Abstract
Background
The in-hospital treatment of patients with traumatic brain injury (TBI) is considered to be expensive, especially in patients with severe TBI (s-TBI). To improve future treatment decision-making, resource allocation and research initiatives, this study reviewed the in-hospital costs for patients with s-TBI and the quality of study methodology.
Methods
A systematic search was performed using the following databases: PubMed, MEDLINE, Embase, Web of Science, Cochrane library, CENTRAL, Emcare, PsychINFO, Academic Search Premier and Google Scholar. Articles published before August 2018 reporting in-hospital acute care costs for patients with s-TBI were included. Quality was assessed by using a 19-item checklist based on the CHEERS statement.
Results
Twenty-five out of 2372 articles were included. In-hospital costs per patient were generally high and ranged from $2,130 to $401,808. Variation between study results was primarily caused by methodological heterogeneity and variable patient and treatment characteristics. The quality assessment showed variable study quality with a mean total score of 71% (range 48% - 96%). Especially items concerning cost data scored poorly (49%) because data source, cost calculation methodology and outcome reporting were regularly unmentioned or inadequately reported.
Conclusions
Healthcare consumption and in-hospital costs for patients with s-TBI were high and varied widely between studies. Costs were primarily driven by the length of stay and surgical intervention and increased with higher TBI severity. However, drawing firm conclusions on the actual in-hospital costs of patients sustaining s-TBI was complicated due to variation and inadequate quality of the included studies. Future economic evaluations should focus on the long-term cost-effectiveness of treatment strategies and use guideline recommendations and common data elements to improve study quality.
Introduction
Healthcare expenditures are rising worldwide and endanger the affordability of national healthcare systems. [1, 2] To secure their future existence, a thoughtful and righteous distribution of limited resources is essential. Policy makers and healthcare professionals are therefore increasingly expected to study the effectiveness of treatments and its associated costs. [3, 4] After all, the input from high quality cost research is required to make healthcare systems efficient and to achieve the highest quality of care for the lowest costs. [5]
Also in the field of traumatic brain injury (TBI), with an estimated total global annual burden of US$ 400 billion, research efforts are increasingly conducted towards cost- effectiveness. [6–10] After sustaining a TBI, in-hospital treatment is frequently required and generally associated with high costs. [11–14] In the USA, the 2010 TBI-related in-hospital charges totalled US$ 21.4 billion. [15] In-hospital costs after TBI are increasing annually and represent a substantial part of the total financial TBI burden. [15] The highest individual costs in TBI patients are generally seen in patients with severe TBI (s-TBI). [16] These patients also have the longest hospital or intensive care unit (ICU) length of stay (LOS) and the highest number of (neuro)surgical and medical interventions. [16–18] Despite their substantial healthcare consumption, these vulnerable patients show high rates of mortality and unfavourable outcome. Especially for these patients with poor outcome at high costs, a critical appraisal of treatment costs-effectiveness is essential to avoid ineffective expenditures and improve treatment decision-making. [19–22]
Two recent reviews on healthcare costs after TBI have reported about the considerable variation in healthcare costs after TBI between different studies and about the insufficient quality of the available cost studies.[7, 10] These reviews however were mainly focussed on the methodological quality of economic evaluations and therefore did not report the actual in-hospital costs. Insight into in-hospital costs and important components of the costs, such as healthcare utilization and other factors that drive these costs were not provided. This is important information for physicians and policymakers, because this information is needed for decision-making and for correct allocation of resources.
In this systematic review, we have therefore focussed on: (1) providing a detailed insight in the reported in-hospital costs for patients with s-TBI and (2) assessing the (quality of) study methodology.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. [23] (S1 Table) The study protocol was registered in the PROSPERO International Prospective Register of Systematic Review with registration number CRD42018081131.
Literature search
A final systematic literature search was performed on the 8th of August 2018 using the following databases: PubMed, MEDLINE, Embase, Web of Science, Cochrane library, CENTRAL, Emcare, PsychINFO, Academic Search Premier and Google Scholar. The search strategy was developed and conducted with the assistance of a trained clinical librarian. All relevant information on the literature search can be found in S1 Appendix. In addition to the search, the reference lists of all included articles were manually checked for additional relevant studies.
Inclusion/Exclusion criteria
Studies were included when the in-hospital costs or in-hospital charges of a cohort of >10 patients with s-TBI were reported. Because the appellation “severe TBI” encompassed a range of brain injuries considered to be too varied for appropriate comparison the two most widely used classifications for s-TBI were applied: Glasgow Coma Scale (GCS) ≤8 and/or Abbreviated Injury Scale (AIS) ≥4. [24–26] We excluded reviews, commentaries, editorials, conference and meeting abstracts, unpublished data, non-English studies and studies that could not be found or retrieved in full text. Studies were also excluded when in-hospital costs related to acute care were not distinguishable from other costs like indirect non-healthcare related costs (e.g. loss of productivity), (in-hospital) rehabilitation or long-term costs. There were no restrictions on publication date or patient characteristics.
Article selection and data extraction
First, duplicates, non-English and unretrievable records were excluded. Second, two reviewers (JD,MD) independently screened the titles and abstracts of the remaining studies and selected all potential eligible studies. Full-texts were independently reviewed by the same researchers and studies were included according to the above mentioned criteria. During the process, all disagreements were resolved through discussion until consensus or after consulting a third researcher (RO). Data extraction was performed in duplicate using pre-created data extraction sheets. Extracted data was then discussed and combined. Variables that were collected included: study details, study population, definition of TBI (including severity), healthcare consumption, details of costs research methodology and cost outcome results.
Quality assessment
A 19-item checklist was used to assure an accurate quality assessment for the evaluation of in-hospital costs following s-TBI. The checklist was based on the CHEERS statement, which is developed to improve the reporting on economic evaluations. [27–30] We slightly adjusted the items from the CHEERS statement by specifying items like ‘target population and subgroups’ in clear definition of illness and TBI severity, because this was deemed necessary for proper interpretation of study results. Also we intentionally left out items like cost perspective, time horizon and discounting costs since these were considered not relevant for short term in-hospital costs. The final checklist covers items in the areas of study details, population, clinical data, cost data and study methodology. All relevant details can be found in S2 Appendix.
The quality assessment was independently performed by three reviewers (JD, MD, RO). Disagreements were reassessed and discussed in several meetings until consensus was reached. All items were scored according to a predefined scoring manual that included four options: yes (1), suboptimal (0.5), no (0) and not applicable (N/A). A double weight was assigned to several items that were considered to be particularly important in calculating and reporting in-hospital costs. Final scores represented study quality and were presented as a percentage of the maximum score per study. Scores per item and item category were also calculated. All items that were not applicable were excluded from score calculation. When studies used a statistical model, items were scored considering the clear use and description of the model input parameters and sources.
Outcome
All relevant data was reported in a descriptive manner. In line with the inclusion criteria, patients were included from three different severity groups as they were reported in the included studies (GCS≤8, AIS≥4, AIS≥5). These subgroups were also used in the text and figures. In one figure, hospital LOS was presented by using black indicators (■) and ICU LOS by white indicators (□). A clear distinction between hospital costs and hospital charges, when known, was made by using black and white indicators respectively. In-text, both the reported hospital charges and hospital costs were presented as in-hospital costs. The Gross Domestic Product (GDP) per capita of the study country was included as reference value, to improve comparability between the reported costs. The reference year that was used, corresponded with the currency year. [31] All costs, including GDP per capita, were converted to US dollars (2015) using the CCEMG–EPPI-Centre Cost Converter. [32] This web-based tool utilizes Gross Domestic Product deflator index values and Purchasing Power Parities conversion rates provided by the International Monetary Fund. [33] In case a reference year was not provided we used the last year in which patients were included or, when unknown, the year of publication. Figures were designed with GraphPad Prism version 7.0.2.
Results
Literature search and study selection
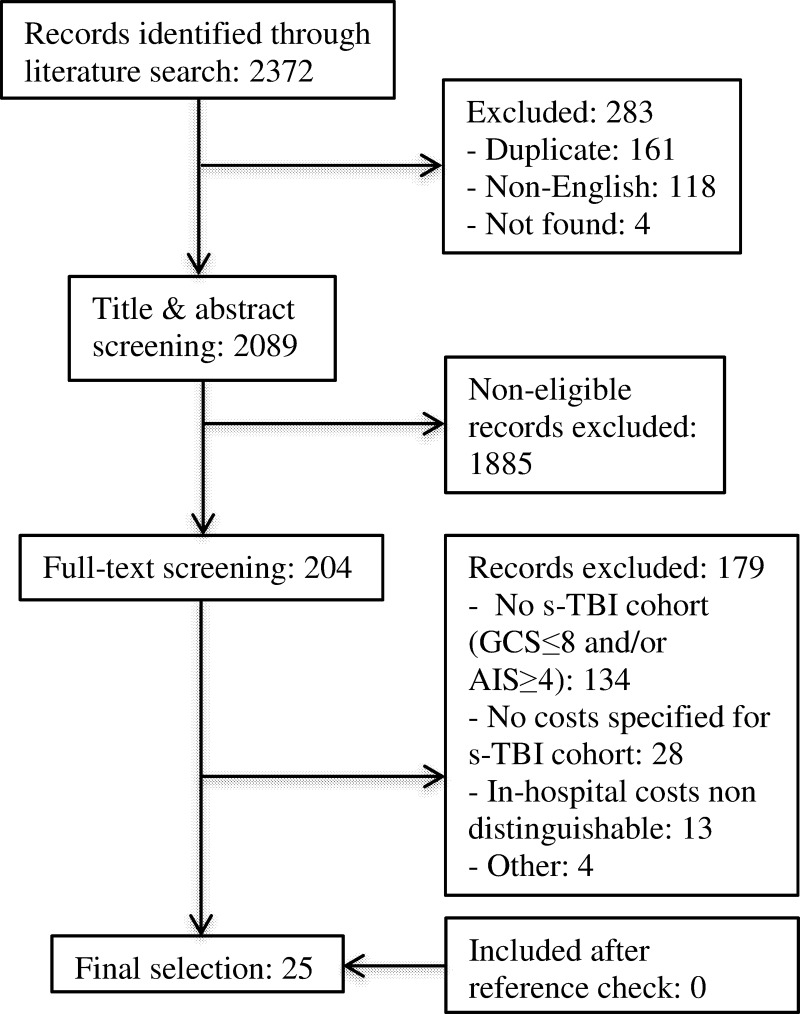
The systematic literature search identified 2372 studies (Fig 1). First, a total of 283 duplicate, non-English or unfindable studies were removed. The remaining 2089 studies were screened on title and abstract, resulting in 204 studies considered eligible for full-text assessment. Studies were excluded because; (1) they did not include a s-TBI cohort defined by a GCS≤8 and/or AIS≥4 (N = 134), (2) they did not report hospital costs for patients with s-TBI (N = 28) or (3) in-hospital acute care costs were not distinguishable from other costs (N = 13). No additional studies were identified through the reference check. Ultimately, 25 articles were included in this systematic review.
