Abstract
Introduction
Women have unique healthcare needs that are not well addressed by our current healthcare system and with healthcare transformation underway the opportunity exists to avoid weaving these age‐old problems into the fabric of the new healthcare design. myAva is an example of a learning health system integrated into a cloud‐based precision health platform. The goal of myAva is to integrate the tools of precision health and principals of a learning health system to improve care for women, starting with polycystic ovary syndrome (PCOS).
Methods
Putting patients at the center in designing a new style of healthcare has been an important concept underlying the development of myAva since inception. Understanding the needs of patients and providers is key to the development of myAva. Surveys were collected from members of the PCOS patient community and patient and medical advisory boards were recruited. For the pilot group comprehensive omic data, biometric and self‐reported data were collected and integrated into a personalized health dashboard enabling providers to formulate personalized treatment plans. The ongoing collection of data will create continuous improvement of healthcare.
Results
Precision health for chronic issues faced is in its infancy and although myriad challenges exist the potential to improve health outcomes is great. myAva's providers, patients, and advisors are encouraged by the early outcomes of the program with improved health outcomes and an increased sense of empowerment reported. It is clear that designing and implementing this type of care requires collaboration, the involvement of all stakeholders, with patients at the center.
Keywords: Polycystic Ovary Syndrome, Precision Health, Women's Health
1. INTRODUCTION
In an era of rapidly evolving healthcare, it is critical that we acknowledge the unique needs of women's health that are not currently well addressed by our traditional healthcare system. These issues must be addressed to prevent perpetuating a cycle of bias, misinformation, and poor health outcomes. New innovations, technology, and the rise of the patient have created a unique environment and presents an exciting opportunity to finally acknowledge, address, and implement strategies for change as it relates to women's health. Moreover, for the first time in the history of modern healthcare, systematic change is taking place with the patient at the center.
A new vision for healthcare has emerged, in which systems are implemented for the continuous improvement of healthcare. These systems are referred to as learning health systems (LHSs). LHSs aim to collect and analyze patient data in real time to form a better understanding of patient health problems and outcomes and to apply this new knowledge to influence future practice, thus improving healthcare.1 Not only do LHSs aim to reduce the 17‐year gap between research and clinical practice, but also LHSs have tremendous potential to empower patients by giving them access to their own health data.
myAva is an example of an LHS integrated into a cloud‐based, patient‐centered health platform that empowers women to advocate for their own healthcare and health outcomes through the use of precision medicine. myAva was founded by a patient (author, S.S.) who experienced firsthand many of the problems that exist in the delivery of women's health care. The platform is named after the late Ava Dale, a courageous woman who taught the author how to advocate for herself in her healthcare. Based on her own experience, Ava encouraged and emphasized the principals of self‐advocacy and patient empowerment to women who had suffered miscarriages or early infant loss long before “patient engagement” became a catchphrase. With Ava's guidance, the author learned that her role as a patient went beyond being a mere bystander in her own care. Ava's gift was one that she soon realized needed to be passed on to other women and was the inspiration that eventually led to the creation of the myAva precision health platform. The goal of myAva is to bring the tools of precision health and principals of an LHS to women's healthcare, starting with the polycystic ovary syndrome (PCOS) community. Women with PCOS have often been neglected and forgotten by the healthcare system and myAva aims to give patients and providers the necessary tools and information to promote the best standard of care.
