INTRODUCTION
Interest in alternatives to conventional medical approaches for psychological and physical maladies has been growing rapidly in recent years. Complementary and integrative (CI) interventions, defined as a set of diverse practices that are not considered a part of conventional medicine (National Center for Complementary and Integrative Health, 2015), may be used in conjunction with or instead of conventional treatment. Over one third of U.S. adults use some form of CI therapy and “mind-body” practices such as deep breathing exercises, meditation, and yoga (Barnes, Bloom, & Nahin, 2008).
Posttraumatic stress disorder (PTSD) is a debilitating psychological disorder that affects 6% of U.S. adults in their lifetimes (Kessler, Chiu, Demler & Walters, 2005), and within the Veterans Health Administration (VHA) PTSD is the third most prevalent psychiatric diagnosis (Stecker, Fortney, Owen, McGovern, & Williams, 2010). Many individuals with PTSD do not seek conventional mental health services due to stigma and accessibility (Hoge, Castro, Messer, McGurk, Cotting, & Koffman, 2004). Moreover, a substantial proportion of those who do seek treatment do not experience relief (Steenkamp, Litz, Hoge, & Marmar, 2015). Empirically-supported treatments for PTSD that direct individuals to recall traumatic events in a controlled fashion have been shown to be clinically effective in ameliorating symptoms (Foa, Hembree, & Rothbaum, 2007; Resick, Monson, & Chard, 2007), but up to 50% of individuals with PTSD either drop out of these standard therapies or are not substantially helped by them (Schottenbauer, Glass, Arnkoff, Tendick, & Gray, 2008; Steenkamp et al., 2015). Thus, other empirically supported treatments are needed to address PTSD symptoms for those who cannot or choose not to engage in the treatments currently available and for those whose symptoms remain after completing treatment.
CI approaches to alleviate symptoms of PTSD are gaining popularity and recent surveys indicate that 20% of those diagnosed with PTSD and up to 46% of veterans and military personnel use CI modalities to address symptoms (Bystritsky et al., 2012; Davis, Mulvaney-Day, Larson, Hoover & Mauch, 2014; Libby, Pilver, & Desai, 2013). In VHA, where up to 25% of returning Veterans seeking medical treatment suffer from PTSD (Schell & Marshall, 2008), over 90% of VA specialized PTSD treatment programs offer CI treatments (Libby, Pilver, & Desai, 2012), with stress management/relaxation, progressive muscle relaxation, and guided imagery most commonly used (VA Healthcare Analysis and Information Group, 2011).
Although CI interventions for PTSD are widely utilized and attract great interest, empirical support has not been well established and the Institute of Medicine (IOM) has called for more research to evaluate the efficacy of these treatments (IOM, 2012). Published reviews of the burgeoning scientific evidence indicate encouraging findings, but underscore the scant extant literature to support CI interventions for PTSD (e.g. Banks, Newman, & Saleem, 2015; Kim, Schneider, Kravitz, Mermier & Burge, 2013b; Hilton et al., 2016; Khusid &Vythilingam, 2016; Wahbeh, Senders, Neuendorf and Cayton, 2014; Wei et al., 2016). For example, in a systematic review using rigorous inclusion criteria, Strauss and Lang (2012) identified seven randomized control trials (RCTs) and two nonrandomized studies and reported that acupuncture had the highest quality evidence, but that evidence was limited to one RCT. A review specifically focused on mind-body therapies for veterans and military personnel across medical and psychiatric conditions noted that available RCTs were generally of low-quality; they concluded that mind-body therapies such as yoga or tai chi, although routinely offered in clinical care, do not seem to be adequately represented in research (Elwy, Johnston, Bormann, Hull and Taylor, 2014).
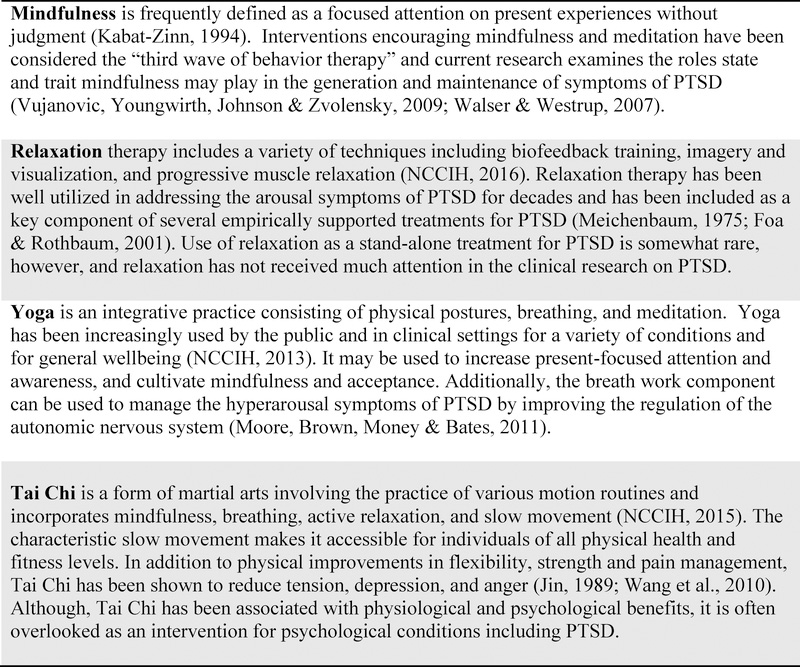
Given the high interest in mind-body therapies in the treatment of PTSD and the proliferation of relevant studies in recent years, periodic reviews of the accumulating literature are useful for guiding treatment offerings and research priorities. The current review differs from previous reviews of CI treatments for PTSD in that it is limited to RCTs, uses strict inclusion criteria, and is focused on four specific mind-body therapies utilized in clinical settings: mindfulness, relaxation, yoga and tai chi. (See Figure 1). These four therapies were chosen because they require active involvement from the participant, are highly “portable,” and have great potential for dissemination because they are typically delivered in group settings with minimal need for equipment. Passive mind-body interventions such as massage or acupuncture were excluded from this review as they are a qualitatively distinct group of treatments that require one-on-one attention from a practitioner and may require specialized equipment (e.g. massage table, acupuncture needles). The purpose of the current manuscript was to review the published RCTs of mindfulness, yoga, tai chi, and relaxation that address PTSD symptoms and meet a standard for quality and relevance.
Figure 1.
Definitions of Mind-body Interventions Searched for to Include in this Review
METHODS
Literature Search and Eligibility Criteria
Electronic literature searches were conducted using PubMed, Published International Literature on Traumatic Stress (PILOTS) and four EBSCO databases (Psychology and Behavioral Sciences Collection, PsycINFO, PsycARTICLES, and SocINDEX). In order to capture all randomized controlled trials that were related to mindfulness, yoga, tai chi, and relaxation, the following mind-body therapy search terms were used: mindfulness, yoga, qigong, qi gong, chi kung, chikung, tai ji, tai chi, relaxation, relaxation therapy, progressive muscle relaxation, breathing exercises, meditation, transcendental meditation, mental healing, faith healing, spiritual healing, prayer, imagery, and guided imagery. The PTSD search terms were: posttraumatic, post traumatic, PTSD, combat stress, soldier, warrior, veteran and combat. The randomized controlled trial search terms were: randomized controlled trial, randomized, and controlled clinical trial.
Additionally, the authors performed a search in Google Scholar with the search terms mind-body, PTSD, and randomized because some journals have yet to be indexed in PubMed, PILOTS and the EBSCO databases. This search resulted in the inclusion of one additional study. Randomized controlled trials conducted on adult populations and published in English between January 1985 and January 2017 were selected. Studies that examined mindfulness, yoga, tai chi, or relaxation as an intervention for PTSD and compared to an intervention or control group were eligible. Mind-body therapies that were used in conjunction with or as a part of other more traditional therapies were excluded from review (e.g. relaxation used in Prolonged Exposure Therapy, mindfulness used in Mindfulness Based Cognitive Therapy).
Risk of Bias Assessment
Based on PRISMA guidelines (Liberati et al., 2009), the following “risk of bias” inclusion criteria were chosen to determine the quality and relevance of the identified articles: (1) study aims that include evaluation of treatment efficacy for PTSD outcomes; (2) eligibility criteria explicitly included a minimal level of symptoms of PTSD or a diagnosis of PTSD; (3) random assignment of individuals to groups; (4) interventions adequately developed and described; (5) valid quantitative outcome measurements; (6) appropriate statistical methods; (7) dropout rates reported; and (8) conclusions supported by findings. For each study included in the systematic review (see Table 1), two investigators independently determined that the 8 criteria described above were met. Additional study characteristics that were considered and used to highlight studies of highest quality include: sample size, use of a credible control intervention, use of blinded assessors, evaluation of treatment fidelity, use of intent to treat (ITT) analyses, reporting of within- and between-group effect sizes, and inclusion of follow-up assessments.
