Abstract
Functional knee-braces are widely used to protect injured or reconstructed anterior cruciate ligaments, despite the fact that few scientific data support their efficacy. We studied seven functional braces, representative of both the typical custom-fit and off-the-shelf designs. The braces were tested on subjects who had a normal anterior cruciate ligament and were scheduled for arthroscopic meniscectomy or exploration of the knee under local anesthesia. After the operative procedure, a Hall-effect strain-transducer was applied to the anterior cruciate ligament. Under low anterior shear loads, two braces provided some protective strain-shielding effect compared with no brace, but this strain-shielding effect did not occur at the higher anterior shear loads expected during the high-stress activities common to athletic events. The DonJoy, Townsend, C.Ti., and Lenox Hill braces demonstrated a strain-shielding effect on the anterior cruciate ligament with an internal torque of five newton-meters applied to the tibia.
None of the braces had any effect on strain on the anterior cruciate ligament during active range of motion of the knee from 10 to 120 degrees or during isometric contraction of the quadriceps. Wearing of a brace did not produce an increase in the value for strain on the anterior cruciate ligament. For the activities that Were evaluated in this study, none of the braces produced adverse effects on the anterior cruciate ligament, and there were no significant differences in the strain on the anterior cruciate ligament between the use of a custom-fit or an off-the-shelf brace design. There were no apparent advantages of the more expensive custom-made braces compared with the off-the-shelf designs.
The sports-medicine community has developed an acceptance of functional knee-braces as a means to treat instability of the knee due to injury of the anterior cruciate ligament1,13,15,19–21,35,36,42,43,45,46,48–50,53,58. Functional braces are designed to facilitate normal kinematics of the tibiofemoral joint while limiting abnormal displacements and loading that might detrimentally strain an injured ligament or a reconstructed replacement or might cause abnormal tibiofemoral subluxations in a knee that has a tom anterior cruciate ligament. The extent to which a functional brace can produce these results is unclear at best. This may be attributed to the difficulty of a direct evaluation of a knee-brace by measurement of tibiofemoral kinematics or ligamentous biomechanics in the in vivo environment under controlled experimental conditions. Cawley et al. recently published a comprehensive review of the literature regarding functional bracing of the knee and called for investigations to validate designs of knee-braces12.
After reconstruction of the anterior cruciate ligament, with its goal of restoration of the normal kinematics of the joint, functional bracing has frequently been used as an augmentation to treatment. Functional knee-braces have been commonly worn by athletes shortly after an operative procedure, as well as during the later stages of recovery after a return to vigorous activities. Braces also are prescribed for athletes who have a sprain of a ligament or for patients in the younger and older age-groups who may not be prime candidates for procedures designed to reconstruct ligaments. Evidence suggests that a brace has a beneficial effect; it protects healing or damaged tissues and may possibly prevent reinjury7,41,46,58. However, recent biomechanical investigations have demonstrated that the application of a functional knee-brace to a knee that has a torn anterior cruciate ligament is effective in the control of abnormal anterior translation of the tibia only at low anterior shear-load conditions and not during the high loads seen during vigorous activity8,11,13,14,61. Furthermore, clinical studies have demonstrated that giving-way of the knee can occur while a brace is worn13,14. Tegner and Lorentzon retrospectively studied the rate and type of injuries to the knee among elite Swedish ice-hockey players and related these data to the use of functional knee-braces56. They demonstrated that even when a functional brace was worn, serious injuries occurred to the ligaments of the knee in athletes who had had no prior injury to the knee, as well as in athletes who had had an injury to the knee but were completely rehabilitated.
Previous studies of functional bracing have reported improvement as subjectively rated by the patient or by indirect measurement of function of the anterior cruciate ligament with an arthrometer. These indirect biomechanical measurements of function have added to the controversy concerning the efficacy of functional braces. No previous studies have measured directly, in vivo, the strain-shielding effects provided by functional braces.
Baker et al.5 used a direct approach to investigate the ligaments of the knee during functional bracing by the application of force-transducers to the anterior cruciate and medial collateral ligaments. The tests were performed on the knees of human cadavera, under a controlled valgus force, with and without a functional brace. They found no apparent difference between forces on the anterior cruciate ligament with or without a brace at both 15 and 30 degrees of flexion of the knee5. In addition, they observed an increase in load on the anterior cruciate ligament when a brace was applied to the knee, and described this as pre-loading of the anterior cruciate ligament.
We also have made direct measurements by the application of the Hall-effect strain-transducer (Micro Strain, Burlington, Vermont) to the anterior cruciate ligament in braced and unbraced knees in cadavera3. That study suggested that bracing does not protect the anterior cruciate ligament when anterior shear loads are applied across the tibiofemoral joint. Instead, strain on the anterior cruciate ligament was increased when the knee was braced in all positions from 0 to 90 degrees of flexion. These findings suggested that a brace may cause anterior displacement of the tibia that increases the strain on the anterior cruciate ligament. Cadaver models, however, are limited by the lack of active musculature and the changes in the compliance of soft tissues surrounding the thigh and calf that have been shown to affect the strain on the anterior cruciate ligament9,23,25. The amount and sequence of contraction of the muscles also alter the stiffness of the interface between the brace and the soft tissue of the leg18. Muscular contraction is not present in studies on cadavera, so it is not possible to reproduce this interface.
A review of the literature revealed no direct objective in vivo evidence suggesting that a functional knee-brace, externally attached to the soft tissues surrounding the knee, can control tibiofemoral motion to the extent that the cruciate ligaments are protected and abnormal tibiofemoral translations and rotations are prevented. The purpose of this study was to quantify the strain on the anterior cruciate ligament, in the presence of normal muscular function, when known loads were applied to a knee fitted with a functional knee-brace and then to determine if bracing altered that strain detrimentally or beneficially. This was accomplished by the temporary arthroscopic implantation of a transducer into the normal anterior cruciate ligament of volunteers9. The values for the strain on the anterior cruciate ligament that were calculated with and without a brace were then compared in each subject. Strain was measured during activities that are commonly encountered in rehabilitation programs after reconstruction of the anterior cruciate ligament.
The specific aims of this study were to determine (1) if functional bracing produces a deleterious increase in strain on the anterior cruciate ligament, (2) if bracing can protect the anterior cruciate ligament from strain when different loads are applied to the knee, and (3) if different braces perform differently on the basis of their effects on the strain patterns in the anterior cruciate ligament. We believe that our investigation is the first attempt to accomplish this task.
Materials and Methods
Braces
Seven functional braces were tested: three custom-fit designs and four off-the-shelf designs. The three custom braces included the C.Ti. Standard with the anterior cruciate ligament cable system (Innovation Sports, Irvine, California), the Lenox Hill derotation brace (Lenox Hill Brace Shop, New York, N.Y.), and the Townsend knee-brace (Townsend Industries, Bakersfield, California). The C.Ti. Standard and Townsend braces incorporate a hinge, post, and shell designed to accommodate the anatomical motion of the knee; the Lenox Hill derotation brace has a pinned hinge, post, and strap design. The four off-the-shelf braces were the DonJoy 4-point Sport ACL brace with anterior cruciate-ligament accessory strap (DonJoy, Carlsbad, California), the 3D dynamic functional knee-brace (3D Orthopaedic, Dallas, Texas), the Bledsoe Sports Rehab brace (Medical Technology, Grand Prairie, Texas), and the Lerman Multi-Lig II brace (United States Manufacturing, Pasadena, California). The DonJoy brace and the Lerman Multi-Lig II brace both have polycentric knee hinges, double upright supports, and a strap-attachment design. The 3D brace has a single medial upright post, hinge, and strap attachment. The Bledsoe brace was designed as a rehabilitative brace as well as an economical alternative to functional braces during non-contact sports. This brace has a hinge, bilateral post, and strap-attachment design.
All custom braces were templated, fitted, and applied by a licensed orthotist according to the manufacturer’s specifications. The off-the-shelf braces were sized, fitted, and applied by one of us (C. M. W.), as instructed by a representative of the company for each brace.
Transducer
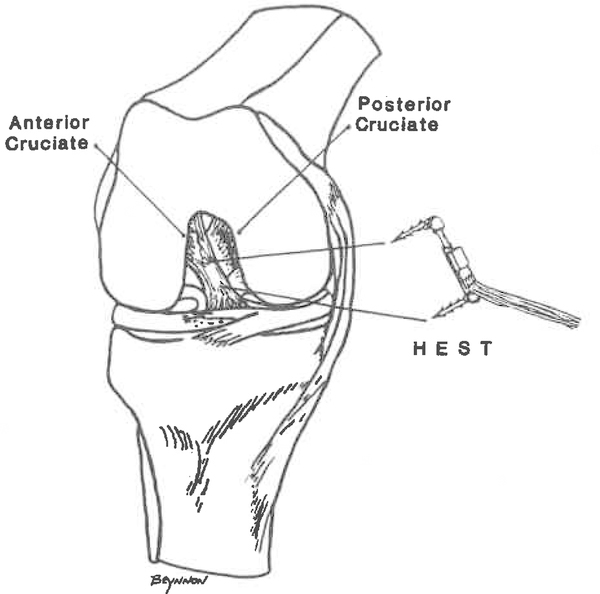
We used the Hall-effect strain-transducer adapted for this in vivo application (Fig. 1). The Hall-effect transducer is capable of the measurement of displacement in the in vivo environment of the ligament and has the sensitivity for the measurement of displacement within small segments of the ligament, thus enabling characterization of strain behavior of the mid-substance of the anterior cruciate ligament. The transducer is arthroscopically implantable. We previously described the current configuration of the transducer, the technique of implantation, and the procedure to measure strain in vivo9,23. The specifications of the Hall-effect transducer were reported by Arms2.
