Abstract
Introduction
Health information exchange (HIE) capabilities meet the demands for a more effective, efficient, and safer health care system. However, organizations and individual providers have pursued different strategies to meet their respective needs for HIE capabilities. Because effective information sharing is necessary to a learning health system, this study sought to explore the perceptions of different approaches' effect on key features of an effective health care system.
Methods
An anonymous web‐based survey was sent to a convenience sample of the membership of the Healthcare Information and Management Systems Society and the Strategic Health Information Exchange Collaborative with knowledge of HIE (n=68). A series of 7‐point Likert‐type items measured perceptions of enterprise health information exchanges (eHIEs) and community health information organizations (cHIOs) in the areas of effect on exchange participation, effect on market dynamics, relationship to DIRECT Secure Messaging and vendor‐mediated exchange, and effect on quality. Also, respondents were asked to rate 13 qualities and services as “more about eHIE” or “more about cHIO.”
Results
Respondents tended to agree on the importance of cHIO and eHIE. Community benefits and support for public health agencies were concepts more often applied to cHIOs.
Discussion
This study affirmed much of the conventional wisdom and anecdotal comments about perceptions of cHIOs and eHIEs. Although the respondents viewed cHIOs and eHIEs differently in terms of broader societal benefit and strategic advantage, nonetheless consistent agreement appeared in areas of importance in relationship to other information sharing strategies and overall effect on the quality of care.
Keywords: health information exchange, organizational strategy, policy
1. INTRODUCTION
Health care providers and health service organizations need to exchange patient information to meet the demands for a more effective, efficient, and safer health care system. Health information exchange (HIE) supports better communication for care coordination, facilitates access to information during care transitions, enables population health monitoring and analytics, and leads to more efficient care. In the US health care system, significant support exists for HIE. For example, federal health policies emphasize the need for HIE1, 2 and consider HIE as a fundamental step in the progress to a learning health system3 and that it supports the core values of person‐focused health, adaptability, accessibility, and value.4 Likewise, health care providers and service organizations require effective information exchange capabilities to be successful in payment reform initiatives like Accountable Care Organizations and value‐based payment programs, and to respond to quality improvement efforts like the Hospital Readmissions Reduction Program. Although HIE has an important role in the US health care system, no single federal policy or plan specifies how health care organizations are to actually undertake HIE.
In response, US health care organizations and individual providers have pursued different strategies to meet their respective needs for HIE capabilities. One option is participation in a community health information organization (cHIO). cHIOs are generally nonprofit collaboratives, government agencies, or public‐private partnerships with goals of facilitating health information exchange activities for an entire state or region. cHIOs are sometimes referred to as “public HIEs” either because they tend to seek participation from all providers in an area or because they have often been supported by public funding. cHIOs include regional health information organizations and state‐designated entities.5 In addition, health systems have chosen to be the organization that facilitates information exchange themselves. In contrast to the collaborative governance model, enterprise health information exchange (eHIE) is the term applied to a health system led and organized effort. Health systems connect affiliated providers, referring practices, and medical trading partners within their eHIE. eHIEs are also labeled as “private HIEs” because participation is generally not open to all providers in the community. Other HIE options include electronic health record (EHR) vendor‐mediated HIE, where customers of the same vendor can exploit native interoperability to exchange with other customers, and DIRECT Secure Messaging (DSM), a point‐to‐point exchange option, which mimics faxing and is required capability of all government certified EHRs. All of the previously mentioned strategies accomplish information exchange, have potential benefits, and address specific use cases and needs.