Fig 1. Flow chart of the article selection process.
Study characteristics
The main study characteristics can be found in Table 1. Twelve studies were published after 2010, nine between 2000 and 2019, and four before 2000. Cohort size ranged from 20 to 7774 patients. [34, 35] Nineteen studies were conducted in high income countries of which sixteen in the USA. The majority of studies focused on adult patients, while some studies focused on paediatric [34, 36–38] and elderly patients. [35, 39] Nineteen studies (76%) had cost research in TBI patients as a research objective. TBI was often only defined by mentioning “TBI” or “head injury” (N = 9). Six studies provided only little additional information and nine studies used ICD (N = 8) and/or AIS codes (N = 2). Severity was defined by GCS (68%), by AIS (28%) or both (4%). The used GCS was obtained at admission (n = 7), the emergency department (n = 3) and the time remained unknown in 5 studies. A retrospective study design was used in 60% [35–37, 39–50], followed by a prospective design (16%) [34, 51–53] or a combination of both (12%). [54–56] Three studies used a statistical model. [38, 57, 58]
Table 1. Study details & results.
| # | Study info a | Purpose | Study Design | Patient (N) | Definition of TBI | Severity definition | Cost data source | Details on cost calculation | Included costs | Currency (Y) / GDP per capita b | Results ($ 2015) c (% of GDP per capita) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | -Ahmed [40] -2007 -2002–2005 -USA |
Evaluate the impact of early tracheostomy on s-TBI patients | Retrospective cohort study | 55 s-TBI |
TBI, not further specified | GCS≤8 at admission | Hospital accounting database | NP, most likely directly obtained from database | Total hospital charges | US$ (NP) / $52,876 | ET (GCS 4.3±1.9): median $348,858 (660%) (95% CI: $293,682-$468,908) LT (GCS 4.5 ±1.8): median $396,917 (751%) (95% CI: $334,441-$520,808) |
| 2 | -Albrecht [39] -2017 -2008–2012 -USA |
Provide charge estimates of TBI treatment for elderly patients | Retrospective cohort study | GCS<9:247 AIS4:688 AIS5:368 |
ICD-9-CM codes | GCS<9 at admission, AIS>3 | Finance and billing department of (trauma) hospital and university | NP, most likely directly obtained from database | Hospital and physician charges. (Cost-to-charge ratio: 140.65%). | US$ (2012) / $53,681 | GCS <9: $58,899 (110%) ± $74,194 AIS 4: $37,503 (70%) ± $58,025 AIS ≥5: $59,146 (110%) ± $87,230 |
| 3 | --Andelic [57] --2014 -2005–2007 -Norway |
Estimate long-term cost-effectiveness of rehabilitation trajectories | Decision-tree model | 59 s-TBI | ICD-10 codes | GCS≤8 before intubation | Expected costs calculated from a reimbursement system using diagnosis related groups (DRG) | DRG reimbursement multiplied by the DRG cost weight for each patient | Total acute hospitalization costs for first 5 years post-injury | NOK (2009) / $87,894 | All: $112,808 (128%) ± $68,327 Trajectory 1: $123,526 (141%) ± $50,911 Trajectory 2: $101,822 (116%) ± $81,725 |
| 4 | -Brooks [41] -1995 -1989–1990 -USA |
Determine the costs of health care services for TBI patients | Retrospective cohort study | 28 s-TBI | TBI with AIS>0 | AIS 4 and 5 |
Charges are obtained directly from all service providers | Services and billing records were added up to calculate actual/ estimated charges | Initial care charges including EMS, acute care charges and physicians charges of initial hospitalization | US$ (1993) / $40,211 | Acute care: $123,303 (307%) Physicians: $25,767 (64%) Emergency Medical Services (EMS): $1,855 (5%) |
| 5 | -Bryant [42] -1993 -NP -USA |
Find a high-quality cost- effective strategy for head injury rehabilitation | Retrospective cohort study | 47 s-TBI | TBI, not further specified | GCS≤8 in ED | Costs are estimated from financial records of the health maintenance organization (HMO) | Unit costs are multiplied by utilized services | Acute medical care costs using actual operational costs. | US$ (NP) / $40,211 | All: $24,205 (60%) |
| 6 | -Fakhry [43] -2004 -1991–2000 -USA |
Determine effect of following BTF guidelines on outcome and charges | Cohort study with historical controls | 830 s-TBI | TBI defined as blunt traumatic head injury with AIS-head > 2 | GCS≤8 | Trauma registry and individual chart review | NP, most likely directly obtained from registry of charts | Total charges (hospital room, critical care, nursing services, direct and indirect expenses, general hospital charges) | US$ (1997) / $44,428 | 1991–1994 (GCS 4.0): $51,634 (116%) 1995–1996 (GCS 3.5): $42,558 (96%) 1997–2000 (GCS 3.5): $40,002 (90%) |
| 7 | -Farhad [44] -2013 -1993-1994/ 2006–2007 -USA |
Compare TBI-related hospitalization outcomes between 2 periods | Retrospective analysis of NIS data | 317/ 288 s-TBI |
ICD-9-CM codes | ICD/AIS 4–6 | National Inpatient Sample (NIS) database (1993-1994/ 2006–2007) | NP, most likely directly obtained from database | Total charges of hospitalization | US$ (2006–2007) / $53,764 | 1993–1994: $21,427 ± $21,315 corrected for inflation: $29,999 (56%) 2006–2007: $65,002 (121%) ± $60,900 |
| 8 | -Graves [36] -2016 -2007–2011 -USA |
Evaluate guideline adherence on outcome and costs for paediatric s-TBI patients | Retrospective cohort study | 235 s-TBI | ICD-9 codes, head AIS ≥ 3, history of trauma, abnormal admission head CT scan | GCS≤8 at admission | Total charged amounts most likely from hospitals, CCR from HCUP-KID or institution’s billing office | Obtained charges converted to costs with institution specific cost-charge ratio (CCR) | Total costs of hospitalization + ICU care | US$ (2012) / $53,681 | Hospital mean: $106,969 (199%) (95% CI: $96,355 - $117,582) ICU mean: $84,843 (156%) (95%CI: $76,364 - $93,322) |
| 9 | -Ibrahim [51] -2007 -2003 --Malaysia |
CEA of two neuro monitoring modalities in s-TBI management | Prospective observational CEA study | 62 s-TBI | Severe head injury, traumatic in nature, not further specified | GCS≤8 and CT-scan features | All treatment costs measured using budget information | Macro and micro costing approach | Only direct provider costs calculated during admission | US$ (2002) / $5,379 | Group 1 (GCS median 5.5, IQR 2.0): $10,356 ± $6,526 (121%) Group 2 (GCS median 6.0, IQR 2.0): $11,646 ± $8,168 (152%) |
| 10 | -Jaffe [34] -1993 -1987–1988 -USA |
Assess acute and rehab costs of paediatric TBI patients | Prospective cohort study |
20 s-TBI | Non-penetrating TBI with loss of consciousness | GCS≤8, at ED or before paralyzing agents | Hospital/physician charges from hospitals and physicians billing office | NP, most likely directly obtained from billing office | Charges used as proxy for costs. Initial acute care | US$ (1988) / $38,048 | GCS3-8: $93,934 (247%) (range: $8,881–$328,857) AIS4: $32,375 (85%) ($16,378- $81,852) AIS5: $145,573 (383%) ($36,096-$328,857) |
| 11 | -Lehmkuhl [54] -1993 -1989–1992 -USA |
Investigate factors that influence hospital charges for persons with TBI | Retrospective and prospective cohort study | 111 s-TBI, 108 vs-TBI |
TBI, defined as brain tissue damage caused by external force | GCS≤8, lowest score in first 24 hours | Copy of final billed charges submitted to designated payer | NP, most likely the submitted charges | Hospitalization costs (billed charges) for acute care excluding physicians fee | US$ (1989–1992) / $45,150 | GCS6-8: $90,291 (200%) ± $72,243 GCS3-5: $141,813 (314%) ± $84,216 |
| 12 | -Li [35] -2017 -2001–2007 -China |
Epidemiological characteristics of elderly TBI patients | Retrospective analysis of Chinese Trauma Database data | 5238 s-TBI 2536 c-TBI |
ICD-9-CM codes | AIS4: severe AIS5-6: critical |
Chinese Trauma Database dataset. | NP, most likely directly obtained from dataset | Hospitalization costs | US$ (NP) / $3,039 |
AIS4: $2,130 (70%) ± 3,881 AIS5-6: $3,586 (118%) ± 5,384 |
| 13 | -Martini [45] -2009 -2004–2007 -USA |
Resource utilization of brain tissue oxygen monitoring | Retrospective cohort study | 629 s-TBI | TBI, not further specified | GCS≤8 at admission | Hospital administrative records | Charges converted to costs with institution specific CCR | Hospital costs | US$ (2007) / $54,204 | Group 1 (GCS 5.6 ±2.3): $116,387 (215%) ± $85,034 Group 2 (GCS 5.1±2.2): $143,453 (265%) ± $88,079 |
| 14 | -McGarry [46] -2002 -1997–1999 -USA |
Examine treatment outcomes and costs of TBI | Retrospective analysis of database | 2580 s-TBI 1147 c-TBI |