Fig. 1.
Orientation of the implantation of the Hall-effect strain-transducer (HEST) (Micro Strain) on the anteromedial aspect of the anterior cruciate ligament.
Human Subjects
The subjects who were used for analysis of the data were thirteen healthy men, ranging in age from twenty-six to thirty-nine years. All were candidates for diagnostic arthroscopy or arthroscopic partial meniscectomy (Table I). The anterior cruciate ligament and other structures in the knee were carefully inspected for abnormalities. We excluded potential subjects who had clinically detectable instability of any of the four major ligaments of the knee (anterior cruciate, posterior cruciate, medial collateral, or lateral collateral), cardiovascular problems, or any debilitating disease, or who had had previous operations on the knee. Potential subjects were also excluded if they had any form of arthritis or other condition that would affect the normal kinematics or stability of the knee. All subjects had a normal anterior cruciate ligament on clinical and arthroscopic examination. For each subject, the range of motion of the knee and gait pattern were normal at the preoperative visit (Table I). Great care was taken to ensure complete protection for the subjects. Approval from the Institutional Review Board was obtained for the study, full informed consent was given by each participant, and there was no monetary compensation. The operations and experimental procedures were performed under local anesthesia (a mixture of bupivacaine [Marcaine] and chloroprocaine [Nesacaine]), allowing all subjects control of the muscles of the lower extremities during the procedure. An extra forty-five to sixty minutes was needed to perform the experiment, and this did not constitute a notable risk to the subject. No additional cost was incurred by the subject. A minor intraoperative complication occurred in one subject when the Hall-effect transducer broke at the time of removal; additional operative time and exposure to radiation were needed to remove all components of the transducer. No postoperative complications occurred in any subject.
TABLE I.
Clinical Data on the Thirteen Subjects Included in the Analysis of Data
| Subject | Age (Yrs.) | Preoperative Diagnosis* | Arthroscopic Procedure | Outcome |
|---|---|---|---|---|
| 1 | 26 | 2-yr. history of knee locking, medial meniscal tear (L) | Partial medial meniscec. | No complicqt., full return to activity |
| 2 | 28 | 4-yr. history of symptoms, probable meniscal tear (L) | Partial medial meniscec. | No complicat., full return to activity |
| 3 | 28 | Ganglion in quadriceps tendon (R) | Excision of ganglion | No complicat., full return to activity |
| 4 | 37 | Medial meniscal tear (R) | Partial medial meniscec. | No complicat., full return to activity |
| 5 | 35 | Medial meniscal tear (R) | Partial medial meniscec. | No complicat., full return to activity |
| 6 | 36 | Medial meniscal tear (R) | Partial medial meniscec. | No complicat., full return to activity |
| 7 | 34 | Medial meniscal tear (L) | Partial medial meniscec. | No complicat., full return to activity |
| 8 | 35 | Medial meniscal tear (L) | Partial medial meniscec. | No complicat., full return to activity |
| 9 | 36 | Lateral meniscal tear (L) | Partial lateral meniscec. | Lost to follow-up |
| 10 | 28 | Possible meniscal injury (R) | Débridement of fat pad | No complicat., full return to activity |
| 11 | 37 | 1.5-yr. history of knee pain, probable meniscal tear (L) | Partial medial meniscec. | Lost to follow-up |
| 12 | 38 | Probable meniscal tear (L) | Partial medial meniscec. | No complicat., full return to activity |
| 13 | 39 | Probable medial meniscal tear (L) | Partial medial meniscec. | Lost to follow-up |
Preoperatively, all subjects had normal gait and a range of motion similar to that of the normal, contralateral knee.
Experimental Procedure
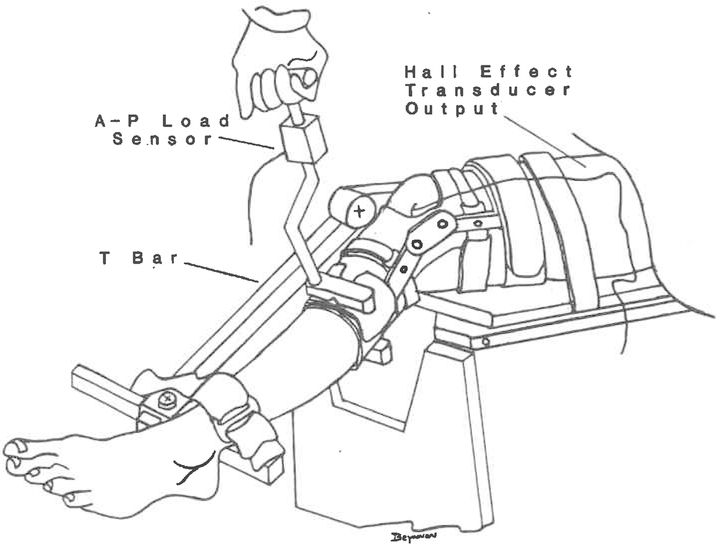
After the scheduled operation was completed, the Hall-effect transducer was implanted by the technique previously described by our group9,23. The subject was then positioned in a seated posture on the end of a modified operating-table. The femur was oriented in the horizontal plane and was secured with a Velcro strap to prevent elevation of the thigh, and the tibia was allowed to hang off the end of the table. The distal aspect of the tibia was strapped to an adjustable T-bar which could be positioned at any angle of flexion (Fig. 2).
Fig. 2.
Anterior-posterior shear load applied with the knee in 30 degrees of flexion and use of the Lerman Multi-Lig II brace (United States Manufacturing).
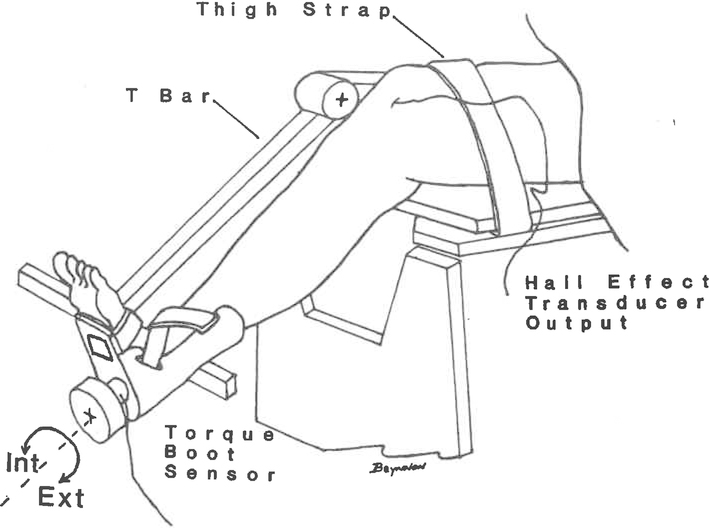
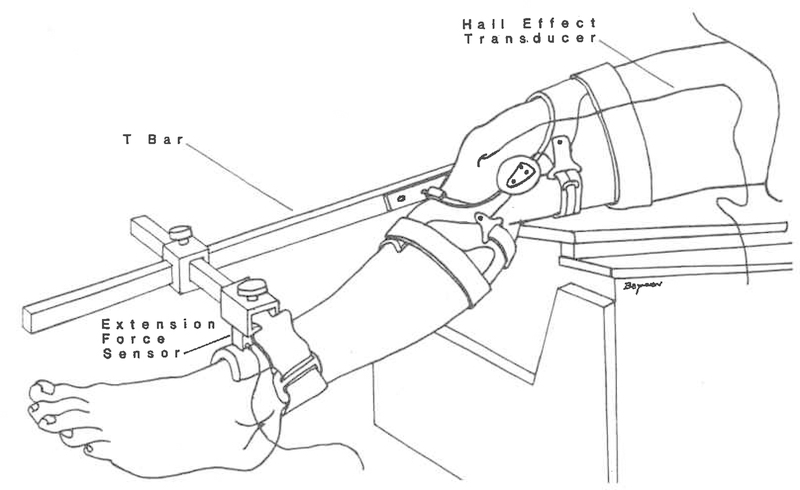
The electrogoniometer portion of the Knee Signature System (Acufex Microsurgical, Norwood, Massachusetts) was placed on the subject’s limb, providing continuous measurement of flexion-extension and internal-external rotation of the knee. A custom device was developed with a load-transducer to allow the application of measured anterior-posterior shear loads to the proximal part of the tibia in a cyclic manner (Fig. 2). This device was known as the anterior-posterior load-transducer. A boot that had an instrumented torque-transducer also was developed to allow the application of measured internal and external torque about the long axis of the tibia (Fig. 3). This device was designed to grip the foot and ankle, along with the distal aspect of the tibia, and was known as the torque boot transducer. A load transducer was developed to measure the extension force produced by the subject’s isometric quadriceps-extension effort. This device was mounted on the T-bar and was designed with adjustments to allow attachment to the anterior aspect of the distal part of the tibia (Fig. 4). This device was called the extension force transducer. The output from the Hall-effect transducer, electrogoniometer, and anterior-posterior load, torque boot, and extension force transducers was transferred to a data-acquisition board (Techmar, Cleveland, Ohio) for analog-to-digital conversion at a frequency of ten hertz.
