Abstract
Objectives
To explore whether the Affordable Care Act (ACA) enactment is associated with changes in the proportion of discharge against medical advice (DAMA) among hospitalizations due to substance use disorders (SUDs).
Methods
Data were drawn from the 2012-2015 National Inpatient Samples. The sample comprised hospitalizations with a principal diagnosis of SUD (i.e., SUD-involved hospitalization) for patients aged 18-64 years (unweighted N=287,629). Interrupted time series analyses were conducted to evaluate the effect of the ACA on monthly proportions of DAMA among SUD-involved hospitalizations.
Results
Overall, approximately 11% of SUD-involved hospitalizations were DAMA. DAMA was most frequently found among hospitalizations for primary opioid use disorder (pre-ACA: 16.4%; post-ACA: 17.2%). Despite the increase in the Medicaid coverage after ACA enactment, there was no significant change in the proportion of DAMA before and after ACA periods across various demographic groups and clinical conditions. Time series analyses also indicated no significant trend effect on the proportion of DAMA during the pre- and post-ACA months.
Conclusions
As many as 1 in 10 SUD-involved hospitalizations were considered as DAMA. Concerted efforts are needed to enhance insurance benefits for SUDs and patients’ knowledge of SUD treatment benefits in order to increase SUD treatment engagement and completion and to reduce DAMA, especially for substance-using patients with Medicaid or opioid use disorder.
Keywords: Against Medical Advice, Substance Use Disorder, The Affordable Care Act, Medicaid, Treatment
1. Introduction
Notably, substance use disorders (SUDs: alcohol or drug use disorders) is among the most prevalent diagnoses in discharge against medical advice (DAMA) hospitalizations in the United States, with an estimated proportion of 14% (Spooner et al., 2017). DAMA is indicative of the receipt of inadequate treatment for SUD following an episode of SUD problems, which is associated with SUD treatment readmissions and poorer outcomes (Alfandre, 2009; Southern et al., 2012; Wines et al., 2007). However, few studies have focused on DAMA behaviors among patients admitted to SUD treatment, and there is a lack of data using large samples to better characterize DAMA related to drug use disorders (Ti and Ti, 2015). Thus, it is important to study DAMA and its pattern in a large national sample of patients admitted to SUD treatment in order to provide generalizable estimates to inform efforts aimed at reducing DAMA and improving the linkage to proper specialty treatment or follow-up care.
Furthermore, the Affordable Care Act (ACA) may increase access to SUD treatment and enhance the quality of such treatment for previously uninsured or under-insured SUD patients through expanding coverage and associated SUD benefit of Medicaid expansion and health insurance exchange programs (Abraham et al., 2017; Beronio et al., 2013). Prior to ACA, having Medicaid or no insurance was associated with DAMA in samples of general or detoxification hospitalizations (Blondell et al., 2006; Tawk et al., 2013). Thus, the ACA may potentially improve the uptake for SUD treatment and its treatment length to reduce DAMA. However, to date, there has been no empirical study to examine changes in DAMA among SUD patients after ACA. One study found that, among adults with SUD, the prevalence of Medicaid coverage increased significantly from 11.6% in 2011-2013 to 16.0% in 2014, but there was no significant change in the prevalence of SUD treatment utilization (Saloner et al., 2017). Particularly, the United States is amid the opioid epidemic, and there is a need to maximize the benefit of Medicaid expansion to address the opioid epidemic (Humphreys, 2018; Sharp et al., 2018). A detoxification center reported that over half of opioid-using detoxification patients were DAMA (Kenne et al., 2010). It is imperative to investigate DAMA by using national samples to inform intervention needs and strategies for improving SUD treatment engagement for patients at-risk for DAMA, especially for opioid use disorders (OUDs).
To better understand the extent of DAMA within the context of ACA enactment, this study uses a nationally representative inpatient sample to (1) examine the proportions of DAMA among hospitalizations due to SUD before and after ACA periods, and (2) determine the effect of ACA on the proportions of DAMA.
2. Methods
2.1. Data Source
The data were drawn from the National Inpatient Sample (NIS), the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (HCUP, 2017). The NIS is a nationally representative sample of inpatient discharges from non-rehabilitation and non-long-term acute care community hospitals. The study period was from January 2012 to September 2015. The fourth quarter of 2015 data was excluded because the conversion from the ICD-9-CM to the ICD-10-CM coding system may create diagnosis discontinuity problems (Hesiln et al., 2017).
