Abstract
The underlying mechanisms of Mycoplasma pneumoniae pneumonia (MPP) pathogenesis are not clearly understood. This study aimed to investigate the correlation between immune response and lung injury in MPP. The clinical characteristics of MPP were compared between patients treated with and without immunosuppressive chemotherapy, and demographic, clinical, and laboratory data were compared between patients with severe and mild MPP. To determine the effect of immune response on lung lesions, mouse MPP and immunosuppression models were established by intranasal inoculation of M129 and intraperitoneal injection of cyclophosphamide, respectively. Myeloperoxidase and oxidant–antioxidant enzyme activities were evaluated for mechanism studies. The immunosuppressant group had a lower incidence of MPP and fewer cases of severe MPP than the non-immunosuppressant group. The severe MPP group had a greater incidence of severe immune disorders than the mild MPP group. Relative to immunosuppressed mice, wild mice exhibited more severe inflammatory infiltration and lung injury as well as a significant increase in myeloperoxidase and malondialdehyde levels and a decrease in superoxide dismutase level after MP infection. In conclusion, immunological responses likely play a vital role in MPP pathogenesis. Lung injury occurring after MP infection—which might be caused by oxidant–antioxidant imbalance—can be reduced by immunosuppression.
Subject terms: Bacterial infection, Respiratory tract diseases
Introduction
Mycoplasma pneumoniae (MP), a common pathogen of community-acquired pneumonia in children and adolescents, accounts for 10–40% of cases of community-acquired pneumonia in children. It can cause not only MP pneumonia (MPP) but also a variety of extra-pulmonary multiple systemic complications.
Although MP infection is typically self-limiting, a steadily increasing number of recent cases have progressed to refractory, severe, life-threatening pneumonia. Hence, clinical paediatricians should pay more attention to the incidence of severe MPP. Relevant studies have suggested that aggravation of MPP is related to abnormal immune response1, macrolide resistance2, increase in MP copy number3, and co-infection with other pathogens4. As previously reported, in refractory MPP, proper treatment with glucocorticoids and immunoglobulins can significantly inhibit inflammatory reactions and reduce clinical symptoms5,6, which suggests that immune inflammatory injury is an important mechanism of MPP.
An increasing number of studies have reported that immune response acts as a double-edged sword, not only playing an antibacterial role in the early stages of infection but also causing tissue damage as a persistent effect in many types of bacterial infection7. While pulmonary lesions caused by MP infection are usually minimal in immunodeficient children8, immunosuppressive therapy often results in a state of temporary or permanent immune dysfunction and can render an organism more sensitive to pathogens owing to the damage to the immune system. As previously reported, increased activation of T cells and neutrophils in bronchoalveolar lavage fluid (BALF) plays a role in the pathogenesis of acute and severe MPP9.
Neutrophils play a central role in innate immunity, which is involved in the development and progression of inflammatory responses7. Neutrophil infiltration is widely recognized as one of the characteristics of MPP. In refractory MPP, especially, patients have significantly high numbers of neutrophils in BALF and peripheral blood9,10. In addition, patients with corticosteroid-resistant refractory MPP have been reported to have relatively high neutrophil numbers in peripheral blood11. Lai et al.12 have confirmed that neutrophils are not essential for clearance of MP from the lungs; nevertheless, neutrophil accumulation might lead to “hyperinflammation” owing to the release of myeloperoxidase (MPO), matrix metalloproteinase (MMP)-9, and neutrophil elastase (NE)13.
The incidence of MPP, especially severe MPP, has gradually increased in recent years, particularly among younger patients14. However, the pathogenesis of MPP is not entirely clear. In this study, we aimed to explore the relationship between immune response and lung injury after MP infection by comparatively analyzing the clinical data of MPP from patients who received treatment with and without immunosuppressants and by comparing clinical data between patients with mild and severe MPP between January 1 and December 31, 2016. We also established MPP and immunosuppression models in mice for in vivo analysis.