Fig. 3.
Internal-external torque applied to the tibia with the knee in 30 degrees of flexion.
Fig. 4.
Isometric contraction of the quadriceps performed with the knee in 30 degrees of flexion and the use of the C.Ti. brace (Innovation Sports).
As data were sampled, they were simultaneously stored on a computer. In addition, data on displacement of the anterior cruciate ligament that were obtained from the Hall-effect transducer also were recorded on an X-Y plotter for independent feedback during the experimental procedure.
The experimental protocol consisted of four different loading activities: (1) anterior-posterior shear loading at 30 degrees of flexion of the knee (Lachman test57), (2) internal and external torque applied to the tibia with the knee flexed 30 degrees, (3) isometric contraction of the quadriceps with the knee flexed 30 degrees, and (4) active flexion-extension movement of the lower limb from 5 to 110 degrees. These activities were chosen because they are commonly encountered in rehabilitation programs for reconstruction of the anterior cruciate ligament and produce joint loads that strain the anterior cruciate ligament9 or its replacement.
Anterior-Posterior Shear Loading
The anterior-posterior load-transducer was used to apply measured loads to the tibia (Fig. 2). The load-cell was positioned in a transverse plane directed through the middle of the tibial tuberosity, and the subject was instructed to relax all muscles of the lower extremity. Shear loading was then applied in four alternate cycles to the limit of ± 200 newtons. Data from the Hall-effect transducer and the anterior-posterior load-transducer were recorded simultaneously while the shear load was applied to the tibia. Shear loading was applied by the same one of us (C. M. W.) throughout all experimental procedures.
The Hall-effect transducer measures displacement, enabling the calculation of strain on the anteromedial bundle of the anterior cruciate ligament. Depending on the magnitude and the direction of the applied tibiofemoral shear load, the anteromedial bundle may be in a strained or an unstrained state. Calculation of strain can differentiate between the two states through the use of a reference based on the strained-unstrained transition state of the anteromedial bundle9. The anterior-posterior shear-loading activity with the knee in 30 degrees of flexion was done to determine an appropriate reference to differentiate between strained and unstrained states of the ligament. This was performed to allow comparisons of the values for strain on the anteromedial bundle when the ligament was in a strained state rather than an unstrained state, in which this portion of the ligament is slack and is not a kinematic restraint to tibiofemoral motion.
Internal and External Torques of the Tibia
The torque boot was strapped on the subject’s foot (Fig. 3), and the thigh remained secured to the seat while the distal strap was released to allow free rotation of the tibia. The subject was instructed to relax all muscles of the lower extremity while four cycles of internal and external torques of at least five newton-meters were applied alternately. Internal and external torques were applied by the same one of us (C. M. W.) throughout all experimental procedures. Data from the Hall-effect transducer and the torque boot transducer, and corresponding tibiofemoral rotations, were simultaneously recorded while torque was applied to the tibia.
Isometric Contraction of the Quadriceps
With the femur secured in the horizontal plane, the distal part of the tibia was positioned and secured at 30 degrees of flexion of the knee. The extension force transducer was positioned in front of the distal part of the tibia, immediately superior to the malleoli (Fig. 4). The distance from the joint line of the knee to the center of the extension force transducer was measured with a hand-held tape and was recorded. This distance was used as the moment-arm in the calculation of extension torque. The subject was then instructed to contract the quadriceps and extend the leg against the sensor four times, with approximately 80 per cent of maximum effort. Data from the Hall-effect and extension force transducers were simultaneously recorded while the subject performed the extension efforts.
Active Range of Flexion-Extension of the Knee
The subject remained upright and seated, with the thigh strapped to the operating-table. The T-bar was secured so as not to interfere with the tibia during flexion-extension of the knee. For active range of motion, the subject was instructed to extend and flex the lower limb in a cyclic pattern between the limits of 5 and 110 degrees of flexion. Full extension was avoided to prevent impingement of the gauge against the roof of the femoral intercondylar notch. Four continuous cycles of data from the Hall-effect transducer and electrogoniometer were simultaneously recorded while the subject actively extended the knee.
Each subject went through the following test protocol. First, all four loading activities were performed without a brace on the knee, and the four activities then were repeated after a brace had been applied. Next, anterior-posterior shear loading and active range of motion of the knee (again each with four cycles) were repeated, without a brace, as a means to assess the reproducibility of the measurements with the Hall-effect transducer. A different brace was applied, the four loading activities were done again, and then the tests were repeated without a brace. When time permitted, we were able to evaluate three braces on a subject. For each loading activity, this experimental design facilitated three comparisons of values for strain on the anterior cruciate ligament: comparisons of repeated tests on a knee without a brace, comparisons between testing of each brace and testing without a brace, and an over-all comparison among braces. A random number table was used to assign the type of brace to be used and the order of evaluation of the brace for all of the subjects in the study.
Statistical Analysis
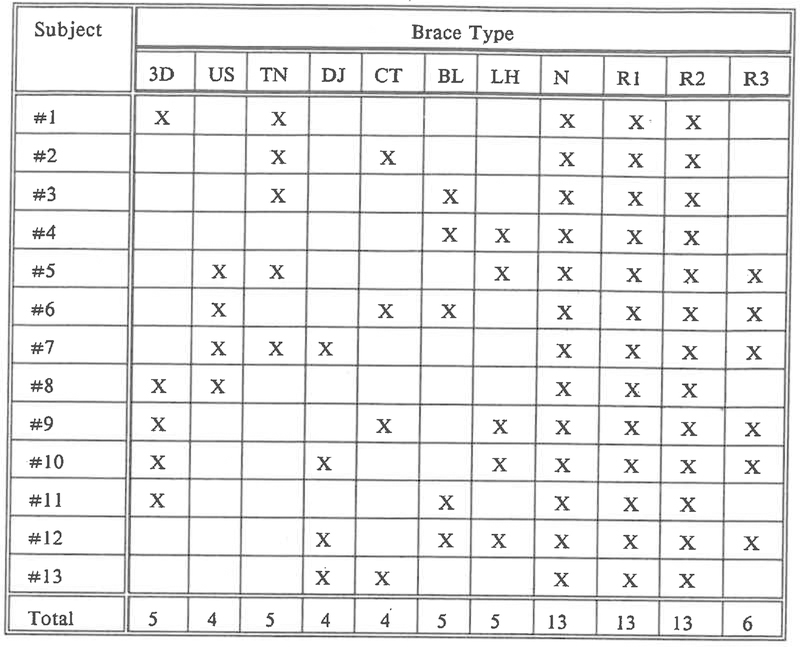
Because the time in the operating room was limited, only two or three of the seven braces were tested on each subject. Therefore, our study was structured originally as a balanced incomplete block design, with the braces considered as treatments and the subjects as blocks. The actual experimental design (Fig. 5) is not balanced because of the various number of braces per subject and the loss of some subjects.
Fig. 5.
Incomplete block experimental design for the study. The results for thirteen of twenty-seven potential subjects were included in the analysis of the data. Seven were excluded because of technical failure, and another seven were not included because of inconsistent measurements during repeated testing without a brace (caused by impingement of the Hall-effect strain-transducer as the knee was brought into full extension (0 degree). 3D = 3D dynamic functional knee-brace (3D Orthopaedic), US = Lerman Multi-Lig II brace (United States Manufacturing), TN = Townsend brace (Townsend Industries), DJ = DonJoy 4-point Sport ACL brace (DonJoy), CT = C.Ti. brace with ACL cable system (Innovation Sports), BL = Bledsoe Sports Rehab brace (Medical Technology), and LH = Lenox Hill derotation brace (Lenox Hill Brace Shop). N = normal test (without a brace), R1 = first repeated test, R2 = second repeated test, and R3 = third repeated test.