Table 1.
Randomized Controlled Trials of Mindfulness and Yoga for Posttraumatic Stress Disorder
| Source | Population N = enrolled Age (% women) | Mind-Body Intervention(s) n (Frequency and Duration) | Comparison Intervention(s) n (Frequency and Duration) | PTSD Outcome Measures (Additional Measures) | Pre to Post Effect Sizes (Underlined treatment indicates greater symptom reductions) |
|---|---|---|---|---|---|
| MINDFULNESS (8 ARTICLES) | |||||
| Bormann et al. (2008) | Veterans with PTSD N = 33 Mean age = 56 (0% women) | Mantram Repetition (MR) Randomized: n = 14 Completed: n = 14 (6 weekly 90-min group sessions) | Delayed-Intervention Control Group (DI) Randomized: n = 15 Completed: n = 15 | CAPS; PCL (BSI-I8; FACIT-SpEx4; MAAS; Q-LES-Q: SF; STAXI-2) | Between Groups: CAPS: MR vs DI (d = 0.33) PCL: MR vs DI (d = 0.72) Within Group: CAPS (NR) PCL (d = 0.70) |
| Bormann et al. (2013) | Veterans with PTSD N = 146 Mean age = 57 (3% women) | Mantram Repetition Program (MR) + Treatment-As-Usual Randomized: n = 71 Completed: n = 66 (6 weekly 90-min group sessions) | Treatment-As-Usual (TAU) Randomized: n = 75 Completed: n = 70 | CAPS; PCL (BSI-18; FACIT-Sp; SF-12) | Between Groups: CAPS: MR vs TAU (= 0.03) PCL: MR vs TAU (= 0.03) Within Group: CAPS (NR) PCL (NR) |
| Kearney et al. (2013) | Veterans with PTSD N = 47 Mean age = 52 (21.3% women) | Mindfulness-Based Stress Reduction + Treatment-As-Usual (MBSR) Randomized: n = 25 Completed: n = 21 (8 weekly 2.5-hr group sessions plus 7-hr group session) | Treatment-As-Usual (TAU) Randomized: n = 22 Completed: n = 21 | PCL-C (BADS; FFMQ; PHQ-9; SF-8) | Between Groups: PCL-C: MBSR vs TAU (d = 0.51) Within Group: PCL-C (d = 0.63) |
| Kelly & Garland (2016) | Female Survivors of IPV N = 45 Mean age = 41.5 (100% women) | Trauma Informed -Mindfulness-Based Stress Reduction (TI-MBSR) Randomized: n = 24 Completed: n = 20 (8 weekly 2–2.5-hr group sessions) | Wait-List Control Group (WL) Randomized: n = 21 Completed: n = 19 | PCL-C (BDI-II; RSQ) | Between Groups: PCL-C: TI-MBSR vs WL (d = 0.94) Within Group: PCL-C (NR) |
| Kim et al. (2013a) | Intensive care unit nurses N = 29 Mean age = 45.7 (96.6% women) | Mindfulness- Based Stretching and Deep Breathing Randomized: n = 11 Completed: n = 11 (16 twice-weekly 60-min group sessions) | Wait-List Control Group Randomized: n = 11 Completed: n = 10 Non-PTSD Group Randomized: n = 7 Completed: n = 7 | PCL-C (Plasma ACTH; Serum Cortisol; Serum DHEAS) | Between Groups: PCL-C (NR) Within Group: PCL-C (NR) |
| Niles et al. (2012) | Veterans with PTSD N = 33 Age range = 52.0 (0% women) | Telehealth Mindfulness (TM) Randomized: n = 17 Completed: n = 16 (2 in-person 45-min sessions and 6 weekly 20-min telephone sessions) | Telehealth Psychoeducation (TP) Randomized: n = 16 Completed: n = 14 (2 in-person 45-minute sessions and 6 weekly 20-min telephone sessions) | CAPS; PCL-M | Between Groups: CAPS: TM vs TP (= 0.183) PCL-M: TM vs TP (= 0.303) Within Group: CAPS (= 0.502) PCL-M (= 0.556) |
| Polusny et al. (2015) | Veterans with PTSD N = 116 Mean age = 58.5 (16% women) | Mindfulness-Based Stress Reduction (MBSR) Randomized: n = 58 Completed: n = 47 (8 weekly 2.5-hr group sessions and a 6.5-hr retreat) | Present-Centered Therapy (PCT) Randomized: n = 58 Completed: n = 57 (9 weekly 1.5-hr group sessions) | CAPS; PCL (CEQ; FFMQ; LEC; PHQ-9; WHOQoL-BRIEF) | Between Groups: CAPS: MBSR vs PCT (d = 0.41) PCL: MBSR vs PCT (d = 0.40) Within Group: CAPS (NR) PCL (NR) |
| Possemato et al. (2016) | VA primary care patients with symptoms of PTSD N = 62 Mean age = 46.4 (12.9% women) | Primary Care Brief Mindfulness Training (PCBMT) Randomized: n = 36 Completed: n = 16 (4 weekly 1.5-hr group sessions) | Primary Care Treatment As Usual (PCTAU) Randomized: n = 26 Completed: n = 24 | CAPS; PCL-S (PHQ-9; MAAS; FFMQ) | Between Groups: CAPS: PCBMT vs PCTAU (d = 0.24) PCL-S: PCBMT vs PCTAU (d = 0.26) Within Group: CAPS (NR) PCL-S (NR) |
| YOGA (5 ARTICLES) | |||||
| Carter et al. (2013) | Vietnam veterans with PTSD N = 50 Mean age = 58.5 (0% women) | Sudarshan Kriya Yoga (Y) Randomized: n = 16 Completed: n = 14 (22-hr group sessions over 5 days plus 9 2-hr follow-up sessions) | Delayed-Intervention Control Group (DI) Randomized: n = 15 Completed: n = 11 | CAPS; PCL-M (AUDIT; CES-D; MINI-Plus; WHOQoL-BRIEF) | Between Groups: CAPS: Y vs DI (= 0.17) PCL-M: Y vs DI (= 0.41) Within Group: Y: CAPS (d = 0.90) PCL-M (NR) DI after intervention: CAPS (d = 1.20) PCL-M (NR) |
| Jindani et al. (2015) | Individuals with PTSD N = 80 Median age = 41 (88.8% women) | Kundalini Yoga (Y) Randomized: n = 59 Completed: n = 29 (8 weekly 90-min group sessions) | Wait-List Control Group (WL) Randomized: n = 21 Completed: n = 21 | PCL-17 (RS; PANAS; FFMQ; ISI; PSS; DASS 21) | Between Groups: PCL-17: Y vs WL (= 0.25) Within Group: PCL-17 (NR) |
| Mitchell et al. (2014) | Individuals with PTSD (veterans and civilians) N = 38 Mean age = 44.4 (100% women) | Kripalu Yoga (Y) Randomized: n = 20 Completed: n = 14 (12 75-min group sessions option for weekly or twice-weekly) | Assessment Control Group (ACG) Randomized: n = 18 Completed: n = 12 (12 weeks) | PCL-C (PSS-I; TLEQ; CES-D; STAI) | Between Groups: PCL-C: Y vs ACG (0.20)* Within Group: PCL-C (NR) |
| Seppala et al. (2014) | OEF/OIF Veterans with PTSD N = 21 Mean age = 28.65 (0% women) | Sudarshan Kriya Yoga (Y) Randomized: n = 11 Completed: n = 10 (7 daily 3-hr group sessions) | Wait-List Control Group (WL) Randomized: n = 10 Completed: n = 9 | PCL-M (MASQ) | Between Groups: PCL-M: Y vs WL (d = 1.16) Within Group: PCL-M (NR) |
| van der Kolk et al. (2014) | Individuals with chronic, treatment-resistant PTSD N = 64 Mean age = 42.9 (100% women) | Trauma-Informed Hatha Yoga (Y) Randomized: n = 32 Completed: n = 31 (10 weekly 60-min group sessions) | Supportive Women’s Health Education (SWHE) Randomized: n = 32 Completed: n = 29 (10 weekly 60-min group sessions) | CAPS; DTS (SCID-IV; BDI; IAS) | Between Groups: CAPS: Y vs SWHE (d = 0.41) DTS: Y vs SWHE (d = 0.34) Within Group: CAPS (d = 1.07) DTS (d = 0.52) |
Note. Cohen’s d effect sizes: small = 0.1–0.3; moderate = 0.3–0.5; large = >0.5.