ICD-9-CM codes | ICD/AIS4: severe ICD/AIS5: critical |
Billed charges from a large multihospital database | Charges converted to costs with CCR | Hospitalization costs of acute treatment | US$ (1999) / $47,467 | AIS4: $23,017 (48%) AIS5: $45,981 (97%) |
| 15 | -Morris [47] -2008 -2000–2005 -England/Wales |
Investigate cost of care for hospitalised TBI patients | Retrospective analysis of database | 2460 s-TBI 2573 c-TBI |
TBI defined using 1998 AIS codes | AIS4: severe AIS5: critical |
Trauma Audit and Research Network database and reference unit costs from different sources | Resource use from database and unit count multiplied by unit costs for other costs | National Health Service hospital costs | £ (NP) / $49,803 | AIS4: $16,110 ± $30,088 (60%) AIS5: $29,504 ± $29,944 (60%) |
| 16 | -Palmer [55] -2001 -1994–1999 -USA |
Report impact of TBI guideline implementation on outcome in s-TBI patients | Cohort study using retro- and prospective data | 93 s-TBI | Closed head injury and evidence of brain injury on examination or CT-scan | GCS≤8 at admission | Patient records and/or financial data | NP, most likely directly obtained from records or financial data | Hospital charges | US$ (NP) / $47,467 | Before implementation (GCS 6.4±0.7): $268,902 (567%) ± $31,761 After implementation (GCS 6.9±0.5): $401,808 (846%) ± $27,364 |
| 17 | -Prang [48] -2012 -1995–2004 -Australia |
Describe details of care services after transport related TBI | Analysis of a compensation database | 316 s-TBI | Transport related-TBI, not further specified. | GCS3–8: severe |
Accepted claims from Compensation Research Database | Mean costs calculated for each service category | Direct cost of healthcare over 5-year period post-injury | AUD $ (2009) / $46,885 | Acute hospital services: $45,384 (98%) ± $38,720 |
| 18 | -Salim [52] -2008 -2000–2004 -USA |
Evaluate outcome of ARDS in patients with s-TBI | Prospectively collected cohort in ARDS dataset | 28 s-TBI+ ARDS 56 s-TBI |
Blunt trauma patients with TBI, AIS defined. | Head AIS ≥ 4 | Hospital’s trauma registry | NP, most likely directly obtained from trauma registry | Hospital charges | US$ (NP) / $51,638 | TBI+ARDS group (GCS 4±2): $258,790 (501%) ± $296,186 TBI group (GCS 5±2): $142,074 (275%) ± $198,248 |
| 19 | -Schootman [49] -2003 -1996 -USA |
Hospitalization charges for acute care in TBI patients in the USA | Population based descriptive study | 1789 s-TBI | ICD-9-CM codes | ICD/AIS 4–6 | National Inpatient Sample (NIS) of 1996 | Database contains patient-level clinical and resource use information | Hospitalization billed charges for acute care | US$ (1996) / $43,035 | Mean $47,004 (109%) ± $3,238; Median $20,886 |
| 20 | -Siddiqui [56] -2015 -2002–2009 -Pakistan |
Identify impact of early tracheostomy in s-TBI patients | Cohort study using retro- and prospective data | 100 s-TBI | TBI, not further specified | GCS<8 | Institution’s billing department | NP, most likely directly obtained from billing department | Inpatient treatment costs (ED, ICU, ward, lab, imaging, surgery) | US$ (2009) / $1,105 | Group 1 (GCS 5.4±1.7): $8,811(797%) Group 2 (GCS 6.0±1.7): $10,934 (990%) |
| 21 | -White [37] -2001 -1991–1995 -USA |
Determine predictors in paediatric s-TBI patients | Retrospective cohort study | 136 s-TBI | Non-penetrating head injury, not further specified | GCS≤8 at admission to ED | NP: “were available” | Charges converted to costs using hospital based CCR | Hospitalization costs | US$ (1998) / $45,866 | Survivors (GCS 5.4±1.9): $12,247 (27%) ($2,199-$127,555) Non-survivors (GCS 3.4±0.8): $7,081 (15%) ($2,305-$32,622) |
| 22 | -Whitmore [58] -2012 -N/A -USA |
Determine the cost-effectiveness of treatment strategies in s-TBI patients | Decision-analytical model | N/A | TBI, not further specified | GCS≤8 and motor component of ≤5 at admission | Obtained from literature and Medicare reimbursement rates | Cost calculations follow general principles earlier described in literature and methods section | Direct acute medical care costs, primarily associated with the initial hospitalization | US$ (2011) / $52,910 | Comfort care: GOS1: $60,582 (115%) GOS2-3: $111,067 (210%) GOS4-5: $43,753 (83%) Routine care: GOS 1: $77,410 (146%) GOS 2–3: $136,309 (258%) GOS4-5: $52,167 (99%) Aggressive care: GOS1-5: $124,725 (236%) |
| 23 | -You [50] -2018 -2015–2016 --Malaysia |
Assign costs to treatment of surgically treated patients with TBI | Retrospective cohort study | 26 s-TBI | ICD-10 codes | GCS3-8 on presentation | Hospital revenue department, finance department and financial reports | Micro- and macro- costing methods. Activity units multiplied by unit costs | Total cost of treatment (including hospitalization, surgery and investigations) | US$ (2016) / $9,416 | GCS3-8: $8,964 (95%) ± $5,753 |
| 24 | Yuan [53] -201) -2004 -China |
Acute treatment costs for TBI | Prospective observational multicentre study | 2500 s-TBI | TBI diagnosis was made by admitting neurosurgeons or ER physicians and confirmed by CT | GCS≤8 at admission | Unsubsidized total hospital billings | NP, most likely directly obtained from hospital billings | Total acute hospitalization treatment costs | US$ (2004) / $1,859 | GCS3-8: median $3,115 (168%) ($1,468 - $6,046) Isolated TBI: $2,844 (153%) TBI with other injury: $3,207 (173%) |
| 25 | -Zapata-Vazquez [38] -2017 -N/A --Mexico |
Cost-effectiveness of ICP monitoring in paediatric s-TBI patients | Decision-tree model | Based on 33 s-TBI patients | TBI, not further specified |
GCS3-8 | Most costs taken from official journal of the federation. Medicine price catalog, ICP probe price provided by supplier. | Amount of supplies multiplied by unit price | Costs of hospitalization (direct medical costs + clinical complications) medicines, laboratory, imaging, surgery, LOS ICU/Ward. | Mex$ (2015) / $9,291 | ICP monitoring group (GCS 5.5±1.7): $66,263 (713%) ± $31,436 Control group (GCS 7.0±1.5): $41,783 (450%) ± $10,622 |
AIS, Abbreviated Injury Scale; ARDS, Adult Respiratory Distress Syndrome; BTF, Brain Trauma Foundation; CCR, Cost to Charge Ratio; CEA, Cost Effectiveness Analysis; CT, Computed Tomography; c-TBI, critical TBI; DRG, Diagnosis Related Groups; ED: Emergency Department; EMS, Emergency Medical Services; ET, Early Tracheostomy; GCS, Glasgow Coma Scale; HCUP-KID, Healthcare Cost and Utilization Project—Kids’ Inpatient Database; HMO, Health Maintenance Organization; ICD-10, International Classification of Diseases, 10th Revision; ICD-9-CM, International Classification of Diseases, Ninth Revision; ICP, Intracranial Pressure; ICU, Intensive Care Unit; LOS, Length of Stay; LT, Late Tracheostomy; N/A, not applicable; N, Number; NIS, National Inpatient Sample; NP, Not provided; s-TBI, severe Traumatic Brain Injury; TBI, Traumatic Brain Injury; vs-TBI, very severe Traumatic Brain Injury; Y, Year
a Name first author [reference #]—year of publication—Cohort inclusion period—Study country.
b GDP per capita from year of currency and converted to $ 2015.
c When available, severity defined by GCS was further specified by adding the mean GCS ± SD. (Unless stated otherwise)
Quality of study methodology
The results of the quality assessment are presented in detail in S2 Table. Study quality was variable with an average total score of 71% and a range of 48% to 96%. Seven studies achieved a score above 80%, representing “high quality”. [36, 38, 39, 47, 50, 53, 58] Especially items in the ‘cost data’ subgroup scored poorly (49%). All but one study mentioned their cost data source, but a clear description was missing in 24%. Also, the design and methods of costs analysis were not mentioned in 36% and were unclear in another 16%. Eleven studies properly assessed hospital activity data but only three studies appropriately valued and reported unit costs. Hospital costs were disaggregated in 20% of studies and in 52% charges were reported instead of costs. Major assumptions were tested in a sensitivity analysis in only 16% and a reference year was missing in 14% of the studies. The subgroups ‘study details’, ‘population’ and ‘methodology’ had the highest scores (100%, 87% and 78%). There were infrequent statements on source of funding and conflicts of interest, unsatisfying TBI definitions and inadequate evaluation of study findings.