The various approaches to HIE, which have developed in the US health care system, are not necessarily mutually exclusive. Nevertheless, evidence suggests that those in health care may view the approaches as incompatible or even in competition. Such a view has the risk of creating information silos and not fostering broad information exchange across all settings and providers of care. Perceptions of incompatibility are most notable in cHIO and eHIE comparisons. For example, some cHIO leaders and policy makers reportedly view eHIEs as a barrier to participation in community‐based exchange efforts6 and health systems have opted not to participate in cHIOs in favor of pursing eHIE.7 Such perceptions are not unidirectional. Early publications promoting eHIE clearly touted the strategy as better or superior to cHIOs.8, 9 Regardless of perceptions, at a minimum, eHIEs and cHIOs are in competition for organizational resources such as time, skilled staff, and financing.10 Additionally, divisions in perceptions also extend to the roles of DSM and vendor‐mediated exchange as federal policy increased emphasis on these strategies, while decreasing emphasis on cHIOs.6, 11 Despite these seemingly prevailing perceptions, a number of health service organizations have embraced multiple strategies; health systems with Enterprise HIE have been active participants in cHIOs while also leveraging vendor‐mediated exchange and cHIOs also offer DSM.
1.1. Research interests
The objective of this study was to explore perceptions of approaches to HIE and to see how these perceptions varied between cHIO, eHIE, and those unaffiliated with an exchange organization. HIE, which supports information sharing for ongoing population monitoring, effective care transitions, and aggregated analyses, is a necessary underlying component of the learning health system. HIE is a tool to meet the demands for a more effective, efficient, and safer health care system.12 However, our knowledge of the health care systems views on the different approaches to HIE has been based on a few qualitative studies and anecdotal evidence. We surveyed a broad set of stakeholders and health care professionals in order to quantitatively compare perceptions of cHIOs and eHIEs in two important areas of an effective health care system:
Effect on the delivery of health care services
Support for community and public goods.
2. METHODS
2.1. Sample and data collection
We targeted the membership of the Healthcare Information and Management Systems Society (HIMSS) with knowledge of HIE for an anonymous, web‐based survey. Survey invitations were advertised and announced through various HIMSS‐maintained communication channels, such as e‐mail distribution lists and weekly digital newsletters and announcements within relevant volunteer group meeting agendas, as well as targeted marketing to the members of the Strategic Health Information Exchange Collaborative (SHIEC). Recruitment ran from 5/18/2016 until 7/30/2016. Respondents were generally in business and managerial roles with job titles such as chief executive officer, program manager, executive director, chief information officer, chief medical informatics officer, senior vice president, or director.
2.2. Survey instrument and items
The survey covered the areas of organizational demographics, participation in HIE organizations, perceptions, and market characteristics. A series of 7‐point Likert‐type items measured perceptions of eHIEs and cHIOs in the areas of effect on participation in other types of HIE, effect on market dynamics, relationship to DSM and vendor‐mediated exchange, and effect on quality. In addition, respondents were asked to rate an additional 13 items as “more about eHIE” or “more about cHIO.” These were measured on 5‐point Likert‐type scale with “applies equally to both” as the neutral choice. The items in the eHIE/cHIO comparisons covered a range of areas, including information and vendor quality as well as support of public and population health. See Appendix A for survey items. Before the survey went public, we piloted the survey with 3 volunteers (representing a cHIO, a health service organization, and a government agency) for comprehension, content area, and length.
2.3. HIE participation types
We grouped respondents based on their primary place of work's participation in, or leadership of, HIE efforts. The cHIO group included all respondents that identified a cHIO or State Designated Entity as their primary place of work and those respondents from hospitals and other health service organizations that reported their primary place of work participated in at least 1 cHIO. The eHIE group included all respondents whose primary place of work (eg, health system, hospital, or ambulatory care) participated or lead an eHIE. Because of the small sample size, respondents who reported their primary place of work participated in both a cHIO and an eHIE were included in the eHIE group. The unaffiliated group included all other respondents. Participation was self‐reported.
2.4. Analysis
Frequencies and percentages describe the organizations and HIE participation types in the study sample. Items on the perceptions of cHIOs and eHIEs were summarized using medians and interquartile ranges. Differences in perception scores between HIE participation type were assessed using the nonparametric Kruskal–Wallis rank test. For items directly comparing cHIOs with eHIEs, we tabulated the distribution of responses and compared perceptions against the neutral (“applies equally to both) category using the Wilcoxon signed‐ranks test.
