Abstract
Objective
We aimed to assess the safety of opioids in the management of osteoarthritis (OA) in a systematic review and meta-analysis of randomized, placebo-controlled trials.
Methods
A comprehensive literature search was undertaken in the MEDLINE, Cochrane Central Register of Controlled Trials (Ovid CENTRAL), and Scopus electronic databases. Randomized, double-blind, placebo-controlled, parallel-group trials that assessed adverse events (AEs) with opioids in patients with OA were eligible for inclusion. Two authors appraised titles, abstracts and full-text papers for suitability and then assessed the studies for random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data and selective outcomes reporting. The primary outcomes of interest were gastrointestinal (GI) disorders, cardiac disorders, vascular disorders, nervous system disorders, skin and subcutaneous tissue disorders, renal and urinary disorders, respiratory, thoracic and mediastinal disorders, as well as overall severe and serious AEs and drug-related AEs. Secondary outcomes were withdrawals due to AEs (i.e. the number of participants who stopped the treatment due to an AE) and total number of AEs (i.e. the number of patients who experienced any AE at least once).
Results
Database searches identified 2189 records, from which, after exclusions, 17 papers were included in the meta-analysis. More disorders of the lower GI tract (constipation, fecaloma) were reported with both immediate-release (IR) and extended-release (ER) formulations of opioids versus placebo: IR opioids (relative risk [RR] 5.20, 95% confidence interval [CI] 3.42–7.89); ER opioids (RR 4.22, 95% CI 3.44–5.17). The risk of upper GI AEs increased fourfold with ER opioids compared with placebo (RR 4.03, 95% CI 0.87–18.62), and the risk of nausea, vomiting or loss of appetite increased four- to fivefold with both formulations: IR opioids (RR 3.39, 95% CI 2.22–5.18); ER opioids (RR 4.03, 95% CI 3.37–4.83). An increased risk of dermatologic AEs (rash and pruritis; IR opioids: RR 3.60, 95% CI 1.74–7.43; ER opioids: RR 7.87, 95% CI 5.20–11.89) and central nervous system disorders (dizziness, headache, fatigue, somnolence, insomnia; IR opioids: RR 2.76, 95% CI 1.90–4.02; ER opioids: RR 2.76, 95% CI 2.19–3.47) was found with all opioid formulations versus placebo.
Conclusions
Our results confirm that there are considerable safety and tolerability issues surrounding the use of opioids in OA, and support the recommendation of international and national guidelines to use opioids in OA after other analgesic options, and for short time periods.
Electronic supplementary material
The online version of this article (10.1007/s40266-019-00666-9) contains supplementary material, which is available to authorized users.
Key Points
| Our analysis shows that oral opioids are associated with an increased risk of adverse events of the gastrointestinal, dermatologic, and central nervous systems when compared with placebo, regardless of whether the immediate-release or extended-release formulations are employed. |
| We recommend cautious use of opioids in the treatment of osteoarthritis in light of these findings. |
Introduction
Osteoarthritis (OA) is the most common form of joint disease and a leading cause of pain and physical disability in older people [1, 2]. OA is a progressive, degenerative disease of the synovial joints causing joint pain and functional impairment with different degrees of disease severity that requires long-term management with various treatment options over the course of the disease [3]. Opioids are potent analgesics that work by targeting mainly spinal and supraspinal opioid receptors. Cellular studies suggest that there are peripheral opioid receptors in inflamed osteoarthritic synovial tissue that may mediate analgesic effects [4]. Opioid prescription for OA is certainly common [5], but prescribing practices vary widely [6]. Opioids may be considered in OA if the pain is severe, or if other analgesics are contraindicated [7].
However, evidence regarding the safety and efficacy of opioids in OA is contradictory [8, 9], and thus some guidelines regard the use of opioids in OA as uncertain (the Osteoarthritis Research Society International [OARSI]) [10], while others limit their use to the last pharmacologic option for the severely symptomatic knee OA patient before surgery (the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases [ESCEO]) [11, 12], or for patients with hip or knee OA who have had inadequate response to other therapies and are either unwilling to undergo or are not suitable candidates for surgery (the American College of Rheumatology [ACR]) [13].
A Cochrane review of oral or transdermal opioids in 22 randomized controlled trials (RCTs) up to 2012 concluded that the small mean benefit of non-tramadol opioids is contrasted by a significant increase in the risk of adverse events (AEs) [7, 14]. The estimated effect size for pain was 0.28 (standardized mean difference [SMD], 95% confidence interval [CI] − 0.35 to − 0.20), which corresponds to a difference in pain score of 7 mm on a 100 mm visual analogue scale (VAS) between opioids and placebo; this was considered as being of questionable clinical relevance since the 95% CI did not include the minimal clinically important difference (MCID) of 0.37 SMD (9 mm on a VAS) [7]. AEs were more frequent in patients receiving opioids than controls; the relative risk (RR) of any AE was 1.49 (95% CI 2.93–4.82). Patients receiving opioids were nearly fourfold as likely to withdraw due to AEs (RR 3.76, 95% CI 3.06–5.38), and threefold as likely to experience a serious AE (SAE) [RR 3.35, 95% CI 0.83–13.56) [14].
A meta-analysis of 19 RCTs and review of opioids found that in spite of analgesic effects, many OA patients stop chronic opioid use due to AEs. Analgesic effects were significantly better than placebo in opioid-treated patients (p = 0.01) [15, 16]; however, opioid treatment was associated with a significantly increased total dropout rate (odds ratio [OR] 1.3, 95% CI 1.2–1.4), and discontinuation of treatment was related to AEs (OR 4.0, 95% CI 3.4–4.6).
A recent meta-analysis of oral and transdermal opioids for pain in musculoskeletal conditions in older patients (aged > 60 years) found that opioid analgesics had only a limited effect on pain and disability. Opioids had a small effect on decreasing pain intensity (SMD − 0.27, 95% CI − 0.33 to − 0.20), while the odds of AEs with opioids were threefold higher (OR 2.94, 95% CI 2.33–3.72) and the odds of treatment discontinuation due to AEs was fourfold higher (OR 4.04, 95% CI 3.10–5.25) [17].
Extended-release (ER) or controlled-release (CR) formulations may improve opioid tolerability in OA patients by preventing the high plasma peaks that are associated with the AEs observed with the immediate-release (IR) formulations [18]. A meta-analysis of four RCTs of patients with musculoskeletal pain found that ER tapentadol (100–250 mg/day) is associated with a reduction in pain intensity in comparison with placebo and oxycodone. In addition, no increase in SAEs was reported when comparing tapentadol with placebo (RR 1.02, 95% CI 0.47–2.16) [19].
There is a paucity of meta-analysis data assessing the relative safety of opioids in OA, for both IR and ER formulations. The objective of our study was to assess the safety of opioids in the management of OA in a systematic review and meta-analysis of randomized, placebo-controlled trials.
Methods
The protocol of this systematic review and meta-analysis was previously registered in the PROSPERO database (registration number CRD42017068249). The systematic review was performed in accordance with the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions [20], and the findings are reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21]. The entire review process (study selection and risk of bias assessment) was undertaken using Covidence, the Cochrane platform for systematic reviews, and was performed by EC, NF, SS and LS.