For each loading activity, the average results for strain in the four cycles were used for statistical analysis. For each subject and for each loading activity on a knee with a brace, the results of the repeated testing without a brace were compared with the results of the original testing without a brace through a difference of the values for strain. Unusually large differences between results for original and repeated tests without a brace were considered as evidence of non-reproducibility of the results that were obtained with the Hall-effect transducer, and the associated results of tests with a brace were not used. Non-reproducible behavior was found to be caused by mechanical impingement of the Hall-effect transducer against the roof of the femoral intracondylar notch as the knee was brought into full extension. This occurred in the first seven subjects and was eliminated when the subjects were instructed to extend the knee to nearly full extension (approximately 5 degrees). In another seven subjects, moisture in the electrical connection of the Hall-effect transducer caused technical failure. The results in subjects who had data that were non-reproducible or in whom there was a technical failure were not included in the analysis.
A two-way analysis of variance by braces and subjects was performed on the differences in strain between testing with and without a brace — in particular, at forty, 100, and 180 newtons for anterior shear loading, at five newton-meters for internal and external torques, at thirty newton-meters of extension torque for isometric contraction of the quadriceps, and at 20 degrees of flexion during active range of motion (chosen because this was the angle of the knee that yielded the maximum strain for this activity) — as well as on the valid data on differences between repeated tests without a brace, to confirm that there were no systematic differences. Within each brace, the differenced results were plotted to check consistency and then were checked by paired t tests to confirm centering at zero. All statistical analyses were performed with the SAS system54.
For each loading activity, differences in values for strain between testing with and without a brace were calculated for further statistical analysis, because a zero difference indicates no effect from the brace, a negative difference shows a protective strain-shielding by the brace, and a positive difference shows a deleterious increase in strain on the anterior cruciate ligament. Differences were used to provide controlled comparisons within each subject. In the case of anterior shear loading, a three-factor analysis of variance was performed for the series of loads (zero, ten, twenty(twenty) ... 200 newtons) for all subjects and braces. Also, the Tukey multiple-comparisons method was used to contrast average differences among each of the braces. At the loads of forty, 100, and 180 newtons, the over-all mean difference was tested for centering at zero with use of the t test as described by Searle55, and a two-way analysis of variance was used to compare braces.
Similar analyses were done for selected levels of internal torque (+5 newton-meters) and external torque (−5 newton-meters), at thirty newton-meters of extension torque for isometric contraction of the quadriceps, and at 20 degrees of extension of the knee during active range of motion, in order to test for significant differences in strain (from zero) (with the t test described by Searle55) for all braces.
For all loading activities, the differences in values for strain were plotted on a graph by brace across the tested range of zero to 200 newtons of anterior shear load, +10 to −10 newton-meters for internal and external torque respectively, zero to eighty newton-meters of extension torque for isometric contraction of the quadriceps, and 5 to 100 degrees of extension of the knee in active range of motion (although particular subjects may not have been tested to the full ranges indicated). This allowed a check for consistency among subjects for each brace and for a comparison among braces after averaging across the subjects who wore particular braces. Paired t tests were used at a series of loads, torques, and positions of the knee to check for significant effects of each individual brace on strain on the anteromedial bundle.
Results
Anterior Shear Loading
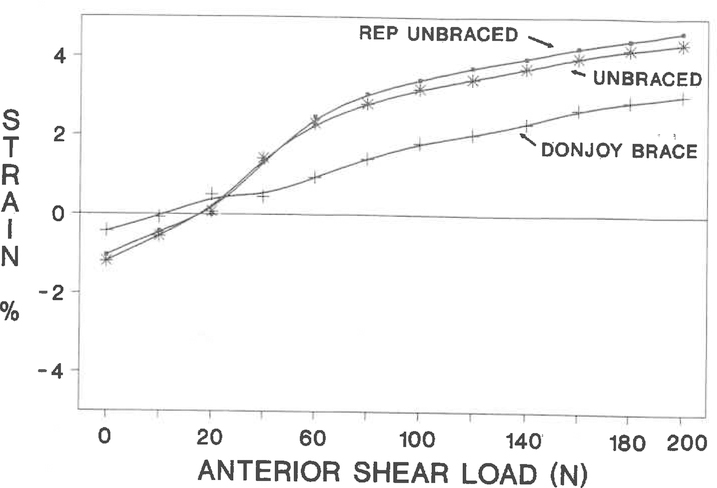
For each subject who was included in the analysis of the data, the anterior shear-loading activity produced similar values for strain on the anterior cruciate ligament for initial and repeated testing without a brace, and some of the functional knee-braces decreased the values for strain at low anterior shear loads (Fig. 6). The most effective means of describing the effect of each brace on the pattern of strain on the anteromedial bundle was to plot the mean difference in strain, calculated as the difference between testing with and without a brace, along with the corresponding 95 per cent confidence levels for all of the subjects at selected levels of load or position of the knee (Fig. 7). If the mean difference in strain was along the zero line, then a knee-brace did not produce an effect on the strain on the anterior cruciate ligament. Negative differences indicated protective strain-shielding by the brace and positive differences, a deleterious increase in strain on the anterior cruciate ligament. A two-way analysis of variance by subjects and braces was done with use of the differences between initial and repeated tests without a brace at selected loads (forty, 100, and 180 newtons) to ensure that there were no systematic differences by brace or for certain subjects for the repeated tests; no statistically significant differences were noted. The other checks on the repeated testing without a brace (detailed in the Materials and Methods section) also revealed no significant differences in the repetition.
Fig. 6.
Results from anterior shear loading applied with the knee in 30 degrees of flexion. The percentage of strain is plotted against anterior shear load (in newtons). Tue mean values for strain, averaged across four loading cycles, for testing without a brace and with the DonJoy brace, and for repeated testing without a brace. REP = repeated.
Fig. 7.
The mean difference in values for strain (with the convention of strain for testing with a brace. minus strain for testing without a brace) at selected shear loads for the DonJoy brace. Tue 95 per cent confidence limits are included.
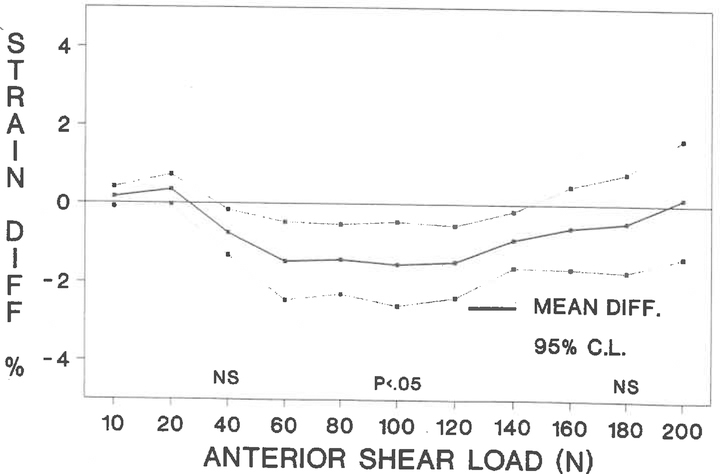
In order to compare all braces across the entire range of loads, a three-way analysis of variance by brace, subject, and load level (zero, ten, twenty(twenty) ... 180 newtons) was performed on the differences in the strain between testing with and without a brace. No significant interaction of braces with load level was found (p > 0.05), although no brace had an effect on strain on the anterior cruciate ligament until after a twenty-newton load, and then some braces appeared to have greater strain-shielding effects than others (Fig. 8).
Fig. 8.
The mean difference in values for strain across subjects (with the convention of strain for testing with a brace minus strain for testing without a brace) for anterior shear loading with the knee in 30 degrees of flexion for all seven braces. The differences were used to provide controlled comparisons of values for strain in each subject. A zero difference indicates no effect by the brace, a negative difference shows a protective strain-shielding by the brace, and a positive difference shows a deleterious increase in strain on the anterior cruciate ligament. An identical method was used for presentation of the data in Figures 9, 10, and 11. The 95 per cent confidence limits for mean differences between testing with and without a brace are displayed centered at the zero strain value for forty, 100, and 180-newton load levels. The observations for each individual knee-brace are described in Table II. 3D = 3D dynamic functional knee-brace (3D Orthopaedic), US = Lerman Multi-Lig II brace (United States Manufacturing), TN = Townsend brace (Townsend Industries), DJ = DonJoy 4-point Sport ACL brace (DonJoy), CT = C.Ti. brace with ACL cable system (Innovation Sports), BL = Bledsoe Sports Rehab brace (Medical Technology), and LH = Lenox Hill derotation brace (Lenox Hill Brace Shop).
The Tukey studentized range test was used for pairwise comparisons among the seven braces, to evaluate further the significant differences among braces. The DonJoy brace had significantly greater average strain-shielding (p < 0.05) than either the 3D or the Lerman brace across zero, ten, twenty(twenty), and 180 newtons of anterior shear load. Also, the Townsend and C.Ti. braces were associated with a greater average reduction in strain (p < 0.05) than the 3D brace.