Methods and Materials
Study population
Patients with pneumonia admitted to the Department of Respiratory Medicine and Department of Hematology, Children’s Hospital of Nanjing Medical University, between January 1 and December 31, 2016, were enrolled. All patients met the following inclusion criteria:
Clinical or radiological signs and symptoms of pulmonary infection
Evidence of acute MP infection on the basis of absence of other pathogens.
First, the patients were divided into two groups: the immunosuppressant group, which included patients with MPP who received immunosuppressive chemotherapy for any malignant disease, and the non-immunosuppressant group, which included patients with MPP who did not receive immunosuppressive chemotherapy. Second, patients in the non-immunosuppressant group were divided into the mild and severe MPP groups, which were defined on the basis of previously described criteria15.
Peripheral blood samples were collected upon admission for determining the complete blood count; C-reactive protein (CRP), L-lactate dehydrogenase (LDH), creatine kinase, and immunoglobulin concentrations; and levels of subpopulations of T lymphocytes.
Ethics approval and consent to participate
The study protocol (Protocol number 201703058) was approved by the ethics committee of the Children’s Hospital of Nanjing Medical University and is in compliance with the Declaration of Helsinki. Informed consent was obtained from the parents of all patients included in this study.
Laboratory animals
A total of 96 specific-pathogen-free (SPF) BALB/c mice (age, 6–8 weeks; body weight, 18–20 g) were procured from the animal core facility of Nanjing Medical University. The mice were fed a normal diet and assigned to different groups of 6 each. They were anesthetized for inoculation and euthanasia by injection of 4% chloral hydrate (0.1 mL/10 g body weight). All mice experiments were performed with approval from the Institutional Animal Care and Use Committee, Nanjing Medical University (reference number: IACUC-1601078). We confirm that all experimental procedures were carried out in accordance with the guidelines established by the Institutional Animal Care and Use Committee, Nanjing Medical University, and every effort was made to minimize suffering.
MP culture and quantification
Mycoplasma pneumoniae international standard strain M129 was provided by Professor Chen Z.M. (Children’s Hospital, Zhejiang province). The strain was cultured in a mycoplasma broth consisting of mycoplasma broth base, mycoplasma selective supplement G, 0.5% glucose, and 0.002% phenol red. For in vivo experiments, MP was quantified by measuring the number of colony forming units (CFU) in mycoplasma agar plates, which contained mycoplasma agar base, mycoplasma selective supplement G, and 0.5% glucose16.
Immunosuppression models in mice
Mice were administered intraperitoneal injections of 10 mg/mL cyclophosphamide (CYP) at baseline (200 mg/kg body weight) and 72 h later (100 mg/kg body weight)17,18 Control mice were injected with sterile saline. For in vivo infection studies, mice were inoculated with MP at the time of the second CYP injection.
MP infection models in mice
A total of 96 BALB/c mice were randomly allocated to the MP infection and control groups (48 mice, each). The mice were kept in an SPF animal house and fed separately under standard conditions. After being anesthetized, mice in the infection group were inoculated with 108 CFU of M129 in a 200-µL solution, and the control mice were administered sterile saline, with the head tilted at an angle of 30° to 45° to ensure that the fluid entered the lower respiratory tract through natural breathing movements. Test samples were collected from infected and control mice at five time points — 0, 1, 2, 4, and 8 days after infection.
Collection and analysis of blood and BALF samples
At the time of euthanasia, blood samples from mice were collected in individual microcentrifuge tubes containing ethylenediaminetetraacetic solution to prevent clotting. In all mice, BALF samples were collected three times using 1 mL saline each time; the samples were centrifuged, and the supernatants were stored at −80° C for analysis. Total blood leukocyte and BALF cell counts were determined by manual counting, and differential counts were performed using Giemsa-stained smears.