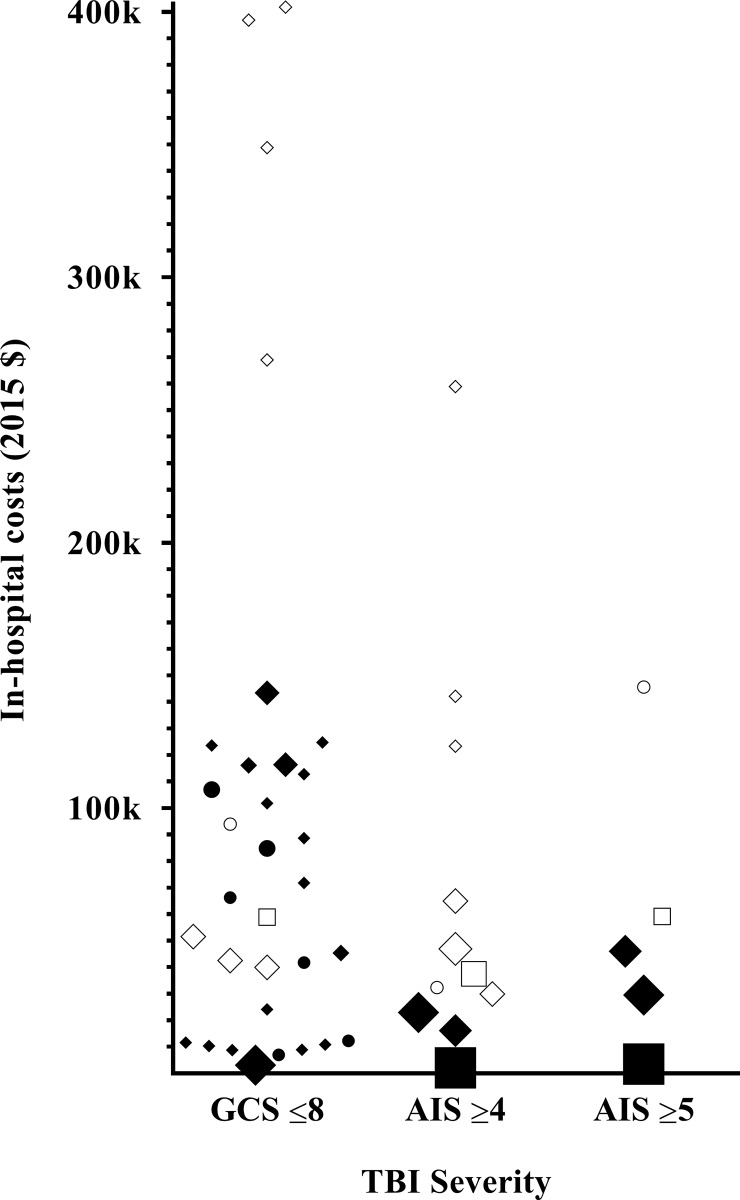
Hospital costs & healthcare consumption
The median reported in-hospital costs per patient were $55,267 (mean $87,634) and ranged from $2,130 to $401,808 (Fig 2). The lowest costs were seen in studies from China, Pakistan and Malaysia ($2,130 to 10,356) [35, 50, 51, 53, 56] and in a subgroup of paediatric non-survivors in the USA ($7,081). [37] The highest in-hospital costs ($258,790 to $401,808) were found in three studies describing different patient cohorts from the USA. [40, 52, 55] The in-hospital costs as percentage of the GDP per capita (median 128%, mean 234%) were highly variable and ranged from 15% to 990%. [37, 56] Mean percentages were not significantly different between high and lower income countries and between charges and costs (204% vs. 333% and 289% vs. 202%).
Fig 2. In-hospital costs and in-hospital charges of a patient with s-TBI.
Black indicators represent in hospital costs, while white indicators represent in-hospital charges. A bigger indicator size, represents a bigger study cohort size. ● ○: Paediatric ♦ ◊: Adult ■ □: Elderly.
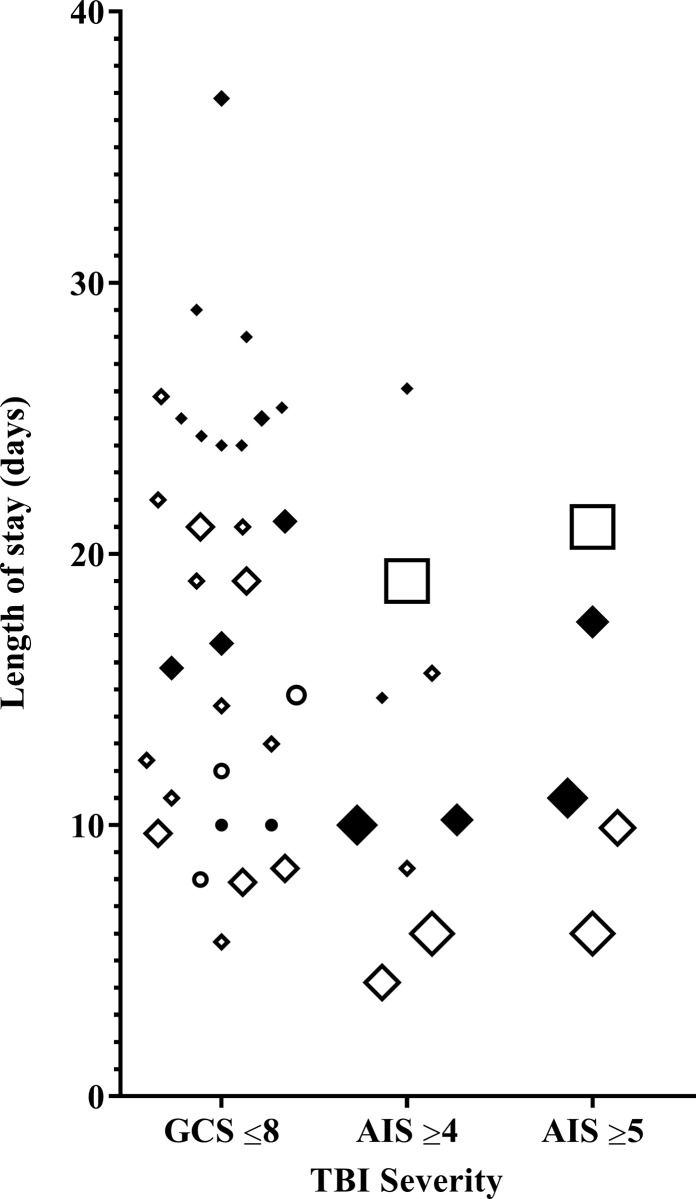
Fourteen studies reported LOS for patients with s-TBI, also showing major variation (Fig 3). [35, 36, 38, 40, 43, 45–47, 50–52, 54–56] ICU LOS ranged from 7.9 to 25.8 days (GCS≤8) [40, 43], 6 to 19 days (AIS≥4) and 6 to 21 days (AIS≥5). [35, 47] Hospital LOS ranged from 10 to 36.8 days (GCS≤8) [38, 54], 10 to 26.1 days (AIS≥4) [47, 52] and 11 to 17.5 days (AIS≥5). [46, 47]
Fig 3. ICU and hospital length of stay of a patient with s-TBI.
Black indicators represent hospital length of stay, while white indicators represent ICU length of stay. A bigger indicator size, represents a bigger study cohort size. ● ○: Paediatric ♦ ◊: Adult ■ □: Elderly.
Some studies reported costs related to acute care to be 46% to 67% of total hospitalization costs, while inpatient rehabilitation costs accounted for 26% to 41%. [41, 42, 54, 57] Various studies found that costs related to hospital LOS and ICU LOS were the main drivers of hospital costs. [36, 38, 39, 47, 50, 53] Costs related to ICU care comprised the biggest part of total hospital costs (51–79%), followed by costs related to ward admission (12–38%), surgery (4–8%) and imaging/laboratory (<3%). [36, 38, 47] Physician charges were reported to be 12% to 20% of total costs. [39, 41] One study included the salary of paramedics and found salary to be the most important contributor (71–79%) to total provider costs. [39, 41, 51] The majority of costs, up to 90%, were made in the first year after trauma and were generally associated with TBI-related hospitalization costs. [41, 48, 57] The share of acute hospital services (18%) and rehabilitation (27%) on total costs decreased when a long-term follow-up period was used. [52]
Several studies provided some additional information on clinical factors that were associated with reported costs. A higher TBI severity was generally related with an increased LOS and costs. [34, 35, 37–39, 41, 42, 46–50, 53, 54] Even among patients with a s-TBI, patients with a GCS3-5 or AIS = 5 were more expensive than patients with a GCS6-8 or AIS = 4, respectively. [34, 35, 39, 40, 46, 47, 54] A higher overall injury severity was also related with higher costs. [39, 47, 53] Male gender was linked with higher costs [35, 39, 53] and two studies mentioned that a higher age was more expensive. [47, 50] Costs were also influenced by trauma mechanism and were higher for motor vehicle accidents and gunshot wounds and lower after an assault to the head. [34, 35, 39, 46, 53, 54] The use of surgical intervention, intracranial pressure monitoring or mannitol were all related to longer LOS and higher costs. [37, 38, 45, 53, 54] Also, the introduction of guidelines and evidence based medicine protocols appeared to increase LOS and hospital costs [43, 55], while improvement of guideline adherence did not change ICU and hospital costs in another study. [36] Three studies related costs to outcome and found lower costs for patients that died or made a good recovery. [37, 53, 58]
Discussion
This systematic review demonstrates that the in-hospital costs related to acute care for patients with s-TBI are generally high and increase with severity of TBI and overall severity of the injury. Both healthcare consumption and in-hospital costs are highly variable between studies and associated with factors such as mechanism of injury and treatment strategy.