2.2. Study Sample
The unit of analysis is a hospitalization encounter. We focused on the hospitalizations with a principal diagnosis of SUD (i.e., SUD-involved hospitalizations) for patients aged 18-64 years, excluding cases of death in hospital and cases with a missing disposition status or admission month (about 1% of the sample). SUDs (i.e., alcohol or drug use disorders) were identified based on the ICD-9-CM diagnosis codes 291-292 and 303-305 (excluding tobacco use disorder and remission codes). The principal diagnosis was defined as the condition chiefly responsible for the hospital admission. This sample represented a national sample of hospitalizations with patients receiving treatment for substance-related diagnoses in community hospitals (Weiss and Heslin, 2018). The unweighted sample size for this analysis is 287,629.
2.3. Study Variables
The primary outcome of this study was the proportion of DAMA among SUD-involved hospitalizations. We identified DAMA hospitalizations as patients whose disposition status was DAMA (i.e., UB-04 billing claim form: left against medical advice or discontinued care). We divided the study period into two intervals to reflect the policy change of the ACA starting in 2014: pre-ACA (January 2012-December 2013) and post-ACA (January 2014-September 2015) periods.
2.4. Statistical Analysis
We aggregated the data and calculated the monthly weighted proportion of DAMA among SUD-involved hospitalizations at the national level by considering the NIS’s complex sample designs. We had estimated 45-month time-series data on the proportion of DAMA among SUD-involved hospitalizations. Next, we conducted the single-group interrupted time series analysis (ITSA) to evaluate changes in DAMA proportions before and after ACA periods (policy interruption point: January 2014) in the total sample and among selected insurance (Medicaid, private) and SUD diagnosis (alcohol, drug, opioid) subgroups. The ITSA has been commonly used as a quasi-experimental method to assess the immediate effect of health policies (Bernal et al., 2017; Linden, 2015). Our models included three key predictors: (1) the time elapsed (month); (2) intervention indicator (pre-ACA=0; post-ACA=1); and (3) interaction of time and intervention variables. Additionally, the autocorrelation and seasonality of outcome data were checked and adjusted in six models. Stata 15.1 software was used for all estimates (StataCorp, 2017).
3. Results
3.1. Proportion of DAMA Before and After the ACA Enactment (Supplementary Tables S1 And S2)1
From January 2012 to September 2015, approximately 11% of SUD-involved hospitalizations were DAMA, and the annual DAMA proportion was relatively stable over time. Of note, the proportion of Medicaid coverage increased by 10% in the post-ACA years (2015Q1-Q3: 42.1%, 2014: 40.0% vs. 2013: 30.1%, 2012: 31.2%).
About 10.8% and 11.0% of SUD-involved hospitalizations were DAMA in the pre-ACA period and the post-ACA period, respectively. There was no significant change in the proportion of DAMA among SUD-involved hospitalizations before and after ACA periods across demographic and clinical groups. Hospitalizations primarily due to OUD (i.e., OUD-involved hospitalizations) had the highest proportion of DAMA (pre-ACA: 16.4%; post-ACA: 17.2%).
3.2. The Effect of The ACA on The Proportion of DAMA (Table 1 and Figure 1)
Table 1.