In order to compare the three custom braces with the four off-the-shelf braces, a separate three-way analysis was run for all subjects across the range of loads. On average, no significant difference in reduction of strain was seen between these two categories of braces.
A comparison of the reduction in strain between the group of braces as a whole and no use of a brace, at selected loads of forty, 100, and 180 newtons, indicated that at 100 newtons there was an average reduction of strain of 0.6 per cent (p < 0.05, Searle55 t test). The average reduction at forty or 180 newtons was not statistically significant. Further paired t analysis was done at the same selected load levels to consider the braces individually. This revealed that, at the 100-newton load, the DonJoy and Townsend braces were associated with a significant reduction in strain (p < 0.05) as compared with no brace (Table II and Fig. 8). No individual brace was associated with a significant reduction at forty or 180 newtons.
TABLE II.
Statistical Results for Comparisons between Testing with Each Individual Brace and Testing without a Brace*
| Knee-Brace | Anterior Shear Load (100 N)† | Active Range of Motion at 20 Degrees | Internal Torque (5 N-m) | Isometric Contraction of Quadriceps (30 N-m) |
|---|---|---|---|---|
| DonJoy | p ≤ 0.05 | NS | p ≤ 0.05 | NS |
| Townsend | p ≤ 0.05 | NS | p ≤ 0.05 | NS |
| C.Ti. | NS | NS | p ≤ 0.05 | NS |
| Lenox Hill | NS | NS | p ≤ 0.05 | NS |
| Bledsoe | NS | NS | NS | NS |
| Lerman | NS | NS | NS | NS |
| 3D | NS | NS | NS | NS |
NS = not significant.
Anterior shear loading at forty and 180 newtons produced non-significant differences in values for strain for all braces.
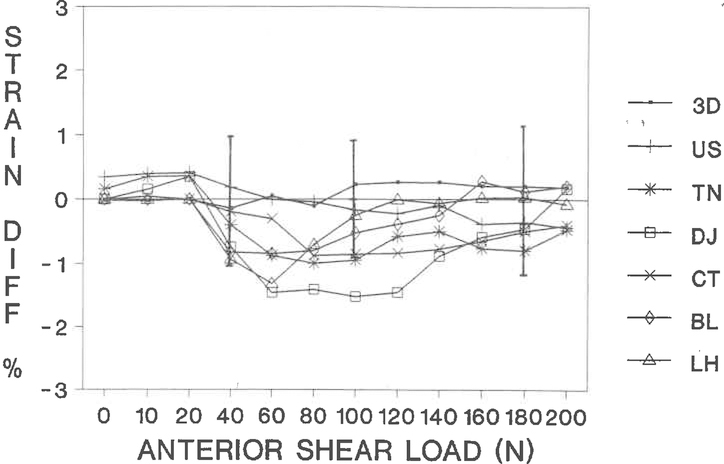
Internal and External Torque of the Tibia
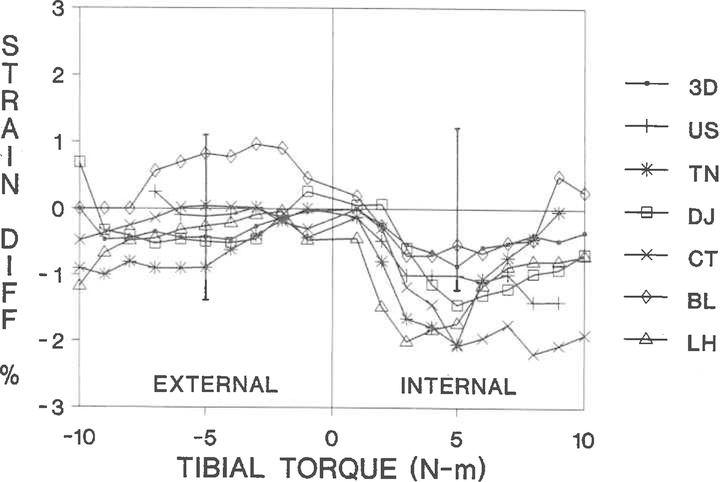
For internal and external torques of five newton-meters, there were no significant differences over-all among the braces (two-way analysis of variance). Comparisons of the braces as a group with no brace revealed no significant differences for external torque. However, for five newton-meters of applied internal torque, the value for strain on the anteromedial bundle was an average of 1.3 per cent less than the value under normal conditions (p ≤ 0.01).
A comparison between testing with each individual brace and testing with no brace revealed that the DonJoy, Townsend, C.Ti., and Lenox Hill braces significantly reduced strain on the anteromedial bundle at an applied internal torque of five newton-meters (Table II). The ability of each brace to provide strain-shielding in the anteromedial bundle was dependent on the magnitude of applied torque (Fig. 9).
Fig. 9.
The mean difference in values for strain across subjects (with the convention of strain for testing with a brace minus strain for testing without a brace) for internal and external applied torque at 30 degrees of flexion of the knee. All seven braces are included with the 95 per cent confidence limits for the mean differences between testing with and without a brace, displayed centered at the zero strain value, for internal (positive values) and external (negative values) tibial torque of five newton-meters. The observations for each individual brace are presented in Table II. 3D = 3D dynamic functional knee-brace (3D Orthopaedic), US = Lerman Multi-Lig II brace (United States Manufacturing), TN = Townsend brace (Townsend Industries), DJ = DonJoy 4-point Sport ACL brace (DonJoy), CT = C.Ti. brace with ACL cable system (Innovation Sports), BL = Bledsoe Sports Rehab brace (Medical Technology), and LH = Lenox Hill derotation brace (Lenox Hill Brace Shop).
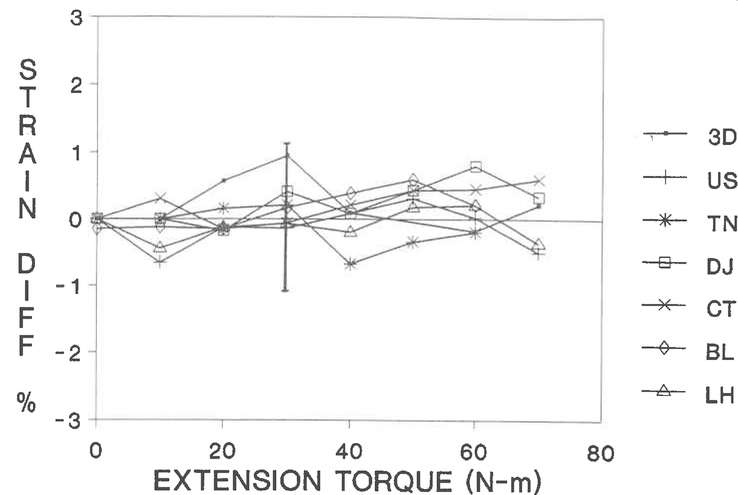
Isometric Contraction of the Quadriceps
There were no significant differences in the values for strain among braces at extension torque of thirty newton-meters. Similarly, there were no significant differences in strain on the anteromedial bundle when the results for the braces as a group were compared with those for no brace. Analysis of each brace individually revealed no significant difference in strain between testing with and without a brace at thirty newton-meters of extension torque (Fig. 10).
Fig. 10.
Plot of the mean difference in values for strain calculated across subjects (with the convention of strain for testing with a brace minus strain for testing without a brace) for isometric contraction of the quadriceps with the knee flexed 30 degrees. All seven braces are included with the 95 per cent confidence limits for the mean differences between testing with and without a brace, displayed centered at the zero strain value, for isometric quadriceps-extension torque to the level of thirty newton-meters. 3D = 3D dynamic functional knee-brace (3D Orthopaedic), US = Lerman Multi-Lig II brace (United States Manufacturing), TN = Townsend brace (Townsend Industries), DJ = DonJoy 4-point Sport ACL brace (DonJoy), CT = C.Ti. brace with ACL cable system (Innovation Sports), BL = Bledsoe Sports Rehab brace (Medical Technology), and LH = Lenox Hill derotation brace (Lenox Hill Brace Shop).
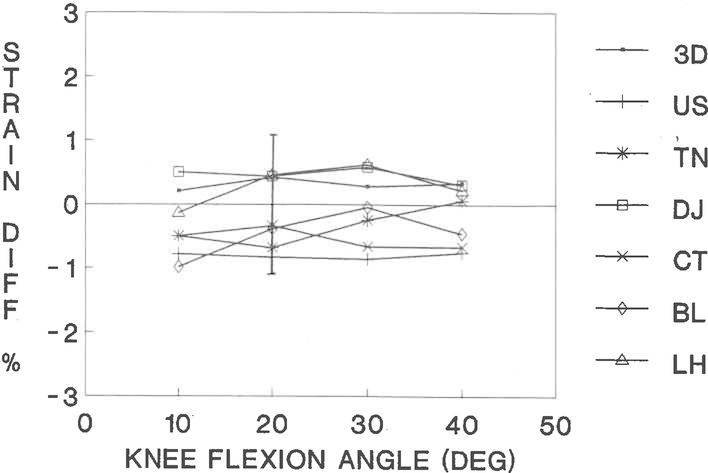
Active Range of Flexion-Extension of the Knee
There were no significant differences in strain among the braces when the knee was in 20 degrees of flexion. This was also true for the comparison between repeated testing without a brace and initial testing without a brace. For the comparison between the braces as a group and no brace, there were no significant differences. Analysis of each brace individually revealed no significant difference in values for strain between testing with a brace and without a brace (Fig. 11).
