Abstract
Introduction
The overall enterprise of health care delivery is considered. The 4 levels of the enterprise include clinical practices, processes that provide capabilities and information, structure that includes the business entities involved, and ecosystem that includes Centers for Medicare and Medicaid Services and Congress, as well as societal values and norms. It is argued that the enterprise of health care delivery needs to be transformed to enable high‐quality, affordable care for everyone.
Discussion
The constructs of enterprise transformation and organizational learning are reviewed. The distinction of single‐loop versus double‐loop learning is discussed and illustrated for all levels of the health care delivery enterprise. Three health care examples are used to elaborate this distinction—cancer, population health, and health IT. Four strategies are outlined that the health care delivery enterprise can use to more effectively learn at all levels of the enterprise.
Conclusions
This overall line of reasoning suggests several important research issues. The health care delivery enterprise involves much more than treating disease and paying for it. We need to improve our methods and tools for addressing the overall enterprise. Research is also needed on better means for portraying consequences of decisions to the full range of stakeholders in the enterprise. In general, the overall goal should be a healthy, educated, and productive population that is competitive in the global marketplace. We need to better understand the available levers for achieving this goal and how to best portray the intricacies of the overall enterprise to motivate those who can pull these levers to do so.
Keywords: enterprise transformation, health care delivery enterprise, learning strategies, organizational learning
1. INTRODUCTION
Four levels of the overall health care delivery enterprise are shown in Figure 1.1, 2 This framework provides a conceptual model for understanding relationships among the various elements of this enterprise, ranging from patient‐clinician interactions at the bottom to policy and budget decisions by Congress and Centers for Medicare and Medicaid Services (CMS) at the top. In the middle, providers and payers make investment decisions that balance the patients' needs from below and the “rules of the game” from above.
Figure 1.
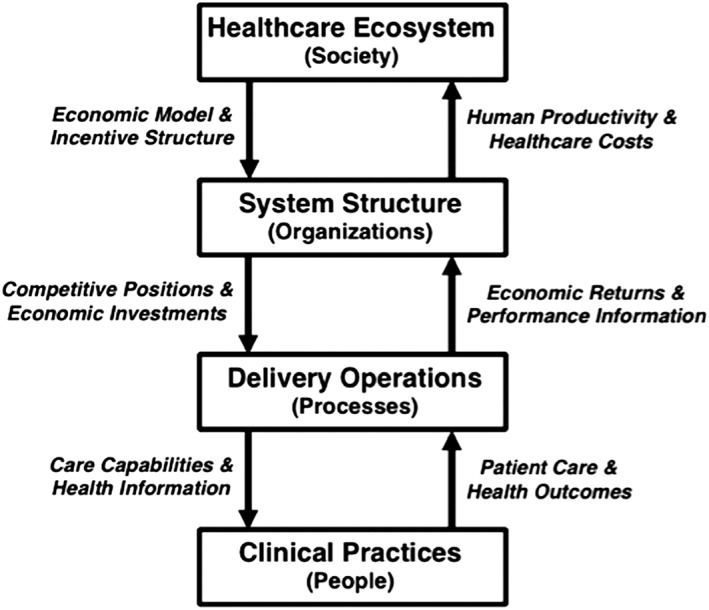
Health care delivery enterprise
Note that “medicine” is delivered on the bottom level of this figure. Additional functions associated with health care delivery occur on the other 3 levels. To foster high‐value health for everyone, learning has to occur at all of the levels.
This enterprise is being challenged by needs for fundamental change. The Affordable Care Act, evolving payment schemes, and market and technology opportunities and threats have resulted in an enormous number of initiatives at all levels of the enterprise. Orchestrating these initiatives is very much complicated by the complex adaptive nature of the health care system.3 Put simply, there are millions of independent agents reacting to the forces driving change. All of these agents are rapidly learning in the process, but the enterprise as a whole is learning much more slowly. This paper addresses this mismatch.
We begin by considering the construct of enterprise transformation. This construct is defined. A framework for transformation is presented and elaborated in the context of health care delivery. We next review what is known about organizational learning, with particular emphasis on single‐loop versus double‐loop learning. Three health care examples are used to illustrate this distinction—cancer, population health, and health IT. This leads to a discussion of 4 strategies that the health care delivery enterprise can use to more effectively learn at all levels of the enterprise. We conclude with a discussion of important research issues that need to be addressed.
This article integrates several analytic frameworks that were initially developed in other industries. This raises the question of whether health care is substantially different from other industries. In particular, health care delivery is highly fragmented, much like retail was before the consumer product companies and the big box retailers consolidated the industry over the past few decades.
However, the health care industry has in recent years exhibited more mergers and acquisitions than any other segment of the economy. Integration into large health systems is proceeding briskly.1, 2 This has enabled adoption of best practices from other industries, eg, integrated supply chain management.
We have found several analytic frameworks and methods that work well across industries ranging from health care to automotive, aerospace, retail, and telecommunications.4 Comparisons across industries can provide valuable benchmarks that can augment within‐industry comparisons, for example, across health care providers.5
Finally, an overarching theme of this paper is captured by the results of an informal survey of a large number of top executives. They were asked 1 question. “What single issue keeps you awake at night?” The most common response was, “Running the enterprise I have while trying to create the enterprise I want.” This is what motivates our desire to understand learning in the health care enterprise.
2. TRANSFORMING THE ENTERPRISE
It has been suggested that transforming health care delivery is akin to rewiring a building while the power is on. How can we design and develop a transformed system while also avoiding operational deficiencies or unintended consequences in the process? To address this question, we need a deeper understanding of the notion of enterprise transformation.
Our earlier studies6, 7 have led us to formulate a qualitative theory, “Enterprise transformation is driven by experienced and/or anticipated value deficiencies that result in significantly redesigned and/or new work processes as determined by management's decision making abilities, limitations, and inclinations, all in the context of the social networks of management in particular and the enterprise in general.”
