Abstract
The health system in Switzerland is considered as one of the best in the world. Nevertheless, to effectively and efficiently meet current and future challenges, an infrastructure and culture are needed where the best evidence is systematically made available and used, and the system evolves on the basis of a constant exchange between research, policy, and practice. The Swiss Learning Health System institutionalizes this idea as a multistakeholder national initiative to ensure continuous improvement through ongoing research and implementation. This article presents the objectives and mechanisms of the Swiss Learning Health System in the context of international initiatives to strengthen health systems and improve population health through learning cycles.
Keywords: evidence‐informed decision‐making, LHS infrastructure, management of health information, scientific capacity building, stakeholder dialogue
1. INTRODUCTION
Modern health systems will face increasing challenges over the coming years. These include a growing aging population, a growing noncommunicable disease burden with increasing numbers of multimorbid patients and technological advances, including the digitalization of health; all of which will change the demands on health care providers and health systems at large.
In Switzerland, the Swiss Federal Office of Public Health (FOPH) emphasized already in 2012 the need to strengthen health services research and to develop a health system that is tailored to the needs of the population.1, 2 Despite important progress made over the last years, the FOPH still considers the further development of health services research to be central.3 The Swiss Academy of Medical Sciences (SAMS) in cooperation with the Bangerter Ryhner Foundation,4 for example, provided significant funding for research projects focusing on health services, and the National Research Programme “Smarter Health Care” (NRP74) ensures that innovative research in the field will receive continuous funding at least until 2022.5 The SAMS sees health services research, alongside biomedical and clinical research, as the third pillar in the health sciences.6 In line with this, the SAMS has formulated a number of recommendations for the medium to long‐term development of research competencies, including the systematic promotion of young researchers, infrastructure projects, and data collection efforts.6 (p8)
The Swiss Learning Health System (SLHS) project was launched in response to this call. Supported by the State Secretariat for Education, Research and Innovation (SERI), and initially by seven academic funding partner institutions, the SLHS aims to develop and implement a national platform for health systems and services research, policy, and practice. The overarching objective of the SLHS is to strengthen the health system in Switzerland and to create a culture of shared decision‐making in which sound scientific evidence is continuously integrated into the health system.
In the following, we will give a brief overview of the learning health system (LHS) concept and the current status of LHS initiatives worldwide before describing the vision and goals of the SLHS. We will outline the SLHS mechanisms, in particular the development and implementation of structured learning cycles for bridging research, policy and practice, scientific capacity building, and the management of standardized health information. We will highlight current activities to establish the SLHS as a national initiative and provide a tentative outlook on global LHS developments.
2. LEARNING HEALTH SYSTEMS
The idea of a LHS is based on the assumption that a health system can learn when it can rely on cyclic processes.7, 8, 9, 10, 11 These processes collect relevant data for the health system, which serve as a basis for the generation of new evidence. The evidence is transferred into practice for implementation, and data generated from practice as well as experience from implementation are fed back into the cycle, to learn from it, and possibly change or refine policies and practice to improve outcomes. Friedman et al12 describe this cyclical process as: data to knowledge (D2K), knowledge to performance (K2P), and performance to data (P2D). The aim of such a cycle is to identify effective and efficient measures to address specific problems. Such problems can be on all levels of the health system, from microlevel to mesolevel and macrolevel, and are not restricted solely to the provision of health care services but include all components of the health system.
While LHS structures have mainly been established in the United States since 2007, partly supported and promoted by the National Science Foundation12, 13, 14 (examples for LHS initiatives in the United States include CancerLinQ,15 PCORnet,16, 17 the Sentinel Initiative,18 or the Health Care Systems Research Network19), interest in LHSs has now spread globally and is gaining more and more interest. Examples include the TRANSFoRm project supported by the European Union20 the European Institute for Innovation through Health Data,21 the Learning Healthcare Project in the United Kingdom,22 or the Asia Pacific Network for Health Systems Strengthening23; see also Friedman et al12 for a summary and short description of these different LHS initiatives.
For a health system to be able to learn, there is need for a suitable infrastructure and culture that support the routine application of learning cycles. Above all, a functioning LHS relies on a constant exchange between research, policy, and practice. This is not only a question of communication and dissemination of research results, it is also a matter of timeliness and the suitability of research to address health system needs. The willingness of a solution‐oriented discourse of all stakeholders is a precondition to identify and understand current and future problems and collaboratively develop suitable solutions and implementation strategies. Therefore, a constant and systematic involvement of the various stakeholders in the health system is an essential basis for a LHS.
