Abstract
Introduction
The current Learning Health Systems literature affords insufficient attention to the process of learning. In response, Billings Clinic focused on how to advance its learning capabilities and subsequently to contribute new insights into the process of learning to the LHS literature.
Methods
An environmental scan was conducted, including the grey literature (eg, technical reports and white papers) and peer‐reviewed research publications. Semistructured interviews were also conducted with Clinic staff members to determine the motivation of their engagement in meaningful quality improvement, or learning, initiatives.
Results
Six learning principles emerged from the literature review and staff interviews: (1) draw on wisdom of groups and value connections; (2) embrace sensemaking over decision making in dealing with the unexpected; (3) bring diverse perspectives to complex challenges; (4) animate people, provide direction, update regularly, and interact respectfully; (5) appreciate the power and ubiquity of emergent change and the limitations of planned change; and (6) concentrate on small wins and characterize challenges as mere problems. Examples of how these principles are beginning to influence how learning and improvement are understood and approached at Billings Clinic are described and serve as illustrations of the principles in action.
Conclusion
Becoming adept in learning is essential to realizing the vision of Learning Health Systems—to harness science, clinical research, and information generated by digital technology to inform and accelerate improvement in quality health care. This article seeks to contribute to greater understanding of this process by sharing a set of principles that are proving useful at one health care organization and to a more comprehensive conceptualization of Learning Health Systems.
Keywords: complexity science, learning, learning health systems, quality improvement, self‐determination theory, sensemaking
1. INTRODUCTION
A group of rural primary care professionals in New Mexico cures patients with hepatitis C virus at rates as good as or sometimes better than those of leading specialists at an academic medical center.1 Their patients also experience a lower rate of serious adverse events. We believe we know why. Built into the architecture of Project ECHO, the program that produced these results, are principles of learning. Project ECHO answers the call by a growing chorus of visionaries to improve learning in health care.
The development of Learning Health Systems (LHSs) is advocated by the Institute of Medicine as a way to “produce high‐quality healthcare that continuously learns to be better” and reduce the cost of excellent care.2 (pix) A Learning Health System is defined as one “in which progress in science, informatics, and care culture align to generate new knowledge as an ongoing, natural by‐product of the care experience, and seamlessly refine and deliver best practices for continuous improvement in health and healthcare.”3 To this, Etheredge adds an emphasis on speed and timeliness of learning around treatment planning for patients.4
Information technology infrastructure needed to capture, analyze, and disseminate data, and information is the focus of the current LHS literature. Leading scholars highlight the importance of learning from data and new knowledge, and accelerating knowledge generation.2, 4, 5, 6, 7, 8, 9 Krumholz observes that “important lessons on how to leverage massive amounts of data, and for learning from such data” will emerge from efficacious LHSs.9 (p47)
Despite acknowledging the importance of learning, there is insufficient attention in the LHS literature to the process of learning and how learning can be cultivated. For purposes of this article, we use the definition of learning in The American Heritage Dictionary—“the act, process, or experience of gaining knowledge or skill” .10(p.1025)
Missing from the Institute of Medicine's list of LHS characteristics—culture, design and processes, patients and public, decisions, care, outcomes and costs, knowledge, digital technology, and health information—are any that deal directly with the process of learning.7 Similarly, the 9 components of a learning health system articulated by Psek do not explicitly address learning processes.11
Etheredge identifies 4 essential opportunities for a Learning Health System agenda: clinical research and development, comparative effectiveness research, health information technology, and improving patient care.4 While these opportunities guide development of new information infrastructure and tools to advance clinical care, they do not address how health care professionals learn to apply the information generated through research and technology to achieve better care.
Friedman and colleagues describe the benefits of sharing data, speeding the creation and validation of new biomedical knowledge, and translating knowledge into practice.5 The implicit assumption in this body of work is that feeding “the knowledge of ‘what works best’ back to clinicians, public health professionals, patients, and other stakeholders”5 (p44) will result in learning and change. Reference in this article to sociotechnical challenges and cyber‐physical‐social system suggests that learning and change are complex social processes that can be informed by information systems. Group Health Cooperative (GHC) has developed an approach that deals with the technical and social challenges of learning, articulated in 6 phases of learning: (1) scanning and surveillance, (2) design, (3) implementation, (4) evaluation, (5) adjustment, and (6) dissemination.6
This overview can lead one to the conclusion that fulfillment of the LHS vision would benefit from greater attention to the social, and complex, processes of learning in health care organizations.