Partial eta squared effect sizes: small = 0.01–0.06; moderate = 0.06–0.15; large = >0.15.
= Finegold’s formula for effect size which is analogous to Cohen’s d
Key: ACG (Assessment Control Group); DI (Delayed Intervention); IPV (Interpersonal Violence); MBSR (Mindfulness-Based Stress Reduction); MR (Mantram Repetition); NR (Not Reported); OEF (Operation Enduring Freedom); OIF (Operation Iraqi Freedom); PCT (Present-Centered Therapy); PCBMT (Primary Care Brief Mindfulness Training); PCTAU (Primary Care Treatment As Usual); PTSD (Posttraumatic Stress Disorder); SWHE (Supportive Women’s Health Education); TAU (Treatment-As-Usual); TM (Telehealth Mindfulness); TP (Telehealth Psychoeducation); VA (Veteran Affairs); WL (Wait-List); Y (Yoga)
Measures: AUDIT (Alcohol Use Disorders Identification Test); BADS (Behavioral Activation for Depression Scale); BDI (Beck Depression Inventory); BSI (Brief Symptom Inventory); CAPS (Clinician Administered PTSD Scale); CEQ (Credibility/Expectancy Questionnaire); CES-D (Center for Epidemiological Studies-Depression Scale); DASS 21 (Depression, Anxiety, and Stress Scale); DTS (Davidson Trauma Scale); FACIT-Sp (Functional Assessment of Chronic Illness Therapy-Spiritual Well-being Scale); FACIT-SpEx4 (Functional Assessment of Chronic Illness Therapy-Spirituality-Expanded); FFMQ (Five Facet Mindfulness Questionnaire); IAS (Inventory of Altered Self-Capacities); ISI (Insomnia Severity Index); LEC (Life Events Checklist); MAAS (Mindfulness Attention Awareness Scale); MASQ (Mood and Anxiety Symptoms Questionnaire); MINI (Mini International Neuropsychiatric Interview); PANAS (Positive and Negative Affect Schedule); PCL (PTSD Checklist); PCL-C (PTSD Checklist-Civilian); PCL-M (PSTD Checklist-Military); PCL-S (PTSD Checklist-Specific); PCL-17 (PTSD Checklist 17 Item Self Report); PHQ (Patient Health Questionnaire); PSS (Perceived Stress Scale); PSS-I (PTSD Symptom Scale-Interview); Q-LES-Q: SF (Quality of Life Enjoyment and Satisfaction: Short Form); RS (Resilience Scale); SCID-IV (Structured Clinical Interview for DSM-IV); SF (Health Survey Short Form); STAI (State-Trait Anxiety Inventory); STAXI (State-Trait Anger Expression Inventory); TLEQ (Traumatic Life Events Questionnaire); WHOQoL (World Health Organization’s Quality of Life Inventory)
RESULTS
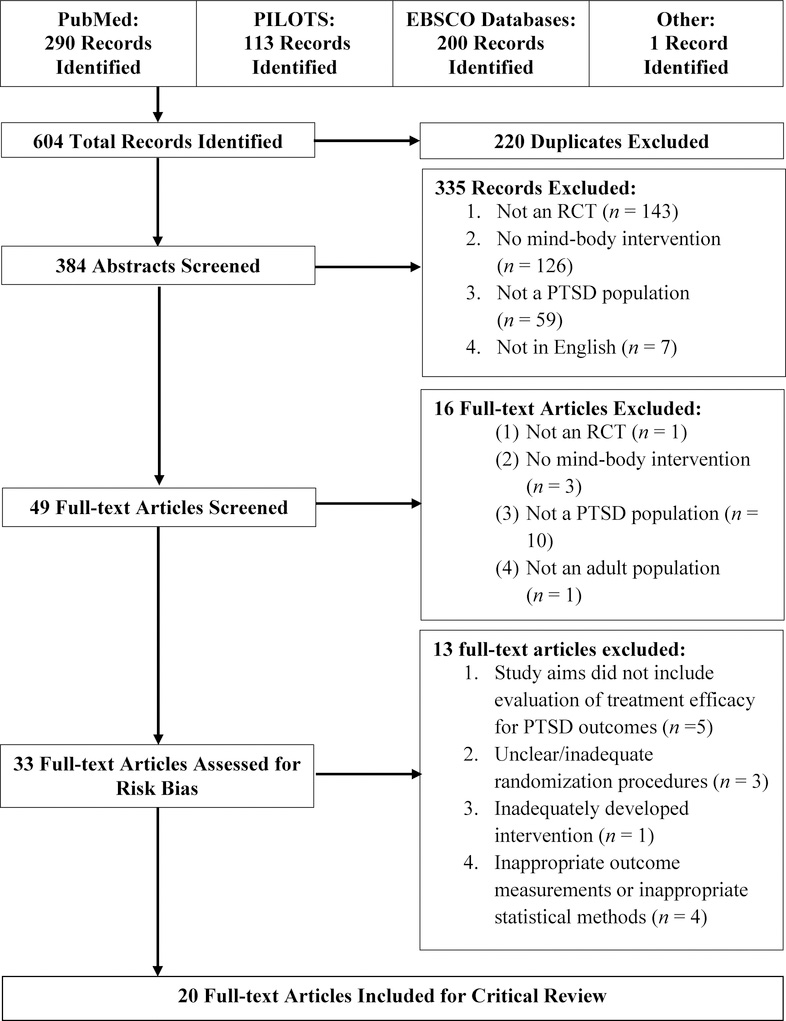
Twenty full-text articles met inclusion criteria and were included for critical review. No RCTs examining tai chi or qi gong for PTSD met the above inclusion criteria. Tables 1 and 2 provide findings from the studies that met criteria for inclusion and each study is reviewed in text below. Figure 2 illustrates the study flow, number of studies screened, and reasons for exclusion.
Table 2.
Randomized Controlled Trials of Relaxation for Posttraumatic Stress Disorder
| Source | Population N = enrolled Age (% women) | Mind-Body Intervention(s) n (Frequency and Duration) | Comparison Intervention(s) n (Frequency and Duration) | PTSD Outcome Measures (Additional Measures) | Within Group Pre to Post Effect Sizes for Relaxation Condition |
|---|---|---|---|---|---|
| RELAXATION (7 ARTICLES) | |||||
| Carletto et al. (2016) | Patients with MS diagnosed with PTSD N = 50 Mean age = 40.1 (81% women) | Relaxation Therapy Randomized: n = 25 Completed: n = 22 (10 60-min sessions conducted over 12–15 weeks) | EMDR Randomized: n = 25 Completed: n = 20 (10 60-min sessions conducted over 12–15 weeks) | CAPS; IES-R; (SCID-IV; HADS; CMDI; FAMS; TAQ; FSS; EDSS) | Within Group: CAPS (= NR) IES-R (= NR) |
| Hinton et al. (2011) | Latino patients with treatment- resistant PTSD N = 24 Mean age = 49.5 (100% women) | Applied Muscle Relaxation Randomized: n = 12 Completed: n = 12 (14 weekly 60-min group sessions) | Culturally-Adapted Cognitive Behavioral Therapy Randomized: n = 12 Completed: n = 12 (14 weekly 60-min group sessions) | PCL-C (Emotion Regulation Scale; Nervios Scale; SCL-90-R) | Within Group: PCL-C (d = 0.80) |
| Markowitz et al. (2015) | Individuals with PTSD N = 110 Mean age = 40.10 (70% women) | Relaxation Therapy Randomized: n = 32 Completed: n = 21 (10 90-min group sessions over 14 weeks) | Prolonged Exposure Randomized: n = 38 Completed: n = 27 (10 90-min group sessions over 14 weeks) Interpersonal Psychotherapy Randomized: n = 40 Completed: n = 34 (14 weekly 50-min group sessions) | CAPS; PSS-SR (IIP; Q-LES-Q; SAS-SR; Self-initiated In Vivo Exposure Scale) | Within Group: CAPS (d = 1.32) PSS-SR (d = 0.71) |
| Marks et al. (1998) | Individuals with PTSD N = 87 Mean age = 38 (35.6% women) | Relaxation Randomized: n = 21 Completed: n = 20 (10 90-min sessions) | Prolonged Exposure Randomized: n = 23 Completed: n = 20 Cognitive Restructuring Randomized: n = 19 Completed: n = 18 (10 90-min individual sessions) Exposure + Cognitive Restructuring Randomized: n = 24 Completed: n = 19 (10 105-min sessions) | CAPS; IES; PSS (BDI; Fear Questionnaire; GHQ; STAI) | Within Group: CAPS (d = 0.60) IES (d = 0.08) PSS (NR) |
| Taylor et al. (2003) | Individuals with PTSD N = 60 Mean age = 37 (75% women) | Relaxation Training Randomized: n = 19 Completed: n = 15 (8 1 hr sessions) | Prolonged Exposure Randomized: n = 22 Completed: n = 15 EMDR Randomized: n = 19 Completed: n = 15 (All interventions: 8 1.5 hr sessions) | CAPS; PSS (SCID-IV; BDI; RTQ) | Within Group: CAPS (η2> 0.47) PSS (η2> 0.13) |
| Vaughan et al. (1994) | Individuals with PTSD N = 36 Mean age = 32 (63.9% women) | Applied Muscle Relaxation Randomized: n = 11 Completed: n = 11 (3–5 50 min sessions over 2–3 weeks) | Waitlist Control Group Randomized: n = 17 Completed: n = 17 EMD Randomized: n = 12 Completed: n = 12 Image Habituation Training Randomized: n = 13 Completed: n = 13 (Both interventions: 3–5 50 min sessions over 2–3 weeks) | IES; SI-PTSD (ADIS-R; STAI; BDI) | Within Group: SI-PTSD (NR) IES (NR) |
| Zucker et al. (2009) | Individuals in residential substance use treatment with PTSD symptoms N = 50 Age range = 18–60 (44.7% women) | Progressive Muscle Relaxation Randomized: n = NR Completed: n = 19 (At least 20-min daily for 4 weeks) | Respiratory Sinus Arrhythmia Biofeedback Randomized: n = NR Completed: n = 19 (At least 20-min daily for 4 weeks) | PCL-C; PTS-T scale from DAPS (BDI; ISI; SDNN; Substance Cravings Question) | Within Group: PCL-C (NR) PTS-T (NR) |
Note. All interventions contain individual treatment sessions unless otherwise noted.