1.1. The Complexity of PCOS
PCOS is a chronic and serious health condition with genetic underpinnings2 and involves a complex array of endocrine, metabolic, psychological, and dermatologic features. This lifelong condition affects approximately 116 million women worldwide.3 PCOS is the leading cause of infertility and is the most common endocrine disorder in women of reproductive age. Women with PCOS suffer from a vast number of chronic health symptoms that have a significant impact on quality of life.4, 5 Women with PCOS have a significantly increased risk for cardiovascular disease, endometrial cancer, obstructive sleep apnea, and diabetes. In fact, 50% of women with PCOS will develop diabetes by the time they are 40 years old.6 It is a poorly defined disorder with a complex pathophysiology and a wide variety of clinical presentations making the diagnosis of PCOS problematic. Since first described in 1935 by Stein and Leventhal,7 the syndrome has gone through a name change and a number of diagnostic criteria changes, which have generated vigorous debate among physicians, researchers, and patients alike. Despite the current name, not all women with PCOS present with polycystic ovaries. It is believed that millions of women are undiagnosed and that this out‐dated name is an exacerbating factor.8 As a result, a heated and controversial debate over a potential name change continues today.9 Most medical professionals agree that early intervention is important10; yet, 50% to 70% of women are undiagnosed or misdiagnosed,11 making PCOS one of the most medically underserved patient communities. The economic burden to the United States alone is estimated to be in excess of $4.36 billion dollars annually.12 Currently, most healthcare providers focus on symptom management for issues such as infertility and diabetes. Treatment for PCOS is complex and without a comprehensive, multi‐faceted, and personalized approach, women are often left on their own to deal with hirsutism, acne, hair loss, menstrual irregularities, and obesity. Even with treatment, women with PCOS suffer from a lower quality of life.13, 14
A combination of gender, weight, and age bias has further confounded the inherent problems in diagnosing and treating women and girls with PCOS. Women have never, in the history of modern healthcare, had a role in the design, research, delivery, and reporting of healthcare that is equal to men. Weight bias is of particular concern to our patient population, as obesity has long been considered a hallmark of PCOS. Although there is some controversy, some US studies report obesity rates in women with PCOS of up to 80%.15 Weight discrimination in the US has increased by almost 66%16 in the past decade, with a greater frequency among women.17 This obesity stigma has important ramifications as it has been shown that overweight women may delay care and screening18, 19, 20 and receive lower quality of care than non‐obese patients.21 On the other side of the spectrum, because of the close association between PCOS and obesity, lean women face the opposite bias and some report having been denied screening for PCOS because they are not overweight. Ageism in healthcare is a growing topic of discussion and women with PCOS are at risk of experiencing age bias at both ends of the spectrum. PCOS symptoms are often present even before the onset of puberty,22 and quality of life is lower for these young girls with PCOS than their same‐age peers.23, 24 Because of the extreme focus on fertility in this patient population, a common complaint within the PCOS community is feeling brushed aside by healthcare providers if they are not trying to conceive or are postmenopausal. Yet from a patient's perspective, a variety of non‐reproductive symptoms, such as obesity and hirsutism, are considered very distressing and negatively impact their quality of life,14, 25 and metabolic risks become critical for the more mature postmenopausal PCOS population.26, 27
An LHS framework provides a roadmap for addressing many of the complex problems associated with PCOS. One major goal of myAva is to provide actionable knowledge that is based on real‐world data from a large sample size of women with PCOS. This article describes our experience developing the myAva Precision Health Platform and the experiences of the pilot group in the program.
2. METHODOLOGY
myAva was developed to address the wide range of serious and ongoing issues in women's health. The general approach for the development of myAva included the following: (1) surveying the PCOS community to determine their experience and needs, (2) recruiting patient and medical advisory boards, and (3) developing the myAva Precision Health Platform with patient needs in mind (Figure 1).
Figure 1.

The myAva Precision Health Program was developed using a patient‐centric model
2.1. Survey of Members of the PCOS Community
Historically, decisions about patients have been made without the involvement of patients.28 Our first step in development of the myAva platform was to survey the PCOS community. We partnered with the leading PCOS patient support organization, PCOS Challenge, to launch an email campaign in the Atlanta, Georgia, area. The email campaign targeted 1000 members of the PCOS community who were invited to participate through a link provided in the email. Seventy‐nine responses were received and surveys were sent out to 66 women with PCOS to collect information from a patient perspective on the current state of PCOS care and to determine eligibility for myAva's patient advisory board. Because of the complexities and multiple phenotypes associated with PCOS, understanding the problems patients face requires a deep understanding that only a patient can provide. Our survey included questions aimed at understanding these challenges and 55 survey responses were received.
Based on these surveys, we obtained valuable information about the healthcare experiences of women with PCOS. The results indicated that women with PCOS want more and better information, access to more treatment options, doctors who listen and who have expertise in PCOS or are willing to learn, access to comprehensive laboratory testing, to be allowed to participate in their care, less fragmentation, more research, and ongoing support.
PCOS management requires a multifaceted approach that includes lifestyle interventions29; however, according to our survey, women who received a diagnosis were either given no information or were simply given a brochure explaining their condition. In fact, women with PCOS often learn about the syndrome themselves after many years of searching for answers and then present this information to her physician. For example, 1 patient recognized her lifelong medical problems while in her 40s while reading a woman's magazine. Another patient was watching an episode of a popular weight loss–related television program and recognized her symptoms immediately. Both women presented their findings to their physician, which eventually led to their diagnosis. All of our respondents revealed they felt a need to self‐educate and self‐advocate, and many women indicated that the information they found most useful came from patient advocacy websites30 rather than a healthcare provider.