Real-time PCR for detection of MP
A real-time PCR procedure (Daan Gene Co. Ltd, Guangzhou, China) approved as a clinical diagnostic kit by the State Food and Drug Administration of China was used for detection of MP In brief, one each of equally divided samples of nasopharyngeal aspirate and BALF was shaken for 30 s and centrifuged at 15,000 × g for 5 min. The sediment was collected, and DNA was extracted from a 400-μL sample of the sediment, in accordance with the manufacturer’s instructions. Then, PCR was performed using primers and probes purchased from Daan Gene Co. Ltd. Quantification curves were plotted using several concentrations of standard control samples.
Assay of enzyme and protein levels in lung homogenate and serum samples
Mice were euthanized, following which samples of the left lobe of lungs were collected. These lung-tissue samples were immediately homogenized (100 μg) in 1 mL phosphate-buffered saline at 4 °C and centrifuged at 12,000 rpm for 15 min at 4 °C. The supernatant was then preserved at −70 °C for analysis. Concentrations of total protein, MPO, superoxide dismutase (SOD), and malondialdehyde (MDA) were determined by visible spectrophotometry (Jiancheng Bioengineering Institute, Nanjing, China) using homologous kit reagents.
Hematoxylin–eosin (HE) staining
After infection, mice were euthanized by injection of chloral hydrate. Samples of the right lower lung lobe were collected in 4% formaldehyde solution, fixed, embedded in paraffin, sliced, and stained with hematoxylin–eosin for histopathological analysis.
Data analysis
Statistical analyses were performed using SPSS software, version 17.0 (IBM, Armonk, NY, USA). Normally distributed data were expressed as mean ± standard deviation ( ± s) and compared using the independent samples t-test. Numeration data were analyzed using the chi-square test, and measurement data were analyzed using the Student t-test or a non-parametric test (Mann–Whitney U-test or Wilcoxon test) if data distribution was non-normal. Pearson’s or Spearman’s correlation analysis was used to assess correlations on the basis of normal or non-normal data distribution. Statistical significance was defined as P < 0.05.
Results
The immunosuppressant group had a lower incidence of MPP than the non-immunosuppressant group
A total of 3571 hospitalized children with pneumonia were enrolled in this study, including 201 and 3370 children with pneumonia who did and did not receive immunosuppressant chemotherapy, respectively; in these two groups, 19 (9.4%) and 789 (23.4%) children, respectively, were diagnosed with MPP.
Table 1 presents a comparison of relevant demographic, clinical, laboratory, and radiological data between patients with MPP in the non-immunosuppressant and immunosuppressant groups. In short, there was no significant difference between patients with MPP in the two groups with respect to age or sex distribution. However, among patients with MPP, the non-immunosuppressant group had a greater incidence of complications and severe MPP than the immunosuppressant group (P < 0.001). With regard to laboratory findings, among patients with MPP, the WBC, peripheral neutrophil, and CRP levels in the non-immunosuppressant group were significantly higher than those in the immunosuppressant group (P < 0.001). Furthermore, there was no significant difference between the two subgroups in peripheral lymphocyte population or LDH levels (P < 0.001).
Table 1.
Comparison of clinical characteristics of MPP between the immunosuppressant and non-immunosuppressant groups.
| Non-immunosuppressant group (n = 789/3370) |
Immunosuppressant group (n = 19/201) |
P value | |
|---|---|---|---|
| MP incidence, % | 23.41 | 9.45 | 0.000 |
| Age, years | 3.57 ± 2.797 | 3.79 ± 2.76 | 0.222 |
| Sex (male/female) | 428/361 | 9/10 | 0.553 |
| Complications | 159 (20.15%) | 3 (15.78%) | 0.001 |
| Severe cases | 220 (27.8%) | 0 (0%) | 0.000 |
| WBC × 109/L | 9.80 ± 4.51 | 6.01 ± 7.26 | 0.000 |
| Neutrophils × 109/L | 5.46 ± 3.49 | 2.43 ± 2.46 | 0.001 |
| Lymphocytes × 109/L | 3.36 ± 2.55 | 2.81 ± 5.56 | 0.669 |
| CRP, mg/L | 16.32 ± 20.78 | 43.19 ± 44.34 | 0.043 |
| LDH, IU/L | 383.80 ± 216.16 | 297.18 ± 109.69 | 0.099 |
MPP, Mycoplasma pneumoniae pneumonia; MP, Mycoplasma pneumoniae; WBC, white blood cells; CRP, C-reactive protein; LDH, L-lactate dehydrogenase. Data are presented as mean ± standard deviation or number (percentage).