Cohen’s d effect sizes: small = 0.1–0.3; moderate = 0.3–0.5; large = >0.5
Partial eta squared effect sizes: small = 0.01–0.06; moderate = 0.06–0.15; large = >0.15
Key: EMD (Eye Movement Desensitization); EMDR (Eye Movement Desensitization and Reprocessing); Multiple Sclerosis (MS); NR (Not Reported); NS (Not Significant); PTSD (Posttraumatic Stress Disorder); R (Relaxation/Relaxation Training)
Measures: ADIS-R (Anxiety Disorders Interview Schedule-Revised); BDI (Beck Depression Inventory); CAPS (Clinician Administered PTSD Scale); CMDI (Chicago Multiscale Depression Inventory); DAPS (Detailed Assessment of Posttraumatic States); EDSS (Expanded Disability Status Scale); FAMS (Functional Assessment of Quality of Life in Multiple Sclerosis); FSS (Fatigue Severity Scale); GHQ (General Health Questionnaire); HADS (Hospital Anxiety and Depression Scale); IES (Impact of Events Scale); IES-R (Impact of Events Scale-Revised); IIP (Inventory of Interpersonal Problems); ISI (Insomnia Severity Index); PCL-C (PTSD Checklist-Civilian); PSS (PTSD Symptoms Scale); PSS-SR (Posttraumatic Stress Scale-Self Report); PTS-T (Posttraumatic Stress-Total on the Detailed Assessment of Posttraumatic States); Q-LES-Q (Quality of Life Enjoyment and Satisfaction); RTQ (Reactions to Treatment Questionnaire); SAS-SR (Social Adjustment Scale-Self Report); SCID-IV (Structured Clinical Interview for DSM-IV); SCL (Symptom Checklist); SDNN (Standard Deviation of Normal-to Normal); SI-PTSD (PTSD Structured Interview); STAI (State-Trait Anxiety Inventory); TAQ (Trauma Antecedent Questionnaire)
Figure 2.
Article Selection Process.
Mindfulness
Two of the eight mindfulness studies identified evaluated mantram repetition with veteran participants (Bormann, Thorp, Wetherell & Golshan, 2008; Bormann, Thorp, Wetherell & Golshan, 2013). This meditation-based group treatment teaches tools for training attention and regulating emotion, including the silent repetition of a word or phrase called a mantram. The initial feasibility study (Bormann et al., 2008) used a delayed treatment control and found large between-group effects. The second, larger trial (Bormann et al., 2013) used a treatment-as-usual control. Between-group effect sizes on both clinician-assessed and self-reported PTSD symptoms were small in the second trial, although it is notable that the mantram repetition group showed additional reductions in clinician-assessed symptoms during the 6-week follow-up period, suggesting continued improvement following the intervention. Furthermore, the proportion of participants who showed clinically meaningful change in clinician-assessed PTSD symptoms was significantly higher in the mantram repetition group (24%) than in the control (12%).
Mindfulness-Based Stress Reduction (MBSR) was compared to treatment as usual in a study of veterans with PTSD (Kearney, McDermott, Malte, Martinez, & Simpson, 2013). No reliable between-groups effects on PTSD symptoms were found using ITT or completer analyses and there were no differences in the proportion of participants who achieved clinically significant changes in PTSD symptoms. However, a large within-group effect on PTSD symptoms was reported in the mindfulness condition.
Kim and colleagues (2013a) delivered 16 sessions of mindfulness-based stretching and deep breathing to Intensive Care Unit nurses with sub-clinical symptoms of PTSD. In this small study, between-groups ITT analyses indicated that those randomized to the mindfulness condition showed greater drops in self-reported PTSD symptoms than those in the waitlist control; symptom reductions were maintained at the 8-week follow-up.
A study with veteran participants examined a very brief (3.5 hours total) mindfulness intervention that was partially delivered via telephone and compared to a psychoeducation intervention of equal length (Niles, Klunk Gillis, Ryngala, Silberbogen, Paysnick, & Wolf, 2012). Completer analyses found large between-group effects on both clinician-assessed and self-reported PTSD symptoms as well as a significant difference between groups in the proportion of participants who achieved clinically significant change in self-reported symptoms (54% for mindfulness and 8% for psychoeducation). However, symptoms returned to baseline and the two groups did not differ significantly at the 6-week follow-up.
Primary care was the setting for a recent trial comparing 4-sessions of mindfulness training to treatment as usual for veterans with symptoms of PTSD (Possemato, Bergen-Cico, Treatman, Allen, Wade, & Pigeon, 2016). The authors found no differences between the two groups using ITT analyses and attributed this to the large proportion of veterans who did not attend even one mindfulness session (44.44%). Of the completers, the authors reported medium to large within group effect size changes and most (75%) experienced a clinically significant change in symptoms in either clinician-assessed or self-reported PTSD. The effect size and clinically significant changes were maintained at the 8-week follow-up.
A study conducted by Kelly and Garland (2016) randomized 45 female survivors of Interpersonal Violence (IPV) into either an 8-week Trauma Informed MBSR (TI-MBSR) program or a waitlist control. Using ITT analyses, it was found that participants in the TI-MBSR condition experienced a significant reduction in their self-reported posttraumatic stress symptoms when compared to the waitlist control. In addition, a large effect size was found for TI-MBSR on PTSD symptoms. Furthermore, at posttreatment there was a significant reduction in the proportion of participants whose PCL-C scores met the diagnostic cutoff for PTSD in the TI-MBSR group, but not in the waitlist control group. Treatment retention was also very high for TI-MBSR with 95% attending at least five of the eight sessions.
A recent trial by Polusny and colleagues (2015) investigating the efficacy of MBSR for veterans with PTSD used a rigorous experimental design (i.e. large sample, active control group, blinded assessment of outcomes, assessment of treatment fidelity, and ITT analyses). This study compared MBSR to present-centered therapy and found that both self-reported and clinician-assessed PTSD symptoms declined in both groups. However, improvement in the MBSR group was significantly greater than in the present-centered group in both self-reported and clinician-assessed PTSD, although the authors concluded that the magnitude of the average improvement was moderate. Participants in the MBSR condition were more likely than those in present-centered therapy to experience clinically significant change in self-reported PTSD at the 2-month follow-up. However, there were no significant differences between the two groups in clinician-assessed PTSD symptoms or rates of diagnostic remission. Of note, the treatment dropout at follow-up was substantially higher in the MBSR group (22.4%) than in the present-centered group (6.9%).
The eight mindfulness studies differed substantially from one another in terms of methodology. Almost all examined predominantly male veteran outpatient populations, although two studied predominantly female populations (Kelly & Garland, 2016; Kim et al., 2013a). Two (Niles et al., 2012; Polusny et al., 2015) utilized an active treatment control and the others used a waitlist or treatment-as-usual control condition. Most studies utilized rigorous ITT analyses, but two (Borman et al., 2008; Niles et al., 2013) conducted completer analyses only. All but two studies (Bormann et al., 2008; Kelly & Garland, 2016) included a follow-up assessment. The range of total treatment hours was very wide, from 3.5 hours (Niles et al., 2012) to 27 hours (Kearney et al., 2013; Polusny et al., 2015). Seven studies employed an in-person group session format whereas one (Niles et al., 2012) employed an individual telehealth format.