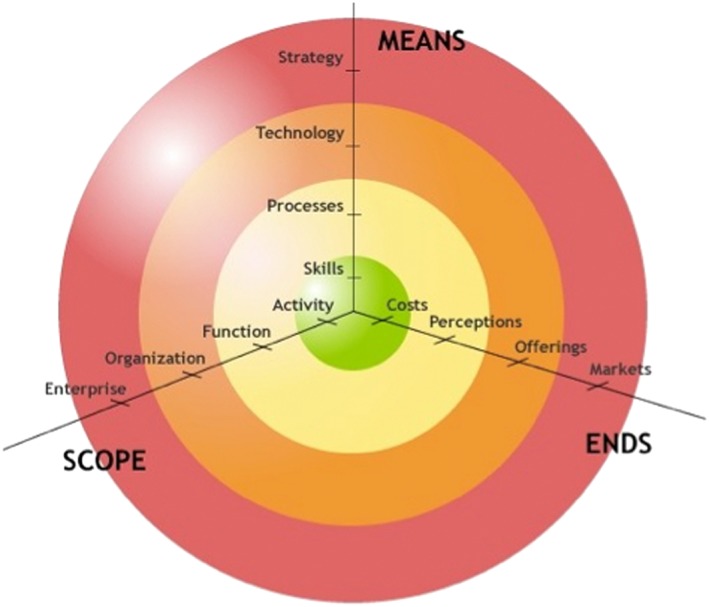
There is a wide range of ways to pursue transformation. Figure 2 summarizes conclusions drawn from a large number of case studies. The ends of transformation can range from greater cost efficiencies, to enhanced market perceptions, to new product and service offerings, and to fundamental changes of markets. The means can range from upgrading people's skills, to redesigning business practices, to significant infusions of technology, and to fundamental changes of strategy. The scope of transformation can range from work activities, to business functions, to overall organizations, and to the enterprise as a whole.
Figure 2.
Transformation framework
The framework in Figure 2 has provided a useful categorization of a broad range of case studies of enterprise transformation. Considering transformation of markets, Amazon leveraged IT to redefine book buying, while Wal‐Mart leveraged IT to redefine the retail industry. In these 2 instances at least, it can be argued that Amazon and Wal‐Mart just grew; they did not transform. Nevertheless, their markets were transformed.
Illustrations of transformation of offerings include UPS moving from being a package delivery company to a global supply chain management provider, IBM's transition from manufacturing to services, Motorola moving from battery eliminators to radios to cell phones, and CNN redefining news delivery. Examples of transformation of perceptions include Dell repositioning computer buying, Starbucks repositioning coffee purchases, and Victoria's Secret repositioning lingerie buying. The many instances of transforming business operations include Lockheed Martin merging 3 aircraft companies, Newell Rubbermaid resuscitating numerous home products companies, and Interface adopting green business practices.
The costs and risks of transformation increase as the endeavor moves farther from the center in Figure 2. Initiatives focused on the center will typically involve well‐known and mature methods and tools from industrial engineering and operations management. In contrast, initiatives towards the perimeter will often require substantial changes of products, services, channels, etc, as well as associated large investments.
It is important to note that successful transformations in the outer band of Figure 2 are likely to require significant investments in the inner bands also. In general, any level of transformation requires consideration of all subordinate levels. Thus, for example, successfully changing the market's perceptions of an enterprise's offerings is likely to also require enhanced operational excellence to underpin the new image being sought. As another illustration, significant changes of strategies often require new processes for decision making, eg, for R&D investments.
The transformation framework can be applied to thinking through a range of scenarios for health care delivery. The inner circle in Figure 2 focuses on provider efficiency by, for example, focusing on particular activities, the skills needed for these activities, and the costs of these activities. In contrast, the outer circle of Figure 2 might focus on population health (discussed later), addressing the whole enterprise, rethinking strategy, and fundamentally changing the health care marketplace.
Changes in the outer circle will very likely require changes in the adjacent circle. New offerings in a range of organizations will be enabled by new technologies. Success of these offerings is likely to involve changes of perceptions in the next circle at the functional level, enabled by new processes. Thus, we can see that moving to population health will require reconsideration of everything the enterprise does.
This does not imply that everything will change. Instead, it means that everything needs to be considered in terms of how things consistently fit together, function smoothly, and provide high‐value outcomes. This may be daunting but is entirely feasible. The key point is that one cannot consider transforming health without considering how the delivery enterprise itself should be transformed.
We hasten to note that, at this point, we are only addressing what is likely to have to change, not how the changes can be accomplished. In particular, we are not considering how to gain the support of stakeholders, manage their perceptions and expectations, and sustain fundamental change.7, 8, 9
3. ORGANIZATIONAL LEARNING
The nature of fundamental change portrayed above suggests that the health care enterprise has much to learn, especially about itself. How can the health care delivery enterprise learn? To address this question, we first need to review what is known about organizational learning in general, ranging from how it is defined to how it is pursued, including the behavioral and social factors affecting it.
Enterprise learning is defined as the capacity or process whereby an enterprise maintains or improves performance based on experience. An enterprise that learns will facilitate the learning of all its elements, enabling it to continuously transform itself. Learning is considered a distributed phenomenon that remains within the organization even as different elements of the enterprise undergo various transformations. Based on the architecture of public‐private enterprises in Figure 1, the phenomenon of learning can be understood by examining the knowledge foundation and processes at each of the levels within the architecture.
At the work practices (people) level, learning can be viewed in terms of classic production learning. On the delivery operations (processes level), an example of learning is the continual improvement or redesign of processes for planning new products and services. At the system structure (organization) level, the improvement of economic decision making occurs. Finally, on the ecosystem (society) level, policy decision making becomes refined and integrated. The abilities of the overall enterprise to learn are influenced by the learning abilities and capabilities at each level.
3.1. Production learning
Learning is a powerful source of productivity growth. As organizations produce more of a product, the unit cost of production typically decreases. Such a phenomenon is commonly referred to as a learning curve, a progress curve, an experience curve, or learning by doing. Wright10 reported production learning curves for airframe production that illustrated unit labor costs declining with cumulative output.
Learning curves have been documented in many organizations, both in the manufacturing and service sectors.11 However, the rate at which organizations learn can vary greatly from those with minimal or no learning to those with impressive productivity growth. Labor intensive organizations such as health care, education, and government have difficulty achieving the learning rates such as those seen for airplane, automobile, and semiconductor production where technology facilitates learning.2
3.2. Process learning
Frederick W. Taylor, Harvey Gantt, and Frank Gilbreth pioneered scientific management in the early decades of the 20th century. Walter Shewhart championed quality assurance and quality control a bit later. W. Edwards Deming and Joseph Juran were thought leaders in Total Quality Management in the 1970s and 1980s, perhaps epitomized by Deming's bestseller Out of Crisis.12
Process‐oriented approaches became increasingly popular as more data and computing power became widely available.13, 14 The construct of continuous improvement involves an array of techniques that can yield substantial improvements to organizations across various industries. While the production learning curve forecasts the rate of cost reductions over time, continuous improvement identifies what changes to make, and how to implement them better and faster.