2.2. Creation of Patient Advisory Board
The email campaign also invited women to participate on a patient advisory board, who would be the pilot group for the myAva Precision Health Program. Participation on the advisory board was open to adult women who had previously received a diagnosis of PCOS, resided in the Greater Atlanta Area, and were willing to participate for a minimum of 1 year. Women who were pregnant at the time, had a cardiac or respiratory illness which precluded them from participating in physical activity, were undergoing gene therapy, cell therapy, chemotherapy, or radiotherapy treatment or were awaiting major surgery were excluded from participating. Based on interest and eligibility, 42 women were invited to attend 1 of 2 informational and group interview sessions. At those meetings, the myAva team shared their vision for a new style of healthcare for women with PCOS and provided an overview of myAva's Precision Health Platform. At these meetings, the women were invited to share their patient narratives, views on diagnosis, and care and explain why they wanted to participate as an advisor in an open discussion format. Ten patient advisors were selected to become the first participants in myAva's Precision Health Program, along with the CEO of myAva (author S.S.).
2.3. Recruitment of a Medical Advisory Board
Another key step in the development of the myAva precision health platform was the recruitment of a medical advisory board. An active, enthusiastic, and distinguished medical advisory board was recruited from the author's global network of healthcare providers. Members of the medical advisory board include both medical and naturopathic doctors with various specialties, such as integrative medicine, obstetrics and gynecology, microbiomics, and extensive expertise in PCOS. These advisors provide commentary, direction, and insight to the myAva scientific team and enhance the expertise of our healthcare providers. The medical advisory board has provided critical guidance to the myAva team in supporting physicians as they adopt these changes into their practice. All the members of the medical advisory board are excited by the innovation happening in healthcare and are motivated to shape the future of healthcare for women.
2.4. myAva Precision Health Program
To achieve our objectives to deliver timely care to women, as well as to build a comprehensive molecular model of each patient through a diverse set of diagnostic testing, we followed a multistep process. Two group appointments were held where blood, urine, fecal, and vaginal samples were collected from the participants. With no single laboratory able to conduct all of the analysis, we distributed samples to labs across North America. Each data set was analyzed; however, the overall challenge with aggregating this much data is that it exists in different formats and needs to be transformed into a consistent machine‐readable format. Because different data sets were ready for delivery within different time intervals, we broke the analysis down into immediate, mid‐term, and long‐term components. With myAva still under development, we had the opportunity to figure this out in real time. A mini‐diagnostic panel was designed to enable the immediate delivery of care to the participants. As the data became available, the care team along with the scientific support team delivered the results to the patient. During the consultation with the physician, results were reviewed and an action plan implemented, which included both preventative measures, such as lifestyle modifications, as well as any necessary medical interventions.
Over time, the myAva precision health platform will create a molecular map of the patient by assembling genomic, transcriptomic, proteomic, metabolomic, microbiomic, as well as biometric and self‐reported data to provide insights into the patient's current state of health. Baseline data will be collected and then analyzed when a patient joins myAva's Precision Health Program. Every 90 days, a new measurement cycle will capture the effectiveness of the recommendations and treatments and trends over time are reported.
2.5. myAva Precision Health Platform
The objective of the myAva Precision Health Platform is to improve the experience of diagnosis, treatment, and prevention for women by providing women and providers access to the information they need, when they need it, and in the format they prefer. In addition, providers are given the tools and intelligence to create an treatment plan for their patients by bringing their own insight, experience, and expertise together with the data.
A personalized health dashboard that can be accessed by both the patient and provider helps achieve this aim. The individualized data available through the myAva dashboard are carefully organized and can be viewed by patients and providers in a variety of relevant ways, including (1) by health category such as reproductive health, vascular health, metabolic health, etc; (2) by health condition such as diabetes, kidney disease, endometrial cancer, etc; (3) by molecular category such as proteomics, metabolomics, genomics, microbiomics, etc; and (4) by molecular measure such as individual analytes such as estriol, luteinizing hormone, etc. In addition, a pharmacogenomic report is created for each patient promoting the safe use and dosage of medications.
Search capabilities allow providers and patients to quickly and easily access biomarkers and their values. Each measure is indicated numerically as well as on a spectrum of ranges from low, to normal, to high (Figure 2). The values are color coded using the universally accepted red, amber, and green. Every measure includes a description along with the associated conditions, as well as clickable links that provide instant access to relevant evidence‐based research, and each biomarker can be easily bookmarked for future referencing. Providers can create action plans and notes from anywhere within the dashboard, including directly from the biomarker value, which can then be easily monitored over time. For example, a physician viewing a patient's elevated glucose levels can create an action plan or attach a note relevant to a specific biomarker to be followed up on at a later date.