Six of the mindfulness studies, (all but Kearney et al., 2013; Possemato et al., 2016), indicated significant reductions in PTSD symptoms from pre- to posttreatment for the mindfulness condition when compared to the control. The between-groups effect sizes ranged from small and nonsignificant (Bormann et al., 2013: Possemato et al., 2016) to large (Bormann et al., 2008; Niles et al., 2012). Within-group effect sizes, when reported, were uniformly large, (Bormann et al., 2008; Kearney et al., 2013; Niles et al., 2012) which suggests that mindfulness can have a considerable impact on PTSD symptoms. Overall, dropouts during treatment were low, ranging from 0 (Kim et al., 2013a) to 22% (Polusny et al., 2015); however, nonattendance at the first session was high in the study conducted in a primary care setting (44.44%; Possemato et al., 2016). Four studies (Bormann et al., 2013; Kim et al., 2013a; Polusny et al., 2015; Possemato et al., 2016) reported that treatment gains were largely maintained or improved over the 6 to 8 week follow-up period; the Niles et al. (2012) study reported that PTSD symptom reductions were not maintained and suggested this may be due to the low dose of 3.5 hours of the intervention. In general, mindfulness interventions are accessible and feasible, associated with reductions in PTSD symptoms and can be delivered individually, in a group, through a telehealth format, in a primary care setting, or at a mental health clinic.
Yoga
Five studies of yoga met the inclusion criteria. An Australian study by Carter and colleagues (2103) examined an intensive yoga intervention that consisted of 22 hours of guided group yoga instruction over five days followed by nine 2-hr follow-up sessions. Completer analyses showed significant decreases in both clinician-assessed and self-reported PTSD six weeks following intervention completion, whereas the waitlist group had no decline; the between-group effect sizes were large. Furthermore, following the delayed yoga intervention, the waitlist group also improved significantly on clinician-assessed PTSD with large within-group effect sizes.
Mitchell and colleagues (2014) completed a pilot study with women using a much less intensive yoga intervention and a more active control condition. The 12-session yoga condition was compared to a 12-session assessment control condition in which the participants completed questionnaires in a group format. ITT analyses showed that there was a significant drop in self-reported PTSD symptoms over time, but that there was no significant difference between the groups indicating no advantage for yoga over group assessment. Within-group analyses indicated that PTSD symptoms decreased significantly for the yoga group. Improvements in self-reported PTSD symptoms were maintained at the 1 month follow-up assessment for both groups.
In another pilot study designed to investigate if yoga can reduce PTSD symptomology and improve overall wellness, a predominantly female (89%) group of participants were randomized to either 8 weekly sessions of Kundalini yoga or a waitlist control group (Jindani, Turner, & Khalsa, 2015). Using completer analyses, the posttreatment assessment indicated that those who received yoga had significantly greater reductions in self-reported PTSD than the waitlist control, with a small to moderate effect size. The differential dropout rate was notable as all participants in the control group completed the study while more than half (51%) dropped out of the yoga condition and did not complete the study.
Significant and lasting benefits were noted following a short period of time in a small study that examined Sudarshan Kriya yoga, a breathing-based meditation. Seppälä and colleagues (2014) provided 3-hour group sessions daily for 7 days to recently returning veterans and compared outcomes to a waitlist control. ITT analyses indicated that participants in the yoga group experienced a significant reduction in self-reported PTSD symptoms with large between-group effect sizes, with the strongest effect on the hyperarousal and reexperiencing symptoms. The symptom reductions were maintained at 1 month and 1 year follow-up.
In a large recent study, van der Kolk and colleagues (2014) compared a 10-week trauma-informed yoga intervention to a health education control group. ITT analyses indicated that both groups showed significant reductions in clinician-assessed PTSD, but the yoga group exhibited larger decreases than the control group with a moderate between-group effect size. Both groups also experienced significant decreases in self-reported PTSD symptoms mid-treatment; however, the gains were maintained in the yoga group at post-treatment whereas symptoms worsened in the control group. Within-group analyses of the yoga group indicated that the effect sizes were large for both clinician-assessed and self-reported PTSD symptom reductions. A significantly higher proportion of participants in the yoga group (53%) fell below the diagnostic cutoff for PTSD diagnosis after treatment compared to 21% in the control group.
Two of the yoga studies had only female participants (Mitchell et al., 2014; van der Kolk et al., 2014), one had a mostly female group of participants (88.8%; Jindani et al., 2015), and the other two had only male participants (Carter et al., 2013; Seppälä et al., 2014 ). Three studies employed ITT analyses (Mitchell et al., 2014; Seppälä et al., 2014; van der Kolk et al., 2014) and two used completer analyses (Carter et al., 2013; Jindani et al., 2015). Van der Kolk et al. (2014) utilized an active treatment control condition while the other four studies utilized a waitlist or assessment control condition. The total hours of treatment varied greatly across the four studies, from 10 (van der Kolk et al., 2014) to 40 hours (Carter et al., 2013). Different types of yoga were investigated in the studies; Sudarshan Kriya yoga was utilized in Carter et al. (2013) and Seppälä et al. (2014), Kripalu-based hatha yoga was used in Mitchell et al. (2014), Kundalini yoga was examined in Jindani et al. (2015), and trauma-informed hatha yoga was employed in van der Kolk et al. (2014). Four of the five yoga studies (all but Mitchell et al., 2014) found significant between-group effects ranging from moderate to large effect sizes. All reported within-group effects were large. The van der Kolk study, in particular, with a large sample size and an active comparison treatment, provides important support for yoga as an efficacious treatment for PTSD.
Relaxation
All seven of the studies identified for review in this section examined relaxation as a control comparison for other treatments under study. Therefore, this section is primarily focused on pre- to posttreatment within-group differences. We also note differences, or lack thereof, between the relaxation condition and the target treatment(s) on primary outcome measures.
Applied muscle relaxation was compared to culturally-adapted cognitive behavioral therapy for PTSD in a small study with Latino patients by (Hinton, Hofmann, Rivera, Otto, & Pollack, 2011). Large pre- to posttreatment effect sizes were reported for the participants in the relaxation condition on self-reported PTSD. The between groups effect size demonstrated a larger effect for cognitive behavioral therapy and all participants in that condition achieved clinically significant change (10 point decrease on the PCL). However, one third of the participants in the relaxation condition also achieved clinically significant change.
A study that examined relaxation in comparison to three other active treatments (prolonged exposure, cognitive restructuring, and the two combined) found large treatment effects on both self-reported and clinician-assessed PTSD for all four treatments (Marks, Lovell, Noshirvani, Livanou and Thrasher, 1998). Compared to the other treatments, however, gains were modest for the relaxation group. Fifteen percent of the participants in the relaxation condition achieved clinically significant change (<2 SDs on the CAPS) compared with 47% to 53% for the other conditions. Notably, there were no significant differences between groups on how many met PTSD diagnostic criteria at posttreatment. The authors reported completer analyses but stated that ITT analyses yielded similar outcomes.
Taylor and colleagues compared relaxation to prolonged exposure and eye movement desensitization and reprocessing (EMDR; Taylor, Thordarson, Maxfield, Fedoroff, Lovell, & Ogrodniczuk, 2003). Completer analyses indicated that all three treatments were efficacious in reducing clinician-assessed and self-reported PTSD. However, prolonged exposure showed advantage over the other treatments on some measures, such as the proportion of individuals who no longer met diagnostic criteria for PTSD and the proportion who achieved clinically significant changes in symptom clusters at posttreatment and follow-up. Of note, the dosage for relaxation therapy was less than both EMDR and exposure by a third (i.e., 8 hours versus 12 hours). Despite the differences among the treatments, the authors also note that outcomes did not significantly differ at posttreatment or follow-up and ITT analyses for self-reported PTSD indicated no significant between-group effects.
Relaxation was compared to two active treatments (eye movement desensitization and image habituation training) as well as a waitlist control in a study by Vaughan and colleagues (Vaughan, Armstrong, Gold, O’Connor, Jenneke, & Tarrier, 1994). Despite small group sizes and short treatment duration (3 to 5 sessions total), all three active treatment groups improved significantly in clinician-assessed PTSD compared with waitlist and improvements were sustained at follow-up. No differences were found among the treatment groups in, clinician-assessed PTSD, or the proportion of individuals who qualified for a PTSD diagnosis following treatment.