Eligibility Criteria
Randomized, double-blind, placebo-controlled, parallel-group trials that have assessed the AEs associated with oral opioids, i.e. IR (codeine, oxycodone, tramadol, tapentadol IR) and ER (CR codeine, CR oxycodone, CR tramadol, hydrocodone ER, morphine sulfate/sequestered naltrexone, OROS hydromorphone, tapentadol ER, morphine sulfate ER, oxymorphone ER), in comparison with placebo or other oral analgesic comparator drugs (specifically non-steroidal anti-inflammatory drugs [NSAIDs], cyclooxygenase [COX-2] inhibitors, paracetamol, nefopam hydrochloride, tricyclic antidepressants [amitriptyline, nortriptyline], gabapentin, pregabalin and duloxetine) in patients with OA were identified.
Studies that allowed concomitant anti-OA treatments during the trial (other than rescue medication as paracetamol or aspirin) were then excluded, as were animal trials.
Data Sources and Search Strategies
A comprehensive literature search was undertaken in the MEDLINE (via Ovid), Cochrane Central Register of Controlled Trials (Ovid CENTRAL) and Scopus electronic databases. We searched for randomized placebo-controlled trials of opioids in OA, using a combination of study design-, treatment-, and disease-specific keywords and/or Medical Subject Heading (MeSH) terms. The databases were searched from inception to 30 June 2017.
While adverse effects were the outcomes of interest for this study, we decided to avoid the outcome-specific keywords in the search strategies because of the possibility that a study on the efficacy of a drug may have not mentioned terms related to AEs in its title, abstract or in the keywords sections. The search was limited to English and French publications and to human subjects. Detailed search strategies for the MEDLINE/CENTRAL and Scopus databases are reported as electronic supplementary material (ESM) 1.
Two clinical trials registries, ClinicalTrials.gov (clinicaltrials.gov/) and the World Health Organization’s International Clinical Trials Registry Platform Search portal (apps.who.int/trialsearch/) were also checked for trial results that would not have been published. Finally, recent meta-analyses were also screened for any additional relevant studies.
Study Selection
Two members of the review team independently evaluated each title and abstract to exclude only obvious irrelevant studies, according to the predefined eligibility criteria. At this step, the criteria related to adverse effects was not considered for selection as studies focusing on the efficacy of a treatment may not report data about adverse effects in the abstract; this means that all trials mentioning only the efficacy information were retrieved at this step. After this first step, the two investigators independently reviewed each of the full-text of the articles not excluded during the initial screening stage to determine whether the studies met all the selection criteria. At this stage, studies were excluded due to previously unidentified duplication, conference abstracts alone being available, the absence of a placebo arm against opioid medication in the trial, an indication other than OA, safety not being included as an outcome of the trial, a non-opioid intervention, or incorrect study design. All differences of opinion regarding the selection of articles were resolved through discussion and consensus between the two investigators; any persistent disagreement was solved with the intervention of a third person (another member of the review team).
Data Extraction
The full-texts of the selected studies were screened by independent reviewers for extraction of relevant data, using a standard data extraction form. Outcome results data were independently extracted by two investigators of the review team. For each study, the following data were extracted: characteristics of the manuscript, characteristics of the trial, objective and design of the study, characteristics of the patients, characteristics of the disease, characteristics of the treatments, AEs (outcomes) reported during the trial, and the main conclusion of the study. In the case of multiple dosage arms for opioids being included in a trial, the maximum dose was used to categorize the study. If multiple follow-up times were included, the longest follow-up time was used to categorize the study. The raw data (number of events in each group) were extracted for each outcome. The number of patients who experienced any body system-related AE at least once (e.g. nervous system, gastrointestinal [GI] system), as well as AEs within each body system (e.g. headache, abdominal pain) were extracted. As much as possible, data from the intention-to-treat (ITT) analysis were considered.
Outcomes of Interest
The main System Organ Classes (SOCs) that are likely to be affected by the use of opioids in the treatment of OA were explored in this meta-analysis. The primary outcomes of interest were safety and tolerability outcomes, especially those associated with specific bodily systems, i.e. GI disorders, cardiac disorders, vascular disorders, nervous system disorders, skin and subcutaneous tissue disorders, renal and urinary disorders, respiratory, thoracic and mediastinal disorders, along with overall severe and serious AEs. Secondary outcomes were withdrawals due to AEs (i.e. the number of participants who stopped the treatment due to an AE), and the total number of AEs (i.e. the number of patients who experienced any AE at least once).
Assessment of Risk of Bias in the Included Studies
Two authors of the review team independently assessed the risk of bias in each study, using the Cochrane Collaboration’s tool for risk of bias assessment [20]. The following characteristics were evaluated:
Random sequence generation: We assessed whether the allocation sequence was adequately generated.
Allocation concealment: We assessed the method used to conceal the allocation sequence, evaluating whether the intervention allocation could have been foreseen in advance.
Blinding of participants and personnel: We assessed the method used to blind study participants and personnel from knowledge of which intervention a participant received and whether the intended blinding was effective.
Blinding of outcome assessment: We assessed the method used to blind outcome assessors from knowledge of which intervention a participant received and whether the intended blinding was effective.
Incomplete outcome data: We assessed whether participants’ exclusions, attrition and incomplete outcome data were adequately addressed in the paper.
Selective outcomes reporting: We checked whether there was evidence of selective reporting of AEs.
Each of these items was either categorized as either ‘low risk of bias’, ‘high risk of bias’, or ‘unclear risk of bias’. ‘Low risk of bias’ or ‘high risk of bias’ was attributed for an item when there was sufficient information in the manuscript to judge the risk of bias as ‘low’ or ‘high’, otherwise ‘unclear risk of bias’ was attributed to the item. Disagreements were solved by discussion between the two reviewers during a consensus meeting, and involved, when necessary, another member of the review team for final decision.
Data Analysis
Analyses were performed using STATA 14.2 software. The units of analysis were the number of participants experiencing a specific AE. We described harms associated with the treatment as risk ratio with 95% CI, and computed an overall effect size for each primary or secondary outcome (AE). Anticipating substantial variability among trial results (i.e. the interstudy variability), we assumed heterogeneity in the occurrence of the AEs; thus, we planned to use random-effects models for the meta-analyses. We estimated the overall effects and heterogeneity using the DerSimonian and Laird random-effects model [22]. As this method provides biased estimate of the between-study variance with sparse events [23, 24], we also performed the meta-analyses using the restricted maximum likelihood (REML) method [25].
We tested heterogeneity using the Cochran’s Q test. As we were performing a random-effect meta-analysis, we used the Tau-squared (Tau2) estimate as the measure of the between-study variance. The I-squared (I2) statistic was used to quantify heterogeneity, measuring the percentage of total variation across studies due to heterogeneity [26]. In the case of substantial heterogeneity, we aimed to undertake subgroup analyses, stratifying the analyses according to participants’ age in the intervention group, duration of the OA complaint, location of OA (knee, hand, hip), number of joints involved, drug dose, duration of the treatment, combination of the opioid analgesic with other analgesics, analgesic potency of the opioid (stronger vs. weaker); pharmacologic activity of the opioid analgesic (opioid receptors agonist only vs. opioid receptor agonists with other pharmacologic activity); and risk of bias in the study (e.g. studies with a low risk of bias versus all other studies). The quality of each evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach [27], and a table summarising the findings was prepared using the GRADEpro online software [28].