Against this background, the SLHS in Switzerland is the first initiative worldwide that builds an LHS at the national level.12 The conceptual basis for the SLHS is given by the Health Systems Framework of the World Health Organization (WHO24, 25, 26) and the concept of the LHS of the Institute of Medicine and the National Academy of Medicine in the United States.7, 8, 9 Of particular relevance for developing the SLHS is the systems thinking approach for health systems strengthening.25, 26 This approach highlights the dynamic architecture and interconnectedness of the health system building blocks (service delivery, health workforce, the health information system, essential medical products and technologies, health care financing, leadership, and governance) and the role of people at the center of the health system, as mediators, beneficiaries, and drivers of the system.25
3. GOALS OF THE SWISS LEARNING HEALTH SYSTEM
The vision of the SLHS is a health system that is responsive to current and future health needs, where services, programs, and policies are based on the best evidence available, where improvement is continuous through ongoing research and implementation, and where infrastructure enables learning processes on all levels of the system.27 In order to achieve this vision, the SLHS seeks to establish mechanisms that support decision‐makers in finding and using the best evidence available and through deliberative dialogue, to engage them to implement change that will strengthen the health system, on all levels and along the continuum of care.
The goals of the SLHS are therefore
to establish a bridging mechanism between research, policy, and practice;
to build scientific capacities for health systems and services research;
to develop standards for the management of health information.
These goals shall be achieved by applying specific mechanisms, as outlined in the next sections.
4. BRIDGING RESEARCH, POLICY, AND PRACTICE
The establishment of a bridging mechanism between research, policy, and practice is at the heart of the SLHS. This mechanism can be represented by the cycle shown in Figure 1.
Figure 1.
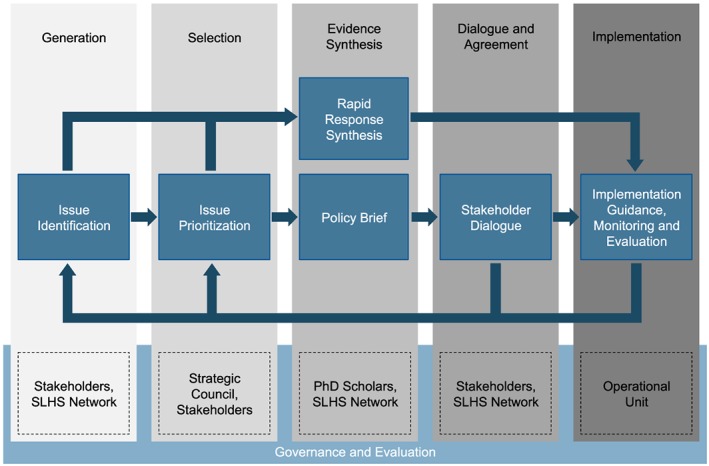
Bridging mechanism in the Swiss Learning Health System (SLHS)—the SLHS cycle
4.1. Issue identification and prioritization
Through a systematic and ongoing dialogue between researchers, policy‐makers, and practitioners, the SLHS continuously identifies and monitors current challenges (issues) in the Swiss health system. This is realized in part through exchange at existing meetings at the local and national level and through carefully planned stakeholder meetings, workshops, and focus groups, involving stakeholders from all areas of the health system. The Strategic Council of the SLHS, which is currently represented by the existing funding partner institutions (see first page), plays a central role in the process of topic prioritization. In close collaboration with all stakeholders—and taking into account ethical and legal principles as well as the expertise of the various research groups involved in the SLHS—topics that are relevant to the Swiss health system are prioritized for the initiation of learning cycles.
4.2. Evidence synthesis
For prioritized topics, the SLHS develops the so‐called evidence syntheses. All academic partner institutions and their networks are involved in this process. The process involves the development of policy briefs (as input for stakeholder dialogues) or rapid response syntheses. Policy briefs have the goal of describing and explaining the problem of interest, including all contextual factors and specific aspects of the Swiss health system. At the same time, they identify evidence‐based solutions to the problem and evaluate their costs and benefits. The policy brief also discusses possible barriers to and opportunities for implementation. For spontaneously occurring and pressing issues that may require prompt action, the SLHS provides rapid response syntheses as an alternative mechanism. Based on the current state of research knowledge, rapid response syntheses summarize the best available solutions for a specific problem in an abbreviated and accelerated manner.
