx
C. Case Studies 1-5 - Facilitator Version.docx
D. Sample PrEP Workshop.pptx
E. PrEP Workshop Student Reflection Instrument.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Acknowledgments
The authors graciously acknowledge the student team who collaborated to make this project come to fruition: Adam Koss, Amanda Sailors, Brianna Norris, Christopher Gideon, Javier Navarrete, Jessica Matthiesen, Kaitlyn Woodman, Morgan Schumacher, Natalie Shovlin-Bankole, Nikhil Patel, and Yousef Nafal.
Disclosures
None to report.
Funding/Support
The Department of Student Life at Rosalind Franklin University of Medicine and Science provided funding for workshop printing and supplies through the Franklin Fellowship Program during the 2017–2018 academic year.
Ethical Approval
Reported as not applicable.
References
- 1.Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol 29 http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html Published November 2018. Accessed February 2, 2019. [Google Scholar]
- 2.Eaton LA, Matthews DD, Bukowski LA, et al; POWER Study Team. Elevated HIV prevalence and correlates of PrEP use among a community sample of black men who have sex with men. J Acquir Immune Defic Syndr. 2018;79(3):339–346. https://doi.org/10.1097/QAI.0000000000001822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant RM, Lama JR, Anderson PL, et al; for iPrEx Study Team. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. https://doi.org/10.1056/NEJMoa1011205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson PL, Glidden DV, Liu A, et al; for iPrEx Study Team. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra125 https://doi.org/10.1126/scitranslmed.3004006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCormack S, Dunn DT, Desai M, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60. https://doi.org/10.1016/S0140-6736(15)00056-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tetteh RA, Yankey BA, Nartey ET, Lartey M, Leufkens HGM, Dodoo ANO. Pre-exposure prophylaxis for HIV prevention: safety concerns. Drug Saf. 2017;40(4):273–283. https://doi.org/10.1007/s40264-017-0505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcus JL, Hurley LB, Hare CB, et al. Preexposure prophylaxis for HIV prevention in a large integrated health care system: adherence, renal safety, and discontinuation. J Acquir Immune Defic Syndr. 2016;73(5):540–546. https://doi.org/10.1097/QAI.0000000000001129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis–to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018;28(12):841–849. https://doi.org/10.1016/j.annepidem.20106.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDS. 2015;29(8):423–42. https://doi.org/10.1089/apc.2014.0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hammack PL, Meyer IH, Krueger EA, Lightfoot M, Frost DM. HIV testing and pre-exposure prophylaxis (PrEP) use, familiarity, and attitudes among gay and bisexual men in the United States: a national probability sample of three birth cohorts. PLoS One. 2018;13(9):e0202806 https://doi.org/1371/journal.pone.0202806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krakower DS, Oldenburg CE, Mitty JA, et al. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: results from a survey of healthcare providers in New England. PLoS One. 2015;10(7):e0132398 https://doi.org/10.1371/journal.pone.0132398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krakower DS, Mayer KH. The role of healthcare providers in the roll out of preexposure prophylaxis. Curr Opin HIV AIDS. 2016;11(1):41–48. https://doi.org/10.1097/COH.0000000000000206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, Kelly JA. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21(5):1256–1267. https://doi.org/10.1007/s10461-016-1625-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar V, Patil K, Munoli K. Knowledge and attitude toward human immunodeficiency virus/acquired immunodeficiency syndrome among dental and medical undergraduate students. J Pharm Bioallied Sci. 2015;7(6):666–671. https://doi.org/10.4103/0975-7406.163598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mani SB, Bral DO, Soltanianzadeh Y, et al. Evaluating HIV and STI attitudes and knowledge in first-year medical students. J Student-Run Clin. 2018;4(1). [Google Scholar]
- 16.Nama N, MacPherson P, Sampson M, McMillan HJ. Medical students’ perception of lesbian, gay, bisexual, and transgender (LGBT) discrimination in their learning environment and their self-reported comfort level for caring for LGBT patients: a survey study. Med Educ Online. 2017;22(1):1368850 https://doi.org/10.1080/10872981.2017.1368850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seaborne LA, Prince RJ, Kushner DM. Sexual health education in U.S. physician assistant programs. J Sex Med. 2015;12(5):1158–1164. https://doi.org/10.1111/jsm.12879 [DOI] [PubMed] [Google Scholar]
- 18.Hillenburg KL, Murdoch-Kinch CA, Kinney JS, Temple H, Inglehart MR. LGBT coverage in U.S. dental schools and dental hygiene programs: results of a national survey. J Dent Educ. 2016;80(12):1440–1449. [PubMed] [Google Scholar]
- 19.Cornelius JB, Enweana I, Alston CK, Baldwin DM. Examination of lesbian, gay, bisexual, and transgender health care content in North Carolina schools of nursing. J Nurs Educ. 2017;56(4):223–226. https://doi.org/10.3928/01484834-20170323-06 [DOI] [PubMed] [Google Scholar]
- 20.Stewart K, O’Reilly P. Exploring the attitudes, knowledge and beliefs of nurses and midwives of the healthcare needs of the LGBTQ population: an integrative review. Nurse Educ Today. 2017;53:67–77. https://doi.org/10.1016/j.nedt.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 21.Ford JV, Barnes R, Rompalo A, Hook EW III. Sexual health training and education in the U.S. Public Health Rep. 2013;128(2)(suppl 1):96–101. https://doi.org/10.1177/00333549131282S111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bauler TJ, Cole S, Gibb T, Van Enk R, Lutwick L, Dickinson BL. HIV/AIDS: a case-based learning module for first-year medical students. J Microbiol Biol Educ. 2018;19(2). https://doi.org/10.1128/jmbe.v19i2.1587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sell J, George D, Levine MP. HIV: a socioecological case study. MedEdPORTAL. 2016;12:10509 https://doi.org/10.15766/mep_2374-8265.10509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koechlin FM, Fonner VA, Dalglish SL, et al. Values and preferences on the use of oral pre-exposure prophylaxis (PrEP) for HIV prevention among multiple populations: a systematic review of the literature. AIDS Behav. 2017;21(5):1325–1335. https://doi.org/10.1007/s10461-016-1627-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention: US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf Published March 2018.