2. LHS EXPLORATIONS AT BILLINGS CLINIC
Interest in Learning Health Systems at Billings Clinic, an integrated health care delivery system in Montana, emerged as a multidisciplinary group of clinicians and leaders studied complexity science and the implications it held for health care improvement.12 They learned that complexity science scholars view learning as a self‐organizing process shaped by the interactions within a system, dependent on the diversity of perspectives, the network of individuals involved, and the characteristics of relationships and the flow of information within the network.13, 14, 15, 16, 17 As the term suggests, self‐organization means that in systems with many elements outcomes cannot be controlled or engineered since they are determined by the multiple actions and interactions among the agents comprising the system.
Armed with these new perspectives on learning and stimulated by the literature on Learning Health Systems, these staff members formed a Learning Health System Network, dedicated to advancing LHS capabilities for the benefit of improved patient care and organizational performance. Among its members were the Clinic's chief medical officer—hospital, director of medical‐surgical nursing, chief medical information officer, an occupational therapist, an advanced practice nurse, chair of psychiatry, nursing administrative officer, a research analyst, and director of the partnership for complex systems and health care innovation.
This practically oriented group, as a result of its examination of the LHS literature and its familiarity with the complexity science literature and its emphasis learning as a process, concluded that a more comprehensive conceptualization of Learning Health Systems should include greater attention to the process of learning. To address this, members undertook a broad search of the literature on organizational learning, behavior change, and improvement. This search led them to appreciate the relevance of the scholarship of Weick on the social psychology of organizations,18, 19, 20 of Ryan and Deci human development and self‐determination theory,21 and McDaniel and colleagues on complexity science and health care management.15, 22
During this search, the group noticed that many of the principles they were discovering from the literature were supported by findings from a past Clinic initiative to understand what motivated and supported staff engagement in quality improvement. This 2013 project, the results of which have not been previously published, entailed semistructured interviews with a purposive sample of 127 staff members (30 physicians; 29 nurses; 16 managers and executives; 3 human resource and organizational development professionals; 14 quality, safety, risk, and improvement experts; and 35 staff members from other departments such as finance, dietary, research, information services, and laboratory services). Members of a multidisciplinary task force on staff participation in quality improvement conducted the interviews using an interview guide. (Examples of questions used in the interviews are shown in Table 1) Task force members also worked collaboratively to draw out key findings and illustrative quotations from the interview data.
Table 1.
Sample questions used in staff interviews
| Sample Questions from Semistructured Interview Guide |
| ■ What quality efforts have you been engaged in that make you feel most proud? Why? |
| ■ In your time at Billings Clinic, when did you feel most engaged in quality work? What made this possible? |
| ■ Whom do you most admire for how they engage with colleagues in quality work? What do they do? |
3. LEARNING PRINCIPLES
Considered together—findings from the literature and the interviews—the LHS Network members derived a set of 6 principles to guide effective learning. Consonance between the literature and the interview findings bolstered confidence among LHS Network members in the 6 principles and their suitability for use in the organization.
The 6 principles are shown in Exhibit 1 and discussed below with appropriate references to Weick, McDaniel, Ryan, Deci, GHC learning phases, and insights from the interview findings.
Exhibit 1.
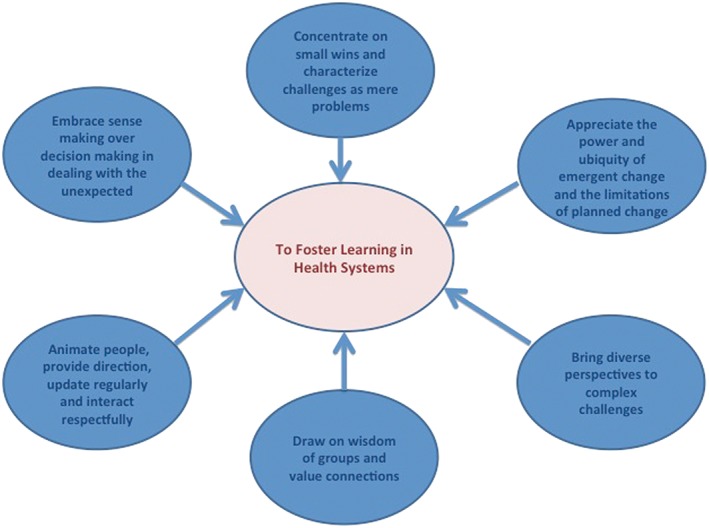
Six proposed learning principles
3.1. Draw on wisdom of groups and value connections
Weick, in his scholarship on sensemaking, contends that groups composed of individuals with diverse perspectives can, through interaction, build an understanding of a complex issue that is more complete and capable of informing wise action than any individual in the group.18 He writes, “Out of interconnections, there emerges a representation of the world that none of those involved individually possessed or could possess.”18 (p53) The design phase at GHC also stresses the benefit of engaging key stakeholders who work together in groups to tackle complex challenges.