Immune inflammation was involved in lung injury after MP infection
Of the 789 patients receiving non-immunosuppressant therapy who were diagnosed with MPP between January 1 and December 31, 2016, 569 patients (male, 313; female, 256; median age, 3.32 years) were assigned to the mild MPP group, and 220 patients (male, 115; female, 105; median age, 4.19 years) were assigned to the severe MPP group. The median age of the severe MPP group was significantly higher than that of the mild MPP group (P = 0.000). However, there was no significant difference in sex distribution between the two groups (Table 2).
Table 2.
Demographic data and clinical and laboratory characteristics of the severe and mild MPP groups.
| Mild MPP (n = 569) |
Severe MPP (n = 220) |
P value | |
|---|---|---|---|
| Age, years | 3.32 ± 2.68 | 4.19 ± 2.98 | 0.000 |
| Sex (male/female) | 313/256 | 115/105 | 0.524 |
| Duration of fever before hospitalization, days | 4.23 ± 3.31 | 5.47 ± 4.03 | 0.000 |
| Length of hospitalization, days | 8.16 ± 2.22 | 9.6 ± 3.95 | 0.000 |
| Fever, n (%) | 476 (83.65%) | 191 (86.81) | 0.323 |
| Cough, n (%) | 569 (100%) | 219 (99.5%) | 1.000 |
| Wheezing, n (%) | 160 (28.11%) | 66 (30.00%) | 0.599 |
| WBC × 109/L | 9.71 ± 4.31 | 10.03 ± 5.00 | 0.367 |
| Neutrophils, % | 52.68 ± 16.64 | 58.80 ± 17.59 | 0.000 |
| Lymphocytes, % | 37.75 ± 28.47 | 32.51 ± 16.33 | 0.048 |
| Platelets × 109/L | 275.72 ± 28.47 | 301.59 ± 116.85 | 0.004 |
| LDH, U/L | 382.16 ± 222.91 | 387.81 ± 159.21 | 0.749 |
| CRP, mg/L | 14.59 ± 17.47 | 20.78 ± 27.09 | 0.002 |
| Cell-mediated immunity, % | |||
| CD3+ cells | 64.70 ± 10.39 | 63.82 ± 11.11 | 0.330 |
| CD3 + CD4+ cells | 35.70 ± 9.01 | 35.39 ± 8.99 | 0.682 |
| CD3 + CD8+ cells | 25.80 ± 7.62 | 25.21 ± 8.06 | 0.365 |
| CD3 − CD19+ cells | 19.28 ± 8.63 | 19.18 ± 9.46 | 0.888 |
| CD3 − CD(16+ 56+)+ natural killer cells | 12.01 ± 6.91 | 12.55 ± 7.19 | 0.372 |
| CD4+/CD8+ | 1.52 ± 0.66 | 1.55 ± 0.71 | 0.584 |
| Humoral immunity, g/L | |||
| IgA | 1.07 ± 0.68 | 1.05 ± 0.68 | 0.736 |
| IgG | 7.85 ± 3.39 | 8.56 ± 3.12 | 0.008 |
| IgM | 2.19 ± 2.39 | 1.88 ± 1.93 | 0.084 |
| Log(MP DNA) | 5.10 ± 1.33 | 5.26 ± 1.40 | 0.132 |
MPP, Mycoplasma pneumoniae pneumonia; WBC, white blood cells; LDH, L-lactate dehydrogenase; CRP, C-reactive protein; CD, cluster of differentiation; Ig, immunoglobulin; MP, Mycoplasma pneumoniae. Data are presented as mean ± standard deviation or number (percentage).