Figure 2.
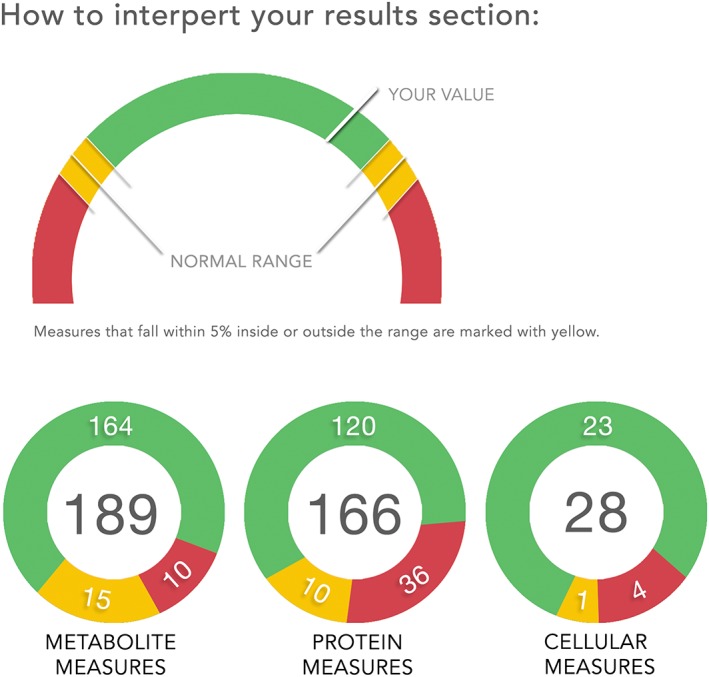
Example of curated data inputs and values interpreted as either being inside or outside of the normal range
From their myAva dashboard, patients can visualize the overall state of their health in the form of a summary report as well as access targeted treatment plans, notes from their provider(s) and a learning “library” of vetted evidence‐based health articles. Patients can also interact with a data map of the interrelations between conditions. Also collected is comprehensive phenotypic data, such as medical history, family history, current and past symptoms, health questionnaires, and other information provided by the patient. It is fully editable at any time and auto‐saved for convenience.
In addition, myAva providers and patients receive molecular‐level data that is filtered and prioritized to form a patient's risk score for a particular health issue. The raw data and research underlying these scores are readily accessible on the platform in real time. Using data visualization tools, providers and patients can track trends away from or toward disease over time. Furthermore, patients are able to contribute to their health record as well as interact with their data. With the ability to educate themselves and data in hand, patients have the ability to advocate for their health by easily recognizing trends in either a positive or negative direction.
In the future, myAva will incorporate additional advocacy tools and features by working with patients to define what the actual tools should be based on what is important to them.
2.6. Actionable Intelligence: myAva Precision Nutrition Program
A majority of the women on myAva's Patient Advisory Board report that they have encountered weight bias as well as a lack of guidelines and support regarding weight loss strategies from healthcare providers. Although weight loss has been shown to improve many symptoms of PCOS, due to the metabolic factors associated with the syndrome, losing weight can present an extreme challenge.31 Without ongoing support or guidelines to achieve success, the healthcare system has set PCOS patients up for failure. Studies have indicated that lifestyle modifications should be the first line of defense for PCOS patients,32, 33 and myAva's Precision Nutrition Program is an example of such a strategy. First, women participated in a group appointment and education session to learn about PCOS and the latest nutritional recommendations. Patients then received a one‐on‐one nutrition consultation. Rather than a one‐size‐fits‐all approach, the nutrition plan was personalized for each patient and was tied to her molecular profile. The Precision Nutrition Program can be altered in accordance with the biomarkers that are tracked over time. For example, because the majority of women with PCOS are insulin resistant and are at risk of developing type II diabetes, they are provided with a nutrition plan related to their personal health goals and the severity of their insulin resistance or diabetes. The women receive follow‐up consultations and ongoing nutritional support as well as the opportunity to ask questions in an online nutrition‐focused group and can access their nutrition portal 24/7.