In the Billings Clinic staff interviews, participants were asked to identify quality improvement efforts that made them most proud. Respondents highlighted experiences with teams composed of professionals from multiple disciplines that made a difference in how they understood and addressed patient safety issues, such as infection prevention, obstructive sleep apnea, hypertension, and sepsis. One physician stated, “Teams have more wisdom than one person, they open out a bigger environment of possibilities.”
3.2. Embrace sensemaking over decision making in dealing with the unexpected
Issues that are unexpected, including errors, represent opportunities to learn. McDaniel asserts that many health care professionals regard surprise negatively, as a mistake or failure, rather than an opportunity for critical examination that can inform subsequent action. He writes, “instead of asking ‘How can I keep this from happening?’ one should ask ‘Can I make use of what is happening?’”23 (p275)
Weick maintains sensemaking is especially critical in health care because the environment is “often unknowable and unpredictable”.29 (p165) To cope with such environments, he argues for sensemaking rather than decision making, for cultivation of ambivalence rather than rationality. The value of such an approach is captured in Weick's favorite quote from Paul Gleason, a renowned wildland firefighting commander:
“If I make a decision, I take pride in it, I tend to defend it and not listen to those who question it. If I make sense, then this is more dynamic and I listen and I can change it. A decision is something you polish. Sensemaking is a direction for the next period.”18 (p58)
A sensemaking orientation comes through in the GHC evaluation and dissemination phases. Timely feedback that “can guide subsequent actions” is advocated in the evaluation phase6 (p209); the dissemination phase emphasizes the importance of open conversations among staff about evaluation findings.
A sensemaking orientation also appears in interview responses to the questions: Whom do you most admire for how they engage with colleagues in quality and improvement work? What do they do? Staff named colleagues who valued participation by others, listened well, treated others with respect, fostered dialogue in teams, and brought people together to make sense of an issue and chart a way forward.
3.3. Bring diverse perspectives to complex challenges
Weick extends his development of sensemaking by drawing on Ashby's law of requisite variety. Ashby argued that to tackle a complex challenge, organizations must draw on diverse perspectives to generate a reasonable understanding of the issue and a wide repertoire of actions to respond to the challenge.24 Uncovering diverse perspectives and creating action possibilities depend on respectful interactions within groups.29 Weick observes that in systems characterized by large power differentials, such as health care organizations, efforts to reduce these differentials are beneficial because they increase access to variety and reduce the tendency of those in power to “define reality.” Weick places more value on insights from those closest to the action than those in positions of power as those closest often identify problems earlier. Being attentive to their concerns effectively increases requisite variety.
The interview data contain evidence for the value of diverse perspectives and respectful interaction. A nursing leader commented how proud she felt to be part of the effort to reduce sepsis, “because it was a multidisciplinary team that was highly functional, engaged, and demonstrated mutual respect.”
3.4. Animate people, provide direction, update regularly and interact respectfully
Weick, in “Emergent Change as a Universal in Organizations,” examined factors common to meaningful change efforts Weick noted that effectiveness of such efforts varies depending on how well groups use, facilitate, or block 4 essential components of sensemaking.20 (p236) These are:
Animate people to confront issues they care about;
Provide direction to organize action and learning;
Encourage updating, meaning ongoing attention to what is happening, and
Feature respectful interaction.