Three previous reviews on costs after TBI were generally in line with our results, but results were difficult to compare with the present review due to differences in study objectives and substantial variation between the included studies that was mainly caused by differing methodological and clinical characteristics. [7, 59, 60] Elaborating on these reviews, we specifically investigated the in-hospital costs related to acute care for patients with s-TBI aiming to reduce variation and improve study comparability. Methodological and clinical heterogeneity remained present, likely contributing to the variation in in-hospital costs between studies. The highest in-hospital costs were found in studies from the USA that reported charges instead of costs. Because hospital charges are not actual costs and usually higher than hospital costs, this increased total amounts. Charges are also often non-transparent and the resultant of deals between hospitals and insurance companies or other stakeholders. It is therefore preferred to calculate and report total costs by using healthcare utilization with its corresponding unit costs. Also, USA healthcare expenditures are twice as high as expenditures in other high-income countries. [2, 61] While healthcare utilization patterns were rather similar between high-income countries, the higher expenditures were especially caused by higher prices of labour, goods, pharmaceuticals and administrative costs. [2, 62] Large international differences were also seen between European countries when assessing injury related hospitalization costs. [63] Likewise, the lowest in-hospital costs were found in studies from lower-income countries, which is also in accordance with literature. [64] These absolute costs are lower because of lower prices, lower treatment intensity and higher mortality rates with associated lower resource utilization. [64, 65] In-hospital costs reported as percentage of GDP per capita were however not significantly different between high and low income countries, suggesting a similar financial impact for patients. Differences in costs might also be caused by hospital associated factors (e.g. level of trauma center, volume, treatment protocols) and by the major epidemiological differences of trauma populations between countries. [6] The different timeframes included in this review could also contribute to variation, since treatment strategies have changed over time and healthcare costs have been increasing globally over the years. [15, 64, 66] Comparing in-hospital costs from different healthcare systems in different timeframes is therefore problematic.
As in literature, the identified in-hospital costs increase with higher TBI severity. [9, 16, 60, 67] Costs increase because they primarily consist of costs related to LOS and surgical interventions and because the utilization of both is higher in more severely injured TBI patients. [68–71] After all, healthcare expenses are equal to utilization multiplied by associated prices. [62] Also in other studies, physician charges are another important contributor to in-hospital costs. [2, 72] Length of stay results and its variability seemed to be in accordance with literature, but were difficult to compare due to this variation. [68, 69] Like in previous research, extracranial injuries and overall injury severity contributed to higher healthcare consumption and in-hospital costs. [67, 69, 73–75] Distinguishing costs that are related to TBI or associated extracranial injuries is nearly impossible. Therefore, four studies explicitly investigated patients with isolated-TBI. [44, 51, 53, 56] Motor vehicle accidents and gunshot wounds were reported to be related to higher costs, most likely because of higher injury severity and accompanying extracranial injuries. Although a higher age is often considered to be more expensive, only few studies mentioned this and comparison between the age groups did not show obvious differences in LOS or in-hospital costs. [15, 63, 67, 73]
Hospital and acute care costs were reported to be important constituents of total costs followed by in-patient rehabilitation. However, the limitations of a short follow-up period have been recognized before. [7] Although the in-hospital costs are obviously an important part, post-discharge rehabilitation and other long term care costs are also major contributors to the total costs after TBI. [12] When including the enormous long-term or lifetime costs and the loss of productivity, the share of in-hospital costs on the total burden significantly decreases. [12, 14, 76] A long-term follow up period would provide a better overview for two reasons. First, the assessment of patient outcome will be more accurate, because health problems might persist, improve or deteriorate several years after trauma. [77, 78] Second, the cost analysis will be more comprehensive, since a changing health situation influences healthcare consumption and productivity for both patients and relatives. Therefore, especially for establishing the cost-effectiveness of treatments, a long-term follow-up should be included.
The identified most important reasons for (outcome) variation were probably all caused by different study objectives. Study objectives determined study methodology and consequently also the studied participants, interventions and outcome. Although most study objectives included costs research, the major differences between them likely caused the aforementioned methodological and clinical heterogeneity. Heterogeneity has earlier been reported for TBI cost studies and complicates study comparison and outcome interpretation. [7, 10, 59, 60] Heterogeneity is not limited to TBI cost research, but is very common in general TBI research and likewise complicates comparability, generalizability and interpretation of other studies. [79–82]
Study quality also influenced interpretation of study results, since poor methodological quality compromises quality and therefore value of data. Two recent reviews specifically assessed the methodological quality of TBI cost evaluation studies and identified important limitations regarding the adherence to the methodological principles of economic evaluations. [7, 10] More specifically, these limitations include not reporting all relevant costs on a long-term or lifetime horizon, not discounting future costs, not performing incremental analysis of cost-effectiveness and applying sensitivity analysis. Our quality assessment found variable and overall inadequate study quality. Only few studies were considered high quality and especially items concerning the calculation and reporting of costs scored poorly. Cost results were often provided without relevant context. A description of costs analysis methods, required to understand and interpret the results, was frequently missing. Studies also rarely calculated in-hospital costs by transparently multiplying healthcare consumption with associated unit costs. Almost no study reported the highly informative and important disaggregated costs. Even reference years were missing in several studies. Because several studies did not focus on reporting costs after TBI, they might have scored low on our quality assessment, despite appropriately investigating their specific study objectives.
Strengths and limitations
This systematic review benefits from an extensive literature search in multiple databases and strict inclusion criteria, which improve study comparability and interpretation of results. The PRISMA guidelines were used during the review process and the quality assessment made use of a checklist that was based on the CHEERS statement and allowed the critical appraisal of the included articles. Although the assignment of scores is partly subjective, our experiences regarding the quality assessment using this checklist were positive. In addition, this is by our knowledge, the first detailed overview of in-hospital costs in patients with s-TBI.
This study also has several limitations. The article selection criteria resulted in the exclusion of some patients, that were severely injured but lacked the required severity classification. Also, regarding in-hospital costs, studies were excluded that not clearly distinguished acute care in-hospital costs from rehabilitation costs, indirect costs or other non in-hospital costs. Data from these patients could have contributed to our results, but the introduction of additional methodological and clinical heterogeneity would have compromised comparability and interpretation of study results. In addition, the used TBI severity criteria have their limitations. The GCS has been criticized for its general applicability although it shows adequate reliability in a recent review. [24, 83] A patient can be scored ‘false-low’ due to intubation and sedation overestimating injury severity, while the severity of patients who quickly deteriorate after admission will be underestimated. Also, a decreased GCS is not always caused by TBI and could also be caused by extracranial injury alone. [84] Last, patients could be at the lower or the higher end of the spectrum within the GCS 3–8 group. This could have substantial impact on study results, because severity is related to costs. Regarding AIS, the classification system changed over time and the 2005 version codes similar injuries with a lower severity score compared to the 1998 version. [85] Also, some researchers suggest using AIS≥5 as severe, instead of AIS≥4. [86] Despite this, using both criteria is very relevant because they are the most widely used criteria for s-TBI. [24] Limiting the selection to patients with s-TBI improves comparability, but fails to assess the financial burden caused by minor and/or moderate TBI. Although individual costs are lower for these injuries, the total burden on society is much higher because of their more frequent occurrence. [16] Although the distinction is clearly made throughout, including hospital charges and hospital costs may have compromised comparability of study results. Since both are frequently reported, it did however make a comprehensive review of in-hospital expenses possible and points out the difficulty of cost research. Last, the focus on in-hospital costs, dramatically underestimated the total financial burden caused by s-TBI. [12, 14, 76]
Future research
Because a righteous and ethical distribution of limited healthcare resources is essential to secure the future existence of successful healthcare systems around the world, policymakers increasingly request high quality evidence regarding the cost effectiveness of treatments. [3] To improve the future quality of TBI cost research, investigators should equalize methodological and clinical heterogeneity by using specific methodological guidelines and common data elements. [27, 87] As seen in this systematic review, one of the biggest challenges in TBI cost research is heterogeneity. Checklists could be helpful, but the development of international guidelines on economical evaluations for TBI patients is preferred. Patient outcome should be investigated along with the financial burden of treatments. Therefore, cost-effectiveness analysis should be included in upcoming trials investigating TBI treatment strategies. Patients from all ages should be investigated because all are confronted with the consequences of TBI. Because TBI related consequences and associated costs are variable over time, economic evaluations should include a long-term or even lifetime horizon. [6] All associated costs adding to the total burden on society, like indirect costs and loss of productivity, should be included to accurately map expenditures. Also, health and financial implications for family and proxies deserve investigation. Last, the use of accurate cost calculation methods using exact healthcare consumption and cost price data could further improve the accuracy of cost calculations and thus outcome results. [88, 89]
Conclusions
We conclude that healthcare consumption and in-hospital costs for patients with s-TBI are generally high. In-hospital costs mostly consist of costs related to LOS and surgical interventions. The major variation of study results is primarily caused by methodological and clinical heterogeneity. Study quality was variable but often inadequate and especially items considered important in calculation and reporting of in-hospital costs scored poorly. High quality future economic evaluations could guide physicians and policy-maker in improving clinical decision-making and resource allocation. Studies should therefore focus on the long-term cost-effectiveness of treatments and improve both study quality and equality by using guidelines and common data elements.