Results
Study Selection
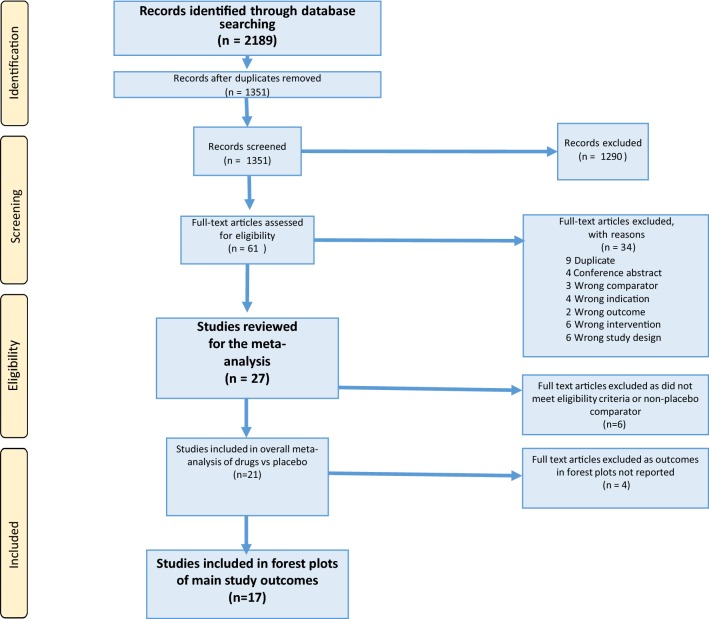
Database searches initially identified 2189 records. After exclusions, 61 articles were screened in full against the inclusion criteria. A flowchart (Fig. 1) with the number of studies at each step was established, including the reasons for excluding studies during the full-text reading process. Twenty-seven of these studies met the eligibility criteria, of which a further six were excluded as the trial lacked a placebo arm, and four were excluded as the reported outcomes were not relevant to the meta-analysis. Finally, 17 papers were included in the analysis of main study outcomes [29–45].
Fig. 1.
Study selection process
Study Characteristics
Table 1 presents the characteristics of the studies included through the systematic review process. The year of publication of the included studies ranged from 1998 to 2015, and the follow-up time ranged from 10 days to 16 weeks. Twelve studies included ER or CR formulations of opioids, and five studies included IR opioids. The number of trials including an arm for each specific opioid (or two arms if two opioids were included) were as follows: tramadol, 8; oxycodone, 6; tapentadol, 2; hydromorphone, 2; and hydrocodone, 1 trial. Furthermore, the anatomical regions included per trial were as follows: knee, 15; hip, 10; spine, 1; any location, 2; low back pain, 1; or awaiting joint replacement, two trials.
Table 1.
Characteristics of the studies included through the systematic review process
| Study, year | Location of OA | Age of participants by study group, years (mean ± SD or median [P25–P75]) | Active treatment | Dose | Trial duration | Data provided in the article (type of AE) |
|---|---|---|---|---|---|---|
| Afilalo et al., 2010 [29] | Knee | Placebo 58.2 (9.15)/active 58.4 (10.09) | Tapentadol ER | 100–250 mg od | 12 weeks | TEAEs reported, covering some SOCs (headache, GI disorders overall, pruritis, vomiting, somnolence, fatigue, nervous system disorders, constipation, diarrhoea, dry mouth, dizziness, nausea) |
| Afilalo et al., 2010 [29] | Knee | Placebo 58.2 (9.15)/active 58.2 (10.29) | CR oxycodone | 20–50 mg od | 12 weeks | TEAEs reported, covering some SOCs (nervous system disorders, diarrhoea, headache, nausea, GI disorders overall, constipation, somnolence, fatigue, dizziness, dry mouth, vomiting, pruritis) |
| Burch et al., 2007 [30] | Knee | Placebo 62 (9)/active 62 (9) | CR tramadol | 200–300 mg od | 12 weeks | AEs and TEAEs reported, covering some SOCs (overall discontinuation, somnolence, constipation, overall adverse event, nausea, dizziness/vertigo) |
| DeLemos et al., 2011 [31] | Hip/knee | Placebo 58.9 (11.6)/active 59.5 (10.2)—tramadol 100 mg od Placebo 58.9 (11.6)/active 62.0 (9.9)—tramadol 200 mg od Placebo 58.9 (11.6)/active 59.7 (11.4)—tramadol 300 mg od |
CR tramadol | 100 mg od 200 mg od 300 mg od | 12 weeks | AEs and TEAEs covering some SOCs, plus discontinuations reported (at least one AE occurred; nervousness, flushing, diarrhoea, fatigue, vomiting, dizziness, headache, anorexia, constipation, nausea, somnolence, dry mouth, upper respiratory tract infection, insomnia, pruritus) |
| Fishman et al., 2007 [32] | Knee | Placebo 61 (10)/active 63 (8)—tramadol 100 mg od Placebo 61 (10)/active 61 (9)—tramadol 200 mg od Placebo 61 (10)/60 (9)—tramadol 300 mg od |
CR tramadol | 100 mg od 200 mg od 300 mg od | 12 weeks | TEAEs reported, including deaths and discontinuations of treatment (constipation, insomnia, somnolence, small bowel obstruction, gastritis, discontinuation due to AE, dry mouth, vomiting, dizziness/vertigo, nausea, sweating, pruritis, lower abdominal pain, headache, death from myocardial infarction) |
| Fleischmann et al., 2001 [33] | Knee | Placebo 62.45 (9.62)/active 62.52 (8.68) | Tramadol | 200–400 mg od | 91 days | TEAEs not by SOC and discontinuations reported (pruritus, nausea, constipation, dizziness, headache) |
| Friedmann et al., 2011 [34] | Hip and/or knee | Placebo 58.5 (8.44)/active 58.0 (7.86) | Oxycodone | 20 mg bid | 12 weeks | TEAEs not by SOC and discontinuations reported (SAE, dizziness, pruritus, dry mouth, somnolence, vomiting, headache, fecaloma, orthostatic hypotension, nausea) |
| Gana et al., 2006 [35] | Hip/knee | Placebo 56.4 (9.8)/active 58.4 (10.9)—tramadol 100 mg od Placebo 56.4 (9.8)/active 59.1 (9.9)—tramadol 200 mg od Placebo 56.4 (9.8)/active 58.5 (9.4)—tramadol 300 mg od Placebo 56.4 (9.8)/active 58.4 (9.7)—tramadol 400 mg od |
Tramadol | 100 mg od 200 mg od 300 mg od 400 mg od | 12 weeks | TEAEs not by SOC and discontinuations due to AEs reported (postural hypotension, sweating increase, anorexia, flushing, dizziness, insomnia, diarrhoea, somnolence, dry mouth, pain, nausea, vomiting, fatigue, headache, pruritus, constipation) |
| Hale et al., 2015 [36] | Any site or low back pain | Placebo 52.7 (12.1)/active 53.6 (10.4) | Hydrocodone ER | 15–90 mg bid | 12 weeks | TEAEs not by SOC, SAEs and discontinuations due to AEs reported (dry mouth, constipation, upper respiratory tract infection, nausea, pruritus, somnolence, headache, back pain, dizziness, vomiting, pancreatitis, fatigue) |
| Hartrick et al., 2009 [37] | Awaiting joint replacement | Placebo 62.0 (20–79)/active 62.0 (41–79) | CR oxycodone | 10 mg, 4–6 hourly | 10 days | TEAEs not by SOC and discontinuations due to AEs reported (fatigue, diarrhoea, somnolence, vomiting, nausea, headache, dizziness, pruritus, constipation) |