The scholarship of Ryan and Deci on self‐determination theory delves into factors that contribute to social development.21 They point out “Perhaps no single phenomenon reflects the positive potential of human nature as much as intrinsic motivation, the inherent tendency to seek out novelty and challenges, to extend and exercise one's capacities, to explore, and to learn.”21 (p70) They contend that people are endowed with these tendencies, but that they require supportive conditions to be sustained. Several of the conditions that support intrinsic motivation align with Weick's factors for successful change. Autonomy—“choice, acknowledgment of feelings, and opportunities for self‐direction”21 (p70)—relates to Weick's principle of animating people. To be truly animated, individuals must have the freedom to embrace an issue important to them. Self‐determination theory suggests intrinsic motivation is enhanced when individuals are in environments characterized by security and relatedness. Such conditions are congruent with Weick's insight that successful change is a consequence of respectful interaction. Together, these observations suggest that health care leaders and policy makers temper their reliance on external motivation and create opportunities to tap the power of intrinsic motivation.
Greene's presentation of the design phase of GHC's rapid‐learning health systems highlights the value of gathering committed groups together to achieve improvements. Such commitment emerges from animated people. Weick's updating principle relates directly to GHC's evaluation phase, where timely feedback is provided to guide future implementation activities.
The concepts of relatedness, respectful interaction, direction, and autonomy are referenced in the interviews. When staff members were asked when they felt most engaged in improvement and what conditions made this possible, they mentioned working collaboratively with others (relatedness and respectful interaction) and being guided by clarity of purpose (direction) to address something important to the well‐being of patients (animation). A nurse recollected an effort to reduce infections associated with medical devices (direction):
“All departments from outpatient to hospital surgery and infection control wanted to help and worked together well. Open and positive lines of communication. I met a diverse group of people through the process and really enjoyed the physician commitment and their engagement…It was all about the patient.”
Other participants commented on the significance of ownership (autonomy) of problems by the staff. One physician leader remarked on efforts to improve care of patients with sleep apnea and reduce surgical site infections. Groups leading these efforts have “taken ownership of the challenges.”
3.5. Appreciate the power and ubiquity of emergent change and the limitations of planned change
Weick posits the significance of planned, top leadership‐led change is grossly overrated and the power of ongoing experimentation and adaptation by workers at the frontline is grossly underrated.20
“We are in thrall of the story of dramatic change interventions in which heroic figures turn around stubbornly inertial structures held in place by rigid people who are slow learners. This is a riveting story. It is also a deceptive story. It runs roughshod over capabilities that are already in place, over the basics of change, and over changes that are already underway”.28 (p238)
Weick also observes that emergent change, the small‐scale, frontline staff‐led process of sensemaking can, over time, lead to significant change that lasts. Because such local change efforts are going on constantly, they can be material sources of learning and improvement.
The value of frontline‐led change comes across in the interviews. Staff attributed improvement in MRSA infection rates, surgical care of patients with sleep apnea, prevention of venous thromboembolism, and emergency department‐hospitalist‐ICU communication to frontline leadership.
3.6. Concentrate on small wins and characterize challenges as mere problems
Weick asserts that how we describe and label problems impacts our ability to tackle them.19 Problems labeled “massive” tend to overwhelm the ability of individuals to cope. Fear is aroused because people believe the problem is beyond their abilities. People may also lack sufficient information to fully comprehend the issue. Such factors limit action. “Ironically, people often can't solve problems unless they think they aren't problems.19 (p30) Calling a situation a ‘mere problem’ allows responses “that are more complex, more recently learned, and more responsive to more stimuli in changing situations” and more likely to produce “lasting change in dynamic problems.”19 (p30) These responses, when they produce small wins, offer insights into an issue, foster learning, and attract additional support, new problem‐solvers and the ideas they bring. Problems a little beyond “mere” are now in sight.
4. INFORMING ACTION AT BILLINGS CLINIC
The learning principles that emerged from this work are beginning to impact how Clinic personnel think about and approach challenges and change. They are informing choices on new clinical programs and improvement processes. Examples of resulting initiatives, described below, arose contemporaneously with LHS explorations and represent new approaches to learning. Decisions to implement these initiatives and the manner in which they were implemented were influenced by the learning principles uncovered by LHS Network members. These projects are highlighted because they illustrate the principles in action and represent movement towards a more robust learning culture at Billings Clinic. We suggest that development of such a culture prepares an organization to realize the vision of Learning Health Systems: to harness science, clinical research and data, and information generated by digital technology to inform and accelerate improvement in quality health care.
