1. INTRODUCTION
Health information was once generally collected and reserved either to inform clinical care, conduct research, or survey the public's health. Today, with digital data infrastructure, health information can technically flow between all of these purposes simultaneously, enabling learning health systems (LHSs) and related enterprises. LHSs are emerging through infrastructural innovation that allows for connectedness in data collection, analytics to transform data to knowledge, and application of that knowledge in practice and in ways that generate new data through evaluation of outcomes (Figure 1).1 LHSs create cycles of continuous improvement that will allow health systems to address well‐known, chronic maladies—e.g., high rates of medical error, spiraling costs, the slow rate of translational science, and failure to implement agreed‐upon best practices.2, 3 LHSs represent an innovation in health infrastructure such that learning occurs at multiple levels of scale, ranging from individuals, single practices, and systems to systems of systems spanning organizational and geopolitical boundaries. LHSs are successful when platforms and culture support efficient organization of technology, people, processes, and policy.4
Figure 1.
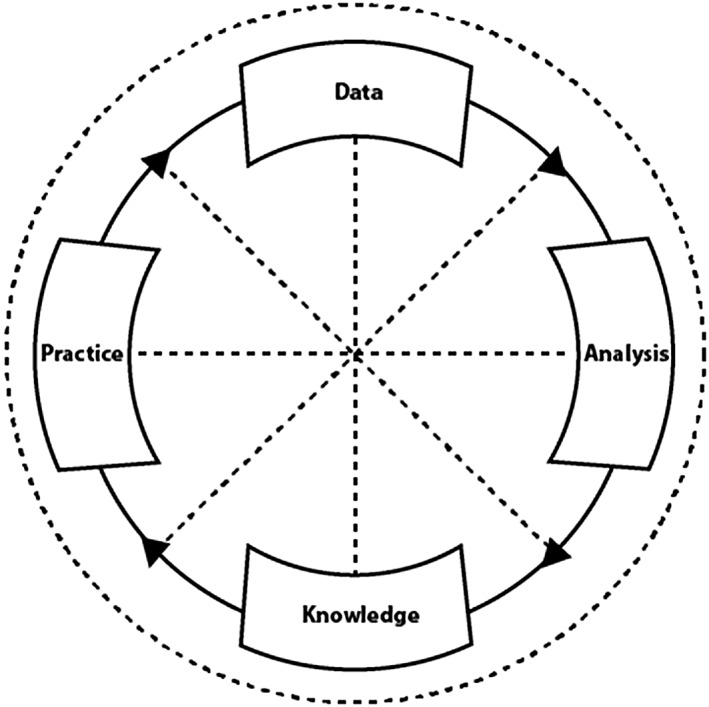
Learning health systems are infrastructural innovations
The use of data for learning presents both opportunities for reform of, and challenges to, existing regulations and ethical and legal frameworks for health information and knowledge exchange. At present, these frameworks govern information according to the intended, primary use of data collection. HIPAA, for example, sets boundaries for use and disclosure of protected health information, including electronic health record data, across covered users. Rules requiring consent for the use of patient data are shaped by type of use: for example, for treatment, payment, health care operations, or “public interest and benefit activities.”5 The complex legal and regulatory environment for health information has contributed to siloed and redundant systems with separate pipelines for research, public health, health care administration, and health care services.6 Current ethical and legal frameworks often allow exceptions at the individual level such as allowing for a waiver of informed consent for a research project under certain circumstances. Researchers conducting quality improvement studies rather than research also do not require Institutional Review Board (IRB) oversight.
Proponents of LHSs claim a moral imperative, which remains to be empirically tested, for data to be amassed, unencumbered by “outdated” frameworks that hinder the pursuit of knowledge and the timely dissemination of important findings.7, 8, 9 Ruth Faden and colleagues, for example, have offered a widely cited framework that reevaluates the obligations of stakeholders in the context of health as a learning health system as an initial position from which to launch a deeper dialogue and empirical evaluation of alternatives, implementation strategies, as well as the acceptability of this framework to the public and other stakeholders.10 There is much work to be done to examine the ethical, legal, and social implications of learning health systems (ELSI‐LHS). This special issue of Learning Health Systems, focused on ELSI‐LHS, contributes to the early stages of this work to inform health care in the digital age for individuals, communities, and systems to ensure the trustworthiness of LHSs.