Processes are a set of logically related tasks that are performed to achieve a defined outcome. Historically, process redesign was intended to streamline procedures and eliminate obvious bottlenecks and inefficiencies. More recently, particularly in the 1990s, process‐oriented thinking has been applied to a variety of functions, ranging from information technology infrastructures15, 16 to new product planning.17
3.3. Decision‐making learning
The focus on making better decisions has been a central concern of decision theory for many decades. According to Amit and Shoemaker,18 “For managers, the challenge is to identify, develop, protect, and deploy resources and capabilities in a way that provides the firm with a sustainable competitive advantage and, thereby, a superior return on capital.”
They note that managerial decisions involving resources and capabilities are often laced with uncertainty, complexity, and organizational conflict. This can make it difficult to identify the “best” decision. Simon's “satisficing” is often the only viable approach.19
A related concept is policy learning,20 which address the ways that policy systems create and use knowledge about the motivations, design, operation, and impacts of policies and policy mixes. Policy learning requires organizational capabilities to appropriately frame issues and trade‐offs in terms of problems and solutions, while taking a holistic view and anticipating future needs.
3.4. Theories of learning
Learning has, of course, long been a topic of study, with emphasis on education, training, and, more recently, organizational development and change. Classically, organizational learning has been regarded as routine based, history dependent, and target oriented.21 Routine‐based organizational learning can be extremely powerful when the learning is guided by clear short‐term feedback.22 The nature of routines, the development of effective routines, and how they change over time are key elements.
Organizational actions are history dependent in that prior knowledge enables the assimilation of new knowledge.23 Two features of absorptive capacity—cumulativeness and expectation formation—enable this historical dependency. Organizations with higher levels of absorptive capacity will be more likely to exploit opportunities present in the environment not solely based on current performance measurements. Organizations with mild absorptive capacity will be reactive and find that they are often responding to failure.
It has been observed that organizations are target oriented,24, 25 with success dependent on the relationship between the target and actual performance outcomes. It is important to note that targets change over time as measures of success are modified, particularly in response to market and technology opportunities and threats.
Most theories of organizational learning are based on the observations of individual learning.26, 27 Organizational learning is a dynamic process, based on knowledge flowing across different levels.28 A study focused on the communication of the results of leaning across units and levels found that organizational learning across levels is more relevant for organizational performance than either individual or group learning.29
Senge argues that “system thinking” is a core competency of a learning organization, with system dynamics modeling as a central enabling tool.26 Caldwell30 criticizes the idea that organizations rather than individuals learn and, in particular, find system dynamics to be an inappropriate tool. Caldwell builds on Giddens31 who argues that patterns of human interaction are created by human agency and rejects the positivist search for abstract models of learning.
Crossan, Lane, and White28 proposed a comprehensive framework of organizational learning that seeks to integrate and extend previous organizational learning research by March.32 The 2 critical challenges of renewal are recognizing and managing the tension between exploration and exploitation. Their framework of organizational learning has 4 processes: intuiting, interpreting, integrating, and institutionalizing. Intuiting and interpreting take place at the individual level while integrating and institutionalizing take place at the group and organization levels, respectively.
This framework portrays organizational learning as a dynamic process where learning occurs over time and across levels with tension among new learning/exploration, feed forward, and exploiting feedback. This relates to Weick33 and his theory of organizational sense making. The concept of sense making relates to the cognitive activity of attaching meaning to experienced situations. This involves a collaborative process of creating shared awareness and understanding drawn from different individuals' perceptions and perspectives.
3.5. Machine learning
In this era of large data sets and powerful computing, it is useful to consider machine learning. Valiant34 provides an analysis of the properties of machine learning. His recent book35 addresses adaptive computations, which he terms “ecorithms.” Ecorithms are algorithms that derive their power by learning from whatever environment they inhabit to be able to behave effectively within it. If there are good mathematical rules for predicting the process of transforming this information into knowledge, Valiant terms the process “theoryful” and everything else as “theoryless.” For both cases, whether the entity involved is a computer or not, the core of making this transformation is learning. While space does not allow a more detailed discussion of these ideas, it does suggest the possibility that humans need not be the only agents of learning in the health care enterprise.
4. SINGLE‐LOOP AND DOUBLE‐LOOP LEARNING
Chris Argyris has articulated the notions of single‐loop and double‐loop learning. “[A] thermostat that automatically turns on the heat whenever the temperature in a room drops below 68°F is a good example of single‐loop learning. A thermostat that could ask, 'why am I set to 68°F?' and then explore whether or not some other temperature might more economically achieve the goal of heating the room would be engaged in double‐loop learning.”36
Single‐loop learning uses given goals and decision‐making rules to improve performance outcomes. Double‐loop learning entails the modification of goals or decision‐making rules in the light of experience to achieve better outcomes—which may be different outcomes. Thus, double‐loop learning recognizes that the ways in which problems are defined and solved can, in themselves, be sources of problems.
This does not imply that double‐loop learning should be preferred, with single‐loop learning inherently being inferior. Instead, we should heed Peter Drucker's sage advice, “There is nothing quite so useless as doing with great efficiency something that should not be done at all.”37 In other words, first, make sure you are doing the right things; then focus on doing them right.
Of course, it would be impractical and likely incorrect to reconsider everything, eg, continually question every medical practice. Single‐loop learning should enable continually improving every practice. When it is found that performance goals cannot be achieved in this way, then double‐loop learning is likely warranted. In other words, the ways in which problems of interest are being defined and solved should be questioned.
Table 1 combines Argyris' construct with Figure 1 to yield examples of the 2 types of learning at the 4 levels of the enterprise. The single‐loop learning column reflects the aspirational status quo in the enterprise, in the sense that many organizations aspire to adopt these business best practices—and some have been successful. The double‐loop learning column represents the possibility of the enterprise learning to deliver a substantially new value proposition in health care. The remainder of this section explicates the contrast between these 2 columns.
Table 1.