4.1. Relational coordination
Relational coordination (RC) in the ICU became a method for fostering learning. Relational coordination is a theory that explores attributes that enable teams to accomplish complex tasks.25 It proposes that learning and performance are enhanced in teams where members share goals, and knowledge, interact respectfully, and communicate frequently, accurately and in a timely and problem‐solving manner. Several years ago when members of the LHS Network read the about RC, the conversation turned quickly to where to gain experience with this novel theory of collaboration. The intensive care unit (ICU) was suggested because it was moving to a much larger facility and staff was afraid the size of the unit would diminish face‐to‐face communication and undercut working relationships. The ICU was targeted because staff members placed a high value on collaboration and were constantly searching for new ways to enhance working relationships. They recognized that rapid adjustments (learning) to changing patient conditions were key to effective care.
Learning Health System Network members appreciated the similarity between RC dimensions and the learning principles. Relational Coordination advocates frequent, timely, accurate, and respectful communication within teams, which when enacted enable diverse perspectives to be accessed. Learning Health System principles call for reliance on regular updates, sensemaking, diversity, and respectful interactions in groups.
Staff members in the ICU have recognized the benefits of the RC initiative. In interviews, they stated that colleagues from different disciplines are more comfortable with raising concerns, suggestions, and solving problems together; staff involved in care have a better understanding of the complexities of care and the contributions others can make; and that care is better because teamwork has improved and staff are more engaged in ongoing improvement efforts.
As part of the ICU RC initiative, a survey revealed the rehabilitation department was rated poorly by other professional groups on RC dimensions. Armed with this knowledge, members of the department embraced the challenge of becoming better professional partners in the ICU. At an early meeting of the multidisciplinary team guiding the RC effort, a critical care physician asked, “What does timely communication mean to us?” In the resulting discussion an idea emerged. The ICU nurse case manager asked, “What if you [the rehab staff present] contacted each patient's nurse in the morning to discuss the goals of care, planned treatments and the best timing of rehab treatment?” Those at the meeting realized greater involvement of rehab staff in ICU patient care, and early rehab treatment could improve pain management and recovery. The next morning the plan was implemented. Over time, this strategy greatly improved working relationships between nurses and rehabilitation specialists. A follow‐up RC survey that showed scores for the rehabilitation staff improved more than any other discipline. A rehabilitation manager expressed it this way, “I've noticed big changes in the ICU. For years the ICU was an unwelcoming environment for therapists. Now it's become a desirable assignment. No longer does staff feel like they are walking onto an island.”
4.2. Safe and Reliable Healthcare
Another outside influence that has helped Billings Clinic make sense of the essential dimensions of learning is a project with Safe and Reliable Healthcare, a consultancy with extensive experience in safety culture.26 The project featured the creation of frontline teams that identified aims for improvement in both clinical and cultural areas, and worked together to develop solutions that were implemented through rapid testing cycles. Teams sought frequent input and shared results on publically displayed learning and process boards.
The Inpatient Medical Unit (IPM) improvement team worried that some patients transferred from other facilities arrived on their unit much sicker than anticipated and had to be transferred to intensive care within a few hours of arrival. Concern for the increased risk this caused to the patients and the waste to the system led the improvement team to select this problem as its clinical aim. Allowing the team to choose its own aim animated members of the team.
Embracing the concept of sensemaking rather than decision making, the group forged a partnership with the Emergency Department (ED) to test its first solution and bring more diverse perspectives to the problem‐solving conversations. Making use of the ED staff's expertise in triage, the initial test involved a brief assessment of selected patients in the ED prior to their admission to IPM.
This test failed and was discontinued in less than 24 hours. Communication errors resulted in an additional 20 patients, rather than the anticipated 2 to 3 patients, being routed through the ED. In addition, the first day of the test coincided with one of the ED's busiest days. The ED was overwhelmed, and the test was aborted.
Making sense of the failure of this trial became a source of real learning and a lesson to the staff of the value of sensemaking and updating.
Rich conversations between the personnel from the 2 units led to a real understanding of what worked, what did not work, and what they should try next, and to better working relationship between the units. And 1 of the 20 patients seen that day in the ED was diverted to the ICU, demonstrating the value of their work. The second trial solution was aborted the day before implementation when frontline staff detected flaws. The third trial focused on improving communication between nurses at the outside referring facilities and the IPM receiving nurses, and using the ED to triage the highest risk patients. This trial succeeded: It eliminated placement errors and in several instances led to better care plans that resulted from richer nurse‐to‐nurse communication. It also served as an example of the “small wins” principle.
In the months following the initial test, the IMU improvement team resolved other problems, many of which had previously resisted resolution. There was an appreciation of and commitment to continuous learning and improvement. When asked what staff members felt was responsible for their success, the answer was unanimous—the initial failure. This failure led them into a cycle of sensemaking that taught them far more than an initial success would have.