2.7. The Future of myAva: Deep Learning
The underlying principles of diagnosis, treatment, and delivery of patient care are changing rapidly due to the advent of big data, artificial intelligence, and deep learning. The myAva platform amasses patient data from multiple sources at multiple time points, potentially accumulating up to 1 terabyte of data per patient annually. In the future, deep‐learning systems can be developed to make connections between the individualized data and the treatment outcomes and will drive efficiencies and increase accuracy and speed in diagnostics and interpreting data. Today, AI and deep learning are used as decision support tools to the provider; however, as deep learning takes over and becomes more reliable, the future may include decision support direct to the patient. (A full discussion of AI and deep learning is beyond the scope of this paper.) As data are collected continuously, the benefits of treatment interventions specific to a patient are analyzed so that action plans can be further optimized (Figure 3). With the addition of more patients and more data over time, there is an increasingly powerful opportunity for learning. Deep learning will help bridge the gap between the current standard of care and the new, more personalized, standard of care. As more molecular data, combined with the biometric, patient‐reported, and physician‐reported data, are collected, the gap between science and healthcare delivery begins to close. The confluence of big data and machine learning will tell a compelling patient story.
Figure 3.
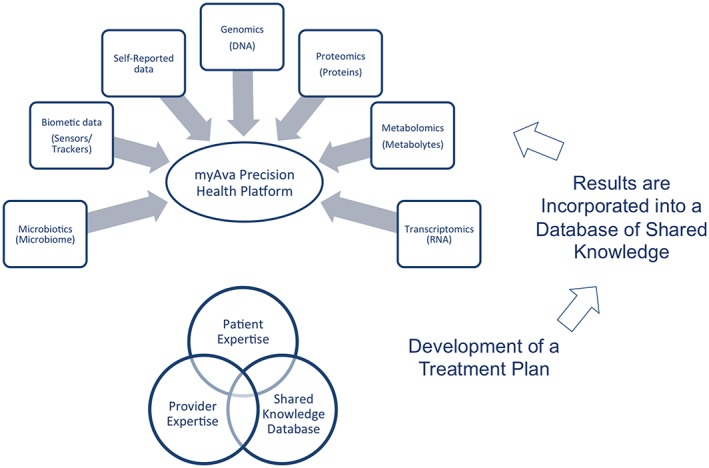
myAva: a model for precision health. As data inputs are collected and curated over time, patients and providers can work together to formulate a personalized treatment plan, taking into consideration the results of other women who have implemented similar treatment options. The results of the treatment plan are monitored and recorded over time and added to a database of shared knowledge. This process is repeated to provide continuous improvement of healthcare to the individual and the community
Over time, the myAva platform will collect data from a large number of women who can then be tracked and analyzed and thus bring clarity to the complexities related to the pathophysiology of PCOS. With research lacking and traditional methods of discovery being slow and tedious, and taking years to find their way the clinic, myAva implements a big data approach to improving healthcare. This approach has the potential to alter the future of diagnosis, care, and treatment guidelines for the PCOS patient population in near real time.
Furthermore, deep learning has the potential to uncover and remove biases and drive the integrity of the LHS. An interesting example was uncovered by John Hopkins Hospital when designing their blood clot prevention protocol; they accidentally discovered that checklists removed gender bias completely.34 Such stigma and bias reduction strategies are being pursued and built into the design of myAva, including steps, reminders, and checklists, and suggested actions to enhance a provider's ability to diagnose, treat, and care for a patient with a goal to remove hidden biases that could potentially affect decision making.
3. RESULTS
Precision health is in its infancy and there is still so much to learn. The challenges are immense, and the collective healthcare community is still discovering how to deliver precision health. Our early experience indicates that clinics and labs are lacking the infrastructure and workflows for precision health methods; furthermore, patients and providers do not have models and expectations for the process of implementing a precision health program. Moreover, in the end, who will pay for this type of care? The process of transitioning from an old model to a new model of healthcare will require collaboration, trial and error, and innovation. myAva is still in the early phases of development, and there is still much room for growth, improvement, and learning. However, the myAva platform has created a movement of people from different disciplines across the globe that are all committed to and motivated by the fact that the PCOS patient community represents a cohort of women that have been underserved for too long.
Despite these challenges, both the myAva medical advisory board and the patient advisory board have given overwhelmingly unanimous support for the ongoing delivery of this type of innovation in women's health. Our physicians, advisors, collaborators, and partners have experienced the ups and downs of developing a new style of healthcare for women and have worked diligently with us from the early stages. The overall sentiment is that there is strong value in having such comprehensive data to aid clinicians in the delivery of patient care.
3.1. Patient Empowerment and Engagement
One major goal of myAva is to empower women to be their own advocate. In order for a patient to advocate for herself, it is critical that she have access to her own healthcare data.
Every woman who has participated in the advisory board thus far has reported a greater sense of empowerment, a deeper understanding of her body, her health, and the implications of the decisions she makes in her health. One woman described it this way, “The best part about myAva has been learning about my body and PCOS on a deeper level. I feel more equipped than ever to fight this disease.” All of the women reported an improvement in overall well being. Some also noted that their willingness to understand and share their data has opened the lines of communication with their other providers.