The duration of fever and length of hospitalization were longer in the severe MPP group than in the mild MPP group (P < 0.01). However, the two groups exhibited no significant difference in the incidence of cough or wheezing (P < 0.05). The laboratory data of patients in the mild and severe MPP groups at admission are shown in Table 2. The severe MPP group exhibited higher neutrophil, platelet, CRP, and immunoglobulin G levels and lower lymphocyte levels than the mild MPP group. Surprisingly, there was no statistically significant difference in the level of cell-mediated immunity or MP DNA copy number between the mild and severe MPP groups (Table 2).
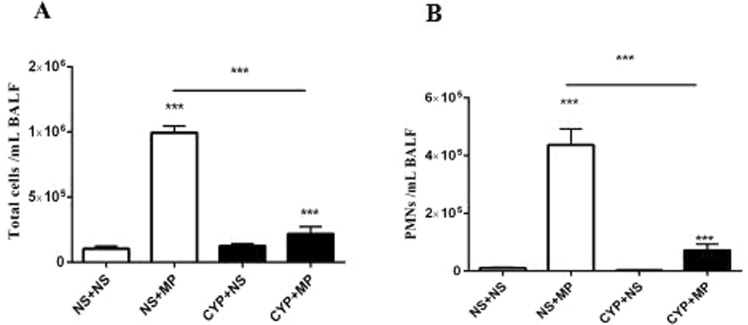
Immunosuppressants inhibited the recruitment of inflammatory cells, especially neutrophils, into lung tissues
In mice, treatment with CYP at 200 and 100 mg/kg at baseline and 72 h later, respectively, caused a significant reduction in leucocyte count (from 3833 ± 749 to 1313 ± 312 leucocytes/mm3), especially in case of polymorphonuclear neutrophils (PMNs; from 1167 ± 111.6 to 216.7 ± 45.3 PMNs/mm3). Intranasal inoculation of 108 CFU of M129 resulted in MPP, with a significant increase in PMN recruitment to the lungs by 96 h post-infection (Fig. 1). Lung pathology and PCR (number of MP DNA copies in BALF) findings proved that the MPP model was successful, thus providing the basis for follow-up experiments.
Figure 1.
Inflammatory cell recruitment into lung tissues after MP infection. The number of cells in BALF collected from mice pre-treated with CYP/saline and injected with 108 colony forming units of MP/saline for 96 h is shown. (A) Total number of cells in BALF. (B) PMNs in BALF. Data are presented as mean ± standard deviation (n = 5–7). MP, Mycoplasma pneumoniae; BALF, bronchoalveolar lavage fluid; CYP, cyclophosphamide; PMN, polymorphonuclear neutrophils; NS + NS, uninfected immunocompetent mice; CYP + NS, uninfected immunocompromised mice; NS + MP, infected immunocompetent mice; CYP + MP, infected immunocompromised mice. ***P < 0.001.