4.3. Project ECHO
Project ECHO (Extension for Community Healthcare Outcomes) is a novel approach to providing the benefits of specialty care to underserved populations through learning communities of primary care professionals and specialists.1, 27 Using advanced telehealth technology, virtual ECHO clinics are attended by primary care staff from multiple practices and a specialist team. For example, the hepatitis C clinic run by the University of New Mexico is “staffed” by a gastroenterologist specializing in liver disease, a pharmacist, a psychiatrist, and primary care providers. During these clinics, primary care practitioners present cases and solicit guidance from the specialist team and primary care colleagues from other practices. A treatment plan is codeveloped. In subsequent clinics, the team reviews the status of treatment and makes changes as indicated. Research has shown that treatment for hepatitis C, a complex disease, can be brought to underserved communities by well‐supported primary care practitioners and yield cure rates that are comparable to those achieved by specialists in academic medical centers.1 “Prior to Project ECHO, fewer than 1,600 New Mexico residents and no state prison inmates had received treatment for HCV [hepatitis C virus] and chronic liver disease, despite there being an estimated 34,000.”28 (p1125)
When LHS Network members discovered Project ECHO, they immediately recognized the structure of the offering was concordant with the 6 learning principles. Consequently, they helped create the first Billings Clinic Project ECHO offerings that brought mental health and addictions expertise to patients and prisoners in underserved areas of Montana. Psychiatrists, counselors, and social workers from Billings interact with nurse practitioners, physician assistants, counselors, and family medicine physicians from outlying rural clinics and state prisons. The concern these professionals have for the well‐being of patients without access to specialty mental health care animates those who participate. By interacting regularly through weekly virtual clinic sessions, regular updating is accomplished. Formation of this new group composed of professionals from multiple disciplines brings new and diverse expertise into the treatment planning discussions. Those who lead ECHO clinics were trained to facilitate respectful interactions between the specialty and primary care professionals. Concentrating on small wins—the joint creation of treatment plans for individual patients—strengthens the capabilities of participating health professionals to improve mental health care across a large rural area.
One can grasp how these ingredients can lead to the development of what the creator of Project ECHO called a “knowledge network.”27
One can also see how these ingredients embody the 6 principles the Billings team identified to create a learning culture.
5. CONCLUSION
The current LHS literature, while exploring many dimensions of Learning Health Systems, devotes insufficient attention to the actual process of learning. Without such attention in the literature and to the practices within health care organizations, it seems unlikely the full potential of Learning Health Systems will be realized.
One organization, Billings Clinic, in an attempt to move towards the LHS vision, has identified a set of principles from the social science literature, insights on improvement uncovered in staff interviews and from experience to foster learning and the creation of a learning culture.
Draw on wisdom of groups and value connections
Embrace sensemaking over decision making in dealing with the unexpected
Bring diverse perspectives to complex challenges
Animate people, provide direction, update regularly, and interact respectfully
Appreciate the power and ubiquity of emergent change and the limitations of planned change
Concentrate on small wins and characterize challenges as mere problems.
Health care systems can become Learning Health Systems by integrating progress in science, advances in research, and data and information generated by digital technology into a robust learning culture. Such a culture can be supported by the types of novel programs and change models—RC, Safe and Reliable Healthcare, Project ECHO—adopted at Billings Clinic. Fulfilling the promise of LHS, dramatic improvement in health system performance now becomes imaginable.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGEMENTS
The authors wish to dedicate this article in memory of Reuben M. McDaniel, Jr, a scholar and friend who served as an inspiration to us and his many students and colleagues.