For example, some of the patients reported feeling validated when a review of their genomic report revealed a genetic disposition toward obesity. Furthermore, participants reported that providers seemed to be more understanding of their obesity upon attribution of a genetic predisposition. The initial reaction from patients regarding collecting such vast amounts of phenotypic data to correlate these data against the molecular data over time has been overwhelmingly positive. The patients have expressed their hopefulness that by sharing this deep level of information the subsequent analysis will provide a wealth of knowledge unlike anything they or their healthcare providers have seen before. They also share their enthusiasm over the potential that this could lead to new discoveries that will benefit not only them, but also the entire PCOS “cysterhood.”
3.2. Patient Engagement and Improved Health Outcomes
The world of healthcare is increasingly data driven,35 and patients have begun to demand access to their health data. Although substantial measures have been taken to increase patient access to data,36 the best healthcare does not end at merely giving patients their data. The mere act of “giving” is paternalistic. “To give” means to bestow, to accord, to allow, to grant, to offer, to present.37 Giving data is not enough and is not empowerment. Data is the starting point and needs to be turned into actionable intelligence in the form of a treatment plan.
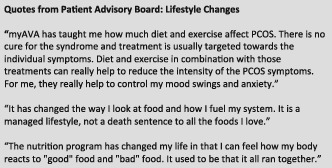
Women on the patient advisory board expressed an increased level of responsibility for their own health outcomes, especially in implementing myAva's Precision Nutrition Plan. Women with PCOS have typically tried multiple diet trends usually with limited success. Having a plan personalized to them and tied to their molecular profile empowers women by giving them a roadmap for success beyond just weight loss.
3.3. Increased Provider Empowerment
Through the myAva platform, providers are given the tools and intelligence to create an action plan for their patients by bringing their own insight, experience and expertise together with the data. This is an opportunity for an LHS, like myAva, to empower providers with the knowledge they need to deliver optimal care for patients in real time. In fact, when asked what they felt was the biggest challenge faced by PCOS patients, 57% of respondents surveyed commented that it is the lack of physician knowledge and understanding. One respondent described her healthcare experience as a “battlefield” she had endured for 10 years. Improving provider confidence in delivering care is an important concept for myAva. For example, in a study that looked at obesity, only 56% of physicians felt qualified to treat obesity.38 With a significant number of PCOS patients struggling with obesity, myAva will provide the information, knowledge and tools with an aim to increase physician confidence in treating obese patients.
There is no doubt, however, having this much data, some of it unfamiliar, has raised additional questions that requires deeper exploration by providers. Providers require support to begin delivering precision health and 2 of the major limitations to delivering this type of care are the increased consultation time required and the current incentive model is not well suited to precision health. Initial consultations delivered to myAva's patient advisory board members took up to an hour; however, our providers believe that as they become more accustomed to this new model, their proficiency will increase and the clinic will develop a new cadence, potentially involving other members of the clinical team. In addition, as the LHS begins to take over more of the patient education and creates efficiencies, we anticipate further reductions in provider time spent. In the meantime, myAva is working closely with providers to understand the barriers they face and supports physicians every step of the way as they adopt the changes into their practice.
3.4. Community Support
Women with PCOS often feel isolated because of the lack of understanding of their health condition, even among family and friends, and often do not know other women who face the same day‐to‐day challenges. Recognizing the benefit of a PCOS “Cysterhood,” myAva ensures that women have the opportunity to connect with an online PCOS patient community. For many of the women who attended our information meetings, it was the first time they had ever met another woman (affectionately nicknamed “cyster”) who was facing the same challenges that their PCOS served up to them on a daily basis.
As the women incorporate lifestyle modifications, the support from other women with PCOS through an online social group has been one of the most popular benefits experienced by myAva's patient Advisory Board. Connecting with other women in a safe and social way has been an unequivocal success and it is the women themselves that offer other patients the ongoing support they need, taking a large load off the clinical support team. Women describe the support of other PCOS patients with comments like, “Linking arms with other ladies with PCOS has been a powerful experience” and “It's a relief to know and interact with other women who have PCOS.”