A study focused on heart rate variability of individuals in residential treatment for substance use also examined PTSD outcomes in an RCT comparing progressive muscle relaxation and biofeedback for respiratory sinus arrhythmia (Zucker, Samuelson, Muench, Greenberg, & Gevirtz, 2009). The interventions were used as adjunctive interventions in the treatment program. Both groups showed significant reductions in self-reported PTSD and there were no significant differences between groups.
A recent study by Carletto and colleagues (2016) compared relaxation therapy to EMDR among patients with multiple sclerosis who were diagnosed with PTSD. Within-group analyses revealed large effect sizes for both conditions on clinician-assessed and self-reported PTSD symptoms and between-groups analyses revealed no differences by treatment condition. Completer analyses indicated that 100% of participants in the EMDR condition and 77% of participants in the relaxation therapy condition no longer met criteria for a PTSD diagnosis at the six-month follow-up, a statistically significant difference.
Markowitz and colleagues (2015) used relaxation therapy as an active control in a noninferiority trial comparing interpersonal therapy to prolonged exposure for PTSD. This rigorous study used a large sample, active control group, blinded assessment of outcomes, and assessment of treatment fidelity, as well as an ITT approach to analyses. The authors employed sophisticated longitudinal mixed-effects models using multiple imputations for missing values to evaluate efficacy. Within group pre-to-post analyses of all therapies revealed large effect sizes, and between-groups analyses found no significant differences among the three conditions in posttreatment clinician-assessed PTSD symptoms or remission rates. Compared to the relaxation group, participants in the prolonged exposure and interpersonal therapy groups reported significantly greater reductions in self-reported PTSD symptoms and showed higher rates of response (defined as improvement of > 30% on CAPS). Nevertheless, the improvements seen in the relaxation group were substantial and there were no differences among the groups on many of the reported outcomes.
All seven of the relaxation studies focused primarily on the efficacy of the target interventions in the RCTs and in general provided limited detail about the procedures and results for the relaxation condition. There was substantial variability regarding the session length (20 to 90 minutes), frequency of the sessions (daily to weekly), and duration of the intervention (2 to 15 weeks). Importantly, the within-group effects that were the focus of the current review were not uniformly reported and were based on small group sizes. Five of the studies had a participant pool that was predominantly or all female (64% to 100%), while both Marks et al. (1998) and Zucker et al. (2009), included more male participants (64% and 55%, respectively). Four of the studies used ITT analyses (Carletto, et al., 2016; Hinton, et al., 2011; Markowitz, et al., 2015; Vaughn et al., 1994), while the remaining used completer analyses (Marks et al., 1998; Taylor et al., 2003; Zucker et al., 2009).
In four studies (Hinton, et al. 2011; Markowitz et al., 2015; Marks et al., 1998; and Taylor et al., 2003) large pre to post within-group effect sizes for relaxation were reported indicating that the relaxation treatment had a salutary effect on PTSD symptoms. The remaining three studies (Carletto et al., 2016; Vaughan et al., 1994; Zucker et al., 2009) did not report within-group effect sizes but both reported reduced PTSD severity for all treatment conditions. In the majority of studies, no significant between-group differences were detected in the primary condition-by-time analyses, indicating that outcomes for relaxation were comparable with the other treatments; however, two of the studies (Hinton, et al. 2011; Marks et al., 1998) reported greater treatment efficacy for the target treatments than relaxation on the primary PTSD outcome measures.
DISCUSSION
The evidence provided by the mindfulness, yoga, and relaxation studies reviewed here offers support for mind-body treatments for PTSD. However, the literature base remains limited because many of the trials suffer from methodologic weaknesses (small numbers of participants, lack of active control groups, and un-blinded assessments). It is encouraging that some recent RCTs have addressed many of these problems and some rigorous studies have been added to the nascent evidence base. A prime example is the large-scale trial by Polusny and colleagues (2015) that demonstrates superior outcomes for mindfulness compared to present-centered therapy (PCT), currently considered to be an empirically supported treatment for PTSD by Division 12 of the American Psychological Association (APA, 2013). Similarly the van der Kolk (2014) study provides important support for yoga as an efficacious treatment for PTSD. Given the large within-group effect sizes and the non-significant between-group differences on the main PTSD outcomes in most of the relaxation studies, this review suggests that stand-alone relaxation may be a valuable treatment option for PTSD. The absence of RCTs examining tai chi for PTSD suggests that this may be a fruitful avenue for future research.
This is the first systematic review limited to published RCTs examining active mind-body treatments for PTSD; previous reviews have included single-arm and case studies. In addition, stand-alone relaxation strategies for PTSD have not been included in previous reviews of mind-body treatments, presumably because relaxation has been examined in RCTs only as a comparison or control treatment. The current review reveals the frequent absence of differences in PTSD outcomes between relaxation and the RCT target treatments and highlights the within-group symptom improvements. A strength of this review is that we included a wide variety of interventions within each of the three categories of treatment (e.g. mindfulness included MBSR, mantram repetition, and brief mindfulness interventions). However, this approach made it difficult to succinctly summarize the findings as a whole.
This review has several important limitations. Our focus was strictly on PTSD outcomes so we did not examine other potential benefits, such as improvements in quality of life or physical functioning that have been associated with these interventions in other populations. Additionally, the small number of participants in many of these trials may contribute to an overestimation of the findings as smaller trials tend to be analyzed with less methodological rigor (Coronado-Montoya et al., 2016). Our findings also may be influenced by publication bias because small trials that did not show PTSD symptom improvement may not have been published. Moreover, the applicability of this review may be limited by the specific populations under study (e.g. 6 of the 8 mindfulness studies were done with veterans) and the interventions could perform differently in other populations. Finally, our restriction to English-language publications may have excluded important studies that were published in other languages.
We encourage PTSD mind-body researchers to consider the following recommendations for future research: (1) calculate and report both between-group and within-group effect sizes in order to compare effect sizes across studies; (2) provide detailed descriptions of the interventions to allow researchers and clinicians to replicate them; (3) consider the impact of dose and, when possible, compare different doses of treatment; (4) include follow-up assessments and consider methods to encourage sustained practice of the therapy following the end of treatment; (5) examine how mind-body treatments might be used in conjunction with current evidence-based trauma-focused treatments for PTSD; and (6) investigate the efficacy of tai chi for PTSD. In addition, choice of comparison groups in RCTs is a study design element that deserves careful consideration as there are advantages and drawbacks associated with all comparison groups. Unlike medication trials, there is no true placebo in mind-body or psychotherapy RCTs (Schnurr, 2007) and, as we found was the case with relaxation, control interventions sometimes prove to be efficacious.
The active mind-body treatments reviewed here can be offered easily in venues that are not associated with the stigma of mental health care, such as at primary care practices and community settings. Mind-body interventions may encourage tolerance of distressing physical and emotional states for individuals with PTSD and promote approach-oriented coping that can empower individuals to engage in healthy lifestyle habits. Furthermore, these interventions may reduce persistent hyperarousal symptoms that perpetuate physical and psychological dysregulation and thus initiate a positive cycle of enhanced health. These mind-body approaches may serve as appealing supplements or alternatives to current evidence-based treatments.
Acknowledgments
This study was supported by the Veterans Administration Clinical Science Research and Development (SPLD-004–15S, Drs. Niles and Mori) and the National Center for Complementary and Integrative Health (NCCIH; K24AT007323, Dr. Wang). The investigators are solely responsible for the contents of the manuscript and they do not represent official views of the U.S. Department of Veterans Affairs, the NCCIH, or the United States Government.
Contributor Information
Barbara L. Niles, National Center for PTSD – Behavioral Science Division, VA Boston Healthcare System and Boston University School of Medicine
DeAnna L. Mori, VA Boston Healthcare System and Boston University School of Medicine
Craig Polizzi, National Center for PTSD – Behavioral Science Division, VA Boston Healthcare System.
Anica Pless Kaiser, National Center for PTSD – Behavioral Science Division, VA Boston Healthcare System and Boston University School of Medicine.
Elizabeth S. Weinstein, National Center for PTSD – Behavioral Science Division, VA Boston Healthcare System
Marina Gershkovich, VA Boston Healthcare System.
Chenchen Wang, Center For Complementary And Integrative Medicine, Division of Rheumatology, Tufts Medical Center, Tufts University, School of Medicine.