Single‐loop and double‐loop learning in health care
| Single‐Loop Learning | Double‐Loop Learning | |
|---|---|---|
| Society | Cost control, eg, health care price controls | Payment for outcomes, ie, health, education, etc |
| Organization | Investment via discounted cash flow, ie, NPV | Investment via strategic value, SV = NPV + NOV |
| Process | Process improvement, eg, TQM, Six Sigma | Process reengineering, eg, BPR |
| People | Reductionist by disease and organ, ie, RCTs | Holistic approach to human wellness and health |
Abbreviations: BPR, business process reengineering; NOV, net option value; NPV, net present value; RCT, randomized clinical trial; SV, strategic value; TQM, total quality management.
4.1. Society
The total cost of health care equals the number of uses of health care times the cost per use. If the number of uses grows faster than, say gross domestic product (GDP), then single‐loop learning, like a thermostat, will reduce the cost per use by, in effect, price controls that constrain the fees for health care services. Congress and CMS control this thermostat.
Double‐loop learning questions the goal of cost control. The real goal is a healthy population, which would be easier to achieve with an educated population. This would be even easier with a productive population used in good jobs so that people could afford healthy lifestyles. It might make sense to spend more on health care if this overall goal could be achieved.
4.2. Organization
Investment decisions are informed by projections of time series of investments, operating costs, revenues, and free cash flows. The projected cash flows are converted to a net present value (NPV), by applying a discount rate to future cash flows. Use of NPV as a decision criterion is very conservative, undervaluing investments, because it assumes that later stages of investments will continue despite earlier stages failing. Nevertheless, single‐loop learning uses the NPV thermostat with a misguided sense of rigor.
Peter Boer38 defines strategic value as the sum of NPV and net option value. He argues that NPV reflects the value of what an organization is doing now, while net option value represents the value of what an organization might do in the future if it makes sense at the time. We have applied this thinking with numerous enterprises where double‐loop learning enabled uncovering billions of dollars of value in options that many of these enterprises did not realize were already in their portfolios.39
4.3. Process
The best health care organizations are very process oriented, although many organizations are still function oriented. Once processes are characterized, it is reasonable to try to improve them, perhaps via total quality management12 or Six Sigma. Single‐loop learning involves process improvement, striving for incremental increases of efficiency and effectiveness.
Double‐loop learning questions the existence of processes. It addresses why processes exist—why do we do this at all? The notion of business process reengineering40 often involves obliterating processes rather than automating them. In health care, it involves questioning the extent to which every process demonstrably improves health outcomes. This becomes critical once payment is based on outcomes achieved rather than services provided.
4.4. People
Health care delivery involves a large number of disciplines and subdisciplines. Each tends to focus on particular diseases and organs. Potential interventions, eg, procedures or pharmaceuticals, are evaluated via randomized clinical trials that carefully control experimental conditions to assure that no extraneous factors, eg, comorbidities, affect measured outcomes. Single‐loop learning involves conducting the myriad clinical trials defined by the enormous number of combinations of diseases, organs, and interventions.
Double‐loop learning is much more holistic, focusing on overall human wellness and health, drawing upon biology, physiology, psychology, sociology, and environmental sciences. This inevitably leads to addressing social and economic factors that affect lifestyles and health outcomes. In general, it does not frame life as a series of phases and episodes that potentially need medical attention.41
4.5. Trade‐offs
How much should one invest in each type of learning? Balancing resource investments across these 2 perspectives is an essential challenge of strategic management.8 As mentioned in the introduction, an informal survey of a large number of top executives were asked one question, “What single issue keeps you awake at night?” The most common response was, “Running the enterprise I have while trying to create the enterprise I want.”
We have no choice but to run the health care delivery enterprise we have, constantly improving it via single‐loop learning. At the same time, we need double‐loop learning to create the health care delivery enterprise we want. The goal is high‐value affordable health for everyone. This goal is not achievable without a balance of single‐loop and double‐loop learning.
Nevertheless, as indicated earlier, one cannot continually reconsider everything. A key indicator that double‐loop learning may be warranted is when single‐loop learning is failing to achieve desired performance goals. Then, it is likely that problem formulations need to be reconsidered along with the problem solving rules. Recall Peter Drucker's admonition to not invest in getting really good at something you should not be doing at all.
5. THREE EXAMPLES
This section elaborates 3 very specific examples of the differences between single‐loop and double‐loop learning. The first focuses on understanding and treatment of cancer. The second addresses population health, as contrasted with accountable care organizations (ACOs). The third considers big data and health IT.
5.1. Example no. 1: cancer
The evolution of understanding and treatment of cancer provides good examples of single‐loop vs double‐loop learning.42 The progression of the radical mastectomy provides a vivid example of single‐loop learning. A half million women in the United States with breast cancer endured the horrors of radical mastectomy, “an extraordinarily morbid, disfiguring procedure in which surgeons removed the breast, the pectoral muscles, the axillary nodes, the chest wall and occasionally the ribs, parts of the sternum, the clavicle and the lymph nodes inside the chest” before it was determined that the procedure provided no medical benefits.
Mukherjee43 provides a broad view of how cancer had been seen. “Cancers were lumped into categories based on their anatomical site of origin (breast cancer, lung cancer, lymphoma, leukemia), and chemotherapy treatment, often a combination of toxic drugs, was dictated by those anatomical classifications. The combinations—Adriamycin, bleomycin, vinblastine and dacarbazine, for instance, to treat Hodgkin's disease—were rarely changed for individual patients. The prospect of personalizing therapy was frowned upon: The more you departed from the standard, the theory ran, the more likely the patient would end up being undertreated or improperly managed, risking recurrence. In hospitals and clinics, computerized systems were set up to monitor an oncologist's compliance with standard therapy. If you chose to make an exception for a particular patient, you had to justify the choice with an adequate excuse. Big Chemo was watching you.” This provides another illustration of single‐loop learning.
Exploring the genes of cancer cells enabled double‐loop learning. “In the 2000s, soon after the Human Genome Project, scientists learned how to sequence the genomes of cancer cells. In cancer cells, mutated genes corrupt the normal physiology of growth and ultimately set loose malignant proliferation. Unlike normal cells, cancer cells have forgotten how to stop dividing. Once we could sequence tens of thousands of genes in individual cancer specimens, it became clear that uniqueness dominates. No other human disease is known to possess this degree of genetic heterogeneity. Gene sequencing allows us to identify the genetic changes that are particular to a given cancer. We can use that information to guide cancer treatment—in effect, matching the treatment to an individual patient's cancer.” Mukherjee44 elaborates this example of double‐loop learning in fascinating detail.