Potts J, Thompson R, Merchant R, et al. Learning: Contemplating the unexamined core of Learning Health Systems. Learn Health Sys. 2017;1:e10036 10.1002/lrh2.10036
REFERENCES
- 1. Arora S, Thornton K, Murata G, et al. Outcomes of treatment of hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199‐2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Institute of Medicine (US) . Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 3. Institute of Medicine . Roundtable on value & science‐driven health care 2006. Available at:https://www.nationalacademies.org/hmd/Activities/Quality/VSRT.aspx. Retrieved March 20, 2016. [Google Scholar]
- 4. Etheredge L. Rapid learning: a breakthrough agenda. Health Aff. 2014;33(7):1155‐1162. [DOI] [PubMed] [Google Scholar]
- 5. Friedman C, Rubin J, Brown J, et al. Toward a science of learning systems: a research agenda for the high‐functioning Learning Health System. J Am Inf Assococ. 2015;22:43‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Greene S, Reid R, Larson E. Implementing the Learning Health System: from concept to action. Ann Intern Med. 2012;157(3):207‐210. [DOI] [PubMed] [Google Scholar]
- 7. Institute of Medicine (US) . Digital Infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 8. Institute of Medicine (US) . The Learning Healthcare System: Workshop Summary. Washington, DC: The National Academies Press; 2007. [PubMed] [Google Scholar]
- 9. Krumholz H. Big data and new knowledge in medicine: The thinking, training and tools needed for a Learning Health System. Health Aff. 2014;33(7):1163‐1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The American Heritage Dictionary . Boston: Houghton Mifflin; 1992. [Google Scholar]
- 11. Psek W, Stametz R, Bailey‐Davis L, et al. Operationalizing the Learning Health Care System in an integrated delivery system. Generating Evid Methods Improve Patient Out. 2015;3(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lindberg C, Hatch MM, Ciemins E. Embracing uncertainty: complexity inspired innovations at Billings Clinic In: Sturmberg MC, ed. Handbook of Systems and Complexity in Health. New York: Springer; 2012. [Google Scholar]
- 13. Anderson R, Toles MC, Colon‐Emeric C. Local interaction strategies and capacity for better care in nursing homes: A multiple case study. BMC Health Serv Res. 2014;14(1):1‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kauffman S. At Home in the Universe: The Search for the Laws of Self‐Organization and Complexity. New York: Oxford University Press; 1995. [Google Scholar]
- 15. McDaniel R, Walls M. Diversity as a management strategy for organizations: a view through the lenses of chaos and quantum theories. J Manag Inq. 1997;6(4):371‐383. [Google Scholar]
- 16. Stacey R. Strategic Management and Organisational Dynamics: The Challenge of Complexity. Harlow: Prentice Hall; 2011. [Google Scholar]
- 17. Zimmerman B, Lindberg C, Plsek P. Edgeware: Insights for Health Care Leadership from Complexity Science. Irving: VHA Inc; 1998. [Google Scholar]
- 18. Weick K. Managing the unexpected: complexity as distributed sensemaking In: McDaniel R, Driebe D, eds. Uncertainty and Surprise in Complex Systems. Berlin: Springer‐Verlag; 2005:51‐65. [Google Scholar]
- 19. Weick K. Small wins: redefining the scale of social problems. Am Psychol. 1984;39(1):40‐49. [Google Scholar]
- 20. Ryan R, Deci E. Self‐determination theory and the facilitation of intrinsic motivation, social development, and well‐being. Am Psychol. 2000;55(1):68‐78. [DOI] [PubMed] [Google Scholar]
- 21. Weick K. Emergent change as a universal in organizations In: Weick K, ed. Making Sense of the Organization, Volume 2: The Impermanent Organization. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 22. McDaniel R. Management strategies for complex adaptive systems: sensemaking, learning, and improvisation. Perform Improv Q. 2007;20(2):21‐42. [Google Scholar]
- 23. McDaniel R, Jordon M, Fleeman B. Surprise, surprise, surprise! A complexity science view of the unexpected. Health Care Manage Rev. 2003;28(3):266‐278. [DOI] [PubMed] [Google Scholar]
- 24. Ashby WR. An Introduction to Cybernetics. London: Chapman & Hall LTD.; 1957. [Google Scholar]
- 25. Hoffer Gittell J, Fairfield K, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay. Med Care. 2000;38(8):807‐819. [DOI] [PubMed] [Google Scholar]
- 26. Leonard M, Frankel A, Knight A. What facilitates of hinders team performance in organizations In: Salas E, Frush K, eds. Improving Patient Safety Through Teamwork and Team Training. New York: Oxford University Press; 2013:27‐38. [Google Scholar]
- 27. Arora S, Geppert C, Kalishman S, et al. Academic health center management of chronic diseases through knowledge networks: project ECHO. Acad Med. 2007;82(2):154‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Arora S, Kalishman S, Thornton K, et al. expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010;52:1124‐1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Weick K. Impermanent systems and medical errors; requisite variety mitigates adversity In: Weick K, ed. Making Sense of the Organization, Volume 2: The Impermanent Organization. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]