Fig. 11.
The mean difference in values for strain calculated across subjects (with the convention of strain for testing with a brace minus strain for testing without a brace) for active range of motion of the knee. All seven braces are included with the 95 per cent confidence limits for the mean differences between testing with and without a brace, displayed centered at the zero strain value, for active range of motion of the knee in 20 degrees of flexion (the angle of maximum strain for this activity). 3D = 3D dynamic functional knee-brace (3D Orthopaedic), US = Lerman Multi-Lig II brace (United States Manufacturing), TN = Townsend brace (Townsend Industries), DJ = DonJoy 4-point Sport ACL brace (DonJoy), CT = C.Ti. brace with ACL cable system (Innovation Sports), BL = Bledsoe Sports Rehab brace (Medical Technology), and LH = Lenox Hill derotation brace (Lenox Hill Brace Shop).
Discussion
We believe that this is the first study to demonstrate a safe and reliable means of direct measurement of the effect of a functional knee-brace on the strain biomechanics of the anterior cruciate ligament in vivo. An important aspect of the design of the study was the incorporation of repeated testing without a brace. This was performed as a check to ensure reproducibility of measurement with the Hall-effect transducer and the integrity of the interface between the transducer and the ligament. With reproducible repeated measures through a series of tests without a brace, we were confident that any changes in strain on the anterior cruciate ligament due to application of a brace were caused only by the brace.
In previous studies on functional knee-braces, in which ligamentous strain has been analyzed in vitro, measurements have been based on an arbitrarily defined reference for strain3,4. The techniques used in this study represent an important improvement because the calculation of strain was referenced to the palpable, slack-taut transition point of the ligament, allowing differentiation between values for strain representing conditions when the ligament was strained (load bearing) and values representing conditions when the ligament was unstrained (non-load bearing). Through the use of local anesthesia, this study included the effects of active muscle tone and contraction while strain on the anterior cruciate ligament was measured and performance of the brace was assessed directly. Unlike previous investigations of the performance of functional knee-braces, this study directly measured strain on the anterior cruciate ligament to determine the effect of bracing on the ligaments of the knee. All of the subjects were considered to have normal anterior cruciate ligaments, as assessed by clinical examination and arthroscopic visualization. Subjects who had had a partial meniscectomy, on either the medial or the lateral side, also were considered to have normal biomechanics of the knee. This is supported by the work of Levy et al., who investigated the effect of isolated medial29 and lateral30 meniscectomy on the biomechanics of the knee. The studies showed that anterior-posterior tibiofemoral displacement and coupled tibial rotation are not affected by either medial or lateral meniscectomy. Bargar et al. performed an in vivo study in human subjects and demonstrated that medial meniscectomy alone does not create a measurable change in varus-valgus laxity of the knee joint6. Because the subjects involved in the current study had had only a partial rather than a complete meniscectomy, it was assumed that the operative procedure did not produce abnormal behavior of the knee. The clinical relevance of this study was based on the following premise: if a functional brace is designed to reduce strain on an injured or reconstructed ligament or to minimize subluxations in a knee that has a torn anterior cruciate ligament, then the strain-shielding effects of the brace should be demonstrated in a knee that has a normal anterior cruciate ligament and surrounding ligaments.
In previous studies on specimens from human cadavera, there has been an increase in the load5 or the strain on the anterior cruciate ligament after a brace was applied to the knee3. These studies were the first to suggest that a knee-brace that has a fixed axis of rotation, which is dissimilar to the complex three-dimensional tibiofemoral rotational axes and translatory pathway, may constrain the knee joint and produce a deleterious increase in the values for strain on the anterior cruciate ligament. Our study found no evidence of an increase in strain as a result of the use of a functional knee-brace; this suggests that a patient is not at risk for increased strain on a repaired or reconstructed anterior cruciate ligament when wearing any of the functional knee-braces that were tested in this study.
The compressive joint load produced by body weight and muscle forces is difficult to define and control in vivo. During certain activities, the compressive joint load may provide some restraint to tibiofemoral translations and rotations; however, the extent to which these restraints occur in vivo is currently unknown. Therefore, this portion of the investigation was designed to apply known anterior shear loads and then internal-external torque to the knee joint without an applied compressive joint load, in an effort to challenge the interface between the brace and the knee in a controlled study. This investigation demonstrated that performance of the brace depends on the magnitude of both the anterior shear load and the internal torque applied across the tibiofemoral joint. No significant strain-shielding was demonstrated by any of the functional braces tested when anterior shear loads of 180 newtons were applied with the knee in 30 degrees of flexion. These findings are consistent with previous studies on instrumented laxity and clinical examination7,8,11,13,20,40. Therefore, functional knee-braces apparently can protect the anterior cruciate ligament or its replacement at only relatively low (less than 100-newton) anterior shear loads. This magnitude of load is small compared with the magnitude of anterior shear loads produced during activities of daily living37–39,47. Noyes et al.47 hypothesized that the anterior cruciate ligament is subjected to loads ranging from zero to 454 newtons during most common activities of daily living. Our findings are supported by the in vivo study performed by Jonsson and Kärrholm on subjects who had a torn anterior cruciate ligament24. In this investigation, tantalum balls were implanted in different regions of the knee, and tibiofemoral displacements were measured with a roentgen-stereophotogrammetric technique. On average, the braces reduced the anterior-posterior translation of the injured knee by one-third of the initial value24. None of the braces tested was able to restore the anterior-posterior translation of the injured knee to within the limits of the translation of the normal contralateral knee. Our findings are supported also by the work of Wojtys et al.60, who studied the effect of functional braces on knees with a tom anterior cruciate ligament in cadavera that were tested by anterior shear loading. These authors demonstrated that each of the functional braces evaluated was unable to restore the anterior excursion of the tibia relative to the femur to within normal limits.
The DonJoy and Townsend were the only two braces that provided a strain-shielding effect to the anterior cruciate ligament with an applied anterior shear load of 100 newtons. These braces, as well as the other five, did not significantly reduce the values for strain on the anterior cruciate ligament during isometric contraction of the quadriceps, which also is an anterior shear-loading activity4,9,17,44. This finding is in agreement with the work of Branch et al.11, who performed an in vivo study with the KT-1000 arthrometer (MedMetric, San Diego, California) and found similar results with the active quadriceps anterior-drawer test. This finding may help to explain why some athletes injure the anterior cruciate ligament while wearing a functional brace during non-contact sports. Isometric contraction of the quadriceps produces anterior shear loads that challenge the anterior cruciate ligament and also creates a change in the attachment interface between the brace and soft tissues of the lower limb. As the muscle activity increases and decreases, the compliance at the brace-limb interface also will vary in direct proportion. This variability will affect the ability of the brace to control tibiofemoral motion and to protect the articular cartilage in a knee that has a torn anterior cruciate ligament or an anterior cruciate replacement. The contrast in results between the tests for anterior shear loading and isometric contraction of the quadriceps suggests that evaluation of bracing of the knee should be performed in the in vivo environment, instead of an attempt being made to recreate the complex attachment interface in vitro.
The DonJoy, Lenox Hill, Townsend, and C.Ti. braces demonstrated a significant strain-shielding effect on the anterior cruciate ligament with a five-newton-meter internal torque applied to the knee joint. Because our experimental protocol did not consistently produce magnitudes of torque greater than five newton-meters (torque in excess of this value produced pain in several subjects), we were unable to determine statistically if the braces maintained their strain-shielding effect at values for torque in excess of this magnitude. For all of the braces, the mean strain-difference plot for internal-external torque approached zero at magnitudes of torque of more than five newton-meters (Fig. 9). This suggests that for an applied internal torque to the tibia — a primary mechanism of injury to the anterior cruciate ligament — the protective strain-shielding effect provided by the functional braces decreases as the magnitude of internal torque increases. This finding is supported by the in vivo study of Jonsson and Kärrholm, which revealed that, in subjects who had a torn anterior cruciate ligament, a functional knee-brace did not alter the internal rotatory laxity of the knee resulting from an applied internal torque of eight newton-meters24.