Grady45 discusses harnessing the human immune system to fight cancer. In a similar vein, The Economist 46 addresses the “personalization” of cancer treatment, including immuno‐oncology—coopting the human's immune system to fight tumors. “These days cancer is seen less as a disease of specific organs, and more as one of molecular mechanisms caused by the mutation of specific genes.” This insight has enabled matching drug therapies with the molecular characteristics of the tumor. Blood tests for circulating tumor DNA, including mutations over time, may enable changing therapies as the tumor's genes mutate. The learning associated with cancer in recent years is very impressive.
5.2. Example no. 2: population health
As defined by the CMS, an ACO is a “group of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high quality care to their Medicare patients.” If they can reduce the costs of care for these patients, relative to a defined baseline, they can earn a share of the savings if they satisfy a range of quality metrics. The CMS47 defines a shared savings and losses and assignment methodology in great detail. A key point is that the baseline is redefined each year, making earning the bonuses increasingly difficult. Nevertheless, the percentage of Americans having access to 1 or more ACOs has steadily increased,48 despite serious questions on the economic efficacy of the program.49
The ACO program provides an incentive for a coordinated effort of care for patients—less duplicative and/or unnecessary exams, tests, etc. In 2011, Medicare made almost no payments to providers through alternative payment models. However, we are slowly shifting from volume‐based fee for services to payment schemes based on value. In January 2015, Sylvia Burwell, Secretary of the US Department of Health and Human Services, announced the goal of having 85% of all Medicare fee‐for‐service payments tied to quality or value by 2016 and 90% by 2018 with 30% and 50% achieved through alternative payment models, respectively.50
Fee‐for‐service ACOs represent single‐loop learning in that providers attempt to streamline and tune their processes to incrementally reduce costs while not sacrificing quality. In contrast, population health, in its fullest sense, provides a broad vision for a healthy and educated population.51 This will require double‐loop learning across a variety of businesses and agencies.
Population health has been defined as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group”.52 The concept of population health signifies a change in improvement at the individual level to one that is focused on improving the health of an entire targeted human population. One of the biggest priorities in achieving the shift to population health is reducing health disparities among different population groups due in large part to social determinants of health.53
Societal health is more than the absence of disease and is created through the conditions and collective actions of our daily lives. It goes beyond health care to look at social, financial, and other factors that influence health. Social determinants of health are conditions in the social, environmental, cultural, and physical environment in which people are born, live, work, and age.
In the United States, it has been found that social factors including education, racial segregation, social supports, and poverty accounted for over a third of total deaths in 1 year.54 The United States experiences a direct relation between increased premature deaths as income goes down. Similarly, lower levels of education are directly related to lower income as well as a greater likelihood of smoking and shorter life expectancy.55, 56
The identification and awareness of such differences amongst populations regarding health outcomes and determinants are critical in reducing disparities and achieving health equity through a system of broad‐based population health. Much research has shown a great disparity in the access as well as quality of care based on geographic location. Such variation amongst states and health care regions extends further to include fundamental measures such as having health insurance or a connection to a regular source of care such as a primary physician.57
Accountable care organizations and hospitals, as a coalition, could take on very important roles in population health, although they alone are not likely to have the incentives or capabilities to effect the fundamental changes that population health implies.58 Academic health centers can play a major role but are unlikely to be able to deliver the full range of services.59, 60 The coordination and delivery of the needed range of services will be a challenge. Double‐loop learning will be needed to understand and make sense of the highly fragmented system that delivers health care, education, and social services.
5.3. Example no. 3: big data and health IT
This example builds on the Office of the National Coordinator for Health Information Technology (ONC) vision in Figure 3.61, 62 The aspirations portrayed in this diagram represent important advances in evidence‐based health care delivery. Much of this will be single‐loop learning, ie, getting existing processes to work together seamlessly. However, single‐loop learning within each health IT domain will not be sufficient to realize the ONC vision.
Figure 3.
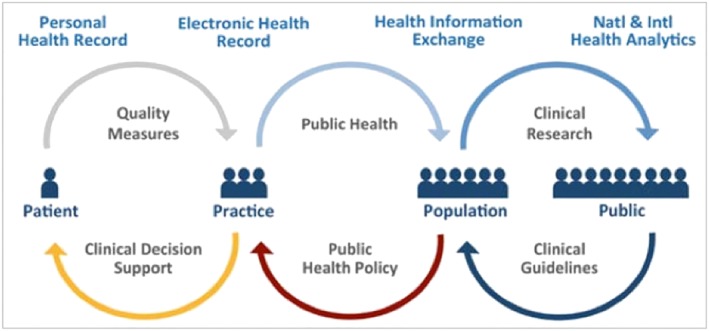
Double‐loop learning across domains, organizations, and political and legal jurisdictions will be required to enable this vision. Double‐loop learning should address overall processes across this spectrum, while also more creatively using the wealth of data generated by the system every day. There are 2 particularly important aspects of this.
William Stead63 observes, “The healthcare industry targets quality improvement at failure points in care processes as they are identified.” However, “A care process must work flawlessly end‐to‐end to improve quality sufficiently to reduce the amount of care needed and the cost of the system.” In other words, we need to improve overall processes not just steps of processes. Reengineering of processes usually involves double‐loop learning.
Second, we need to learn how to glean evidence‐based findings from the data flows in Figure 3, rather than solely relying on randomized controlled trials as the “gold standard” for evidence. The logic that led to randomized controlled trials makes good sense.64 However, it is an expensive and slow way to learn. Further, such trials are typically conducted with cohorts that are not representative of real patient populations, especially for older patients. Thus, results are difficult to extrapolate and scale to real populations.
We need to take advantage of the vast amount of clinical, claims, and financial data generated from everyday patient care, as well as nonhealth data sources such as social media. For example, Bohnsack65 argues, “By combining historical claim information with demographic and social data, healthcare organizations can build a model that will segment a covered population based on risk. In a zip code where individuals have a predisposition to diabetes, it is possible to alter the prevention model. By providing educational services, free testing, and easy‐to‐access preventative care, diabetes can be better managed. Areas that do not meet that criterion will not require such an investment.”
6. LEARNING STRATEGIES
Enterprises have differing abilities to predict their futures, as well as differing abilities to respond to these futures. What strategies might enterprise decision makers adopt to address alternative futures? As shown in Figure 4, we have found that there are 4 basic strategies that decision makers can use: optimize, adapt, hedge, and accept.