Supporting information
(DOCX)
(DOCX)
N/A: Not applicable.
(DOC)
* Item scores with double weight.
(DOCX)
Acknowledgments
We would like to thank Jan Schoones for his assistance in developing and conducting the search strategy.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This study was supported by The European Union seventh Framework Program (https://ec.europa.eu/research/fp7/index_en.cfm) (grant 602150) for Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) and Hersenstichting Nederland (Dutch Brain Foundation) (https://www.hersenstichting.nl/) for Neurotraumatology Quality Registry (Net-QuRe). The funders had nu role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Xu K, Soucat A, Kutzin J, Brindley C, Dale E, Van de Maele N, et al. New perspectives on global health spending for universal health coverage Geneva: World Health Organization. 2018;(WHO/HIS/HGF/HFWorkingPaper/18.2) Licence: CC BY-NC-SA 3.0 IGO:1–44.
- 2.Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. Jama. 2018;319(10):1024–39. Epub 2018/03/15. 10.1001/jama.2018.1150 . [DOI] [PubMed] [Google Scholar]
- 3.Health. DMo. Kamerbrief over beeindiging 'sluis' nivolumab per 1 maart 2016 2016 [22 June 2018]. Available from: https://www.rijksoverheid.nl/documenten/kamerstukken/2016/01/28/kamerbrief-over-beeindiging-sluis-nivolumab-per-1-maart-2016.
- 4.Porter M, Lee T. The strategy that will fix health care. Harv Bus Rev. 2013;91(10). [Google Scholar]
- 5.Porter ME. A strategy for health care reform-toward a value-based system. N Engl J Med. 2009;361(2):109–12. Epub 2009/06/06. 10.1056/NEJMp0904131 . [DOI] [PubMed] [Google Scholar]
- 6.Maas AIR, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. The Lancet Neurology. 2017;16(12):987–1048. Epub 2017/11/11. 10.1016/S1474-4422(17)30371-X . [DOI] [PubMed] [Google Scholar]
- 7.Alali AS, Burton K, Fowler RA, Naimark DM, Scales DC, Mainprize TG, et al. Economic evaluations in the diagnosis and management of traumatic brain injury: a systematic review and analysis of quality. Value in health: the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2015;18(5):721–34. Epub 2015/08/25. 10.1016/j.jval.2015.04.012 . [DOI] [PubMed] [Google Scholar]
- 8.Alali AS, Naimark DM, Wilson JR, Fowler RA, Scales DC, Golan E, et al. Economic evaluation of decompressive craniectomy versus barbiturate coma for refractory intracranial hypertension following traumatic brain injury. Crit Care Med. 2014;42(10):2235–43. Epub 2014/07/24. 10.1097/CCM.0000000000000500 . [DOI] [PubMed] [Google Scholar]
- 9.Ho KM, Honeybul S, Lind CRP, Gillett GR, Litton E. Cost-effectiveness of decompressive craniectomy as a lifesaving rescue procedure for patients with severe traumatic brain injury. The Journal of trauma. 2011;71(6):1637–44. Epub 2011/12/21. 10.1097/TA.0b013e31823a08f1 WOS:000298616400035. [DOI] [PubMed] [Google Scholar]
- 10.Lu J, Roe C, Aas E, Lapane KL, Niemeier J, Arango-Lasprilla JC, et al. Traumatic brain injury: methodological approaches to estimate health and economic outcomes. Journal of neurotrauma. 2013;30(23):1925–33. Epub 2013/07/25. 10.1089/neu.2013.2891 . [DOI] [PubMed] [Google Scholar]
- 11.Faul M, Xu L, Wald M, Coronado V. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths, 2002–2006. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010:1–74. [Google Scholar]
- 12.Scholten AC, Haagsma JA, Panneman MJ, van Beeck EF, Polinder S. Traumatic brain injury in the Netherlands: incidence, costs and disability-adjusted life years. PLoS One. 2014;9(10):e110905 Epub 2014/10/25. 10.1371/journal.pone.0110905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Altes A, Perez K, Novoa A, Suelves JM, Bernabeu M, Vidal J, et al. Spinal cord injury and traumatic brain injury: a cost-of-illness study. Neuroepidemiology. 2012;39(2):103–8. Epub 2012/08/01. 10.1159/000338297 . [DOI] [PubMed] [Google Scholar]
- 14.Tuominen R, Joelsson P, Tenovuo O. Treatment costs and productivity losses caused by traumatic brain injuries. Brain Inj. 2012;26(13–14):1697–701. Epub 2012/11/21. 10.3109/02699052.2012.722256 . [DOI] [PubMed] [Google Scholar]
- 15.Marin JR, Weaver MD, Mannix RC. Burden of USA hospital charges for traumatic brain injury. Brain Inj. 2017;31(1):24–31. Epub 2016/11/11. 10.1080/02699052.2016.1217351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Te Ao B, Brown P, Tobias M, Ameratunga S, Barker-Collo S, Theadom A, et al. Cost of traumatic brain injury in New Zealand: evidence from a population-based study. Neurology. 2014;83(18):1645–52. Epub 2014/09/28. 10.1212/WNL.0000000000000933 . [DOI] [PubMed] [Google Scholar]
- 17.Carroll LJ, Cassidy JD, Cancelliere C, Cote P, Hincapie CA, Kristman VL, et al. Systematic review of the prognosis after mild traumatic brain injury in adults: cognitive, psychiatric, and mortality outcomes: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(3 Suppl):S152–73. Epub 2014/03/04. 10.1016/j.apmr.2013.08.300 . [DOI] [PubMed] [Google Scholar]
- 18.Stein SC, Georgoff P, Meghan S, Mizra K, Sonnad SS. 150 years of treating severe traumatic brain injury: a systematic review of progress in mortality. Journal of neurotrauma. 2010;27(7):1343–53. Epub 2010/04/16. 10.1089/neu.2009.1206 . [DOI] [PubMed] [Google Scholar]
- 19.Beck B, Gantner D, Cameron PA, Braaf S, Saxena M, Cooper DJ, et al. Temporal trends in functional outcomes after severe traumatic brain injury: 2006–2015. Journal of neurotrauma. 2018;35(8):1021–9. Epub 2017/12/20. 10.1089/neu.2017.5287 . [DOI] [PubMed] [Google Scholar]
- 20.Honeybul S, Janzen C, Kruger K, Ho KM. Decompressive craniectomy for severe traumatic brain injury: is life worth living? Journal of neurosurgery. 2013;119(6):1566–75. Epub 2013/10/15. 10.3171/2013.8.JNS13857 . [DOI] [PubMed] [Google Scholar]
- 21.Fountain DM, Kolias AG, Lecky FE, Bouamra O, Lawrence T, Adams H, et al. Survival trends after surgery for acute subdural hematoma in adults over a 20-year period. Annals of surgery. 2017;265(3):590–6. Epub 2016/05/14. 10.1097/SLA.0000000000001682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chieregato A, Venditto A, Russo E, Martino C, Bini G. Aggressive medical management of acute traumatic subdural hematomas before emergency craniotomy in patients presenting with bilateral unreactive pupils. A cohort study. Acta neurochirurgica. 2017;159(8):1553–9. Epub 2017/04/25. 10.1007/s00701-017-3190-4 WOS:000405530900028. [DOI] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–9. Epub 2009/07/23. . [DOI] [PubMed] [Google Scholar]
- 24.Brazinova A, Rehorcikova V, Taylor MS, Buckova V, Majdan M, Psota M, et al. Epidemiology of traumatic brain injury in Europe: a living systematic review. Journal of neurotrauma. 2016; Epub 2015/11/06. 10.1089/neu.2015.4126 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet (London, England). 1974;2(7872):81–4. Epub 1974/07/13. 10.1016/S0140-6736(74)91639-0. . [DOI] [PubMed] [Google Scholar]
- 26.Gennarelli TA, Wodzin E. AIS 2005: A contemporary injury scale. Injury. 2006;37(12):1083–91. Epub 2006/11/10. 10.1016/j.injury.2006.07.009 WOS:000243319200001. [DOI] [PubMed] [Google Scholar]
- 27.Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. BMJ. 2013;346:f1049 10.1136/bmj.f1049 [DOI] [PubMed] [Google Scholar]
- 28.Drummond M, Sculpher M, Torrance G, O'Brien B, Stoddart G, Buskens E. Methods for the economic evaluation of health care programmes. 3rd edition Oxford: Oxford University Press; 2005. [Google Scholar]
- 29.Costa N, Derumeaux H, Rapp T, Garnault V, Ferlicoq L, Gillette S, et al. Methodological considerations in cost of illness studies on Alzheimer disease. Health Econ Rev. 2012;2(1):18 Epub 2012/09/12. 10.1186/2191-1991-2-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molinier L, Bauvin E, Combescure C, Castelli C, Rebillard X, Soulie M, et al. Methodological considerations in cost of prostate cancer studies: a systematic review. Value in health: the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2008;11(5):878–985. Epub 2008/05/23. 10.1111/j.1524-4733.2008.00327.x . [DOI] [PubMed] [Google Scholar]
- 31.Bank TW. Available from: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?end=2015&start=1960.