| Hartrick et al., 2009 [37] | Awaiting joint replacement | Placebo 62.0 (20–79)/active 60.0 (31–79)—tapentadol ER 50 mg Placebo 62.0 (20–79)/active 61.5 (34–78)—tapentadol ER 75 mg |
Tapentadol ER | 50 mg, 4–6 hourly 75 mg, 4–6 hourly |
10 days | TEAEs not by SOC and discontinuations due to AEs reported (fatigue, dizziness, headache, nausea, vomiting, pruritus, diarrhoea, constipation, somnolence) |
| Malonne et al., 2004 [38] | Hip/knee | Placebo 66.4 (9.2)/active 67.1 (7.1) | CR tramadol | 200 mg od | 2 weeks | TEAEs not by SOC and discontinuations due to AEs reported (diarrhoea, somnolence, vomiting, drunken feeling, increased sweating, nausea, asthenia, malaise, constipation, headache, heartburn, epigastric pain, dizziness) |
| Markenson et al., 2005 [39] | Any site | Placebo [mean (range)] 64 (41–89)/active [mean (range)] 62 (38–88) | CR oxycodone | 10–60 mg bid | 90 days | TEAEs not by SOC and discontinuations due to AEs reported (dizziness, diarrhoea, somnolence, constipation, vomiting, increased sweating, nausea, pruritus, headache) |
| Matsumoto et al., 2005 [40] | Hip/knee | Placebo 61.7 (1.0)/active 62.7 (1.0)—CR oxycodone 20 mg bid Placebo 61.7 (1.0)/active 61.4 (1.0)—CR oxycodone 40 mg bid |
CR oxycodone | 20 mg bid 40 mg bid | 4 weeks | TEAEs not by SOC and discontinuations due to AEs reported (dizziness, pruritus, constipation, headache, dry mouth, nausea, somnolence, vomiting) |
| Rauck et al., 2013 [41] | Knee/hip | Placebo 60.0 (11.2)/active 59.7 (10.6)—hydromorphone 8 mg od Placebo 60.0 (11.2)/active 59.5 (10.7)—hydromorphone 16 mg od |
OROS hydromorphone | 8 mg od 16 mg od |
12 weeks | TEAEs not by SOC and discontinuations due to AEs reported (headache, nausea, vomiting, constipation, somnolence, pruritus, dizziness) |
| Roth, 1998 [42] | Hip/knee/spine | Placebo 67.0/active 65.9 | Tramadol | 50–400 mg od | 13 days | TEAEs not by SOC and discontinuations due to AEs reported (dizziness, headache, insomnia, constipation, cold sweats, itching, diaphoresis, vomiting, lightheadedness, dry mouth, nausea, drowsiness, sedation) |
| Spierings et al., 2013 [43] | Hip/knee | Placebo 57.2 (28–75)/active 57.6 (33–75) | Oxycodone | 10–40 mg bid | 16 weeks | TEAEs not by SOC and discontinuations due to AEs reported (somnolence, nasopharyngitis, peripheral burning sensation, hypoesthesia, dysesthesia, hyperesthesia, paresthesia, vomiting, headache, fatigue, hypertension, pruritus, dizziness, arthralgia, constipation, nausea, peripheral neuropathy, decreased vibratory sense) |
| Vojtassak et al., 2011 [44] | Hip/knee | Placebo 66.0 (40–87)/active 65.0 (43–85) | OROS hydromorphone | 4–32 mg od | 12 weeks | TEAEs not by SOC, SAEs and discontinuations due to AEs reported (constipation, nausea and vomiting) |
| Vorsanger et al., 2007 [45] | Hip/knee | Placebo 68.6 (2.4)/active 69.4 (3.0)—CR tramadol 100 mg od Placebo 68.6 (2.4)/active 69.2 (2.6)—CR tramadol 200 mg od Placebo 68.6 (2.4)/active 68.9 (2.7)—CR tramadol 300 mg od Placebo 68.6 (2.4)/active 69.1 (2.8)—CR tramadol 400 mg od |
CR tramadol | 100 mg od 200 mg od 300 mg od 400 mg od | 12 weeks | TEAEs not by SOC and discontinuations due to AEs reported (vomiting, nausea, dry mouth, back pain, postural hypotension, abnormal dreams, dizziness, fatigue, pain in the limb, pruritus, flushing, insomnia, sweating increased, constipation, weight decreased, dyspepsia, weakness, arthralgia, appetite decreased, nasopharyngitis, somnolence, nervousness, headache, pain, anorexia) |
AE adverse event, bid twice daily, CR controlled-release, ER extended-release, GI gastrointestinal, OA osteoarthritis, od once daily, OROS osmotic controlled-release oral delivery system, SAE serious adverse event, SD standard deviation, SOC System Organ Class, TEAEs treatment-emergent adverse events
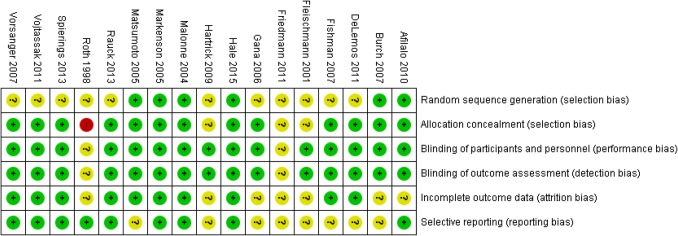
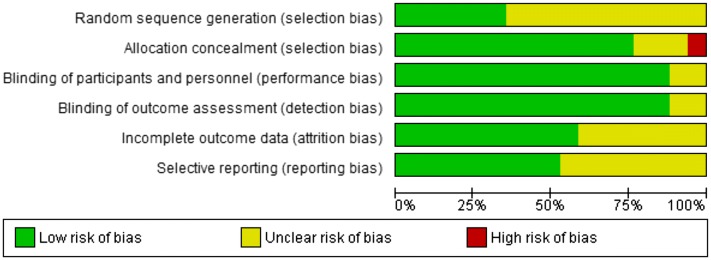
Risk of Bias of Individual Studies
Figures 2 and 3 include a summary of the risk of bias assessed for each study included in the meta-analysis. The majority of our findings were associated with a ‘moderate’ to ‘high’ certainty of evidence, with the exception of total AEs (‘low’ certainty of evidence). Forest plots for analyses are reported in ESM 2.
Fig. 2.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
Fig. 3.
Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies
Primary Outcomes
We reported only the results from the DerSimonian and Laird random-effects model because we found no difference in the effects computed by the two methods.
Too few studies reported data on severe or serious AEs (two studies of IR, two studies of ER) or drug-related AEs (one study of IR and no studies of ER) for opioids versus placebo, and thus the RR could not be calculated in this meta-analysis. The primary outcomes for SOC-related AEs are reported separately for IR and ER opioid formulations.
Immediate-Release Opioids
The RR of lower GI AEs (constipation or fecaloma) was significantly increased fivefold with IR opioids versus placebo (RR 5.20, 95% CI 3.42–7.89; I2 = 0%) [ESM 2]. The combined RR of nausea, vomiting or loss of appetite was significantly increased with IR opioids vs. placebo (RR 3.39, 95% CI 2.22–5.18; I2 = 37.1%), and the risk of dry mouth or oral ulceration was also increased with IR opioids (RR 4.43, 95% CI 0.92–21.24; I2 = 47.5%), although this did not reach statistical significance. The RR of upper GI complications with IR opioids could not be calculated as there insufficient data were reported in RCTs versus placebo.