3.5. Payment Options and Challenges
Because wellness is not currently underwritten in the traditional sense, preventative medicine, including the myAva Precision Health Program, is currently a direct pay model. With advancements in technology, the cost of diagnostics is expected to decrease, ultimately reducing costs. With wellness programs and health spending accounts emerging at the corporate level, employees are able to choose specific health and wellness products and services based on their own personal needs. Along with a growing trend in prevention, the future outlook is for the emergence of wellness insurance to cover preventative treatments using precision health data. Until then patients who want access to integrative or precision health programs will continue to pay a subscription fee for this type of healthcare.
4. CONCLUSION
An unprecedented transformation is underway as healthcare is being redesigned across the globe. A successful outcome requires a fundamental change in the way we view both health and care. Although the future remains uncertain, a formidable and strategic plan that involves sharing data, the collaboration of all stakeholders, and encompasses the values of an LHS will help to ensure success. The opportunity for maximum benefit exists at the intersection of an LHS and precision health. By personalizing healthcare we begin to eliminate the challenges and underlying biases of today and by embedding transformative strategies into the continuous learning loop of an LHS, we empower its users.
Although we are still in the early days, we have already noted significant improvements and uncovered interesting insights into the health of myAva's small group of PCOS patients. The potential for discovery is tremendous as we follow these women and many more over time. We expect discoveries and learning will accelerate and with deep learning will become more reliable, with improved accuracy and leading to optimized outcomes. With effective strategies in place, we believe precision healthcare delivered as an LHS will dramatically improve care for women with PCOS and beyond.
Satveit S. Addressing the unique healthcare needs of women: opportunity for change exists at the intersection of precision health and learning health systems. Learn Health Sys. 2018;2:e10033 10.1002/lrh2.10033
REFERENCES
- 1. Friedman CP, Allee NJ, Delany BC, et al. The science of learning health systems: foundations for a new journal. Learn Health Syst. 2017;e10020. 10.1002/lrh2.10020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Legro RS, Strauss JF. Molecular progress in infertility: polycystic ovary syndrome. Fertil Steril. 2002;78(3):569‐576. [DOI] [PubMed] [Google Scholar]
- 3. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163‐2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barnard L, Ferriday D, Guenther N, Strauss B, Balen AH, Dye L. Quality of life and psychological well being in polycystic ovary syndrome. Hum Reprod. 2007;22(8):2279‐2286. [DOI] [PubMed] [Google Scholar]
- 5. Nasiri Amiri F, Ramezani Tehrani F, Simbar M, Montazeri A, Mohammadpour Thamtan RA. The experience of women affected by polycystic ovary syndrome: a qualitative study from Iran. Int J Endocrinol Metabol. 2014;12(2):e13612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lorenz LB, Wild RA. Polycystic ovarian syndrome: an evidence‐based approach to evaluation and management of diabetes and cardiovascular risks for today's clinician. Clin Obstet Gynecol. 2007;50(1):226‐243. [DOI] [PubMed] [Google Scholar]
- 7. Azziz R, Adashi EY. Stein and Leventhal: 80 years on. Am J Obstet Gynecol. 2016;214(2):247 e1‐247e11. [DOI] [PubMed] [Google Scholar]
- 8. Washburn RA, Lambourne K, Szabo AN, Herrmann SD, Honas JJ, Donnelly JE. Does increased prescribed exercise alter non‐exercise physical activity/energy expenditure in healthy adults? A systematic review. Clin Obes. 2014;4(1):1‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Galeano ME, Martinez M, Amarilla AA, et al. Molecular epidemiology of norovirus strains in Paraguayan children during 2004–2005: description of a possible new GII.4 cluster. J Clin Virol. 2013;58(2):378‐384. [DOI] [PubMed] [Google Scholar]
- 10. Deeks AA, Gibson‐Helm ME, Paul E, Teede HJ. Is having polycystic ovary syndrome a predictor of poor psychological function including anxiety and depression? Hum Reprod. 2011;26(6):1399‐1407. [DOI] [PubMed] [Google Scholar]
- 11. March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25(2):544‐551. [DOI] [PubMed] [Google Scholar]
- 12. Azziz R, Marin C, Hoq L, Badamgarav E, Song P. Health care‐related economic burden of the polycystic ovary syndrome during the reproductive life span. J Clin Endocrinol Metab. 2005;90(8):4650‐4658. [DOI] [PubMed] [Google Scholar]