REFERENCES
- American Psychological Association (2013). Present-Centered Therapy for Post-Traumatic Stress Disorder. Retrieved from http://www.div12.org/PsychologicalTreatments/treatments/ptsd_present.html
- Baer RA (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–143. DOI: 10.1093/clipsy.bpg015 [DOI] [Google Scholar]
- Banks K, Newman E, & Saleem J (2015). An Overview of the Research on Mindfulness‐Based Interventions for Treating Symptoms of Posttraumatic Stress Disorder: A Systematic Review. Journal of clinical psychology, 71(10), 935–963 [DOI] [PubMed] [Google Scholar]
- Barnes PM, Bloom B, & Nahin RL (2008). Complementary and alternative medicine use among adults and children: United States, 2007 National Health Statistics Reports; no 12 Hyattsville, MD: National Center for Health Statistics; [PubMed] [Google Scholar]
- Bormann JE, Thorp S, Wetherell JL, & Golshan S (2008). A spiritually based group intervention for combat veterans with posttraumatic stress disorder: Feasibility study. Journal of Holistic Nursing, 26, 109–116. DOI: 10.1177/0898010107311276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bormann JE, Thorp SR, Wetherell JL, Golshan S, & Lang AJ (2013). Meditation-based mantram intervention for veterans with posttraumatic stress disorder: A randomized trial. Psychological Trauma: Theory, Research, Practice, and Policy, 5(3), 259–267. DOI: 10.1037/a0027522 [DOI] [Google Scholar]
- Bystritsky A, Hovav S, Sherbourne C, Stein MB, Rose RD, Campbell-Sills L, … &Roy-Byrne PP (2012). Use of complementary and alternative medicine in a large sample of anxiety patients. Psychosomatics, 53(3), 266–272. DOI: 10.1016/j.psym.2011.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carletto S, Borghi M, Bertino G, Oliva F, Cavallo M, Hofmann A, … & Ostacoli L (2016). Treating Post-traumatic Stress Disorder in Patients with Multiple Sclerosis: A Randomized Controlled Trial Comparing the Efficacy of Eye Movement Desensitization and Reprocessing and Relaxation Therapy. Frontiers in Psychology, 7 10.3389/fpsyg.2016.00526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter J, Gerbarg PL, Brown RP, Ware RS, D’Ambrosio C, Anand L, … & Katzman MA 2013). Multi-component yoga breath program for Vietnam veteran post traumatic stress disorder: Randomized controlled trial. Journal of Traumatic Stress Disorders and Treatment, 2(3). Retrieved from http://scitechnol.com/multicomponent-yoga-breath-program-for-vietnam-veteran-post-traumatic-stress-disorder-randomizedcontrolled-trial-OPd.php?article_id=1364 DOI: 10.4172/2324-8947.1000108 [DOI] [Google Scholar]
- Cohen J (1988). Statistical power analysis of the behavioral sciences. (2nd ed.). New York, NY: Academic Press. [Google Scholar]
- Coronado-Montoya S, Levis AW, Kwakkenbos L, Steele RJ, Turner EH, & Thombs BD (2016). Reporting of Positive Results in Randomized Controlled Trials of Mindfulness-Based Mental Health Interventions. PloS one, 11(4), e0153220. doi: 10.1371/journal.pone.0153220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MT, Mulvaney-Day N, Larson MJ, Hoover R, & Mauch D (2014). Complementary and alternative medicine among veterans and military personnel: A synthesis of population surveys. Medical care, 52, S83–S90. DOI: 10.1097/MLR.0000000000000227 [DOI] [PubMed] [Google Scholar]
- Elwy AR, Johnston JM, Bormann JE, Hull A, & Taylor SL (2014). A systematic scoping review of complementary and alternative medicine mind and body practices to improve the health of veterans and military personnel. Medical Care, 52, S70–S82. DOI: 10.1097/MLR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- Engelhard IM, van den Hout MA, Weerts J, Hox JJ, & van Doornen LJ (2009). A prospective study of the relation between posttraumatic stress and physical health symptoms. International Journal of Clinical and Health Psychology, 9(3), 365–372. Retrieved from http://www.redalyc.org/articulo.oa?id=33712038001 [Google Scholar]
- Foa EB, & Rothbaum BO (2001). Treating the trauma of rape: Cognitive-behavioraltherapy for PTSD. New York, NY: Guilford Press. [Google Scholar]
- Follette VM, & Vijay A (2009). Mindfulness for trauma and posttraumatic stress disorder In Didonna F (Ed.), Clinical handbook of mindfulness (pp. 299–317). New York, NY: Springer; DOI: 10.1007/978-0-387-09593-6_17 [DOI] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, & Walach H (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. DOI: 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- Hilton L, Maher AR, Colaiaco B, Apaydin E, Sorbero ME, Booth M, Shanman RM, & Hempel S (2016, August 18). Meditation for Posttraumatic Stress: Systematic Review and Meta-analysis. Psychological Trauma: Theory, Research, Practice, and Policy. Advance online publication. 10.1037/tra0000180 [DOI] [PubMed] [Google Scholar]
- Hinton DE, Hofmann SG, Rivera E, Otto MW, & Pollack MH (2011). Culturally adapted CBT (CA-CBT) for Latino women with treatment-resistant PTSD: A pilot study comparing CA-CBT to applied muscle relaxation. Behaviour Research and Therapy, 49(4), 275–280. DOI: 10.1016/j.brat.2011.01.005 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2012). Treatment for posttraumatic stress disorder in military and veteran populations: Initial assessment. Washington, DC: National Academy of Sciences. [PubMed] [Google Scholar]
- Jin P (1989). Changes in heart rate, noradrenaline, cortisol and mood during Tai Chi. Journal of Psychosomatic Research, 33(2), 197–206. DOI: 10.1016/0022-3999(89)90047-0 [DOI] [PubMed] [Google Scholar]
- Jindani F, Turner N, & Khalsa SBS (2015). A Yoga Intervention for Posttraumatic Stress: A Preliminary Randomized Control Trial. Evidence-Based Complementary and Alternative Medicine : eCAM, 2015, 351746 10.1155/2015/351746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion. [Google Scholar]
- Kabat-Zinn J & Hanh TN (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Random House LLC. [Google Scholar]
- Kearney DJ, McDermott K, Malte C, Martinez M, & Simpson TL (2013). Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: A randomized controlled pilot study. Journal of Clinical Psychology, 69(1), 14–27. DOI: 10.1002/jclp.21911 [DOI] [PubMed] [Google Scholar]
- Kelly A & Garland EL (2016). Trauma-Informed Mindfulness-Based Stress Reduction for Female Survivors of Interpersonal Violence: Results From a Stage I RCT. Journal of Clinical Psychology, 72(4), 311–328. DOI: 10.1002/jclp.22273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. DOI: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khusid Marina A MD,N.D., M.S.A., & Vythilingam M M.D. (2016). The emerging role of mindfulness meditation as effective self-management strategy, part 1: Clinical implications for depression, post-traumatic stress disorder, and anxiety. Military Medicine, 181(9), 961–968. doi: 10.7205/MILMED-D-14-00677 [DOI] [PubMed] [Google Scholar]
- Kim SH, Schneider SM, Bevans M, Kravitz L, Mermier C, Qualls C, & Burge MR (2013a). PTSD symptom reduction with mindfulness-based stretching and deep breathing exercise: Randomized controlled clinical trial of efficacy. The Journal of Clinical Endocrinology & Metabolism, 98(7), 2984–2992. DOI: 10.1210/jc.2012-3742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Schneider SM, Kravitz L, Mermier C, & Burge MR (2013b). Mind-body practices for posttraumatic stress disorder. Journal of Investigative Medicine: The Official Publication of the American Federation for Clinical Research, 61(5), 827–834. DOI: 10.231/JIM.0b013e3182906862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby DJ, Pilver CE, & Desai R (2012). Complementary and alternative medicine in VA specialized PTSD treatment programs. Psychiatric Services, 63(11), 1134–1136. DOI: 10.1176/appi.ps.201100456 [DOI] [PubMed] [Google Scholar]
- Libby DJ, Pilver CE, & Desai R (2013). Complementary and alternative medicine use among individuals with posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 5(3), 277–285. DOI: 10.1037/a0027082 [DOI] [Google Scholar]
- Libby DJ, Reddy F, Pilver CE, & Desai RA (2012). The use of yoga in specialized VA PTSD treatment programs. International Journal of Yoga Therapy, 22(1), 79–88. [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, … & Moher D (2009). The PRISMA statement for reporting systematic reviews and meta- analyses of studies that evaluate health care interventions: Explanation and elaboration. Annals of Internal Medicine, 151(4), W-65-W-94. DOI: 10.7326/0003-4819-151-4-200908180-00136 [DOI] [PubMed] [Google Scholar]
- Marks I, Lovell K, Noshirvani H, Livanou M, & Thrasher S (1998). Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: A controlled study. Archives of General Psychiatry, 55(4), 317–325. DOI: 10.1001/archpsyc.55.4.317 [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Petkova E, Neria Y, Van Meter PE, Zhao Y, Hembree E, … & Marshall RD (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry, 172(5), 430–440. 10.1176/appi.ajp.2014.14070908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meichenbaum D (1975). Self-instructional methods In Kanfer FH & Goldstein AP (Eds.), Helping people change (pp. 357–391). Elmsford, NY: Pergamon Press. [Google Scholar]
- Mitchell KS, Dick AM, DiMartino DM, Smith BN, Niles B, Koenen KC, & Street A (2014). A pilot study of a randomized controlled trial of yoga as an intervention for PTSD symptoms in women. Journal of Traumatic Stress, 27(2), 121–128. DOI: 10.1002/jts.21903 [DOI] [PubMed] [Google Scholar]
- Moore M, Brown D, Money N, & Bates M (2011). Mind-body skills for regulating the autonomic nervous system. Arlington, VA: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury. [Google Scholar]
- National Center for Complementary and Integrative Health. (2015, March). Complementary, Alternative, or Integrative Health: What’s In a Name?. Retrieved from https://nccih.nih.gov/health/integrative-health.