The results of the measurements of the strain on the anterior cruciate ligament demonstrated that different braces perform differently. This is consistent with the results of previous in vitro and in vivo studies of static and dynamic testing done with functional knee-braces5,8,14,15,22,28,34–36,52,59,60,62. Previous investigators have suggested a variety of reasons why some designs of braces work better than others. Knutzen et al.26–28 suggested that functional knee-braces can change the kinematics and the kinetics of the knee. Others have found positioning of the brace and placement of the hinge to be critical factors in the determination of performance of a brace16,31–33,51. The wearing of a brace has been demonstrated to make subjects feel more secure and may even increase athletic performance. Cook et al.14 suggested that the use of a functional knee-brace may provide a beneficial proprioceptive effect. However, their investigation revealed that subjects can have tibiofemoral subluxation while wearing a brace. Branch et al.10 refuted the principle that a knee-brace provides a proprioceptive effect by demonstrating that use of the brace did not alter electromyographic activity or change patterns of muscle firing.
The performance of a functional knee-brace is determined by the technique of attachment, design of the brace, and variables in the attachment interface. This study involved careful attention to the technique of attachment; the same certified orthotist fitted and applied all of the custom braces and the same one of us (C. M. W.) fitted all the off-the-shelf braces, according to the recommendations of the manufacturer. The variables in the design of the brace, which included the hinge, geometry of the attachment interface, mechanism of attachment, and materials of fabrication, were not individually studied, since a wide variety of designs of braces are commercially available. The attachment interface refers to how the brace attaches to the compliant muscles of the lower limb in an effort to control osseous tibiofemoral displacements and resultant strain on the ligaments of the knee. This not only involves the concept of fit and rigidity of the brace or how well the contour of the brace matches the contour of the soft tissues surrounding the knee, but it also relates to how much displacement occurs between a rigid brace and compliant soft tissue surrounding the distal part of the femur and the proximal portion of the tibia while loads are applied across the knee. It is possible to alter the rigidity of the brace through different designs; however, the variability of soft-tissue compliance cannot be changed. This may be the limiting factor to the performance of functional knee-braces. An interesting experiment demonstrates this point. Contraction of the muscles of the thigh or the calf (muscles as tense as possible) and pushing of the thumb perpendicular to and directed toward the long bones of the lower limb is a simulation of loading of the interface between the brace and the soft tissues. With a small magnitude of applied force, a relatively large amount of displacement occurs. This simple example demonstrates the weak link in the interface between the brace and the soft tissues and may help to explain why some athletes have episodes of pivot shift while wearing a functional brace14. This in vivo study of strain on the anterior cruciate ligament did not control for the design of the brace and variables of the attachment interface separately but, instead, analyzed them as a group. Additional studies are needed to investigate how these variables individually affect performance of the brace, in order to identify which, if any, variables of design can improve the performance of a functional knee-brace.
Finally, we found that there is no apparent advantage of a custom-made brace over an off-the-shelf brace. Jonsson and Kärrholm made in vivo measurements, using the roentgen-stereophotogrammetric technique, in subjects who had a torn anterior cruciate ligament and also found similar results for the custom and off-the-shelf designs of braces24. Romash et al. supported these findings in tests performed with the KT-1000 arthrometer on custom and off-the-shelf designs53.
Acknowledgments
Although none of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but are directed solely to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated. Funds were received in total or partial support of the research or clinical study presented in this article. The funding sources were Grants R01-AR39213 and R01-AR40174 from the National Institutes of Health; Innovation Sports, Irvine, California; Lenox Hill Brace Shop, New York, N.Y.; Townsend Industries, Bakersfield, California; DonJoy, Carlsbad, California; 3D Orthopaedic, Dallas, Texas; Medical Technology, Grand Prairie, Texas; and United States Manufacturing, Pasadena, Califoinia.
Note: The authors thank Per Renström, M.D., Ph.D., and Ann Erickson, M.S., for intraoperative acquisition of data; Larry D. Haugh, Ph.D., for statistical analysis; and David Spear and Ethan Berke for programming assistance. The authors also thank’ Dave Baylis, C.P.O., for help in the fitting and application of knee-braces throughout the study.
References
- 1.American Academy of Orthopaedic Surgeons: The use of knee braces. AAOS Bulletin, 36:17–18, Jan. 1988. [Google Scholar]
- 2.Arms SA: Miniature Hall effect displacement sensor for medical applications. Read at the Sensors Exposition International, Cleveland, Ohio, Sept. 12, 1989. [Google Scholar]
- 3.Arms S; Donnermeyer D; Renstrom P; Pope M; Johnson R; and Incavo S: The effect of knee braces on anterior cruciate ligament strain. Trans. Orthop. Res. Soc, 12: 245, 1987. [Google Scholar]
- 4.Arms SW; Pope MH; Johnson RJ; Fischer RA; Inga Arvidsson; and Ejnar Eriksson: The biomechanics of anterior cruciate ligament rehabilitation and reconstruction. Am. J. Sports Med, 12: 8–18, 1984. [DOI] [PubMed] [Google Scholar]
- 5.Baker BE; VanHanswyk E; Bogosian S IV; Wemer FW; and Murphy D: A biomechanical study of the static stabilizing effect of knee braces on medial stability. Am. J. Sports Med, 15: 566–570, 1987. [DOI] [PubMed] [Google Scholar]
- 6.Bargar WL; Moreland JR; Markolf KL; Shoemaker SC; Amstutz HC; and Grant TT: In vivo stability testing of post-meniscectomy knees. Clin. Orthop, 150: 247–252, 1980. [PubMed] [Google Scholar]
- 7.Bassett GS, and Fleming BW: The Lenox Hill brace in anterolateral rotatory instability. Am. J. Sports Med, 11: 345–348, 1983. [DOI] [PubMed] [Google Scholar]
- 8.Beck C; Drez D Jr.; Young J; Cannon WD Jr.; and Stone ML: Instrumented testing of functional knee braces. Am. J. Sports Med, 14: 253–256, 1986. [DOI] [PubMed] [Google Scholar]
- 9.Beynnon BD; Howe JG; Pope MH; Johnson RJ; and Fleming BC: Anterior cruciate ligament strain in-vivo. Internat. Orthop, 16: 1–12, 1992. [DOI] [PubMed] [Google Scholar]
- 10.Branch TP; Hunter R; and Donath M: Dynamic EMG analysis of anterior cruciate deficient legs with and without bracing during cutting. Am. J. Sports Med, 17: 35–41, 1989. [DOI] [PubMed] [Google Scholar]
- 11.Thomas Branch; Robert Hunter; and Peter Reynolds: Controlling anterior tibial displacement under static load: a comparison of two braces. Orthopedics, 11: 1249–1252, 1988. [DOI] [PubMed] [Google Scholar]
- 12.Cawley PW; France EP; and Paulos LE: The current state of functional knee bracing research. A review of the literature. Am. J. Sports Med, 19: 226–233, 1991. [DOI] [PubMed] [Google Scholar]
- 13.Colville MR; Lee CL; and Ciullo JV: The Lenox Hill brace. An evaluation of effectiveness in treating knee instability. Am. J. Sports Med, 14: 257–261, 1986. [DOI] [PubMed] [Google Scholar]
- 14.Cook FF; Tibone JE; and Redfern FC: A dynamic analysis of a functional brace for anterior cruciate ligament insufficiency. Am. J. Sports Med, 17: 519–524, 1989. [DOI] [PubMed] [Google Scholar]
- 15.Coughlin L; Oliver J; and Berretta G: Knee bracing and anterolateral rotatory instability. Am. J. Sports Med, 15: 161–163, 1987. [DOI] [PubMed] [Google Scholar]
- 16.D’Ambrosia Robert, and Moshe Solomonow: A viscoelastic knee brace for anterior cruciate ligament deficient patients. Orthopedics, 8: 478–480, 1985. [DOI] [PubMed] [Google Scholar]
- 17.Daniel DM, and Stone ML: KT-1000 anterior-posterior displacement measurements In Knee Ligaments. Structure, Function, Injury, and Repair, pp. 443–447. Edited by Daniel DM, Akeson WH, and O’Connor JJ New York, Raven Press, 1990. [Google Scholar]