- 13. Gibson‐Helm ME, Lucas IM, Boyle JA, Teede HJ. Women's experiences of polycystic ovary syndrome diagnosis. Fam Pract. 2014;31(5):545‐549. [DOI] [PubMed] [Google Scholar]
- 14. Brady C, Mousa SS, Mousa SA. Polycystic ovary syndrome and its impact on women's quality of life: more than just an endocrine disorder. Drug Healthc Patient Saf. 2009;1:9‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sam S. Obesity and polycystic ovary syndrome. Obes Manag. 2007;3(2):69‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17(5):941‐964. [DOI] [PubMed] [Google Scholar]
- 17. Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes (Lond). 2008;32(6):992‐1000. [DOI] [PubMed] [Google Scholar]
- 18. Olson CL, Schumaker HD, Yawn BP. Overweight women delay medical care. Arch Fam Med. 1994;3(10):888‐892. [DOI] [PubMed] [Google Scholar]
- 19. Ferrante JM, Ohman‐Strickland P, Hudson SV, Hahn KA, Scott JG, Crabtree BF. Colorectal cancer screening among obese versus non‐obese patients in primary care practices. Cancer Detect Prev. 2006;30(5):459‐465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wee CC, McCarthy EP, Davis RB, Phillips RS. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med. 2000;132(9):697‐704. [DOI] [PubMed] [Google Scholar]
- 21. Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019‐1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sir‐Petermann T, Codner E, Perez V, et al. Metabolic and reproductive features before and during puberty in daughters of women with polycystic ovary syndrome. J Clin Endocrinol Metab 2009;94(6):1923‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Trent ME, Rich M, Austin SB, Gordon CM. Quality of life in adolescent girls with polycystic ovary syndrome. Arch Pediatr Adolesc Med. 2002;156(6):556‐560. [DOI] [PubMed] [Google Scholar]
- 24. Jones GL, Hall JM, Lashen HL, Balen AH, Ledger WL. Health‐related quality of life among adolescents with polycystic ovary syndrome. J Obstet Gynecol Neonatal Nurs. 2011;40(5):577‐588. [DOI] [PubMed] [Google Scholar]
- 25. Khomami MB, Tehrani FR, Hashemi S, Farahmand M, Azizi F. Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One. 2015;10(4):e0123608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Krentz AJ, von Muhlen D, Barrett‐Connor E. Searching for polycystic ovary syndrome in postmenopausal women: evidence of a dose‐effect association with prevalent cardiovascular disease. Menopause. 2007;14(2):284‐292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shah D, Bansal S. Polycystic ovaries—beyond menopause. Climacteric. 2014;17(2):109‐115. PubMed PMID: 23895379. [DOI] [PubMed] [Google Scholar]
- 28. Grol R, Wensing M, Mainz J, et al. Patients in Europe evaluate general practice care: an international comparison. Br J Gen Pract. 2000;50(460):882‐887. [PMC free article] [PubMed] [Google Scholar]
- 29. Geller DH, Pacaud D, Gordon CM, Misra M, of the D, Therapeutics Committee of the Pediatric Endocrine S . State of the art review: emerging therapies: the use of insulin sensitizers in the treatment of adolescents with polycystic ovary syndrome (PCOS). Int J Pediatr Endocrinol. 2011;2011:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Washburn JD, Birchler JA. Polyploids as a “model system” for the study of heterosis. Plant Reprod. 2014;27(1):1‐5. [DOI] [PubMed] [Google Scholar]
- 31. Khademi A, Alleyassin A, Aghahosseini M, Tabatabaeefar L, Amini M. The effect of exercise in PCOS women who exercise regularly. Asian J Sports Med. 2010;1(1):35‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jayasena CN, Franks S. The management of patients with polycystic ovary syndrome. Nat Rev Endocrinol. 2014;10(10):624‐636. [DOI] [PubMed] [Google Scholar]
- 34. Zeidan AM, Streiff MB, Lau BD, et al. Impact of a venous thromboembolism prophylaxis “smart order set”: improved compliance, fewer events. Am J Hematol. 2013;88(7):545‐549. [DOI] [PubMed] [Google Scholar]
- 35. Chang H. Book review: data‐driven healthcare & analytics in a big data world. Healthc Inform Res. 2015;21(1):61‐62. [Google Scholar]
- 36. Fung CH, Lim Y‐W, Mattke S, Damberg C, Shekelle PG. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med. 2008;148(2):111‐123. [DOI] [PubMed] [Google Scholar]
- 37. Washburn SP, Mullen KA. Invited review: genetic considerations for various pasture‐based dairy systems. J Dairy Sci. 2014;97(10):5923‐5938. [DOI] [PubMed] [Google Scholar]
- 38. Jay M, Kalet A, Ark T, McMacken M, Messito MJ, Richter R, et al. Physicians' attitudes about obesity and their associations with competency and specialty: A cross-sectional study. BMC health services research. 2009;9:106. [DOI] [PMC free article] [PubMed] [Google Scholar]