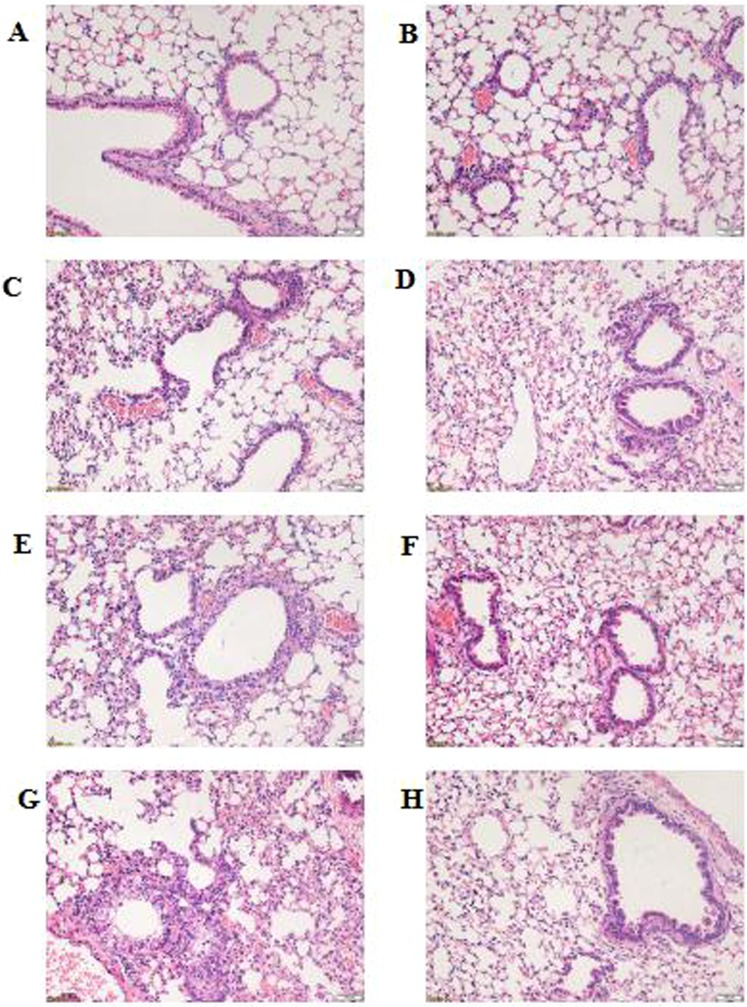
Immunosuppressants inhibited histopathological damage after MP infection
Histopathological changes were evaluated by HE staining of lung-tissue samples harvested after MP infection. As shown in Fig. 2A,B, the NS + NS (uninfected immunocompetent mice) and CYP + NS (uninfected immunocompromised mice) groups exhibited normal pulmonary structure without obvious differences. After MP infection, infected immunocompetent mice (NS + MP group) exhibited significant histological lesions, including cellular infiltration, alveolar-wall thickening, obvious hypersecretion, and even structural collapse (Fig. 2C,E,G), while infected immunocompromised mice (CYP + MP group) only exhibited mild histological lesions (Fig. 2D,F,H).
Figure 2.
Histopathological changes in lung tissues. Histological changes were determined at 0, 24, 48, and 96 h after Mycoplasma pneumoniae infection (hematoxylin–eosin staining; 200×). At 0 h: (A) NS + NS and (B) CYP + NS groups. At 24 h: (C) NS + MP and (D) CYP + MP groups. At 48 h: (E) NS + MP and (F) CYP + MP groups. At 96 h (G) NS + MP and (H) CYP + MP groups. NS + NS, uninfected immunocompetent mice; CYP + NS, uninfected immunocompromised mice; NS + MP, infected immunocompetent mice; CYP + MP, infected immunocompromised mice.
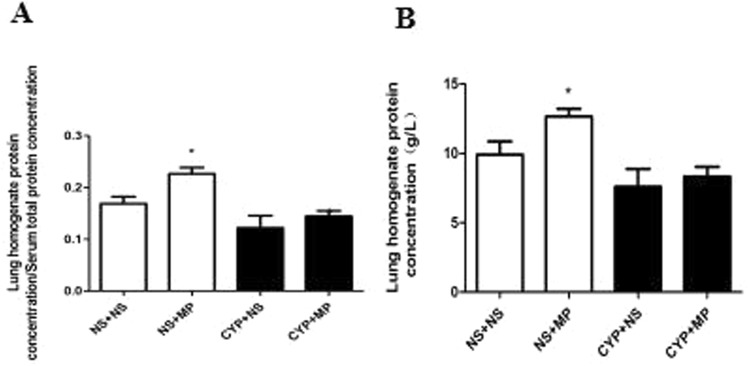
Immunosuppressants inhibited lung injury after MP infection
As shown in Fig. 3A,B, at 4 days after MP infection, both immunocompromised and immunocompetent mice exhibited increases in protein concentration in lung homogenate and ratio of protein concentration in lung homogenate and serum (P < 0.05). In terms of these two indexes, the NS + MP group exhibited a greater increase than the CYP + MP group.