4.3. Stakeholder dialogue
Decision‐making in health policy is a participatory process, which requires stakeholders to interact in order to identify and agree on the best possible solution to a given problem or issue that needs to be addressed. This interaction does not take place in a vacuum but is influenced by many partially conflicting factors, such as the institutional and legal framework, different interests, values, and time and resource constraints. Often, it is also hindered by the communication process itself. As a result, transfer of knowledge and relevant application of new evidence fails. Using a stakeholder dialogue approach, the SLHS aims to provide a mechanism that supports evidence‐based decision‐making in both policy and practice. The stakeholder dialogue, which conceptually draws from the McMaster Health Forum28 (see also references herein29, 30, 31, 32), is a structured communication process in which stakeholders (1) agree on the problem to be discussed, (2) explain and argue for their positions on the various alternative solutions, and (3) agree on the best course of action. Supported by the principles of deliberative communication,33 the SLHS implements the stakeholder dialogue as a normative model of critical discussion to facilitate stakeholders in reaching agreement.34 Stakeholder dialogues, along with policy briefs, are effective mechanisms for identifying and prioritizing evidence‐based measures that can be successfully and sustainably implemented in the health system,34 on all levels of decision‐making from clinical to organizational and policy‐level decisions. In addition, stakeholder dialogues provide opportunities to identify new topics for a research agenda that addresses the needs and existing gaps in the health system.
4.4. Support in the implementation phase
Essential for a LHS is the ongoing evaluation of change to provide new data and insights that will serve as a new input for practice and implementation. The SLHS therefore carefully monitors and accompanies implementation efforts of measures that stakeholders have agreed on in a dialogue or which have been decided on the basis of rapid response syntheses. The collected data are analyzed and made available to stakeholders to evaluate the changes that have been made, and both the data and insights gained from the evaluation are reintegrated into research, policy, and practice for possible revision, refinement, and improvement of change, in the sense of a LHS.
5. BUILDING SCIENTIFIC CAPACITIES
Building scientific capacities is the second important goal of the SLHS. The availability of well‐trained and capable research scientists, with a working ability to understand and structure research at the intersection of science, policy, and practice, is essential for establishing an LHS. Initially, 20 doctoral scholarships are awarded for 4 years (financed by the funding partner institutions and the SERI in a matched funding model). Doctoral students play a central role in the SLHS. They actively contribute to the SLHS cycles in preparing evidence syntheses and stakeholder dialogues and producing new knowledge that directly benefits the Swiss health system. In addition, doctoral students take advantage of the high‐quality course program offered by the Swiss School of Public Health (SSPH+). Together with the SSPH+, the SLHS has developed a structured training program in specific LHS‐related topics. Courses cover a variety of topics, introducing students to concepts and skills relevant to a LHS. The program serves as an opportunity to develop a common understanding and language of a Swiss LHS, despite different academic backgrounds and socializations.
An LHS enhancement program supplements the existing training opportunities in Switzerland, with specific training on the principles of a LHS. These include courses on SLHS‐specific topics such as policy brief development and stakeholder dialogues, and meetings in which SLHS activities are presented and discussed. Activities are open to all interested researchers, policy‐makers, and practitioners. The aim is to develop and promote a common language and to create a shared culture for a LHS that goes beyond the current partners of the SLHS.