3. RESULTS
A total of 68 individuals responded to the survey (Table 1). Respondents working at a cHIO (including state‐designated entities) were the largest group (38.2%), followed by respondents associated with health systems (25.0%). Other respondents included a diverse set of organizations such as vendors, consultants, payers, and financial institutions. Most respondents were participating in or leading an HIE organization (ie, their organization had direct experience). Half (50.0%) were associated with a cHIO and 16.2% were associated with an eHIE. Of the eHIE group, 4 organizations were participating in both a cHIO and an eHIE.
Table 1.
Organizational characteristics of survey respondents
| n (%) | |
|---|---|
| Organization type | |
| Community HIO | 26 (38.2) |
| Health system | 17 (25.0) |
| Hospital (single system or standalone) | 5 (7.4) |
| Ambulatory care | 6 (8.8) |
| Long term care | 2 (2.9) |
| Payer | 2 (2.9) |
| Other | 10 (14.7) |
| Participation in HIE | |
| Community HIO | 34 (50.0) |
| Enterprise HIE | 11 (16.2) |
| No participation | 23 (33.8) |
| Number of Community HIOs in marketa | |
| 0 | 7 (14.3) |
| 1 | 21 (42.9) |
| 2 or more | 21 (42.9) |
| Number of Enterprise HIEs in marketa | |
| 0 | 9 (26.5) |
| 1 | 9 (26.5) |
| 2 or more | 16 (47.1) |
Excluding respondents reporting “I don't know.”
Respondents tended to agree on the importance of cHIO and eHIE and the relationship to alternative HIE strategies. For example, respondents generally agreed with statements that eHIEs will improve the quality of care (Table 2). Likewise, respondents on average disagreed with the statements that DSM or vendor‐mediated exchange eliminated the need for both eHIE. The overall perceptions about quality, DSM, and vendor‐mediated exchange were similar for cHIOs (Table 3). However, respondents differed on their perceived effects of cHIOs and eHIE on data sharing and patient care patterns. Overall, respondents were neutral about the eHIE's effect on patients' ability to seek care from other health systems (Table 2). By contrast, respondents more strongly agreed that cHIOs made it easier for patients to seek care from different health systems and were more likely to disagree with statements that cHIO membership limited data sharing.
Table 2.
Respondents' median agreement (and interquartile range) with statements about enterprise health information exchange (eHIE) by type of participation
| Participation type | |||||
|---|---|---|---|---|---|
| Total | cHIO | eHIE | Unaffiliated | P | |
| Health systems are less likely to share data in an eHIE | 4.0 (4) | 4.0 (4) | 4.0 (3) | 6.0 (1) | 0.028 |
| Hospitals are less likely to share data in an eHIE | 4.0 (4) | 4.0 (3) | 3.0 (3) | 5.5 (3) | 0.047 |
| Independent providers are less likely to share data in an eHIE | 4.0 (3) | 4.0 (3) | 4.0 (4) | 5.0 (3) | 0.174 |
| Changes referral patterns | 5.0 (2) | 5.0 (2) | 5.0 (2) | 5.0 (2) | 0.793 |
| Makes it easier for patients to see different health systems | 4.0 (4) | 3.0 (3) | 6.0 (3) | 5.0 (2) | 0.001 |
| Will encourage market consolidation | 4.0 (2) | 4.0 (2) | 4.5 (2) | 4.0 (1) | 0.505 |
| Vendor‐mediated HIE eliminates need for eHIE | 3.0 (3) | 2.0 (3) | 3.0 (2) | 3.0 (3) | 0.903 |
| DSM eliminates need for eHIE | 1.0 (2) | 1.0 (2) | 1.0 (2) | 2.5 (2) | 0.643 |
| Will improve the quality of care | 5.0 (2) | 5.0 (2) | 6.0 (1) | 5.0 (2) | 0.025 |
Range = strongly disagree (1) to strongly agree (7); cHIO = respondents participating in community health information organization; eHIE = respondents participating in enterprise health information exchange; unaffiliated = respondents participating in neither.
Table 3.