Estimates of interrupted time series models for the monthly proportion of discharge against medical advice (DAMA) among substance use disorder (SUD) involved hospitalizations: National Inpatient Samples, 2012-2015Q3
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Outcomes | Proportion of DAMA among SUD-involved hospitalizations | Proportion of DAMA among SUD-involved hospitalizations with Medicaid coverage | Proportion of DAMA among SUD-involved hospitalizations with private insurance | Proportion of DAMA among SUD-involved hospitalizations with alcohol use disorder | Proportion of DAMA among SUD-involved hospitalizations with drug use disorder | Proportion of DAMA among SUD-involved hospitalizations with opioid use disorder |
| Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | |
| Time (months) | −0.01 (−0.03, 0.01) | −0.03 (−0.08, 0.01) | 0.03 (−0.01, 0.06) | −0.02 (−0.04, 0.01) | 0.001 (−0.03, 0.03) | −0.07 (−0.13, 0.00) |
| Post (pre-ACA=0; post - ACA=1) | 0.06 (−0.39, 0.51) | −0.36 (−1.25, 0.53) | −0.47 (−1.24, 0.29) | 0.30 (−0.26, 0.85) | −0.20 (−0.82, 0.43) | 1.46 (0.13, 2.80) |
| Time*post | 0.03 (−0.001, 0.06) | 0.04 (−0.02, 0.11) | 0.01 (−0.05, 0.07) | 0.03 (−0.01, 0.07) | 0.03 (−0.02, 0.07) | 0.07 (−0.02, 0.17) |
| Quarter (vs. Quarter 1) | ||||||
| Quarter 2 | 0.64 (0.34, 0.94) | 0.68 (0.10, 1.27) | 1.01 (0.51, 1.52) | 0.58 (0.20, 0.96) | 0.80 (0.38, 1.22) | 1.40 (0.50, 2.30) |
| Quarter 3 | 0.68 (0.37, 0.99) | 1.01 (0.41, 1.62) | 0.67 (0.15, 1.19) | 0.63 (0.24, 1.01) | 0.85 (0.42, 1.28) | 1.34 (0.42, 2.26) |
| Quarter 4 | 0.40 (0.06, 0.75) | 0.78 (0.11, 1.45) | 0.23 (−0.36, 0.81) | 0.36 (−0.07, 0.79) | 0.61 (0.13, 1.10) | 0.30 (−0.73, 1.33) |
| Constant | 10.44 (10.14, 10.75) | 13.18 (12.58, 13.78) | 7.56 (7.05, 8.08) | 9.91 (9.53, 10.28) | 11.24 (10.81, 11.66) | 16.38 (15.47, 17.28) |
Notes. Interrupted time series models were adjusted for autocorrelation by using Prais-Winsten method and for seasonality by adding quarterly indictors.
Boldface: p<0.05.CI: confidence interval; DAMA: discharge against medical advice; SUD: substance use disorder.
Figure 1.
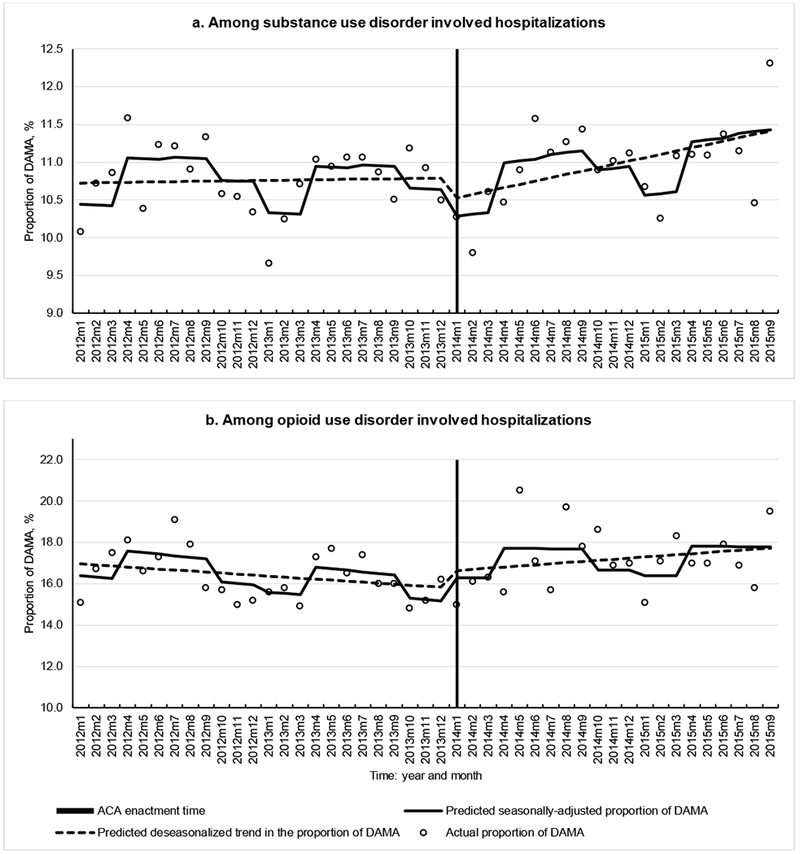
Interrupted time series analysis of monthly proportions of discharge against medical advice (DAMA) among substance and opioid use disorder involved hospitalizations: National Inpatient Samples, 2012-2015Q3.