6. MANAGEMENT OF STANDARDIZED HEALTH INFORMATION
According to the WHO, the availability of health information is a central building block of health systems.24, 25 The collection, analysis, and dissemination of reliable and up‐to‐date information is therefore an important prerequisite for the successful operation of a health system at all levels. In collaboration with the WHO, national and international health professionals, the SLHS aims to develop national data standards that include (1) a comprehensive description of the health system, and (2) comprehensive reporting on the health and functioning of individuals and society as a whole. Conceptually, data standards should serve as a bridging mechanism between common clinical and self‐reported measurement tools. A key aspect of developing data standards is improving data quality. The SLHS Health Data Warehouse is designed to identify, describe, exploit, compare, and network existing data sources (cohort studies, surveys, hospital and insurance data, and general statistics). Moreover, the SLHS Health Data Warehouse allows to provide access to newly collected data, for example, as generated in the learning cycles. The aim is to standardize and facilitate the use of data for researchers within and outside the SLHS. To this end, the SLHS supports the manifest for better health data adopted in 2013 by various institutions and organizations in Switzerland.35
To establish an information infrastructure that supports multiple and simultaneous learning cycles, the SLHS aims at building supplementary data collection efforts. Among others, this includes the Health System Lab, which sets up experimental laboratory facilities to test new theories and simulate policy and practice impact. Further, a knowledge grid is planned to represent the knowledge acquired in the SLHS through research, dialogues, and implementation and make it (re‐)usable and actionable in a given or in alternative contexts, efficiently, and with economies of scale.36, 37
7. SUSTAINABILITY OF THE SLHS AS A MULTISTAKEHOLDER INITIATIVE
The SLHS is set out as the first initiative worldwide to establish a LHS on a national scale. It started in 2017 as a project of the following universities and universities of applied sciences:
University of Basel: Swiss Tropical and Public Health Institute (associated institute),
Université de Neuchâtel,
University of Lucerne,
University of Zurich,
Scuola universitaria professionale della Svizzera italiana,
Zurich University for Applied Sciences.
In addition to existing partner networks and institutions such as the SSPH+, the Institute of Primary and Community Care in Lucerne, or Swiss Paraplegic Research, the SLHS strives to build a broad network in the sense of a nationwide platform for health systems and services research, policy, and practice. To this end, other institutions are currently joining the SLHS as partner institutions, endorsing the following 8 core values of the SLHS (based on the core values developed during the LHS summit in the US in 201238 and adapted by the SLHS Strategic Council in 2017):
Person‐centeredness: Through active engagement with the health system and all its stakeholders, the SLHS is committed to improving people's well‐being and quality of life. It places the person at the center of its activities.
Inclusiveness: Every individual and organization committed to improving population health and strengthening the health system, who abides by the governance of the SLHS, is invited and encouraged to participate.
Transparency and accessibility: The activities of the SLHS are transparent in order to safeguard and deepen the trust of all stakeholders in the health system. All should benefit from the public good that is derived from the SLHS.
Privacy: The SLHS protects the privacy, confidentiality, and security of all data to enable responsible sharing of information and to build trust among all stakeholders.
Adaptability: The SLHS is designed to enable iterative, rapid adaptation, and incremental evolution to meet current and future needs of the health system.
Governance: Through its governance, the SLHS aims at supporting its sustainable operation, setting required standards, stimulating ongoing innovation, and building and maintaining mutual trust among all stakeholders involved.
Scientific integrity: Researchers in the SLHS share a commitment to the most rigorous application of science to ensure the validity and credibility of findings, and open sharing and implementation of new knowledge in a timely and responsible manner.
Quality and value for all: The SLHS supports learning activities that serve to improve the effectiveness and efficiency of services and promote equitable access to high quality care.
Partner institutions of the SLHS actively contribute to the development of the SLHS by initiating new learning cycles, preparing and developing usable relevant evidence, and enabling decision‐makers to implement change through deliberative dialogue. A broad network of partner institutions will help to effectively and efficiently build up the infrastructure needed to successfully run an LHS on a national scale, contribute to the sustainable implementation of the idea of an LHS in Switzerland, and through collaborative action, support continuous health system improvement.
8. CONCLUSION
This article presented the SLHS, a national initiative to establish learning cycles for continuous health system improvement. The SLHS is built around 3 main goals: (1) the establishment of a bridging mechanism between research, policy, and practice, (2) building scientific capacities for a new generation of health researchers, and (3) the development of standards for the management of health information. These 3 priority action areas are understood to be fully integrated components of the SLHS and are essential for the sustainable implementation of an LHS on a national scale. The SLHS is still in its early stages, and learning cycles are just now being initiated. The infrastructure that is currently being developed builds on existing LHS structures and thus is compatible with other LHS initiatives, such as the ones in the United States, the United Kingdom, or other more local initiatives. The overarching perspective is to realize a global LHS. This would be a system in which new knowledge and new information is made available in a timely and actionable manner, within and across countries, where synergies can be fully exploited and health systems learning becomes more effective and efficient, allowing a seamless flow between research, policy, and practice to improve the health and well‐being of individuals and populations across the globe.
DISCLAIMER
Parts of this manuscript are based on the project proposal of the SLHS (available online via https://www.slhs.ch/images/Proposal_Swiss_Learning_Health_System.pdf) and a related article that has been published in German in the journal “Schweizerische Ärztezeitung”, 2017, 98:39.