Respondents' median agreement (and interquartile range) with statements about community health information organizations (cHIO) by type of participation
| Participation type | |||||
|---|---|---|---|---|---|
| Total | cHIO | eHIE | Unaffiliated | P | |
| Health systems are less likely to share data in a cHIO | 3.0 (2) | 3.0 (2) | 3.0 (3) | 3.0 (3) | 0.271 |
| Hospitals are less likely to share data in a cHIO | 3.0 (2) | 3.0 (2) | 3.5 (3) | 3.0 (3) | 0.304 |
| Independent providers are less likely to share data in a cHIO | 3.5 (3) | 3.5 (3) | 3.5 (3) | 3.5 (2.5) | 0.659 |
| Changes referral patterns | 4.0 (2) | 4.0 (2) | 4.0 (1) | 4.0 (1) | 0.773 |
| Makes it EASIER for patients to see different health systems | 6.0 (2) | 6.0 (2) | 6.0 (2) | 5.0 (2) | 0.183 |
| Will encourage market consolidation | 4.0 (2) | 4.0 (2) | 4.0 (0) | 3.5 (2) | 0.759 |
| Vendor‐mediated HIE eliminates need for cHIO | 1.5 (2) | 1.0 (2) | 2.0 (3) | 3.0 (2) | 0.117 |
| DSM eliminates need for cHIO | 2.0 (2) | 1.0 (1) | 1.5 (3) | 3.0 (1.5) | 0.030 |
| Will improve the quality of care | 6.0 (2) | 7.0 (1) | 6.5 (2) | 5.0 (2) | 0.001 |
Range = strongly disagree (1) to strongly agree (7); cHIO = respondents participating in community health information organization; eHIE = respondents participating in enterprise health information exchange; unaffiliated = respondents participating in neither.
Further differences were more notable when stratified by respondents' type of HIE participation (Tables 2 and 3). For instance, respondents whose organizations did not participate in either a cHIO or an eHIE, or the unaffiliated, tended to be more neutral on the ability of cHIOs to improve the quality of care, the ease of which cHIOs or eHIEs allow patients to seek care from different systems, and the potential for DSM or vendor‐mediated exchange options to eliminate the need for cHIOs and eHIE. In addition, respondents associated with cHIOs were in strong agreement with that approach's ability to improve care and viewed the ability of eHIE to support patients seeking care from other systems (Table 2) with more skepticism (P < 0.001). Those associated with eHIEs were different from other respondents, in that they disagreed with the statement that hospitals (P = 0.047) in eHIEs are less like to share data with cHIOs.
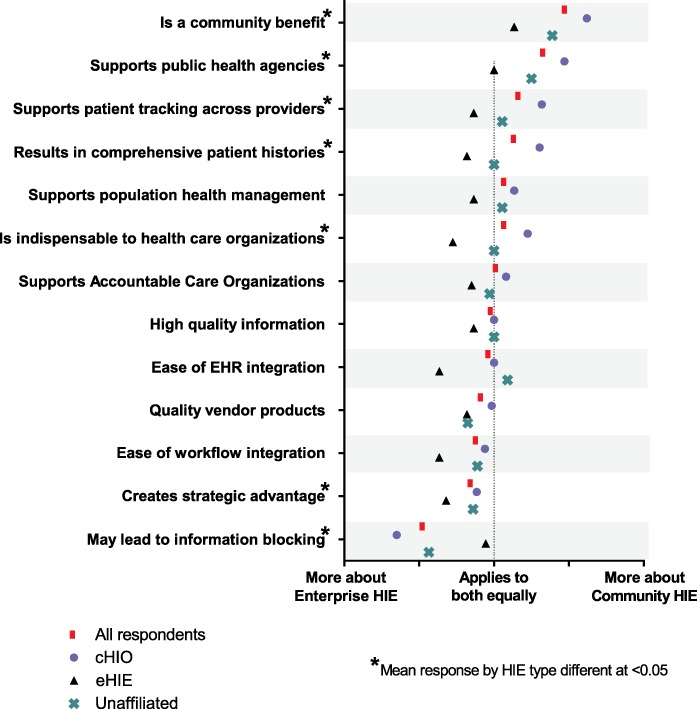
When asked to attribute statements about characteristics, qualities, and capabilities, respondents overall stated that most applied to cHIOs and eHIE equally (Table 4). Nonetheless, several key differences existed. First, being a community benefit (P < 0.001) and support for public health agencies (P < 0.001) were concepts more often applied to cHIOs than eHIEs. Likewise, the perceptions of the ability of each strategy to support patient tracking across providers were