Figure 4.
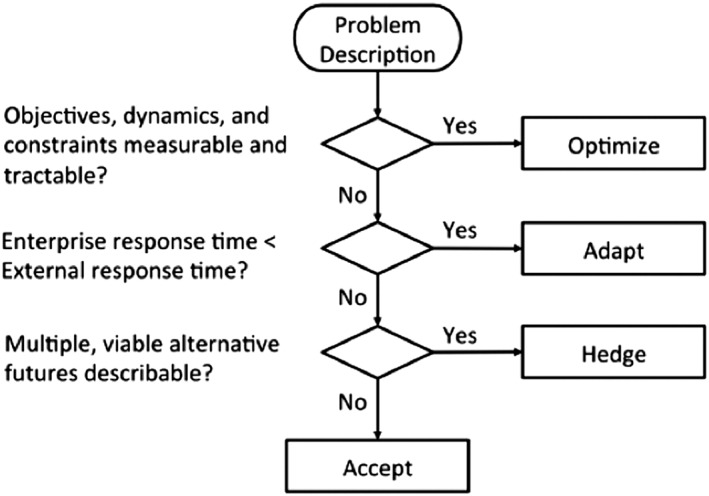
Strategy framework for enterprise decision makers66
If the phenomena of interest are highly predictable, then there is little chance that the enterprise will be pushed into unanticipated territory. Consequently, it is in the best interest of the enterprise to optimize its interventions to be as efficient as possible. In other words, if the unexpected cannot happen, then there is no reason to expend resources beyond process refinement and improvement.
If the phenomena of interest are not highly predictable, but interventions can be appropriately adapted when necessary, it may be in the best interest for the enterprise to plan to adapt. For example, agile capacities can be designed to enable their use in multiple ways, to adapt to changing demands. In this case, some efficiency has been traded for the ability to adapt.
For this approach to work, the enterprise must be able to identify and respond to potential issues faster than the ecosystem changes. For example, consider increased patient flows that tax capacities beyond their designed limits. Designed and building of new or expanded facilities can take considerable time. On the other hand, reconfiguration of agile capacities should be much faster.
If the phenomena of interest are not very predictable and the enterprise has a limited ability to respond, it may be in the best interest of the enterprise to hedge its position. In this case, it can explore scenarios where the enterprise may not be able to handle sudden changes without prior investment. For example, an enterprise concerned about potential obsolescence of some lines of service may choose to invest in multiple, potential new services. Such investments might be pilot projects that enable learning how to deliver services differently or perhaps deliver different services.
Over time, it will become clear which of these options makes most sense, and the enterprise can exercise the best option by scaling up this line of service based on what they have learned during the pilot projects. In contrast, if the enterprise were to take a wait and see approach, it might not be able to respond quickly enough, and it might lose out to its competitors.
If the phenomena of interest are totally unpredictable and there is no viable way to respond, then the enterprise has no choice but to accept the risk. Accept is not so much a strategy as a default condition. If one is attempting to address a strategic challenge where there is little ability to optimize the efficacy of offerings, limited ability to adapt offerings, and no viable hedges against the uncertainties associated with these offerings, the enterprise must accept the conditions that emerge. Learning is still possible, however, as outlined below.
Table 2 considers these 4 strategies versus single‐loop and double‐loop learning. Within each strategy, examples of areas amenable to this strategy are listed. The examples within the optimize strategy are instances of operations research applied to hospitals. Optimizing such processes will enable single‐loop learning. In contrast, reengineering these processes before they are optimized would result in double‐loop learning. Careful consideration of the nature and design of processes provides deeper learning about the services being delivered.
Table 2.
Strategies versus single‐loop and double‐loop learning
| Single‐Loop Learning | Double‐Loop Learning | |
|---|---|---|
| Optimize | ||
| ▫ OR schedule | Current processes | Reengineered processes |
| ▫ Inventory | Current processes | Reengineered processes |
| ▫ Supply chains | Current processes | Reengineered processes |
| Adapt | ||
| ▫ Demand level | Increase/decrease capacities | Create agile capacities |
| ▫ Demand mix | Increase/decrease capacities | Create agile capacities |
| ▫ Inflation | Raise prices if possible | Increase process efficiencies |
| Hedge | ||
| ▫ Business models | Hedge most likely scenario | Create portfolio of hedges |
| ▫ Payment schemes | Hedge most likely scenario | Create portfolio of hedges |
| ▫ Innovation | Hedge primary opportunities | Create portfolio of hedges |
| Accept | ||
| ▫ Population trends | Project primary impacts | Develop causal model |
| ▫ Economic trends | Project primary impacts | Develop causal model |
| ▫ Social trends | Project primary impacts | Develop causal model |
The examples for the adapt strategy involve responding to exogenous forces. Single‐loop learning relates to deciding which capacities to increase or decrease, as well as pricing. Double‐loop learning focuses on the agility needed to reconfigure capacities in response to changes of demand levels or mixes. Double‐loop learning would also focus on steadily improving service efficiencies so that margins can be maintained despite inflation.
The hedge strategy examples relate to potentially disruptive exogenous changes. Payers, particularly the federal government, may dictate changes of payment schemes that force changes of business models. Competitors may offer market or technology innovations that threaten the enterprise market position in 1 or more service lines. Such possibilities can be hedged with investments in options that address the most likely scenarios of primary market or technology opportunities. This would enable single‐loop learning.
In contrast, the enterprise might develop scenarios of a range of potential futures, devise hedges for each of these futures, and invest in a portfolio of options. Not all of these futures would happen, so not all options would be exercised, but the enterprise would be prepared for almost any possibility. Interestingly, the options not exercised can sometimes be licensed to other enterprises where the option has value in their markets.39
The examples for the accept strategy focus on broad trends that the enterprise has to address but can only affect in a limited way. Single‐loop learning focuses on tracking these trends and projecting their primary impacts. Double‐loop learning would attempt to get ahead of these trends by developing causal models of the forces behind these trends. This would be particularly valuable for population health, for example, where understanding these forces might provide insights into new service line offerings needed.