The risk of AEs of the central nervous system (CNS), including dizziness, headache and other ‘consciousness-related’ AEs (including insomnia, drowsiness, sedation and fatigue) was significantly increased with IR opioids compared with placebo (RR 2.76, 95% CI 1.90–4.02; I2 = 45.5%).
A significantly increased risk of dermatological AEs (rash and pruritus) was measured with IR opioids versus placebo (RR 3.60, 95% CI 1.74–7.43; I2 = 37.8%).
Extended-Release Opioids
The RR of lower GI AEs (constipation) was significantly increased with ER opioids versus placebo (RR 4.22, 95% CI 3.44–5.17; I2 = 24.5%) [ESM 2], and the combined RR of nausea, vomiting or loss of appetite was significantly increased with ER opioids vs. placebo (RR 4.03, 95% CI 3.37–4.83; I2 = 33.4%). The risk of dry mouth or oral ulceration was also significantly increased with ER opioids vs. placebo (RR 3.00, 95% CI 1.85–4.86; I2 = 8.1%), and the RR of upper GI AEs (dyspepsia, gastritis, heartburn) was increased with ER opioids versus placebo (RR 4.03, 95% CI 0.87–18.62; I2 = 0%), although this did not reach statistical significance.
The risk of AEs of the CNS was significantly increased with ER opioids compared with placebo (RR 2.76, 95% CI 2.19–3.47; I2 = 72.9%). The RR of specific CNS AEs was as follows: headache (RR 0.98, 95% CI 0.83–1.16; I2 = 0%); dizziness (RR 3.63, 95% CI 2.98–4.41; I2 = 0%); and other (fatigue, somnolence, insomnia, weakness, nervousness) [RR 3.63, 95% CI 2.90–4.53; I2 = 14.9%].
A significantly increased risk of dermatological AEs (rash and pruritus) was measured with ER opioids versus placebo (RR 7.87, 95% CI 5.20–11.89; I2 = 0%).
Secondary Outcomes
For total AEs, a significant increased risk of AEs was found with ER opioids compared with placebo (RR 1.70, 95% CI 1.37–2.12; I2 = 79.6%) [ESM 2]. Insufficient data were collected on total AEs with IR opioid formulations versus placebo to allow comparison in this meta-analysis.
Heterogeneity in the reporting of withdrawal rates due to AEs between trials, with some articles reporting ‘discontinuations’, ‘withdrawn from study’ and an insufficient number providing a clear indication of withdrawals due to AEs meant that there were insufficient data to include the withdrawal rate in the meta-analysis.
GRADE Assessment of Findings
We assessed the certainty of evidence for each primary or secondary outcome for opioids compared with placebo, using the GRADE approach [27]. Our findings were largely associated with ‘moderate’ to ‘high’ certainty of evidence, with the exception of total AEs with ER opioids, for which there was low certainty of evidence. Additionally, for many outcomes, there were too few or no studies reporting on these outcomes for the GRADE analysis to be performed. Tables 2 and 3 summarize the findings for IR and ER opioids for all outcomes assessed in this meta-analysis.
Table 2.
Summary of safety indings for immediate-release opioids versus placebo in patients with osteoarthritis
| Outcomes† | No. of participants Follow-up |
Certainty of the evidence (GRADE) | Relative effect (95% CI) Risk ratio | Anticipated absolute effects | |
|---|---|---|---|---|---|
| Risk with placebo | Risk difference with Immediate release opioids | ||||
| Lower gastrointestinalal AEs | 1700 | ⊕⊕⊕⊕ HIGH |
5.20 (3.42 to 7.89) |
27 per 1000 | 114 more per 1000 (66 more to 187 more) |
| Nausea, vomiting, loss of appetite | 2447 | ⊕⊕⊕⊕ HIGH |
3.39 (2.22 to 5.18) |
45 per 1000 | 108 more per 1000 (55 more to 189 more) |
| Dry mouth or oral ulceration | 860 | ⊕⊕⊕◯ MODERATEa |
4.43 (0.92 to 21.24) |
9 per 1000 | 32 more per 1000 (1 fewer to 187 more) |
| Central nervous system AEs | 5012 | ⊕⊕⊕⊕ HIGH |
2.76 (1.90 to 4.02) |
36 per 1000 | 64 more per 1000 (33 more to 109 more) |
| Rash or pruritus | 1695 | ⊕⊕⊕⊕ HIGH |
3.60 (1.74 to 7.43) |
25 per 1000 | 65 more per 1000 (18 more to 160 more) |
GRADE Working Group grades of evidence: High certainty We are very confident that the true effect lies close to that of the estimate of the effect; Moderate certainty We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; Low certainty Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect; Very low certainty We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect
The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI)
AEs adverse events, CI confidence interval, GRADE Grading of Recommendations Assessment, Development and Evaluation
aThe outcomes total AEs, serious AEs, treatment-emergent AEs, upper gastrointestinal, cardiovascular or cerebrovascular, renal and hepatic, and death were reported in either no or too few studies to analyse
bLarge CI
Table 3.
Summary of safety indings for extended-release opioids versus placebo in patients with osteoarthritis
| Outcomes† | No. of participants Follow-up |
Certainty of the evidence (GRADE) | Relative effect (95% CI) Risk Ratio | Anticipated absolute effects | |
|---|---|---|---|---|---|
| Risk with placebo | Risk difference with Extended release opioids | ||||
| Total AEs | 1915 | ⊕⊕◯◯ LOWa |
1.70 (1.37 to 2.12) |
361 per 1000 | 252 more per 1000 (133 more to 404 more) |
| Upper GI AEs | 1119 | ⊕⊕⊕◯ MODERATEb |
4.03 (0.87 to 18.62) |
0 per 1000 | 0 fewer per 1000 (0 fewer to 0 fewer) |
| Lower GI AEs | 6472 | ⊕⊕⊕⊕ HIGH |
4.22 (3.44 to 5.17) |
52 per 1000 | 186 more per 1000 (134 more to 254 more) |
| Nausea, vomiting, loss of appetite | 10,920 | ⊕⊕⊕⊕ HIGH |
4.03 (3.37 to 4.83) |
46 per 1000 | 141 more per 1000 (110 more to 178 more) |
| Dry mouth or oral ulceration | 2956 | ⊕⊕⊕⊕ HIGH |
3.00 (1.85 to 4.86) |
18 per 1000 | 35 more per 1000 (15 more to 68 more) |
| Central nervous system AEs | 20,266 | ⊕⊕⊕◯ MODERATEc |
2.76 (2.19 to 3.47) |
51 per 1000 | 90 more per 1000 (61 more to 126 more) |
| Rash or pruritus | 4403 | ⊕⊕⊕⊕ HIGH |
7.87 (5.20 to 11.89) |
11 per 1000 | 77 more per 1000 (47 more to 122 more) |
GRADE Working Group grades of evidence: High certainty We are very confident that the true effect lies close to that of the estimate of the effect; Moderate certainty We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; Low certainty Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect; Very low certainty We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect
The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI)
AEs adverse events, CI confidence interval, GI gastrointestinal, GRADE Grading of Recommendations Assessment, Development and Evaluation
aThe outcomes serious AEs, treatment-emergent AEs, cardiovascular or cerebrovascular, renal and hepatic, and death were reported in either no or too few studies to analyse
bI2 > 75% (p < 0.001)
cLarge CI
dI2 between 50 and 75% (p < 0.001)
Discussion
Overall, our meta-analysis found a significantly increased risk of lower GI, nausea/vomiting/loss of appetite, CNS and rash/pruritus in both IR and ER opioids compared with placebo. In addition, we found a significantly increased risk of dry mouth/oral ulceration, and total AEs with ER formulations of opioids compared with placebo. This level of risk is comparable to the findings of a Cochrane meta-analysis of oral and transdermal (non-tramadol) opioids for OA of the knee or hip (da Costa et al. [7] and a recent systematic review and meta-analysis of older people [aged ≥ 60 years] with musculoskeletal pain by Megale et al. [17]). These results may reflect physiological changes in pain processing, pharmacokinetics, and pharmacodynamics in the aging population.