- 32.Campbell and cochrane economics methods group and the evidence for policy and practice information and coordinating centre. CCEMG–EPPI-centre cost converter (v.1.5) [cited 04 June 2018]. Available from: http://eppi.ioe.ac.uk/costconversion
- 33.Shemilt I, Thomas J, Morciano M. A web-based tool for adjusting costs to a specific target currency and price year. Evidence and Policy. 2010;6(1):51–9. 10.1332/174426410x482999 WOS:000289188900004. [DOI] [Google Scholar]
- 34.Jaffe KM, Massagli TL, Martin KM, Rivara JB, Fay GC, Polissar NL. Pediatric traumatic brain injury: acute and rehabilitation costs. Arch Phys Med Rehabil. 1993;74(7):681–6. Epub 1993/07/01. 0003-9993(93)90024-5 [pii]. . [DOI] [PubMed] [Google Scholar]
- 35.Li Y, Zhou J, Chen F, Zhang J, Qiu J, Gu J. Epidemiology of traumatic brain injury older inpatients in Chinese military hospitals, 2001–2007. J Clin Neurosci. 2017;44:107–13. Epub 2017/06/12. 10.1016/j.jocn.2017.05.026 . [DOI] [PubMed] [Google Scholar]
- 36.Graves JM, Kannan N, Mink RB, Wainwright MS, Groner JI, Bell MJ, et al. Guideline adherence and hospital costs in pediatric severe traumatic brain injury. Pediatr Crit Care Med. 2016;17(5):438–43. 10.1097/PCC.0000000000000698 WOS:000379595900015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.White JR, Farukhi Z, Bull C, Christensen J, Gordon T, Paidas C, et al. Predictors of outcome in severely head-injured children. Crit Care Med. 2001;29(3):534–40. Epub 2001/05/25. . [DOI] [PubMed] [Google Scholar]
- 38.Zapata-Vazquez RE, Alvarez-Cervera FJ, Alonzo-Vazquez FM, Garcia-Lira JR, Granados-Garcia V, Perez-Herrera NE, et al. Cost Effectiveness of Intracranial Pressure Monitoring in Pediatric Patients with Severe Traumatic Brain Injury: A Simulation Modeling Approach. Value Health Reg Issues. 2017;14:96–102. Epub 2017/12/20. 10.1016/j.vhri.2017.08.011 . [DOI] [PubMed] [Google Scholar]
- 39.Albrecht JS, Slejko JF, Stein DM, Smith GS. Treatment charges for traumatic brain injury among older adults at a trauma center. J Head Trauma Rehabil. 2017;32(6):E45–E53. Epub 2017/02/15. 10.1097/HTR.0000000000000297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmed N, Kuo YH. Early versus late tracheostomy in patients with severe traumatic head injury. Surg Infect (Larchmt). 2007;8(3):343–7. Epub 2007/07/20. 10.1089/sur.2006.065 . [DOI] [PubMed] [Google Scholar]
- 41.Brooks CA, Lindstrom J, Mccray J, Whiteneck GG. Cost of medical-care for a population-based sample of persons surviving traumatic brain injury. J Head Trauma Rehabil. 1995;10(4):1–13. 10.1097/00001199-199508000-00002 WOS:A1995RN01000002. [DOI] [Google Scholar]
- 42.Bryant E, Sundance P, Hobbs A, Jenkins J, Rozance J. Managing costs and outcome of patients with traumatic brain injury in an HMO setting. J Head Trauma Rehabil. 1993;8(4):15–29. [Google Scholar]
- 43.Fakhry SM, Trask AL, Waller MA, Watts DD, Force INT. Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. The Journal of trauma. 2004;56(3):492–9. 10.1097/01.Ta.0000115650.07193.66 WOS:000220547200007. [DOI] [PubMed] [Google Scholar]
- 44.Farhad K, Khan HMR, Ji AB, Yacoub HA, Qureshi AI, Souayah N. Trends in outcomes and hospitalization costs for traumatic brain injury in adult patients in the United States. Journal of neurotrauma. 2013;30(2):84–90. 10.1089/neu.2011.2283 WOS:000313444000003. [DOI] [PubMed] [Google Scholar]
- 45.Martini RP, Deem S, Yanez ND, Chesnut RM, Weiss NS, Daniel S, et al. Management guided by brain tissue oxygen monitoring and outcome following severe traumatic brain injury. Journal of neurosurgery. 2009;111(4):644–9. Epub 2009/04/28. 10.3171/2009.2.JNS08998 . [DOI] [PubMed] [Google Scholar]
- 46.McGarry LJ, Thompson D, Millham FH, Cowell L, Snyder PJ, Lenderking WR, et al. Outcomes and costs of acute treatment of traumatic brain injury. The Journal of trauma. 2002;53(6):1152–9. Epub 2002/12/13. 10.1097/01.TA.0000025801.33552.71 . [DOI] [PubMed] [Google Scholar]
- 47.Morris S, Ridley S, Lecky FE, Munro V, Christensen MC. Determinants of hospital costs associated with traumatic brain injury in England and Wales. Anaesthesia. 2008;63(5):499–508. Epub 2008/04/17. 10.1111/j.1365-2044.2007.05432.x . [DOI] [PubMed] [Google Scholar]
- 48.Prang KH, Ruseckaite R, Collie A. Healthcare and disability service utilization in the 5-year period following transport-related traumatic brain injury. Brain Inj. 2012;26(13–14):1611–20. 10.3109/02699052.2012.698790 WOS:000311419700007. [DOI] [PubMed] [Google Scholar]
- 49.Schootman M, Buchman TG, Lewis LM. National estimates of hospitalization charges for the acute care of traumatic brain injuries. Brain Inj. 2003;17(11):983–90. Epub 2003/09/30. KGAFLM7A2N99GT59 [pii]. . [DOI] [PubMed] [Google Scholar]
- 50.You X, Liew BS, Rosman AK, Dcsn, Musa KI, Idris Z. The estimated cost of surgically managed isolated traumatic head injury secondary to road traffic accidents. Neurosurgical focus. 2018;44(5):E7 Epub 2018/05/02. 10.3171/2018.1.FOCUS17796 . [DOI] [PubMed] [Google Scholar]
- 51.Ibrahim MI, Abdullah M, Naing L, Abdullah JM, Idris Z, Aljunid SM. Cost effectiveness analysis of using multiple neuromodalities in treating severe traumatic brain injury in a developing country like Malaysia. Asian J Surg. 2007;30(4):261–6. 10.1016/S1015-9584(08)60036-6 WOS:000250689600006. [DOI] [PubMed] [Google Scholar]
- 52.Salim A, Martin M, Brown C, Inaba K, Browder T, Rhee P, et al. The presence of the adult respiratory distress syndrome does not worsen mortality or discharge disability in blunt trauma patients with severe traumatic brain injury. Injury. 2008;39(1):30–5. 10.1016/j.injury.2007.06.015 WOS:000253274700004. [DOI] [PubMed] [Google Scholar]
- 53.Yuan Q, Liu H, Wu X, Sun YR, Yao HJ, Zhou LF, et al. Characteristics of acute treatment costs of traumatic brain injury in Eastern China-a multi-centre prospective observational study. Injury. 2012;43(12):2094–9. 10.1016/j.injury.2012.03.028 WOS:000310458600022. [DOI] [PubMed] [Google Scholar]
- 54.Lehmkuhl DL, Hall K, Mann N, Gordon W. Factors that influence costs and length of stay of persons with traumatic brain injury in acute care and inpatient rehabilitation. J Head Trauma Rehabil. 1993;8(2):88–100. [Google Scholar]
- 55.Palmer S, Bader M, Qureshi A, Palmer J, Shaver T, Borzatta M, et al. The impact on outcomes in a community hospital setting of using the AANS traumatic brain injury guidelines. Americans Associations for Neurologic Surgeons. The Journal of trauma. 2001;50(4):657–64. [DOI] [PubMed] [Google Scholar]
- 56.Siddiqui UT, Tahir MZ, Shamim MS, Enam SA. Clinical outcome and cost effectiveness of early tracheostomy in isolated severe head injury patients. Surg Neurol Int. 2015;6:65 Epub 2015/05/20. 10.4103/2152-7806.155757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Andelic N, Ye J, Tornas S, Roe C, Lu J, Bautz-Holter E, et al. Cost-effectiveness analysis of an early-initiated, continuous chain of rehabilitation after severe traumatic brain injury. Journal of neurotrauma. 2014;31(14):1313–20. Epub 2014/04/12. 10.1089/neu.2013.3292 . [DOI] [PubMed] [Google Scholar]
- 58.Whitmore R, Thawani J, Grady M, Levine J, Sanborn M, Stein S. Is aggressive treatment of traumatic brain injury cost-effective? Journal of neurosurgery. 2012;116(5):1106–13. 10.3171/2012.1.JNS11962 [DOI] [PubMed] [Google Scholar]
- 59.Humphreys I, Wood RL, Phillips CJ, Macey S. The costs of traumatic brain injury: a literature review. ClinicoEconomics and outcomes research: CEOR. 2013;5:281–7. Epub 2013/07/10. 10.2147/CEOR.S44625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dismuke CE, Walker RJ, Egede LE. Utilization and cost of health services in individuals with traumatic brain injury. Glob J Health Sci. 2015;7(6):156–69. Epub 2015/07/15. 10.5539/gjhs.v7n6p156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Finkler SA. The distinction between cost and charges. Annals of internal medicine. 1982;96(1):102–9. Epub 1982/01/01. . [DOI] [PubMed] [Google Scholar]
- 62.Institute HCC. 2016 health care cost and uilization report 2017. Available from: http://www.healthcostinstitute.org/report/2016-health-care-cost-utilization-report/ (accessed 04 June 2018).