There is another possibility that deserves mention—stay with the status quo. Yu, Rouse, and Serban67 developed a computational theory of enterprise transformation, elaborating on the qualitative theory presented earlier in this paper.6, 7 They used this computational theory to assess when investing in change is attractive and unattractive. Investing in transformation is likely to be attractive when one is currently underperforming and the circumstances are such that investments will likely improve enterprise performance. In contrast, if one is already performing well, investments in change will be difficult to justify. Similarly, if performance cannot be predictably improved—because of noisy markets and/or highly discriminating customers—then investments may not be warranted despite current underperformance. Consequently, double‐loop learning can be an unattractive investment.
Health care delivery is currently a very noisy market. Executives have told us that their biggest concern is uncertainty about the payment system in the United States. When will fee for service disappear? How will payment for outcomes be implemented? How will ACO, patient‐centered medical homes, and population health evolve and be financed? These uncertainties make investment decision making difficult and suggest that a bit of “wait and see” might be justified.
7. CONCLUSIONS
This paper has considered learning in the context of the transformation of the health care delivery enterprise. A framework for transformation was presented and elaborated in the context of health care delivery. We reviewed what is known about organizational learning, with particular emphasis on single‐loop versus double‐loop learning.
Three health care examples were used to illustrate this distinction—cancer, population health, and health IT. This led to a discussion of 4 strategies that the health care delivery enterprise can use to more effectively learn at all levels of the enterprise.
This overall line of reasoning suggests several important research issues. First, as articulated in Figure 1, the health care delivery enterprise involves much more than providers and payers. The ecosystem includes many issues beyond treating disease and paying for it. We need to improve our methods and tools for addressing the overall enterprise.
Research is also needed on better means for portraying consequences of decisions to the full range of stakeholders in the enterprise. Healthy people are more able to contribute to society, including working and paying taxes. Thus, investments in health yield significant returns, and the lowest cost health care delivery enterprise is very unlikely to yield the greatest returns.
Broader yet, an educated population will be a healthier population. Thus, population health cannot ignore education. In general, the overall goal should be a healthy, educated, and productive population that is competitive in the global marketplace. We need to better understand the available levers for achieving this goal and how to best portray the intricacies of the overall enterprise to motivate those who can pull these levers to do so.
Rouse WB, Johns MME, Pepe KM. Learning in the health care enterprise. Learn Health Sys. 2017;1:e10024 10.1002/lrh2.10024
REFERENCES
- 1. Rouse WB, Cortese DA. (Eds). Engineering the System of Healthcare Delivery. Amsterdam: IOS Press; 2010. [PubMed] [Google Scholar]
- 2. Rouse WB, Serban N. Understanding and Managing the Complexity of Healthcare. Cambridge, MA: MIT Press; 2014. [Google Scholar]
- 3. Rouse WB. Healthcare as a complex adaptive system: implications for design and management. Bridge. 2008;38(1):17‐25. [Google Scholar]
- 4. Basole RC, Rouse WB. Complexity of service value networks: conceptualization and empirical investigation. IBM Syst J. 2008;47(1):53‐70. [Google Scholar]
- 5. Yu Z, Rouse WB, Serban N, Veral E. A data‐rich agent‐based decision support model for hospital consolidation. J Enterp Transform. 2016;6(3/4):136‐161. [Google Scholar]
- 6. Rouse WB. A theory of enterprise transformation. J Syst Eng. 2005;8(4):279‐295. [Google Scholar]
- 7. Rouse WB. (Ed). Enterprise Transformation: Understanding and Enabling Fundamental Change. Hoboken, NJ: John Wiley; 2006. [Google Scholar]
- 8. Rouse WB. Essential Challenges of Strategic Management. New York: John Wiley; 2001. [Google Scholar]
- 9. Rouse WB. People and Organizations: Explorations of Human‐Centered Design. Hoboken, NJ: John Wiley; 2007. [Google Scholar]
- 10. Wright TP. Factors affecting the cost of airplanes. J Aerosol Sci. 1936;3(4):122‐128. [Google Scholar]
- 11. Epple D, Argote L, Devadas R. Organizational learning curves: a method for investigating intra‐plant transfer of knowledge acquired through learning by doing. Organ Sci. 1991;2(1):58‐70. [Google Scholar]
- 12. Deming WE. Out of Crisis. Cambridge, MA: MIT Press; 1986. [Google Scholar]
- 13. Davenport TH, Short JE. The new industrial engineering: information technology and business process redesign. Sloan Manage Rev. 1990;31(4):11‐27. [Google Scholar]
- 14. Zangwill WI, Kantor PB. Toward a theory of continuous improvement and the learning curve. Manag Sci. 1998;44(7):910‐920. [Google Scholar]
- 15. Andreu R, Ciborra C. Organizational learning and core capabilities development: the role of IT. J Strateg Inf Syst. 1996;5(2):111‐127. [Google Scholar]
- 16. Belmonte RW, Murray RJ. Getting ready for strategic change: surviving business process redesign. Inf Syst Manag. 1993;10(3):23‐29. [Google Scholar]
- 17. Adams ME, Day GS, Dougherty D. Enhancing new product development performance: an organizational learning perspective. J Prod Innov Manag. 1998;15(5):403‐422. [Google Scholar]
- 18. Amit R, Schoemaker P. Strategic assets and organizational rent. Strateg Manag J. 1993;14(1):33‐46. [Google Scholar]
- 19. Simon HA. Rational choice and the structure of the environment. Psychol Rev. 1956;63(2):129‐138. [DOI] [PubMed] [Google Scholar]
- 20. Borras S. Policy learning and organizational capacities in innovation policies. Sci Public Policy. 2011;38(9):725‐734. [Google Scholar]
- 21. Levitt B, March JG. Organizational learning. Annu Rev Sociol. 1988;14:319‐340. [Google Scholar]
- 22. Nelson RR, Winter SG. Evolutionary theorizing in economics. J Econ Perspect. 2002;16(2):23‐46. [Google Scholar]
- 23. Cohen W, Levinthal D. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q. 1990;35(1):128‐152. [Google Scholar]
- 24. Siegel S. Level of aspiration and decision making. Psychol Rev. 1957;64(4):253. [DOI] [PubMed] [Google Scholar]
- 25. Simon HA. A behavioral model of rational choice. Q J Econ. 1955;69:99‐118. [Google Scholar]
- 26. Senge PM. The Fifth Discipline: The Art and Practice of the Learning Organization. New York: Doubleday Business; 1990. [Google Scholar]
- 27. Shrivastava P. A typology of organizational learning systems. J Manag Stud. 1983;20(1):7‐28. [Google Scholar]
- 28. Crossan MM, Lane HW, White RE. An organizational learning framework: from intuition to institution. Acad Manage Rev. 1999;24(3):522‐537. [Google Scholar]
- 29. Bontis N, Crossan MM, Hulland J. Managing an organizational learning system by aligning stocks and flows. J Manag Stud. 2002;39(4):437‐469. [Google Scholar]
- 30. Caldwell R. Systems thinking, organizational change, and agency: a practice theory critique of Senge's learning organization. J Chang Manag. 2012;12(2):145‐164. [Google Scholar]
- 31. Giddens A. The Constitution of Society: Outline of the Theory of Structuation. Berkeley, CA: University of California Press; 1984. [Google Scholar]
- 32. March JG. Exploration and exploitation in organizational learning. Organ Sci. 1991;2(1):71‐87. [Google Scholar]
- 33. Weick K. Sensemaking in Organizations. London: Sage; 1995. [Google Scholar]
- 34. Valiant LG. A theory of the learnable. Proceedings of the 16th ACM Symposium on Theory of Computing, 1984; Washington, DC, 436–445.