- 18.Erickson AR: A dynamic evaluation of prophylactic knee braces. Thesis, University of Vermont, 1991. [Google Scholar]
- 19.Eriksson Ejnar: Comprehensive knee rehabilitation. Bull. Hosp. Joint Dis, 48: 117–129, 1988. [PubMed] [Google Scholar]
- 20.Gerber C; Jakob RP; and Ganz R: Observations concerning the limited mobilisation cast after anterior cruciate ligament surgery. Arch. Orthop. and Traumat. Surg, 101: 291–296, 1983. [DOI] [PubMed] [Google Scholar]
- 21.Helfet AJ; Manley MT; and Vaughan CL: The helicoid knee brace: a lightweight but effective support for the damaged knee. Injury, 15: 189–192, 1983. [DOI] [PubMed] [Google Scholar]
- 22.Hofmann AA; Wyatt RWB; Bourne MH; and Daniels AU: Knee stability in orthotic knee braces. Am. J. Sports Med, 12: 371–374, 1984. [DOI] [PubMed] [Google Scholar]
- 23.Howe JG; Wertheimer CM; Johnson RJ; Nichols CE; Pope MH; and Beynnon BD: Arthroscopic strain gauge measurement of the normal anterior cruciate ligament. Arthroscopy, 6(3): 198–204, 1990. [DOI] [PubMed] [Google Scholar]
- 24.Jonsson Håkan, and Johan Kärrholm: Brace effects on the unstable knee in 21 cases. A roentgen stereophotogrammetric comparison of three designs. Acta Orthop. Scandinavica, 61: 313–318, 1990. [DOI] [PubMed] [Google Scholar]
- 25.Kain CC; McCarthy JJ; Arms S; and Manske PR: An in vivo study of the effect of transcutaneous electrical muscle stimulation on ACL deformation. Trans. Orthop. Res. Soc, 12: 106, 1987. [Google Scholar]
- 26.Knutzen KM; Bates BT; and Joseph Hamill: Electrogoniometry of post-surgical knee bracing in running. Am. J. Phys. Med, 62: 172–181, 1983. [PubMed] [Google Scholar]
- 27.Knutzen KM; Bates BT; and Joseph Hamill: Knee brace influences on the tibial rotation and torque patterns of the surgical limb. J. Orthop. and Sports Phys. Ther, 6: 116–122, 1984. [DOI] [PubMed] [Google Scholar]
- 28.Knutzen KM; Bates BT; Philip Schot; and Joseph Hamill: A biomechanical analysis of two functional knee braces. Med. and Sci. Sports and Exerc, 19: 303–309, 1987. [PubMed] [Google Scholar]
- 29.Levy IM; Torzilli PA; and Warren RF: The effect of medial meniscectomy on anterior-posterior motion of the knee. J. Bone and Joint Surg, 64-A: 883–888, July 1982. [PubMed] [Google Scholar]
- 30.Levy IM; Torzilli PA; Gould JD; and Warren RF: The effect of lateral meniscectomy on motion of the knee. J. Bone and Joint Surg, 71-A: 401–406, March 1989. [PubMed] [Google Scholar]
- 31.Lew WD; Patmchak CM; Lewis JL; and John Schmidt: A comparison of pistoning forces in orthotic knee joints. Orthot. and Prosthet, 36(2): 85–95, 1982. [Google Scholar]
- 32.Lewis JL; Lew WD; Patmchak CM; and Shybut GT: A new concept in orthotics joint design — the Northwestern University knee orthosis system. Orthot. and Prosthet, 37(4): 15–23, 1983–1984. [Google Scholar]
- 33.Lewis JL; Lew WD; Stalberg SD; Patmchak CM; and Shybut GT: A new concept in orthotics — the Northwestern University knee orthosis system. Part II: the complete orthosis. Orthot. and Prosthet, 38(1): 13–28, 1984. [Google Scholar]
- 34.Loubert PV; Wojtys EM; Viviano DM; Samson SY; and Goldstein SA: A quantitative assessment of the efficacy of 14 functional knee braces. Trans. Orthop. Res. Soc, 14: 221, 1989. [Google Scholar]
- 35.Millet Chad, and Drez David Jr.: Knee braces. Orthopedics, 10: 1777–1780, 1987. [PubMed] [Google Scholar]
- 36.Millet CW, and Drez DJ Jr.: Principles of bracing for the anterior cruciate ligament-deficient knee. Clin. Sports Med, 7: 827–833, 1988. [PubMed] [Google Scholar]
- 37.Morrison JB: Bioengineering analysis of force actions transmitted by the knee joint. Bio-Med. Eng, 3: 164–170, 1968. [Google Scholar]
- 38.Morrison JB: Function of the knee joint in various activities. Bio-Med. Eng, 4: 573–580, 1969. [PubMed] [Google Scholar]
- 39.Morrison JB: The mechanics of the knee joint in relation to normal walking. J. Biomech, 3: 51–61, 1970. [DOI] [PubMed] [Google Scholar]
- 40.Mortensen WW; Foreman K; Focht L; and Daniel D: An in vitro study of functional orthoses in the ACL disrupted knee. Trans. Orthop. Res. Soc, 13: 520, 1988. [Google Scholar]
- 41.Nicholas JA: The five-one reconstruction for anteromedial instability of the knee. Indications, technique, and the results in fifty-two patients. J. Bone and Joint Surg, 55-A: 899–922, July 1973. [PubMed] [Google Scholar]
- 42.Nicholas JA: Bracing the anterior cruciate ligament deficient knee using the Lenox Hill derotation brace. Clin. Orthop, 172: 137–142, 1983. [PubMed] [Google Scholar]
- 43.Nicholas JA: Knee braces that protect against sports injuries. J. Musculoskel. Med, 3:56–61, Oct. 1986. [Google Scholar]
- 44.Nisell R: On the biomechanics of the knee — a study of joint and muscle load with application in ergonomics, orthopaedics, and rehabilitation. Dissertation, Karolinska Institute, Department of Anatomy, Stockholm, Sweden, 1985. [Google Scholar]
- 45.Noyes FR; Mangine RE; and Barber S: Early knee motion after open and arthroscopic anterior cruciate ligament reconstruction. Am. J. Sports Med, 15: 149–160, 1987. [DOI] [PubMed] [Google Scholar]
- 46.Noyes FR; Matthews DS; Mooar PA; and Grood ES: The symptomatic anterior cruciate-deficient knee. Part II: the results of rehabilitation, activity modification, and counseling on functional disability. J. Bone and Joint Surg, 65-A: 163–174, Feb. 1983. [DOI] [PubMed] [Google Scholar]
- 47.Noyes FR; Butler DL; Grood ES; Zernicke RF; and Hefzy MS: Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J. Bone and Joint Surg, 66-A: 344–352, March 1984. [PubMed] [Google Scholar]
- 48.Paulos Lonnie; Noyes FR; Edward Grood; and Butler DL: Knee rehabilitation after anterior cruciate ligament reconstruction and repair. Am. J. Sports Med, 9: 140–149, 1981. [DOI] [PubMed] [Google Scholar]
- 49.Paulos LE; France EP; Rosenberg TD; Jayaraman G; Abbott PJ; and Jaen J: The biomechanics of lateral knee bracing. Part I: response of the valgus restraints to loading. Am. J. Sports Med, 15: 419–429, 1987. [DOI] [PubMed] [Google Scholar]
- 50.Podesta Luga, and Sherman MF: Knee bracing. Orthop. Clin. North America, 19: 737–745, 1988. [PubMed] [Google Scholar]
- 51.Regalbuto MA; Rovick JS; and Walker PS: The forces in a knee brace as a function of hinge design and placement. Am. J. Sports Med, 17: 535–543, 1989. [DOI] [PubMed] [Google Scholar]
- 52.Rink PC; Scott RA; Lupo RL; and Guest SJ: A comparative study of functional bracing in the anterior cruciate deficient knee. Orthop. Rev, 18: 719–727, 1989. [PubMed] [Google Scholar]
- 53.Romash MM; Henningsen HJ; and John Claybaugh: Knee braces — comparative functional testing. Orthop. Trans, 13: 501, 1989. [Google Scholar]
- 54.SAS Institute: SAS User’s Guide, Basics Version 5. Cary, North Carolina, SAS Institute, 1985. [Google Scholar]
- 55.Searle SR: Linear Models. New York, Wiley, 1971. [Google Scholar]
- 56.Tegner Y, and Lorentzon R: Evaluation of knee braces in Swedish ice hockey players. British J. Sports Med, 25: 159–161, 1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Torg JS; Wayne Conrad; and Vickie Kalen: Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am. J. Sports Med, 4: 84–93, 1976. [DOI] [PubMed] [Google Scholar]
- 58.Wellington P, and Stother IG: The Lenox Hill derotation brace in chronic post-traumatic instability of the knee. Injury, 15: 242–244, 1984. [DOI] [PubMed] [Google Scholar]
- 59.Wojtys EM; Loubert PV; Samson SY; and Viviano DM: Use of a knee-brace for control of tibial translation and rotation. A comparison, in cadavera, of available models. J. Bone and Joint Surg, 72-A: 1323–1329, Oct. 1990. [PubMed] [Google Scholar]
- 60.Wojtys EM; Redfern MS; Trier EM; and Goldstein SA: A computer assisted system for simultaneous evaluation of multiple mechanical factors on knee joint stability: the Lenox-Hill brace. Trans. Orthop. Res. Soc, 10: 224, 1985. [Google Scholar]
- 61.Wojtys EM; Goldstein SA; Redfern M; Trier E; and Matthews LS: A biomechanical evaluation of the Lenox Hill knee brace. Clin. Orthop, 220: 179–184, 1987. [PubMed] [Google Scholar]
- 62.Zogby RG; Baker BE; Seymour RJ; Van Hanswyk E; and Werner FW: A biomechanical evaluation of the effect of functional braces on anterior cruciate ligament instability, using the GENUCOM knee analysis system. Trans. Orthop. Res. Soc, 14: 212, 1989. [Google Scholar]