skewed toward cHIOs (P = 0.013). By contrast, quality vendor products (P = 0.019), ease of workflow integration (P = 0.013), and strategic advantage (P = 0.021) were more strongly associated with eHIE. Fourth, the statement “may lead to information blocking” was applied more to eHIE (P < 0.001). Although not apparent in the overall distributions, stratified analyses reveals an apparent trend in perceptions (Appendix Figure A1). For each statement that could be considered a positive (eg, is a community benefit, supports population health management, ease of workflow integration, etc.), respondents tended to report the statement applied more to their own type of HIE. In opposite fashion, cHIOs applied the undesirable statement (eg, “may lead to information blocking”) more strongly to eHIEs and eHIEs were more neutral.
Table 4.
Distribution responses to whether qualities apply more to enterprise HIE or community health information organizations
| More about eHIE | Applies equally to both | More about cHIO | P | |||
|---|---|---|---|---|---|---|
| 1 (%) | 2 (%) | 3 (%) | 4 (%) | 5 (%) | ||
| N | 6.4 | 6.4 | 77.9 | 4.8 | 4.8 | 0.594 |
| Quality vendor products | 4.9 | 11.5 | 80.3 | 3.3 | 0.0 | 0.019 |
| Ease of EHR integration | 8.1 | 16.2 | 59.6 | 8.1 | 8.1 | 0.372 |
| Ease of workflow integration | 11.1 | 15.9 | 65.1 | 3.2 | 4.8 | 0.013 |
| Supports population health management | 9.7 | 6.5 | 61.3 | 6.5 | 16.2 | 0.381 |
| Supports patient tracking across providers | 4.8 | 11.3 | 50.0 | 14.5 | 19.4 | 0.030 |
| Supports public health agencies | 3.2 | 0.0 | 54.0 | 14.3 | 28.6 | <0.001 |
| Results in comprehensive patient histories | 4.8 | 8.1 | 62.9 | 4.8 | 19.4 | 0.097 |
| Is indispensable to health care organizations | 5.0 | 6.8 | 68.3 | 10.0 | 10.0 | 0.242 |
| Creates strategic advantage | 17.0 | 20.3 | 47.5 | 8.5 | 6.9 | 0.021 |
| Supports accountable care organizations | 5.0 | 20.0 | 56.7 | 5.0 | 13.3 | 0.673 |
| May lead to information blocking | 41.2 | 19.6 | 33.3 | 5.9 | 0.0 | <0.001 |
| Is a community benefit | 1.6 | 0.0 | 39.7 | 20.6 | 38.1 | <0.001 |
P = Wilcox sign rank test for median against “applies equally to both” response.
4. DISCUSSION
This study affirmed much of the conventional wisdom and anecdotal comments about different perceptions of cHIOs and eHIEs. Although the respondents viewed cHIOs and eHIEs differently in terms of broader societal benefit and strategic advantage; nonetheless, consistent agreement appeared in areas of importance in relationship to other information sharing strategies and overall effect on the quality of care. The areas of diverging viewpoints and the areas of agreement point toward concrete steps organizations can undertake to improve HIE efforts and to foster better collaboration to enable secure and ubiquitous exchange across the country.