The results from ITSA models showed that, among SUD-involved hospitalizations (Model 1), the monthly proportion of DAMA had no significant change in the pre-ACA trend, post-ACA trend (relative to the pre-ACA trend). There was no immediate effect of ACA enactment (the value in January 2014 relative to the corresponding predicated value from the pre-ACA trend). Similarly, no significant change related to ACA policy change was observed for the proportion of DAMA among other subgroups (Models 2-5: SUD-involved hospitalizations with Medicaid, private insurance, alcohol use disorder, and drug use disorder). The only significant findings from ITSA models was a significant immediate increase in the proportion of DAMA among OUD-involved hospitalizations in January 2014 (Model 6). However, the comparison of DAMA proportion before and after ACA periods was not significant (no significant difference in the DAMA proportion among OUD-involved hospitalizations between pre- and post- ACA periods). Figure 1 illustrates the actual and predicated monthly proportions of DAMA among SUD- and OUD-involved hospitalizations from results of ITS A models (Models 1 and 6).
4. Discussion
Patients admitted to the hospital due to SUD diagnosis but leaving hospital against medical advice indicate that opportunities to promote patients’ uptake for SUD treatment and retention are missed, thereby increasing the risk for morbidity (Alfandre 2009; Southern et al., 2012). Hospitalized SUD patients are likely to have a severe medical condition that requires intensive SUD treatment. Their SUD treatment needs thus must be addressed properly. This study analyzed a large nationally representative sample to examine the effect of ACA on the DAMA proportion from SUD-involved hospitalizations. We found that, despite an increase in Medicaid coverage as payer, there was no significant change in the proportion of DAMA among SUD-involved hospitalizations following the ACA enactment. In addition, DAMA was more prevalent among OUD-involved hospitalizations than other demographic and clinical groups. The ITSA models also indicated no significant trend effect in the proportion of DAMA during the pre- and post-ACA months. These findings reinforce a critical need to improve SUD treatment uptake and retention, especially for patients with OUD, in order to reduce DAMA and associated poorer outcomes.
4.1. Key Findings
Our major finding concerns that the increase in Medicaid coverage after ACA was not linked to the reduction of DAMA among hospitalizations due to SUD diagnoses. In line with previous study showing Medicaid coverage as one of the strongest predictors of DAMA in short-stay care hospitals (Tawk et al., 2013), our results show that DAMA was consistently more prevalent among SUD-hospitalizations with Medicaid than those with other insurance types (e.g., private, Medicare) before and after ACA periods. The ACA enactment expands insurance coverage and benefits of SUD treatment to more individuals with SUDs through Medicaid expansion and health exchanges, which also provides the opportunities to reduce DAMA. It was estimated that 14.6% of potentially new Medicaid expansion enrollees have an SUD compared to 11.5% of traditional Medicaid enrollees (Busch et al., 2013). However, the potential constraints of Medicaid coverage for SUD treatment benefits, patient’s lack of adequate knowledge toward SUD treatment benefits, or patient’s financial barriers may contribute to limited utilization of SUD treatments and DAMA (Ali et al., 2017; Cummings et al., 2014; Grogan et al., 2016). For example, the ACA requires that Medicaid expansion must include SUD benefits in the Essential Health Benefits but there is no such mandate requirement for the traditional Medicaid, and Medicaid in the majority of states does not cover comprehensive treatments for SUDs (Grogan et al., 2016). Further, an estimate of less than 50% of addiction treatment programs that accepted Medicaid for SUD treatment coverage were in the states with fewer or limited Medicaid benefits (Andrews et al., 2018). Provisions of financial incentive to states in order to expand Medicaid’s SUD services and developments of more publicly-owned SUD treatment programs are needed to improve SUD treatment and its capabilities (Andrews et al., 2018; Grogan et al., 2016). In addition, SUD patients who left hospital or other treatment facilities prematurely may be related to other individual-level factors. For instance, financial difficulties were common among SUD patients with DAMA or with Medicaid but not seeking SUD treatment (Ali et al., 2017; Brorson et al., 2013). Thus, more efforts aimed at enhancing SUD treatment benefits in the traditional Medicaid and Medicaid expansion and public SUD treatment systems are needed to reduce DAMA and improve SUD treatment outcomes. Given the opioid crisis, our finding of the high proportion of DAMA among patients with OUD highlights the importance of implementing clinical services (e.g., addiction consultation, treatment linkage services) to improve access to medication-assisted treatment for OUD, treatment retention, or follow-up care (Connery, 2015; Shanahan et al., 2010; Trowbridge et al., 2017).