Insufficient data were reported on total AEs and upper GI complications with IR formulations of opioids versus placebo to allow inclusion of a comparison in our meta-analysis. Controlled-, sustained-, and extended-release formulations are designed to avoid the peaks (and troughs) of plasma drug concentrations that are associated with the tolerability issues of IR formulations. A fivefold increased risk of lower GI AEs (constipation), threefold combined increase in nausea, vomiting and loss of appetite, and threefold increase in dermatological AEs was measured with IR opioids compared with placebo.
Our analysis demonstrates that ER opioid formulations are nonetheless associated with a higher rate of AEs compared with placebo: fourfold increase in lower GI AEs, fourfold increase in nausea, vomiting and loss of appetite, threefold increase in dry mouth or ulceration, and sevenfold increase in dermatological AEs (rash or pruritis). A significantly increased risk of CNS AEs occurred with both IR and ER opioids (RR 2.76 for each group), largely relating to sedation, drowsiness, fatigue, dizziness and headache.
Tramadol is a centrally-acting weak opioid analgesic with a dual mode of action as an agonist of the μ-opioid receptor and as a noradrenaline reuptake inhibitor, which rarely causes the AEs of respiratory depression and physical dependence commonly associated with conventional opioid drugs [46]. A review of tramadol found a small but statistically significant benefit for tramadol over placebo in OA (number needed to treat to benefit [NNTB] = 6, 95% CI 4–9); however, the high level of reversible and non-life-threatening AEs reported (number needed to treat to harm [NNTH] = 8, 95% CI 7–12) often caused the participant to withdraw (12.5% of patients taking tramadol), which could limit its usefulness in clinical practice [15]. Our analysis included tramadol in both IR and CR formulations. As an IR formulation, tramadol was associated with GI adverse effects (constipation, nausea, vomiting), CNS AEs (dizziness, headache, fatigue, insomnia, somnolence) and dermatological AEs (itching and pruritus). The CR formulation of tramadol (200–400 mg) was a major contributor to the significantly higher rate of AEs observed with all ER formulations (hydromorphone, oxycodone) included in our study compared with placebo (RR 1.70, 95% CI 1.37–2.12). There is some evidence to suggest that the rate of AEs with tramadol can be minimized with slow upward titration of an ER formulation, to improve tolerability and thus avoid premature treatment discontinuations [47].
Like tramadol, tapentadol has a dual mechanism of action, but unlike tramadol, it has only weak effects on the reuptake of serotonin and is a significantly more potent opioid with no known active metabolites [48, 49]. Tapentadol ER (75 mg 4–6 hourly and 100–250 mg/day) in two studies included in our meta-analysis was also associated with a higher risk of AEs, including GI disorders (constipation, nausea, vomiting, dry mouth, oral ulceration), CNS disorders (dizziness, somnolence, fatigue) and dermatological AEs (rash and pruritus) compared with placebo. In an analysis of four studies of tapentadol ER versus placebo or oxycodone in patients with OA or back pain, tapentadol ER was associated with a 2.7-fold increase in risk of discontinuation due to AEs compared with placebo, but with a 50% reduction in risk of discontinuation due to AEs compared with oxycodone [19].
Limitations
Around half of the studies identified that met the inclusion criteria did not provide AE data suitable for inclusion in the meta-analysis. Many studies lacked detail on AE reporting and there was variation between studies regarding nomenclature and grouping of AEs e.g. ‘common adverse events’, or ‘those experienced in > 5%’. These different names and groupings of AEs may lead to lack of resolution and possible double counting. In combining different drugs and doses into one meta-analysis, we have chosen the highest dose when multiple doses were presented in a trial, e.g. ‘tramadol ER 100/200/300/400 mg’, which could lead to an exaggeration of AEs. Sensitivity analysis of the two approaches (highest dose, versus multiple dose) revealed only marginal differences in the magnitude of the outcome. Included studies were of short duration, i.e. only 2–18 weeks. Our analysis was limited to studies in OA patients, thus safety issues could be missed in relevant subgroups, e.g. other musculoskeletal pain, back pain. Our meta-analysis did not examine IR formulations against ER formulations, however this could be a potential avenue for future research.
Conclusions
In our meta-analysis, oral opioids were associated with an increased risk of GI, CNS and dermatological AEs compared with placebo, for both the IR and ER formulations. The frequent occurrence of adverse effects limits the use of opioids due to poor tolerability and high rates of treatment withdrawal. To maximize the risk: benefit ratio of opioids, the ESCEO recommends that opioids should only be used as a step 3 treatment for severely symptomatic OA patients, preferably as short-term treatment with a weak opioid [11]. Our results confirm that there are considerable safety and tolerability issues surrounding the use of opioids in OA, and support the recommendation of international and national guidelines to reserve the use of opioids in OA as the last resort pharmacologic therapy before surgery [10–13].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This paper was written on behalf of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) Working Group on the safety of anti-OA medications: Nasser Al-Daghri, Nigel Arden, Bernard Avouac, Olivier Bruyère, Roland Chapurlat, Philip Conaghan, Cyrus Cooper, Elizabeth Curtis, Elaine Dennison, Nicholas Fuggle, Gabriel Herrero-Beaumont, Germain Honvo, Margreet Kloppenburg, Stefania Maggi, Tim McAlindon, Alberto Migliore, Ouafa Mkinsi, François Rannou, Jean-Yves Reginster, René Rizzoli, Roland Roth, Thierry Thomas, Daniel Uebelhart, and Nicola Veronese. Philip G. Conaghan is supported in part by the UK National Institute for Health Research (NIHR) Leeds Biomedical Research Centre. The views expressed in this publication are those of the author(s) and not necessarily those of the National Health Service, the NIHR or the Department of Health. The authors would like to express their most sincere gratitude to Dr Lisa Buttle for her invaluable help with the manuscript preparation. Dr Lisa Buttle was entirely funded by the ESCEO asbl, Belgium.
Role of the funding source
The Working Group was entirely funded by the ESCEO, a Belgian not-for-profit organization that receives unrestricted educational grants, to support its educational and scientific activities, from non-governmental organizations, not-for-profit organizations, and non-commercial and corporate partners. The choice of topics, participants, content and agenda of the working groups, as well as the writing, editing, submission and reviewing of the manuscript, are under the sole responsibility of the ESCEO, without any influence from third parties.