For one, results indicate a recognized role in the health care system for both cHIOs and eHIEs. Notably, respondents saw cHIOs and eHIEs equally applicable to a wide number of issues from supporting population health to quality of information. Also, respondents were clear that cHIOs and eHIEs cannot be completely replaced by either DSM or a vendor‐mediated HIE solution. Although both the aforementioned approaches facilitate information sharing between different providers, it is clear they are not substitutable solutions.13 Unlike DSM, cHIOs and eHIEs can generate longitudinal patient health records, which can be pulled on demand by health care professionals and can also be leveraged for analytic purposes. Likewise, vendor‐mediated HIE limits exchange activity to organizations with the same vendor, whereas both cHIOs and eHIEs gather data from multiple EHR platforms. However, the vendor‐supplied landscape is changing rapidly with new initiatives like the CommonWell Health Alliance14 and Epic's work to increase integration of cHIO information within their Care Everywhere EHR.
Second, overall respondents agreed that cHIOs and eHIEs would improve the quality of care. The number of studies indicating the benefits of HIE on cost, quality, and outcomes is growing. Most evidence, such as reductions in utilization15 and cost savings,16 comes from evaluations of cHIOs, but health systems undertake eHIEs with similar expectations.10 Nonetheless, a strong support of HIE was not universal. Respondents whose organizations did not participate in either a cHIO or an eHIE, or the unaffiliated, were less enthusiastic about potential effects on quality. HIE adoption still remains a challenge,17 and the findings of this survey indicate that cHIOs and eHIEs still need to convince a segment of the health care system of the value of HIE.
This survey corroborates earlier qualitative and popular reporting that cHIOs and eHIEs are perceived to serve different purposes within the health care system.8, 9, 10 cHIOs are associated with broader positive effects such as community benefits and support for public health. Conversely, eHIEs were associated with strategic advantage, which is a benefit to the participating organization. Although these perceptions exist, cHIOs and eHIEs are not locked into these roles. For example, cHIOs by definition cannot be a strategic advantage, but cHIOs definitely support the information and technology required for providers to pursue activities like accountable care organizations and population care management encouraged by current health reform as well as the advanced analytics necessary for a learning health system.18 cHIOs must ensure participating organizations understand how their current and growing portfolio of services, like the Patient Centered Data Home pilots initiated by SHIEC fit within these larger opportunities. Likewise, opportunities exist for eHIEs and vendor‐mediated exchange efforts to support public health agencies and to have broader community benefits. For example, eHIEs could serve as a single point of contact to efficiently supply public health agencies with immunization information from a large number of providers. eHIEs could incorporate automatic disease notification systems to improve infections disease surveillance and reporting. Lastly, HIE is a necessary capability to convene the data from multiple stakeholders in support of a learning health system.3 Partnerships between eHIEs and cHIOs would only further progress toward this aim by increasing information accessibility across the entire health care continuum.
Finally, this study highlights different perceptions of information accessibility by type of HIE strategy. Prior research suggests that hospitals avoid participating in information sharing with competitors19, 20 and that as more information is shared within health systems, less information is shared with external organizations.21 Although eHIE may be primarily a strategy to achieve a competitive advantage,10 health systems leading eHIE efforts may expect ongoing scrutiny and questioning around information accessibility and information blocking (ie, knowing and unreasonable interference with electronic information sharing).2 More importantly, if professionals in the field cannot agree about the ultimate accessibility of patient information, how can patients be expected to know when, where, and how their information will be available to their providers? Regardless of which HIE strategy an organization pursues, patients are the key beneficiaries of information sharing infrastructures and potential partners in any learning and improvement initiatives made possible by HIE. Organizations would be advised to proactively publicize the value of accessible information and inform patients about how relevant care transitions information can be shared electronically and how technology benefits individual patients and their communities.
These findings are subject to several limitations. First, the sample size is small and our sampling strategy resulted in respondents who were very knowledgeable in health information technology. Other health care professionals with less technical knowledge may have different perceptions. In addition, the public (ie, consumers, patients, family, and caregivers) is a key stakeholder in all HIE activities, but they were not included in our sampling frame. These preceding factors limit the generalizability of our findings.