Boes S, Mantwill S, Kaufmann C, et al. Swiss Learning Health System: A national initiative to establish learning cycles for continuous health system improvement. Learn Health Sys. 2018;2:e10059 10.1002/lrh2.10059
Consortium of funding partner institutions in the SLHS and local coordinators:
University of Basel, Swiss Tropical and Public Health Institute (SwissTPH); Kaspar Wyss
University of Neuchâtel; Paul Cotofrei, Kilian Stoffel
University of Lugano; Stefano Calciolari, Marco Meneguzzo
University of Lucerne (Lead Institution); Gerold Stucki, Stefan Boes, Adrian Loretan, Bernhard Rütsche
University of Zurich; Thomas Rosemann, Stefan Neuner‐Jehle
University of Applied Sciences and Arts of Southern Switzerland (SUPSI); Luca Crivelli, Carlo De Pietro
Zurich University of Applied Sciences (ZHAW); Karin Niedermann, Astrid Schämann, Simon Wieser
Swiss School of Public Health (SSPH+); Nino Künzli
REFERENCES
- 1. Federal Office of Public Health . Forschungskonzept Gesundheit 2013‐2016. Bern: Federal Office of Public Health (FOPH), Bundeamt für Gesundheit (BAG); 2012. Januar 2012. [Google Scholar]
- 2. Federal Office of Public Health . Health2020. The Federal Council's health‐policy priorities. Bern: Federal Office of Public Health (FOPH) Bundesamt für Gesundheit (BAG); 2013. Januar 2013. [Google Scholar]
- 3. Federal Office of Public Health . Forschungskonzept Gesundheit 2017‐2020. Bern: Federal Office of Public Health (FOPH), Bundeamt für Gesundheit (BAG); 2015. December 2015. [Google Scholar]
- 4. Röthlisberger M, Amstad H. Förderprogramm «Versorgungsforschung im Gesundheitswesen». Schweiz Ärzteztg. 2017;98(3):59‐61. [Google Scholar]
- 5. National Research Programme “Smarter Health Care” (NRP74) . http://www.nfp74.ch/en
- 6. Schweizerische Akademie der Medizinischen Wissenschaften . Stärkung der Versorgungsforschung in der Schweiz. 2014;Swiss Academies Reports 9(1).
- 7. Institute of Medicine . The Learning Healthcare System: Workshop Summary. Washington, DC: The National Academies Press; 2007. [PubMed] [Google Scholar]
- 8. Institute of Medicine . Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 9. National Academy of Medicine (NAM) . Learning health system series. See https://nam.edu/programs/value‐science‐driven‐health‐care/learning‐health‐system‐series [last accessed Feb 12, 2018]
- 10. Institute of Medicine . Table of characteristics of a continuously learning health care system. 2012. See http://www.nationalacademies.org/hmd/Reports/2012/Best‐Care‐at‐Lower‐Cost‐The‐Path‐to‐Continuously‐Learning‐Health‐Care‐in‐America/Table.aspx [last accessed Feb 12, 2018]
- 11. Friedman CP, Wong AK, Blumenthal D. Achieving a nationwide learning health system. Sci Transl Med. 2010;2(57):57cm29. [DOI] [PubMed] [Google Scholar]
- 12. Friedman CP, Rubin JC, Sullivan KJ. Toward an information infrastructure for global health improvement. Yearb Med Inform 2017. 2017;26:16‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Friedman CP, Rubin JC, Brown JS, et al. Toward a science of learning systems: a research agenda for the high‐functioning learning health system. J Am Med Inform Assoc. 2015;22(1):43‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Science Foundation (NSF) . Toward a science of learning systems: the research challenges underlying a national‐scale learning health system: findings from a multi‐disciplinary workshop supported by the national science foundation. Washington, DC; 2013. Nov11. See https://medicine.umich.edu/sites/default/files/content/downloads/NSF%20Report%20Ver%2011.11.13%20FWR.pdf [last accessed Feb 12, 2018]
- 15. CancerLinQ LLC, a subsidiary of the American Society of Clinical Oncology. www.cancerlinq.org
- 16. Collins FS, Hudson KL, Briggs JP, Lauer MS. PCORnet: turning a dream into reality. J Am Med Inform Assoc. 21(4):576‐577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fleurence RL, Curtis LH, Califf RM, Platt R, Selby JV, Brown JS. Launching PCORnet, a national patient‐centered clinical research network. J Am Med Inform Assoc. 2014;21(4):578‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. FDA's Sentinel Initiative, US Food and Drug Administration . https://www.fda.gov/Safety/FDAsSentinelInitiative/default.htm
- 19. Health Care Systems Research Network . http://www.hcsrn.org/en/
- 20. Delaney BC, Curcin V, Andreasson A, et al. Translational medicine and patient safety in Europe: TRANSFoRm—architecture for the learning health system in Europe. Biomed Res Int. 2015;2015. Article ID 961526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kalra D, Stroetmann V, Sundgren M, et al. The European institute for innovation through health data. Learn Health Syst. 2017;1(1):e10008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Foley T. Background: need for LHS. The Learning Healthcare Project UK. Newcastle University UK. 2015. http://www.learninghealthcareproject.org/section/background/need‐for‐lhs [last accessed Feb 12, 2018]
- 23. Asia Pacific Network for Health Systems Strengthening . http://www.anhss.org.