- 35. Valiant L. Probably Approximately Correct: Nature's Algorithms for Learning and Prospering in a Complex World. New York: Basic Books; 2013. [Google Scholar]
- 36. Argyris C. Teaching smart people how to learn. Harv Bus Rev. 1991;69(3):99‐109. [Google Scholar]
- 37. Drucker PF. Managing for business effectiveness. Harv Bus Rev. 1963;41(3):53‐60. [Google Scholar]
- 38. Boer FP. The Valuation of Technology: Business and Financial Issues in R&D. New York: John Wiley; 1999. [Google Scholar]
- 39. Rouse WB, Boff KR. Value‐centered R&D organizations: ten principles for characterizing, assessing & managing value. Syst Eng. 2004;7(2):167‐185. [Google Scholar]
- 40. Hammer M, Champy J. Reengineering the Corporation: Manifesto for Business Revolution. New York: HarperCollins; 2009. [Google Scholar]
- 41. Gawande A. Being Mortal: Medicine and What Matters in the End. New York: Metropolitan; 2014. [Google Scholar]
- 42. Mukherjee S. The Emperor of All Maladies: A Biography of Cancer. New York: Scribner; 2010. [Google Scholar]
- 43. Mukherjee S. The improvisational oncologist. New York Times Sunday Magazine, 2016a; May 15, 43–45.
- 44. Mukherjee S. The Gene: An Intimate History. New York: Scribner; 2016b. [Google Scholar]
- 45. Grady D. Harnessing the immune system to fight cancer. New York Times, 2016; July 30.
- 46. Economist . Cancer treatment: on target. The Economist, 2016; June 11.
- 47. CMS . Shared Savings and Losses and Assignment Methodology: Version 4, December. Baltimore, MD: Centers for Medicare and Medicaid Services; 2015. [Google Scholar]
- 48. Wyman . ACO Update: Accountable Care at a Tipping Point. New York: Oliver Wyman; 2014. [Google Scholar]
- 49. Schulman KA, Richman BD. Reassessing ACOs and health care reform. JAMA. 2016;316(7):707‐708. [DOI] [PubMed] [Google Scholar]
- 50. Burwell SM. Setting value‐based payment goals—HHS efforts to improve US health care. N Engl J Med. 2015;372(10):897‐899. [DOI] [PubMed] [Google Scholar]
- 51. Wen LS. A new vision of true health. Consumer Reports, 2016. http://www.consumerreports.org/health/new‐vision‐of‐true‐health/. [PubMed]
- 52. Kindig D, Stoddart G. What is population health? Am J Public Health. 2003;93(3):380‐383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shortell SM, Casalino LP. Healthcare reform requires accountable care systems. JAMA. 2008;300(1):95‐97. [DOI] [PubMed] [Google Scholar]
- 54. Galea S, Tracy M, Hoggatt KJ, DiMaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101(8):1456‐1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cooper R. Poverty and the Myths of Health Care Reform. Baltimore, MD: Johns Hopkins University Press; 2016. [Google Scholar]
- 56. Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Commission on Social Determinants of Health . Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661‐1669. [DOI] [PubMed] [Google Scholar]
- 57. Radley DC, Schoen C. Geographic variation in access to care—the relationship with quality. N Engl J Med. 2012;367(1):3‐6. [DOI] [PubMed] [Google Scholar]
- 58. Casalino LP, Erb N, Joshi MS, Shortell SM. Accountable Care Organizations and Population Health Organizations. J Health Polit Policy Law. 2015;40(4):819‐835. [DOI] [PubMed] [Google Scholar]
- 59. Curran JW. Social Determinants of Health in the United States: Roles and Limitations of the Academic Health Center. Atlanta, GA: Emory University, Rollins School of Public Health; 2013. [Google Scholar]
- 60. Johns MME, Lewin JS, Jain SH. One path to value‐based care for academic health centers. N Engl J Med Catal. 2016. doi: 10.1056/NEJMe1515517 [DOI] [Google Scholar]
- 61. IOM . Integrating Research and Practice: Health System Leaders Working Toward High‐Value Care. Washington, DC: National Academy Press; 2015. [PubMed] [Google Scholar]
- 62. ONC . Connecting Health and Care for the Nation: A Shared Nationwide Interoperability Roadmap. Washington, DC: Office of the National Coordinator for Health Information Technology; 2015. [Google Scholar]
- 63. Stead WW. Delivering on the promise to reduce the cost of healthcare with electronic health records In: Pate‐Cornell E, Rouse WB, Vest CM, eds. Perspectives on Complex Global Challenges: Education, Energy, Healthcare, Security, and Resilience. Hoboken, NJ: John Wiley; 2016. [Google Scholar]
- 64. Bothwell LE, Podolsky SH. The emergence of the randomized, controlled trial. N Engl J Med. 2016;375(6):501‐504. [DOI] [PubMed] [Google Scholar]
- 65. Bohnsack J. How big data can help healthcare providers manage risk. Health IT & CIO Review, 2013; May 22.
- 66. Pennock MJ, Rouse WB. The epistemology of enterprises. Syst Eng. 2016;19(1):24‐43. [Google Scholar]
- 67. Yu X, Rouse WB, Serban N. A computational theory of enterprise transformation. J Syst Eng. 2011;14(4):441‐454. [Google Scholar]