4.2. Limitations
This study has limitations. The analysis was based on inpatient encounter-level data rather than patient-level data, and patients with repeated treatment admissions could not be identified (HCUP, 2017). The NIS data do not allow the analysis of reasons for DAMA directly as well as provider and system-level factors. In addition, we used 2014 national ACA implementation as a cut-point for DAMA comparison, and we were unable to isolate the Medicaid expansion states before 2014 and control for variations in Medicaid benefits for SUD treatment because NIS cannot be used to support the state-level analysis. In our analysis, we have included variables of the hospital’s region and an indicator of household income quartile to mitigate the potential bias.
5. Conclusions
This study is among the first to examine the potential impact of the ACA on DAMA among hospitalizations for SUDs. The overall findings indicate that despite an increase in the proportion of patients with Medicaid among SUD-involved hospitalizations, no significant change in the proportion of DAMA following the ACA was observed during the study period. Continuous research, training, and outreach efforts are needed to mitigate individual, financial, and structural barriers to admitting SUD treatment and retaining in the treatment, especially among patients on Medicaid or with OUD.
Supplementary Material
Highlights.
Discharge against medical advice (DAMA) increases the morbidity or mortality.
Time series analysis was conducted to examine the national trend in DAMA.
DAMA was common among hospitalizations for substance use disorders.
Hospitalizations for opioid use disorder were most likely to have DAMA.
The Affordable Care Act was not associated the change in DAMA.
Acknowledgments
Role of Funding Sources
This work was made possible by research support from the U.S. National Institutes of Health (UG1DA040317, R01MD007658; PI, Li-Tzy Wu). The sponsoring agency had no further role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: …
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: …
Conflict of Interest
LT Wu has received research funding from Patient-Centered Outcomes Research Institute, Centers for Disease Control and Prevention, Duke Endowment, and Alkermes Inc. H Zhu has no conflict of interest to disclose.
References
- Alfandre DJ, 2009. “I’m going home”: discharges against medical advice. Mayo Clin. Proc 84, 255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham AJ, Andrews CM, Grogan CM, D’Aunno T, Humphreys KN, Pollack HA, Friedmann PD, 2017. The Affordable Care Act transformation of substance use disorder treatment. Am. J. Public Health 107, 31–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali MM, Teich JL, Mutter R, 2017. Reasons for not seeking substance use disorder treatment: variations by health insurance coverage. J. Behav. Health Serv. Res 44, 63–74. [DOI] [PubMed] [Google Scholar]
- Andrews CM, Grogan CM, Westlake MA, Abraham AJ, Pollack HA, D’Aunno TA, Friedmann PD, 2018. Do benefits restrictions limit Medicaid acceptance in addiction treatment? Results from a national study. J. Subst. Abuse Treat. 87, 50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernal JL, Cummins S, Gasparrini A, 2017. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol 46, 348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beronio K, Po R, Skopec L, Glied S, 2013. Affordable Care Act Will Expand Mental Health and Substance Use Disorder Benefits and Parity Protections for 62 Million Americans. U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; http://www.npaihb.org/images/resources_docs/weeklymailout/2013/february/week4/11%20Mental_health_parity_final_19Feb20151%20v5.pdf (accessed January 20, 2018). [Google Scholar]
- Blondell RD, Amadasu A, Servoss TJ, Smith SJ, 2006. Differences among those who complete and fail to complete inpatient detoxification. J. Addict. Dis 25, 95–104. [DOI] [PubMed] [Google Scholar]
- Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F, 2013. Drop-out from addiction treatment: a systematic review of risk factors. Clin. Psychol. Rev 33, 1010–1024. [DOI] [PubMed] [Google Scholar]