2. ORIGINS OF THE ELSI‐LHS ISSUE OF THIS JOURNAL
In November 2016, the University of Michigan sought to begin establishing a community of expertise to explore the ethical, legal, and social implications of learning health systems. This effort included a symposium in Ann Arbor that applied the framework approach of Responsible Research and Innovation (RRI) to the LHS to identify key issues for future research and development. Initially defined in the context of the European Commission's Horizon 2020 initiative, RRI strives to ensure what the EU calls the “Science with and for Society,”11 integrating ELSI research with multi‐stakeholder engagement, system design, and implementation. The symposium brought together experts and leaders in bioethics, social science, medical practice, clinical research, community‐academic partnerships, and law with an interdisciplinary group of participants for a daylong session of presentations and dialogue. A link to a summary of presentations and a video from the November 2016 symposium is provided at the conclusion of this paper.
3. CRITICAL CONCEPTS AND EMERGING FRAMEWORKS
The articles in this special issue identify the need for new ELSI frameworks to inform practice. Scott Kim, Jeffrey Botkin, and John Lantos each reflect on how the de facto boundaries between health research, clinical care, quality improvement, and public health will be challenged by learning health systems and consider the implications for respect for persons and preserving autonomy. In the article, Ethical Issues in Pragmatic Trials of “Standard of Care” Interventions in Learning Healthcare Systems, Kim examines the ethics of pragmatic clinical trials and the integration of research and clinical procedures that could generate valuable data. He questions whether this would confound the research/treatment distinction as some learning health system visionaries have imagined and examines the implications for informed consent. Botkin further explores questions about autonomy and system‐level changes in his article titled Transparency and Choice in Learning Healthcare Systems. He argues that transparency and patient engagement will be critical in addressing potential conflicts between autonomy and public interest, and in maintaining trust, on which the learning health system is said to depend. He proposes that the use of a notice‐and‐opt‐out procedure in the place of traditional consent is appropriate when risks are low and institutional safeguards are in place.
In the Lantos article, The Regulation of Clinical Research: What's Love Got to Do with It, participation in learning is described as a moral obligation for both patients and health professionals who are not well served by our current system of research regulation. Lantos describes our deep history of viewing the moral obligations of clinicians and researchers as different, asserting that researchers do not share the goal—or attending moral authority—of healing the patient. But research, treatment, therapy, research on medical practices, quality improvement, pursuit of knowledge, and learning can be concurrent efforts with overlapping goals. Lantos suggests the shift toward learning health systems will require change not only in oversight and research regulation but also in culture and ethics, beginning with new governance systems that thoroughly engage patients or surrogates in all processes of learning. These conclusions are supported empirically in the article by Ramsberg and R. Platt, Opportunities and Barriers for Pragmatic Embedded Trials—Triumphs and Tribulations. It describes the use of “embedded pragmatic clinical trials” that leverage the availability of routinely collected electronic data. In interviews with researchers and clinicians, the authors note the demand for and cost‐benefit of governance adaptable to embedded pragmatic clinical trials in delivery systems.
Adoption of learning health system models brings tectonic shifts to the structure, culture, and organization of health, raising important questions about how these changes might offer an opportunity to address current inequities endemic to our health system. Frameworks that would support these shifts are explored in the article, Leveraging the Learning Healthcare Model to Improve Equity in the Age of Genomic Medicine, in which authors Bonham and Blizinsky consider how LHSs could address health disparities and health equity. They note that truly inclusive systems pose formidable challenges but might also address the current lacunae in genomic databases that have made it impossible in some cases to inform medical development based on available data because for some populations, we simply do not have data available.
4. THE FUTURE OF ELSI‐LHS
This special issue of Learning Health Systems highlights an initial set of issues for ELSI‐LHS, including the ways in which LHS challenge the ethical, legal, and social differentiations between quality improvement, research, and clinical care. As systems become larger and increasingly fluid between these ethical and legal paradigms, expectations for informed consent and moral obligations of patients, participants, providers, and other stakeholders in health are challenged and need to be further developed and explored. Thus, ELSI‐LHS promises to be an increasingly rich field of inquiry and learning.