5. CONCLUSION
Organizations and individual providers can meet their respective needs for ubiquitous information exchange through participation in cHIOs and eHIEs. Although the respondents viewed cHIOs and eHIEs differently in terms of broader community good and strategic advantage, nonetheless consistent agreement appeared in areas of importance in relationship to other information sharing strategies and overall effect on the quality of care.
ACKNOWLEDGMENTS
This project was funded by the Agency for Healthcare Research and Quality (no. IR03HS020304‐01A1; Vest(PI)).
APPENDIX A. Survey questions
A.1.
Survey respondents were asked to answer the following questions on a 7‐point Likert scale, with 1 = strongly disagree, 4 = neutral, and 7 = strongly agree. Respondents were also offered an “I don't know” option for each response.
In general, please indicate your agreement or disagreement with each of the following statements about Enterprise HIE:
Health systems operating an Enterprise HIE (ie, private exchanges) are LESS LIKELY to share data in a Community HIE (ie, SDO/RHIO/public exchange)
Hospitals that are part of health systems sharing data in an Enterprise HIE (ie, private exchanges) are LESS LIKELY to share data in a Community HIE (ie, SDE/RHIO/public exchange)
Standalone hospitals sharing data in an Enterprise HIE (ie, private exchange) are LESS LIKELY to share data in a Community HIE (ie, SDE/RHIO/public exchange)
Ambulatory care providers that are part of health systems sharing data in an Enterprise HIE (ie, private exchange) are LESS LIKELY to share data in a Community HIE (ie, SDE/RHIO/public exchange)
Independent ambulatory care providers sharing data in an Enterprise HIE (ie, private exchange) are LESS LIKELY to share data in a Community HIE (ie, SDE/RHIO/public exchange)
Participation in an Enterprise HIE will change ambulatory care providers' referral patterns
Enterprise HIEs will make it EASIER for patients to see providers in different health systems
Enterprise HIEs will encourage market consolidation
Vendormediated HIE (eg, Epic's Care Everywhere, CommonWell Health Alliance)
eliminates the need for Enterprise HIE
DSM eliminates the need for Enterprise HIE
Enterprise HIEs will improve the quality of care offered by participating organizations and providers
In general, please indicate your agreement or disagreement with each of the following statements about Community HIE:
Health systems participating in a Community HIE are LESS LIKELY to share data in an
Enterprise HIE
Standalone hospitals participating in a Community HIE are LESS LIKELY to share data in an Enterprise HIE
Independent ambulatory care providers sharing data in a Community HIE are LESS LIKELY to share data in an Enterprise HIE
Participation in Community HIE will change ambulatory care providers' referral patterns
Community HIEs will make it EASIER for patients to see providers in different health systems
Community HIEs will encourage market consolidation
Vendor‐mediated HIE (eg, Epic's Care Everywhere, CommonWell Health Alliance)
eliminates the need for Community HIE
DSM eliminates the need for Community HIE
Community HIEs will improve the quality of care offered by participating organizations and providers
Survey respondents were asked to answer the following questions on a 5‐point Likert scale, with 1 = more about enterprise HIE, 3 = applies to both equally, and 5 = more about community HIE. Respondents were also offered an “I don't know” option for each response.
Below are qualities related to HIE. For each, please indicate whether you think it applies more to Enterprise HIE efforts (ie, private exchanges), Community HIE efforts (including state‐designated entities), or equally to both.
High‐quality clinical information
Quality vendor products
Ease of integration into EHRs
Ease of Integration into workflow
Supports population health management
Supports patient tracking across providers
Supports public health agencies
Results in comprehensive patient histories
Is indispensable to health care organizations
Creates a strategic advantage
Supports accountable care organizations
May lead to information blocking
Is a community benefit
Vest JR, Greenberger MF, Garnatz A. Diverging views on health information exchange organizations. Learn Health Sys. 2017;1:e10031 10.1002/lrh2.10031
REFERENCES
- 1. 114th Congress . Medicare access and CHIP Reauthorization Act of 2015. 2015; 114–10. https://www.congress.gov/bill/114th-congress/house-bill/2 Accessed May 31, 2017.