- National Center for Complementary and Integrative Health (May, 2016). Relaxation Techniques for Health. Retrieved from https://nccih.nih.gov/health/stress/relaxation.htm
- National Center for Complementary and Integrative Health (August, 2015). Tai Chi and Qi Gong: In Depth. Retrieved from https://nccih.nih.gov/health/taichi/introduction.htm
- National Center for Complementary and Integrative Health (June, 2013). Yoga: In Depth. Retrieved from https://nccih.nih.gov/health/yoga/introduction.htm
- Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, & Wolf EJ (2012). Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 538–547. doi: 10.1037/a0026161 [DOI] [Google Scholar]
- Orsillo SM, & Batten SV (2005). Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behavior Modification, 29(1), 95–129. DOI: 10.1177/0145445504270876 [DOI] [PubMed] [Google Scholar]
- Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, … & Lim KO (2015). Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA, 314(5), 456–465. doi: 10.1001/jama.2015.8361 [DOI] [PubMed] [Google Scholar]
- Possemato K, Wade M, Andersen J, & Ouimette P (2010). The impact of PTSD, depression, and substance use disorders on disease burden and health care utilization among OEF/OIF veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 2(3), 218–223. 10.1037/a0019236 [DOI] [Google Scholar]
- Possemato K, Bergen‐Cico D, Treatman S, Allen C, Wade M, & Pigeon W (2016). A Randomized Clinical Trial of Primary Care Brief Mindfulness Training for Veterans With PTSD. Journal of Clinical Psychology, 72(3), 179–193. DOI: 10.1002/jclp.22241 [DOI] [PubMed] [Google Scholar]
- Raman G, Zhang Y, Minichiello VJ, D’Ambrosio C, & Wang C (2013). Tai Chi improves sleep quality in healthy adults and patients with chronic conditions: A systematic review and meta-analysis. Journal of Sleep Disorders Therapy, 2(141). Retrieved from http://omicsgroup.org/journals/tai-chi-improves-sleep-quality-in-healthy-adults-and-patients-with-chronic-conditions-a-systematic-review-and-metaanalysis-2167-0277-2-141.pdf. DOI: 10.4172/2167-0277.1000141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell TL, & Marshall GN (2008). Survey of individuals previously deployed for OEF/OIF In T. T and Jaycox LH (Eds.), Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery (pp. 87–115). Santa Monica, CA: RAND Center for Military Health Policy Research. [Google Scholar]
- Schell TL, Marshall GN, & Jaycox LH (2004). All symptoms are not created equal: the prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology, 113(2), 189–197. 10.1037/0021-843X.113.2.189 [DOI] [PubMed] [Google Scholar]
- Schnurr PP (2007). The rocks and hard places in psychotherapy outcome research. Journal of Traumatic Stress, 20, 779–792. DOI: 10.1002/jts.20292 [DOI] [PubMed] [Google Scholar]
- Seppälä EM, Nitschke JB, Tudorascu DL, Hayes A, Goldstein MR, Nguyen DT, … & Davidson RJ (2014). Breathing‐based meditation decreases posttraumatic stress disorder symptoms in US military veterans: A randomized controlled longitudinal study. Journal of Traumatic Stress, 27(4), 397–405. DOI: 10.1002/jts.21936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss JL & Lang AJ (2012). Complementary and Alternative Treatments for PTSD. PTSD Research Quarterly, 23(2), 1–7. [Google Scholar]
- Stecker T, Fortney J, Owen R, McGovern MP, & Williams S (2010). Co-occurring medical, psychiatric, and alcohol-related disorders among veterans returning from Iraq and Afghanistan. Psychosomatics, 51(6), 503–507. https://search.proquest.com/docview/805137181?accountid=30093 [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, & Marmar CR (2015). Psychotherapy for military-related PTSD: A review of randomized clinical trials. JAMA, 314(5), 489–500. doi: 10.1001/jama.2015.8370 [DOI] [PubMed] [Google Scholar]
- Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, & Ogrodniczuk J (2003). Comparative efficacy, speed, and adverse effects of three PTSD treatments: Exposure therapy, EMDR, and relaxation training. Journal of Consulting and Clinical Psychology, 71(2), 330–338. DOI: 10.1037/0022-006X.71.2.330 [DOI] [PubMed] [Google Scholar]
- VA Healthcare Analysis and Information Group (2011). 2011 complementary and alternative medicine. Washington, DC: Department of Veterans Affairs. [Google Scholar]
- van der Kolk B, Stone L, West J, Rhodes A, Emerson D, Suvak M, & Spinazzola J (2014). Yoga as an adjunctive treatment for posttraumatic stress disorder: A randomized controlled trial. Journal of Clinical Psychiatry, 75(6), 559–565. DOI: 10.4088/JCP.13m08651 [DOI] [PubMed] [Google Scholar]
- Vaughan K, Armstrong MS, Gold R, O’Connor N, Jenneke W, & Tarrier N (1994). A trial of eye movement desensitization compared to image habituation training and applied muscle relaxation in post-traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry, 25(4), 283–291. DOI: 10.1016/0005-7916(94)90036-1 [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Youngwirth NE, Johnson KA, & Zvolensky MJ (2009). Mindfulness-based acceptance and posttraumatic stress symptoms among trauma-exposed adults without axis I psychopathology. Journal of Anxiety Disorders, 23(2), 297–303. DOI: 10.1016/j.janxdis.2008.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahbeh H, Senders A, Neuendorf R, & Cayton J (2014). Complementary and alternative medicine for posttraumatic stress disorder symptoms: A systematic review. Journal of Evidence-based Complementary & Alternative Medicine, 19(3), 161–175. DOI: 10.1177/2156587214525403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walser R, & Westrup D (2007). Acceptance and commitment therapy for the treatment of post-traumatic stress disorder and trauma-related problems: A practitioner’s guide to using mindfulness and acceptance strategies. Oakland, CA: New Harbinger Publications. [Google Scholar]
- Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, & Schmid CH (2010). Tai Chi on psychological well-being: Systematic review and meta-analysis. BMC Complementary and Alternative Medicine, 10(23). Retrieved from http://www.biomedcentral.com/1472-6882/10/23. DOI: 10.1186/1472-6882-10-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Collet JP, & Lau J (2004). The effect of Tai Chi on health outcomes in patients with chronic conditions: A systematic review. Archives of Internal Medicine, 164(5), 493–501. DOI: 10.1001/archinte.164.5.493 [DOI] [PubMed] [Google Scholar]
- Wei D, Coeytaux RR, McDuffie JR, Goode AP, Sharma P, Mennella H, & … Williams JW Jr. (2016). Evidence Map of Yoga for Depression, Anxiety, and Posttraumatic Stress Disorder. Journal Of Physical Activity & Health, 13(3), 281–288. doi: 10.1123/jpah.2015-0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Logue MW, Hayes JP, Sadeh N, Schichman SA, Stone A, … & Miller MW (2016). Accelerated DNA methylation age: Associations with PTSD and neural integrity. Psychoneuroendocrinology, 63, 155–162. DOI: 10.1016/j.psyneuen.2015.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker TL, Samuelson KW, Muench F, Greenberg MA, & Gevirtz RN (2009). The effects of respiratory sinus arrhythmia biofeedback on heart rate variability and posttraumatic stress disorder symptoms: A pilot study. Applied Psychophysiology and Biofeedback, 34(2), 135–143. DOI: 10.1007/s10484-009-9085 [DOI] [PubMed] [Google Scholar]