- 24. World Health Organization (WHO) . Everybody's Business: Strengthening Health Systems to Improve Health Outcomes: Who's Framework for Action. Geneva: WHO; 2007. [Google Scholar]
- 25. De Savigny D, Adam T. (Eds). Systems Thinking for Health Systems Strengthening. Geneva: Alliance for Health Policy and Systems Research, WHO; 2009. [Google Scholar]
- 26. van Olmen J, Marchal B, van Damme W, Kegels G, Hill PS. Health systems frameworks in their political context: framing divergent agendas. BMC Public Health. 2012;12(1):774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Swiss Learning Health System . http://www.slhs.ch
- 28. McMaster Health Forum . http://www.mcmasterforum.org
- 29. Lavis JN, Oxman AD, Lewin S, Fretheim A. SUPPORT tools for evidence‐informed health policymaking (STP). Health Res Policy Syst. 2009;7(Suppl 1):I1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lavis JN, Permanand G, Oxman AD, Lewin S, Fretheim A. SUPPORT tools for evidence‐informed health policymaking (STP). 13. Preparing and using policy briefs to support evidence‐informed policymaking. Health Res Policy Syst. 7(Suppl 1):S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lavis JN, Boyko JA, Oxman AD, Lewin TJ, Fretheim A. SUPPORT tools for evidence‐informed health policymaking (STP). 14. Organising and using policy dialogues to support evidence‐informed policymaking. Health Res Policy Syst. 2009;7(Suppl 1):S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fretheim A, Oxman AD, Lavis JN, Lewin S. SUPPORT tools for evidence‐informed health policymaking (STP). 18. Planning monitoring and evaluation of policies. Health Res Policy Syst. 7(Suppl 1):S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. van Eemeren FH, Grootendorst R. A Systematic Theory of Argumentation: The Pragma‐Dialectical Approach. Cambridge: Cambridge University Press; 2004. [Google Scholar]
- 34. Rubinelli S, von Groote PM. Stakeholder dialogue as deliberation for decision making in health policy and systems: the approach from argumentation theory. Am J Phys Med Rehabil. 2017;96(2):S17‐S22. [DOI] [PubMed] [Google Scholar]
- 35. Public Health Switzerland . Bessere Gesundheitsdaten für ein effizienteres Gesundheitswesen. Manifest presented during the Swiss Public Health Conference 2013 in Zurich. 2013. http://www.public‐health.ch/logicio/client/publichealth/file/130816_Manifest_Gesundheitsdaten_D_def.pdf [last accessed Feb 12, 2018].
- 36. Flynn AJ, Shi W, Fischer R, Friedman CP. Digital knowledge objects and digital knowledge object clusters: unit Holdings in a Learning Health System Knowledge Repository. In: 49th Hawaii International Conference on System Sciences (HICSS) Conference on 2016 Jan 5, (Pp 3308‐3317). IEEE. 2016.
- 37. Flynn AJ, Bahulekar N, Boisvert P, et al. Architecture and initial development of a digital library platform for computable knowledge objects for health. Stud Health Technol Inform. 2017;235:496‐500. [PubMed] [Google Scholar]
- 38. Learning Health Community . Mission, Vision and Values of the LHC. Core Values Underlying a National‐Scale Person‐Centered Continuous Learning Health System. http://www.learninghealth.org/about‐the‐community/