- 2. Office of the National Coordinator for Health Information Technology . Report to Congress: report on health information blocking. Washington DC: Department of Health and Human Services; 2015. [Google Scholar]
- 3. Office of the National Coordinator for Health Information Technology . Connecting health and care for the nation: A shared nationwide interoperability roadmap. Washington DC; 2015. [Google Scholar]
- 4. Rubin JC, Friedman CP. Weaving together a healthcare improvement tapestry: Learning health system brings together health IT data stakeholders to share knowledge and improve health. J AHIMA. 2014;85(5):38‐43. [PubMed] [Google Scholar]
- 5. Rubin RD. The Community Health Information Movement: Where it's been, where it's going In: O'Carroll PW, Yasnoff WA, Ward ME, Ripp LH, Martin EL, eds. Public Health Informatics & Information Systems. New York: Springer; 2003. [Google Scholar]
- 6. Vest JR, Campion TR Jr, Kaushal R, HITEC Investigators . Challenges, alternatives, and paths to sustainability for health information exchange efforts. J Med Sys. 2013; 37(6):9987. [DOI] [PubMed] [Google Scholar]
- 7. Dimick C. Open for business: Private networks create a marketplace for health information exchange. J AHIMA. 2012;83(5):22‐26. [PubMed] [Google Scholar]
- 8. Harris Healthcare Solutions . Harness the power of enterprise HIE, 2012.
- 9. Manos D. Enterprise HIE market poised to soar. Healthcare IT News; 2010. Available at: http://www.healthcareitnews.com/news/enterprise‐hie‐market‐poised‐soar Accessed August 17, 2016.
- 10. Vest JR, Kash B. Differing strategies to meet information sharing needs: the publicly supported community health information exchange versus health systems' enterprise health information exchanges. Milbank Q. 2016;94(1):77‐108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lenert L, Sundwall D, Lenert ME. Shifts in the architecture of the Nationwide Health Information Network. J Am Med Inform Assoc. 2012;19(4):498‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hripcsak G, Kaushal R, Johnson KB, et al. The United Hospital Fund meeting on evaluating health information exchange. J Biomed Inform. 2007;40(6 S1):S3‐S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vest JR, Campion TR, Kern LM, et al. Public and private sector roles in health information technology policy: Insights from the implementation and operation of exchange efforts in the United States. Health Policy Technol. 2014;3(2):149‐156. [Google Scholar]
- 14. Bresnick J. Can CommonWell make health data interoperability a reality? HealthITAnalytics; 2015. Available at: http://healthitanalytics.com/news/can‐commonwell‐make‐health‐data‐interoperability‐a‐reality [Accessed May 10, 2016].
- 15. Frisse ME, Johnson KB, Nian H, et al. The financial impact of health information exchange on emergency department care. J Am Med Inform Assoc. 2012;19(3):328‐333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jung H, Vest JR, Unruh MA, Kern LM, Kaushal R, HITEC Investigators . Use of health information exchange and repeat imaging costs. J Am Coll Radiol. 2015;12(12 Pt B):1364‐1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Furukawa MF, King J, Patel V, et al. Despite substantial progress in EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff. 2014;33(9):1672‐1679. [DOI] [PubMed] [Google Scholar]
- 18. Bielaszka‐DuVernay C. Vermont's blueprint for medical homes, community health teams, and better health at lower cost. Health Aff (Project Hope). 2011;30(3):383‐386. [DOI] [PubMed] [Google Scholar]
- 19. Adler‐Milstein J, DesRoches CM, Jha AK. Health information exchange among US hospitals. Am J Manag Care. 2011;17(11):761‐768. [PubMed] [Google Scholar]
- 20. Vest JR. More than just a question of technology: Factors related to hospitals' adoption and implementation of health information exchange. Int. J Med Inform. 2010;79(12):797‐806. [DOI] [PubMed] [Google Scholar]
- 21. Miller AR, Tucker C. Health information exchange, system size and information silos. J Health Econ. 2014;33:28‐42. [DOI] [PubMed] [Google Scholar]