- Busch SH, Meara E, Huskamp HA, Barry CL, 2013. Characteristics of adults with substance use disorders expected to be eligible for Medicaid under the ACA. Psychiatr. Serv 64, 520–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connery HS, 2015. Medication-assisted treatment of opioid use disorder: review of the evidence and future directions. Harv. Rev. Psychiatry 23, 63–75. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Wen H, Ritvo A, Druss BG, 2014. Health insurance coverage and the receipt of specialty treatment for substance use disorders among US adults. Psychiatr. Serv 65, 1070–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grogan CM, Andrews C, Abraham A, Humphreys K, Pollack HA, Smith BT, Friedmann PD, 2016. Survey highlights differences in Medicaid coverage for substance use treatment and opioid use disorder medications. Health Aff (Millwood). 35, 2289–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HCUP National Inpatient Sample (NIS), 2017. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD: www.hcup-us.ahrq.gov/nisoverview.jsp. [Google Scholar]
- Heslin KC, Owens PL, Karaca Z, Barrett ML, Moore BJ, Elixhauser A, 2017. Trends in opioid-related inpatient stays shifted after the US transitioned to ICD-10-CM diagnosis coding in 2015. Med. Care 55, 918–923. [DOI] [PubMed] [Google Scholar]
- Humphreys K, 2018. How Medicaid can strengthen the national response to the opioid epidemic. Am. J. Public Health 108, 589–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenne DR, Boros AP, Fischbein RL, 2010. Characteristics of opiate users leaving detoxification treatment against medical advice. J. Addict. Dis 29, 383–394. [DOI] [PubMed] [Google Scholar]
- Linden A, 2015. Conducting interrupted time-series analysis for single-and multiple-group comparisons. Stata J. 15,480–500. [Google Scholar]
- Saloner B, Bandara S, Bachhuber M, Barry CL, 2017. Insurance coverage and treatment use under the Affordable Care Act among adults with mental and substance use disorders. Psychiatr. Serv 68, 542–548. [DOI] [PubMed] [Google Scholar]
- Shanahan CW, Beers D, Alford DP, Brigandi E, Samet JH, 2010. A transitional opioid program to engage hospitalized drug users. J. Gen. Intern. Med 25, 803–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp A, Jones A, Sherwood J, Kutsa O, Honermann B, Millett G, 2018. Impact of Medicaid expansion on access to opioid analgesic medications and medication-assisted treatment. Am. J. Public Health 108, 642–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spooner KK, Salemi JL, Salihu HM, Zoorob RJ, 2017. Discharge against medical advice in the United States, 2002–2011. Mayo Clin. Proc 92, 525–535. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. [Google Scholar]
- Southern WN, Nahvi S, Amsten JH, 2012. Increased risk of mortality and readmission among patients discharged against medical advice. Am. J. Med 125, 594–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tawk R, Freels S, Mullner R, 2013. Associations of mental, and medical illnesses with against medical advice discharges: The National Hospital Discharge Survey, 1988–2006. Adm. Policy Ment. Health 40, 124–132. [DOI] [PubMed] [Google Scholar]
- Ti L, Ti L, 2015. Leaving the hospital against medical advice among people who use illicit drugs: a systematic review. Am. J. Public Health 105, e53–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trowbridge P, Weinstein ZM, Kerensky T, Roy P, Regan D, Samet JH, Walley AY, 2017. Addiction consultation services – linking hospitalized patients to outpatient addiction treatment. J. Subst. Abuse Treat 79, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss AJ, Heslin KC, 2018. Payers of opioid-related inpatient stays and emergency department visits nationally and by state, 2010 and 2015. HCUP Statistical Brief #239 Agency for Healthcare Research and Quality, Rockville, MD: www.hcupus.ahrq.gov/reports/statbriefs/sb239-Opioid-Payer-Hospital-Stays-ED-Visits-by-State.pdf (accessed November 1, 2018). [PubMed] [Google Scholar]
- Wines JD, Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH, 2007. Overdose after detoxification: a prospective study. Drug Alcohol Depend. 89, 161–169. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