Conflicts of interest
Olivier Bruyère reports grants from Biophytis, IBSA, MEDA, Servier, SMB and Theramex, outside of the submitted work. Cyrus Cooper reports personal fees from Alliance for Better Bone Health, Amgen, Eli Lilly, GlaxoSmithKline, Medtronic, Merck, Novartis, Pfizer, Roche, Servier, Takeda and UCB, outside of the submitted work. Jean-Yves Reginster reports grants from IBSA-Genevrier, Mylan, CNIEL and Radius Health (through institution); consulting fees from IBSA-Genevrier, Mylan, CNIEL, Radius Health and Pierre Fabre; fees for participation in review activities from IBSA-Genevrier, MYLAN, CNIEL, Radius Health and Teva; and payment for lectures from AgNovos, CERIN, CNIEL, Dairy Research Council (DRC), Echolight, IBSA-Genevrier, Mylan, Pfizer Consumer Health, Teva and Theramex, outside of the submitted work. Elizabeth Curtis reports lecture fees and travel support from Eli Lilly, Pfizer and UCB, outside of the submitted work. Nicholas Fuggle reports travel support from Eli Lilly and Pfizer, outside of the submitted work. Elaine Dennison reports personal fees for lectures or advisory boards from UCB and Pfizer, outside of the submitted work. Nadia Corp reports partial funding of employment at Keele University from Versus Arthritis (registered charity), as well as travel support from Versus Arthritis, outside of the submitted work. Philip G. Conaghan reports consultancy fees or speakers’ bureau fees from Abbvie, BMS, Flexion Therapeutics, GlaxoSmithKline, Merck Serono, Novartis, Pfizer, Roche and Samumed, outside of the submitted work. Germain Honvo, Daniel Uebelhart, Sarah Shaw, Laura Spooner, Georgia Ntani, Camille Parsons and Janis Baird have no discloses to report.
Contributor Information
Nicholas Fuggle, Email: nrf@mrc.soton.ac.uk.
Elizabeth Curtis, Email: bc@mrc.soton.ac.uk.
Sarah Shaw, Email: ss@mrc.soton.ac.uk.
Laura Spooner, Email: laura.j.spooner@gmail.com.
Olivier Bruyère, Email: olivier.bruyere@uliege.be.
Georgia Ntani, Email: gn@mrc.soton.ac.uk.
Camille Parsons, Email: cp@mrc.soton.ac.uk.
Philip G. Conaghan, Email: p.conaghan@leeds.ac.uk
Nadia Corp, Email: n.corp@keele.ac.uk.
Germain Honvo, Email: germain.honvo@uliege.be.
Daniel Uebelhart, Email: Daniel.Uebelhart@hopitalvs.ch.
Janis Baird, Email: jb@mrc.soton.ac.uk.
Elaine Dennison, Email: emd@mrc.soton.ac.uk.
Jean-Yves Reginster, Email: jyreginster@uliege.be.
Cyrus Cooper, Phone: 02380777624, Email: cc@mrc.soton.ac.uk.
References
- 1.Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartil. 2011;19(11):1270–1285. doi: 10.1016/j.joca.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lane NE, Brandt K, Hawker G, Peeva E, Schreyer E, Tsuji W, et al. OARSI-FDA initiative: defining the disease state of osteoarthritis. Osteoarthritis Cartil. 2011;19(5):478–482. doi: 10.1016/j.joca.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Stein C, Pfluger M, Yassouridis A, Hoelzl J, Lehrberger K, Welte C, et al. No tolerance to peripheral morphine analgesia in presence of opioid expression in inflamed synovia. J Clin Invest. 1996;98(3):793–799. doi: 10.1172/JCI118852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thorlund JB, Turkiewicz A, Prieto-Alhambra D, Englund M. Opioid use in knee or hip osteoarthritis: a region-wide population-based cohort study. Osteoarthritis Cartilage. Epub 22 Jan 2019. 10.1016/j.joca.2019.01.005. [DOI] [PubMed]
- 6.Desai RJ, Jin Y, Franklin PD, Lee YC, Bateman BT, Lii J et al. Association of geography and access to healthcare providers with long term prescription opioid use in Medicare patients with severe osteoarthritis: A cohort study. Arthritis Rheumatol. Epub 28 Jan 2019. 10.1002/art.40834. [DOI] [PMC free article] [PubMed]
- 7.da Costa BR, Nuesch E, Kasteler R, Husni E, Welch V, Rutjes AW et al. Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Database Syst Rev. 2014;9:CD003115. [DOI] [PMC free article] [PubMed]
- 8.Avouac J, Gossec L, Dougados M. Efficacy and safety of opioids for osteoarthritis: a meta-analysis of randomized controlled trials. Osteoarthritis Cartil. 2007;15(8):957–965. doi: 10.1016/j.joca.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112(3):372–380. doi: 10.1016/j.pain.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 10.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartil. 2014;22(3):363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Bruyere O, Cooper C, Pelletier JP, Branco J, Brandi ML, Guillemin F, et al. An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally: a report from a task force of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) Semin Arthritis Rheum. 2014;44(3):253–263. doi: 10.1016/j.semarthrit.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Bruyere O, Cooper C, Pelletier J-P, Maheu E, Rannou F, Branco J, et al. A consensus statement on the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) algorithm for the management of knee osteoarthritis—from evidence-based medicine to the real-life setting. Semin Arthritis Rheum. 2016;45(Suppl 4S):S3–S11. doi: 10.1016/j.semarthrit.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64(4):465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 14.Nuesch E, Rutjes AW, Husni E, Welch V, Juni P. Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Database Syst Rev. 2009;4:CD003115. [DOI] [PubMed]
- 15.Cepeda MS, Camargo F, Zea C, Valencia L. Tramadol for osteoarthritis. Cochrane Database Syst Rev. 2006;3:CD005522. [DOI] [PubMed]
- 16.Gehling M, Hermann B, Tryba M. Meta-analysis of dropout rates in randomized controlled clinical trials: opioid analgesia for osteoarthritis pain. Schmerz. 2011;25(3):296–305. doi: 10.1007/s00482-011-1057-9. [DOI] [PubMed] [Google Scholar]
- 17.Megale RZ, Deveza LA, Blyth FM, Naganathan V, Ferreira PH, McLachlan AJ, et al. Efficacy and safety of oral and transdermal opioid analgesics for musculoskeletal pain in older adults: a systematic review of randomized. Placebo-controlled trials. J Pain. 2018;19(5):475.e1–475.e24. doi: 10.1016/j.jpain.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Cnota PJ, Nowak H, Tagarro I, Erb K, Schurer M, Schulz HU, et al. Tramadol SR formulations: pharmacokinetic comparison of a multiple-units dose (capsule) versus a single-unit dose (tablet) Clin Drug Investig. 2005;25(7):435–443. doi: 10.2165/00044011-200525070-00002. [DOI] [PubMed] [Google Scholar]
- 19.Santos J, Alarcao J, Fareleira F, Vaz-Carneiro A, Costa J. Tapentadol for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2015;5:CD009923. [DOI] [PMC free article] [PubMed]
- 20.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration; 2011. http://www.handbook.cochrane.org. Accessed 12 Feb 2019.
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12. [DOI] [PubMed]
- 22.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.Bradburn MJ, Deeks JJ, Berlin JA, Russell Localio A. Much ado about nothing: a comparison of the performance of meta-analytical methods with rare events. Stat Med. 2007;26(1):53–77. doi: 10.1002/sim.2528. [DOI] [PubMed] [Google Scholar]
- 24.Stijnen T, Hamza TH, Ozdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med. 2010;29(29):3046–3067. doi: 10.1002/sim.4040. [DOI] [PubMed] [Google Scholar]
- 25.Normand SL. Meta-analysis: formulating, evaluating, combining, and reporting. Stat Med. 1999;18(3):321–359. doi: 10.1002/(SICI)1097-0258(19990215)18:3<321::AID-SIM28>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94. [DOI] [PubMed]
- 28.GRADEpro GDT: GRADEpro Guideline Development Tool [software]. McMaster University, 2015 (developed by Evidence Prime, Inc.). https://gradepro.org (Evidence Prime, Inc.). Accessed 12 Feb 2019.