- 26.Simmons R, Siegel J. Introduction to HIV and addiction medicine for residents: integrated case-based learning. MedEdPORTAL. 2016;12;10375 https://doi.org/10.15766/mep_2374-8265.10375 [Google Scholar]
- 27.Person A, Chastain C, Skaug L, Rawn L, Wright P. Four standardized patient cases for the infectious diseases fellow. MedEdPORTAL. 2016;12;10379 https://doi.org/10.15766/mep_2374-8265.10379 [Google Scholar]
- 28.Hunt BR, Picard C, Hirschtick JL, Glick N. HIV testing prevalence in selected Chicago community areas: the importance of local-level data. AIDS Care. 2018;30(7):817–820. https://doi.org/10.1080/09540121.2018.1447081 [DOI] [PubMed] [Google Scholar]
- 29.Braun HM, Ramirez D, Zahner GJ, Gillis-Buck EM, Sheriff H, Ferrone M. The LGBTQI health forum: an innovative interprofessional initiative to support curriculum reform. Med Educ Online. 2017;22(1):1306419 https://doi.org/10.1080/10872981.2017.1306419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calzo JP, Melchiono M, Richmond TK, et al. Lesbian, gay, bisexual, and transgender adolescent health: an interprofessional case discussion. MedEdPORTAL. 2017;13;10615 https://doi.org/10.15766/mep_2374-8265.10615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jones SR, Abes ES. Developing student understanding of HIV/AIDS through community service-learning: a case study analysis. J Coll Stud Dev. 2003;44(4):470–488. https://doi.org/10.1353/csd.2003.0040 [Google Scholar]
- 32.Jones SR, LePeau LA, Robbins CK. Exploring the possibilities and limitations of service-learning: a critical analysis of college student narratives about HIV/AIDS. J Higher Educ. 2013;84(2):213–238. https://doi.org/10.1353/jhe.2013.0010 [Google Scholar]
- 33.Sharma M, Pinto AD, Kumagai AK. Teaching the social determinants of health: a path to equity or a road to nowhere? Acad Med. 2018;93(1):25–30. https://doi.org/10.1097/ACM.0000000000001689 [DOI] [PubMed] [Google Scholar]
- 34.Interprofessional Education Collaborative. Core Competencies for Interprofessional Collaborative Practice: 2016 Update. Washington, DC: Interprofessional Education Collaborative; 2016. [Google Scholar]
- 35.Lockeman KS, Dow AW, DiazGranados D, et al. Refinement of the IPEC competency self-assessment survey: results from a multi-institutional study. J Interprof Care. 2016;30(6):726–731. https://doi.org/10.1080/13561820.2016.1220928 [DOI] [PubMed] [Google Scholar]
- 36.Thannhauser J, Russell-Mayhew S, Scott C. Measures of interprofessional education and collaboration. J Interprof Care. 2010;24(4):336–349. https://doi.org/10.3109/13561820903442903 [DOI] [PubMed] [Google Scholar]
- 37.Liaison Committee on Medical Education. Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD Degree. Washington, DC: Liaison Committee on Medical Education; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. PrEP Workshop Facilitator's Guide.pdf
B. Case Studies 1-5 - Participant Version.docx
C. Case Studies 1-5 - Facilitator Version.docx
D. Sample PrEP Workshop.pptx
E. PrEP Workshop Student Reflection Instrument.docx
All appendices are peer reviewed as integral parts of the Original Publication.