- 63.Polinder S, Meerding WJ, van Baar ME, Toet H, Mulder S, van Beeck EF, et al. Cost estimation of injury-related hospital admissions in 10 European countries. The Journal of trauma. 2005;59(6):1283–90; discussion 90–1. Epub 2006/01/06. . [DOI] [PubMed] [Google Scholar]
- 64.Dieleman J, Campbell M, Chapin A, Eldrenkamp E, Fan VY, Haakenstad A, et al. Evolution and patterns of global health financing 1995–2014: development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. Lancet (London, England). 2017;389(10083):1981–2004. 10.1016/S0140-6736(17)30874-7 WOS:000401515300023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Georgoff P, Meghan S, Mirza K, Stein SC. Geographic variation in outcomes from severe traumatic brain injury. World Neurosurg. 2010;74(2–3):331–45. 10.1016/j.wneu.2010.03.025 WOS:000292781100037. [DOI] [PubMed] [Google Scholar]
- 66.Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. The Lancet Neurology. 2008;7(8):728–41. Epub 2008/07/19. 10.1016/S1474-4422(08)70164-9 . [DOI] [PubMed] [Google Scholar]
- 67.Ponsford JL, Spitz G, Cromarty F, Gifford D, Attwood D. Costs of care after traumatic brain injury. Journal of neurotrauma. 2013;30(17):1498–505. Epub 2013/04/11. 10.1089/neu.2012.2843 . [DOI] [PubMed] [Google Scholar]
- 68.Moore L, Stelfox HT, Evans D, Hameed SM, Yanchar NL, Simons R, et al. Hospital and intensive care unit length of stay for injury admissions: a pan-Canadian cohort study. Annals of surgery. 2018;267(1):177–82. Epub 2016/10/21. 10.1097/SLA.0000000000002036 . [DOI] [PubMed] [Google Scholar]
- 69.Tardif PA, Moore L, Boutin A, Dufresne P, Omar M, Bourgeois G, et al. Hospital length of stay following admission for traumatic brain injury in a Canadian integrated trauma system: A retrospective multicenter cohort study. Injury. 2017;48(1):94–100. Epub 2016/11/15. 10.1016/j.injury.2016.10.042 . [DOI] [PubMed] [Google Scholar]
- 70.Su SH, Wang F, Hai J, Liu NT, Yu F, Wu YF, et al. The effects of intracranial pressure monitoring in patients with traumatic brain injury. PLoS One. 2014;9(2):e87432 Epub 2014/03/04. 10.1371/journal.pone.0087432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80(1):6–15. Epub 2016/09/23. 10.1227/NEU.0000000000001432 . [DOI] [PubMed] [Google Scholar]
- 72.Chen A, Bushmeneva K, Zagorski B, Colantonio A, Parsons D, Wodchis WP. Direct cost associated with acquired brain injury in Ontario. BMC Neurol. 2012;12:76 Epub 2012/08/21. 10.1186/1471-2377-12-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Spitz G, McKenzie D, Attwood D, Ponsford JL. Cost prediction following traumatic brain injury: model development and validation. J Neurol Neurosurg Psychiatry. 2016;87(2):173–80. jnnp-2014-309479 [pii]; 10.1136/jnnp-2014-309479 [DOI] [PubMed] [Google Scholar]
- 74.Leitgeb J, Mauritz W, Brazinova A, Majdan M, Wilbacher I. Impact of concomitant injuries on outcomes after traumatic brain injury. Arch Orthop Trauma Surg. 2013;133(5):659–68. Epub 2013/03/07. 10.1007/s00402-013-1710-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Davis KL, Joshi AV, Tortella BJ, Candrilli SD. The direct economic burden of blunt and penetrating trauma in a managed care population. The Journal of trauma. 2007;62(3):622–9. 10.1097/TA.0b013e318031afe3 WOS:000244877300015. [DOI] [PubMed] [Google Scholar]
- 76.Majdan M, Plancikova D, Maas A, Polinder S, Feigin V, Theadom A, et al. Years of life lost due to traumatic brain injury in Europe: A cross-sectional analysis of 16 countries. PLoS medicine. 2017;14(7):e1002331 Epub 2017/07/13. 10.1371/journal.pmed.1002331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stocchetti N, Zanier ER. Chronic impact of traumatic brain injury on outcome and quality of life: a narrative review. Critical care (London, England). 2016;20(1):148 Epub 2016/06/22. 10.1186/s13054-016-1318-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McMillan TM, Teasdale GM, Stewart E. Disability in young people and adults after head injury: 12–14 year follow-up of a prospective cohort. Journal of neurology, neurosurgery, and psychiatry. 2012;83(11):1086–91. Epub 2012/05/31. 10.1136/jnnp-2012-302746 . [DOI] [PubMed] [Google Scholar]
- 79.Cnossen MC, Huijben JA, van der Jagt M, Volovici V, van Essen T, Polinder S, et al. Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: a survey in 66 neurotrauma centers participating in the CENTER-TBI study. Critical care (London, England). 2017;21(1):233 Epub 2017/09/07. 10.1186/s13054-017-1816-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cnossen MC, Polinder S, Andriessen TM, van der Naalt J, Haitsma I, Horn J, et al. Causes and consequences of treatment variation in moderate and severe traumatic brain injury: a multicenter study. Crit Care Med. 2017;45(4):660–9. Epub 2017/02/09. 10.1097/CCM.0000000000002263 . [DOI] [PubMed] [Google Scholar]
- 81.van Essen TA, de Ruiter GC, Kho KH, Peul WC. Neurosurgical Treatment Variation of Traumatic Brain Injury: Evaluation of Acute Subdural Hematoma Management in Belgium and The Netherlands. Journal of neurotrauma. 2017;34(4):881–9. Epub 2016/07/10. 10.1089/neu.2016.4495 . [DOI] [PubMed] [Google Scholar]
- 82.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Variation in adult traumatic brain injury outcomes in the United States. J Head Trauma Rehabil. 2018;33(1):E1–E8. Epub 2017/04/20. 10.1097/HTR.0000000000000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Reith FC, Van den Brande R, Synnot A, Gruen R, Maas AI. The reliability of the Glasgow Coma Scale: a systematic review. Intensive care medicine. 2016;42(1):3–15. Epub 2015/11/14. 10.1007/s00134-015-4124-3 . [DOI] [PubMed] [Google Scholar]
- 84.Becker A, Peleg K, Olsha O, Givon A, Kessel B, Israeli Trauma G. Analysis of incidence of traumatic brain injury in blunt trauma patients with Glasgow Coma Scale of 12 or less. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2018;21(3):152–5. Epub 2018/05/20. 10.1016/j.cjtee.2018.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Carroll CP, Cochran JA, Price JP, Guse CE, Wang MC. The AIS-2005 revision in severe traumatic brain injury: mission accomplished or problems for future research? Ann Adv Automot Med. 2010;54:233–8. Epub 2010/11/06. [PMC free article] [PubMed] [Google Scholar]
- 86.Savitsky B, Givon A, Rozenfeld M, Radomislensky I, Peleg K. Traumatic brain injury: It is all about definition. Brain Inj. 2016;30(10):1194–200. Epub 2016/07/29. 10.1080/02699052.2016.1187290 . [DOI] [PubMed] [Google Scholar]
- 87.Maas AI, Harrison-Felix CL, Menon D, Adelson PD, Balkin T, Bullock R, et al. Common data elements for traumatic brain injury: recommendations from the interagency working group on demographics and clinical assessment. Arch Phys Med Rehabil. 2010;91(11):1641–9. Epub 2010/11/04. 10.1016/j.apmr.2010.07.232 . [DOI] [PubMed] [Google Scholar]
- 88.Hakkaart-van Roijen L, van der Linden N, Bouwmans C, Kanters T, Tan S. Kostenhandleiding: methodologie van kostenonderzoek en referentieprijzen voor economische evaluaties in de gezondheidszorg. Zorginstituut Nederland; 2015;(https://www.zorginstituutnederland.nl/binaries/zinl/documenten/publicatie/2016/02/29/richtlijn-voor-het-uitvoeren-van-economische-evaluaties-in-de-gezondheidszorg/Richtlijn+voor+het+uitvoeren+van+economische+evaluaties+in+de+gezondheidszorg+%28verdiepingsmodules%29.pdf (accessed 30-03-2018)):1–120 (accessed on 30-03-2018). [Google Scholar]
- 89.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev. 2011;89(9):46–52, 4, 6–61. Epub 2011/09/24. . [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
N/A: Not applicable.
(DOC)
* Item scores with double weight.
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.