- 29.Afilalo M, Etropolski MS, Kuperwasser B, Kelly K, Okamoto A, Van Hove I, et al. Efficacy and safety of Tapentadol extended release compared with oxycodone controlled release for the management of moderate to severe chronic pain related to osteoarthritis of the knee: a randomized, double-blind, placebo- and active-controlled phase III study. Clin Drug Investig. 2010;30(8):489–505. doi: 10.2165/11533440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 30.Burch F, Fishman R, Messina N, Corser B, Radulescu F, Sarbu A, et al. A comparison of the analgesic efficacy of Tramadol Contramid OAD versus placebo in patients with pain due to osteoarthritis. J Pain Symptom Manage. 2007;34(3):328–338. doi: 10.1016/j.jpainsymman.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 31.DeLemos BP, Xiang J, Benson C, Gana TJ, Pascual ML, Rosanna R, et al. Tramadol hydrochloride extended-release once-daily in the treatment of osteoarthritis of the knee and/or hip: a double-blind, randomized, dose-ranging trial. Am J Ther. 2011;18(3):216–226. doi: 10.1097/MJT.0b013e3181cec307. [DOI] [PubMed] [Google Scholar]
- 32.Fishman RL, Kistler CJ, Ellerbusch MT, Aparicio RT, Swami SS, Shirley ME, et al. Efficacy and safety of 12 weeks of osteoarthritic pain therapy with once-daily tramadol (Tramadol Contramid OAD) J Opioid Manag. 2007;3(5):273–280. doi: 10.5055/jom.2007.0015. [DOI] [PubMed] [Google Scholar]
- 33.Fleischmann RM, Caldwell JR, Roth SH, Tesser JRP, Olson W, Kamin M. Tramadol for the treatment of joint pain associated with osteoarthritis: a randomized, double-blind, placebo-controlled trial. Curr Ther Res. 2001;62:113–128. doi: 10.1016/S0011-393X(01)80021-7. [DOI] [Google Scholar]
- 34.Friedmann N, Klutzaritz V, Webster L. Efficacy and safety of an extended-release oxycodone (Remoxy) formulation in patients with moderate to severe osteoarthritic pain. J Opioid Manag. 2011;7(3):193–202. doi: 10.5055/jom.2011.0062. [DOI] [PubMed] [Google Scholar]
- 35.Gana TJ, Pascual ML, Fleming RR, Schein JR, Janagap CC, Xiang J, et al. Extended-release tramadol in the treatment of osteoarthritis: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Curr Med Res Opin. 2006;22(7):1391–1401. doi: 10.1185/030079906X115595. [DOI] [PubMed] [Google Scholar]
- 36.Hale ME, Laudadio C, Yang R, Narayana A, Malamut R. Efficacy and tolerability of a hydrocodone extended-release tablet formulated with abuse-deterrence technology for the treatment of moderate-to-severe chronic pain in patients with osteoarthritis or low back pain. J Pain Res. 2015;8:623–636. doi: 10.2147/JPR.S83930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hartrick C, Van Hove I, Stegmann JU, Oh C, Upmalis D. Efficacy and tolerability of tapentadol immediate release and oxycodone HCl immediate release in patients awaiting primary joint replacement surgery for end-stage joint disease: a 10-day, phase III, randomized, double-blind, active- and placebo-controlled study. Clin Ther. 2009;31(2):260–271. doi: 10.1016/j.clinthera.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 38.Malonne H, Coffiner M, Sonet B, Sereno A, Vanderbist F. Efficacy and tolerability of sustained-release tramadol in the treatment of symptomatic osteoarthritis of the hip or knee: a multicenter, randomized, double-blind, placebo-controlled study. Clin Ther. 2004;26(11):1774–1782. doi: 10.1016/j.clinthera.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 39.Markenson JA, Croft J, Zhang PG, Richards P. Treatment of persistent pain associated with osteoarthritis with controlled-release oxycodone tablets in a randomized controlled clinical trial. Clin J Pain. 2005;21(6):524–535. doi: 10.1097/01.ajp.0000146215.86038.38. [DOI] [PubMed] [Google Scholar]
- 40.Matsumoto AK, Babul N, Ahdieh H. Oxymorphone extended-release tablets relieve moderate to severe pain and improve physical function in osteoarthritis: results of a randomized, double-blind, placebo- and active-controlled phase III trial. Pain Med. 2005;6(5):357–366. doi: 10.1111/j.1526-4637.2005.00057.x. [DOI] [PubMed] [Google Scholar]
- 41.Rauck R, Rapoport R, Thipphawong J. Results of a double-blind, placebo-controlled, fixed-dose assessment of once-daily OROS(R) hydromorphone ER in patients with moderate to severe pain associated with chronic osteoarthritis. Pain Pract. 2013;13(1):18–29. doi: 10.1111/j.1533-2500.2012.00555.x. [DOI] [PubMed] [Google Scholar]
- 42.Roth SH. Efficacy and safety of tramadol HCl in breakthrough musculoskeletal pain attributed to osteoarthritis. J Rheumatol. 1998;25(7):1358–1363. [PubMed] [Google Scholar]
- 43.Spierings EL, Fidelholtz J, Wolfram G, Smith MD, Brown MT, West CR. A phase III placebo- and oxycodone-controlled study of tanezumab in adults with osteoarthritis pain of the hip or knee. Pain. 2013;154(9):1603–1612. doi: 10.1016/j.pain.2013.04.035. [DOI] [PubMed] [Google Scholar]
- 44.Vojtassak J, Vojtassak J, Jacobs A, Rynn L, Waechter S, Richarz U. A phase IIIb, multicentre, randomised, parallel-group, placebo-controlled, double-blind study to investigate the efficacy and safety of OROS hydromorphone in subjects with moderate-to-severe chronic pain induced by osteoarthritis of the hip or the knee. Pain Res Treat. 2011;2011:239501. doi: 10.1155/2011/239501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vorsanger G, Xiang J, Jordan D, Farrell J. Post hoc analysis of a randomized, double-blind, placebo-controlled efficacy and tolerability study of tramadol extended release for the treatment of osteoarthritis pain in geriatric patients. Clin Ther. 2007;29(Suppl):2520–2535. doi: 10.1016/j.clinthera.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 46.Grond S, Sablotzki A. Clinical pharmacology of tramadol. Clin Pharmacokinet. 2004;43(13):879–923. doi: 10.2165/00003088-200443130-00004. [DOI] [PubMed] [Google Scholar]
- 47.Tagarro I, Herrera J, Barutell C, Diez MC, Marin M, Samper D, et al. Effect of a simple dose-escalation schedule on tramadol tolerability: assessment in the clinical setting. Clin Drug Investig. 2005;25(1):23–31. doi: 10.2165/00044011-200525010-00003. [DOI] [PubMed] [Google Scholar]
- 48.Singh DR, Nag K, Shetti AN, Krishnaveni N. Tapentadol hydrochloride: a novel analgesic. Saudi J Anaesth. 2013;7(3):322–326. doi: 10.4103/1658-354X.115319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Raffa RB, Buschmann H, Christoph T, Eichenbaum G, Englberger W, Flores CM, et al. Mechanistic and functional differentiation of tapentadol and tramadol. Expert Opin Pharmacother. 2012;13(10):1437–1449. doi: 10.1517/14656566.2012.696097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.