This special issue highlights the importance of respect, honor, and trust as foundational to better care and to LHSs. To make these principles central to the actualization of the LHS vision, major social and cultural changes in health must accompany the technological changes that come with implementing a LHS. Indeed, advocates of ELSI‐LHS will be successful insofar as they work with the technical developers of LHSs, making visible the underlying value systems and identifying opportunities to reduce disparities while providing benefits equitably. As systems that operate at micro and macro levels, LHSs need to identify ways to ameliorate unintended consequences and ensure that the human experience is not lost in a web of big data and new tools. Ideally, this occurs in ways that are compatible and synchronized with technological development and the IT maturity models applicable to LHSs. Careful attention to emerging examples of local, state, national, and global LHSs will ground ELSI frameworks and maturity models in the realm of what is practicable in the near and long term. It will require continued engagement of a transdisciplinary community of stakeholders, including community and patient voices, as well as informaticians, epidemiologists and biostatisticians, medical researchers and practitioners, public health practitioners, social scientists, and bioethicists in their development and implementation.
Harnessing the power of health data for LHSs opens new opportunities to modernize and “hardwire” core principles and values, creating true integration of “social” and “technical” in a sociotechnical system. This issue provides an initial set of work that seeds this partnership. In organizing, pursuing, expanding, and communicating this work, we provide an ecologically friendly soil for an ELSI‐LHS worthy of trust by the people it serves, and a system of health and learning deserving of its name.
5. 2016 ELSI‐LHS SYMPOSIUM
The 2016 ELSI‐LHS Symposium presentations may be viewed at https://youtu.be/pCwdRlNXLms?list=PLrfgcyeUc0IkqAjU_YONaBnM5F1‐FOpEV.
FUNDING STATEMENT
This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
CONFLICTS OF INTEREST
The authors have no competing interests to declare.
CONTRIBUTORSHIP STATEMENT
All authors contributed to the conceptualization, writing, and revision of this manuscript.
Supporting information
A description of the 2016 ELSI‐LHS Symposium and presentations is also available; click the Supporting Information tab associated with the online version of this article.
Supporting Info Item
Platt J, Spector‐Bagdady K, Platt T, et al. Ethical, legal, and social implications of learning health systems. Learn Health Sys. 2018;2:e10051 10.1002/lrh2.10051
REFERENCES
- 1. Friedman C, Rubin J, Brown J, et al. Toward a science of learning systems: a research agenda for the high‐functioning Learning Health System. J Am Med Inform Assoc. 2015;22(1):43‐50. 10.1136/amiajnl-2014-002977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Etheredge LM. A rapid‐learning health system. Health Aff. 2007;26(2):w107‐ww18. [DOI] [PubMed] [Google Scholar]
- 3. Friedman CP, Wong AK, Blumenthal D. Achieving a nationwide learning health system. Sci Translat Med. 2010;2(57):57cm29‐57cm29. [DOI] [PubMed] [Google Scholar]
- 4. Friedman C, Rubin J, Sullivan K. Toward an information infrastructure for Global Health Improvement. Yearbook Med Informat. 2017;26(01):16‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. HIPAA Privacy Rule . 45 CFR Part 160 and subparts A and E of part 164.
- 6. Ainsworth J, Buchan I. Combining health data uses to ignite health system learning. Methods Inf Med. 2015;54(6):479‐487. [DOI] [PubMed] [Google Scholar]
- 7. Krumholz HM. Big data and new knowledge in medicine: the thinking, training, and tools needed for a learning health system. Health Aff. 2014;33(7):1163‐1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Miriovsky BJ, Shulman LN, Abernethy AP. Importance of health information technology, electronic health records, and continuously aggregating data to comparative effectiveness research and learning health care. J Clin Oncol. 2012;30(34):4243‐4248. [DOI] [PubMed] [Google Scholar]
- 9. Schneeweiss S. Learning from big health care data. New Eng J Med. 2014;370(23):2161‐2163. [DOI] [PubMed] [Google Scholar]
- 10. Faden RR, Kass NE, Goodman SN, Pronovost P, Tunis S, Beauchamp TL. An ethics framework for a learning health care system: a departure from traditional research ethics and clinical ethics. Hastings Center Report. 2013;43(s1):S16‐S27. [DOI] [PubMed] [Google Scholar]
- 11. Horizon 2020: Science with and for society. Secondary Horizon 2020: Science with and for Society. https://ec.europa.eu/programmes/horizon2020/en/h2020‐section/science‐and‐society.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A description of the 2016 ELSI‐LHS Symposium and presentations is also available; click the Supporting Information tab associated with the online version of this article.
Supporting Info Item