Figure 3.
Pulmonary vascular permeability damage indexes. Lung tissues and serum were processed to determine the protein concentration in lung homogenate (A) and the ratio of protein concentration in lung homogenate and serum (B) at 96 h after Mycoplasma pneumoniae infection. NS + NS, uninfected immunocompetent mice; CYP + NS, uninfected immunocompromised mice; NS + MP, infected immunocompetent mice; CYP + MP, infected immunocompromised mice. Values are presented as mean ± standard deviation (n = 6). *P < 0.05.
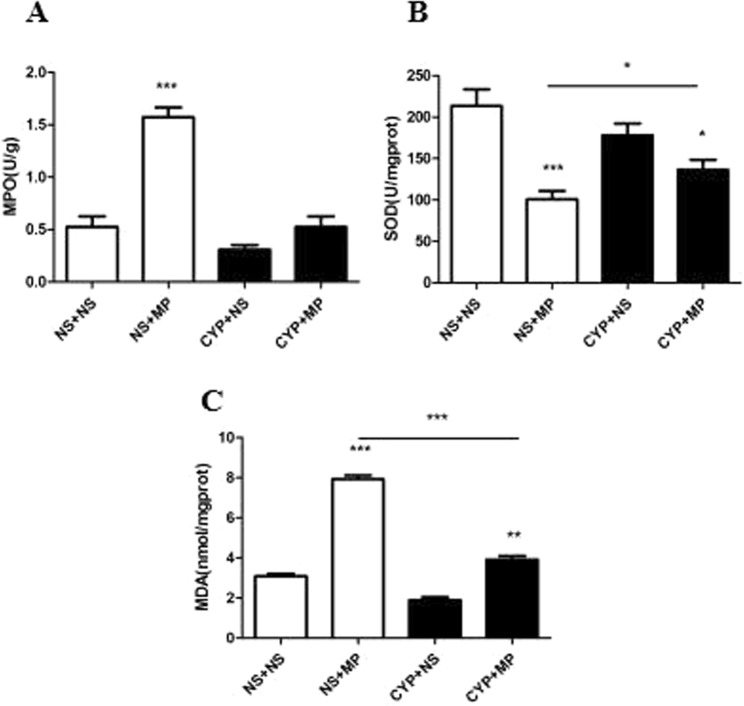
MPO and oxidant–antioxidant enzyme activities mediated the immune response
Myeloperoxidase is an indicator of PMN infiltration. As shown in Fig. 4A, while immunocompetent mice exhibited an increase in MPO activity after MP infection, immunocompromised mice did not. While SOD activity indirectly reflects the antioxidant capacity of the lungs, MDA concentration indicates the severity of reactive oxygen species (ROS) attack. Relative to immunocompromised mice, immunocompetent mice exhibited a significantly greater decrease in SOD level and increase in MDA level after MP infection (P < 0.05).
Figure 4.
MPO and oxidant–antioxidant enzyme activities. Lung tissues were collected and homogenized to determine MPO activity (A) and SOD (B) and MDA (C) levels at 96 h after Mycoplasma pneumoniae infection. MPO, myeloperoxidase; SOD, superoxide dismutase; MDA, malondialdehyde. NS + NS, uninfected immunocompetent mice; CYP + NS, uninfected immunocompromised mice; NS + MP, infected immunocompetent mice; CYP + MP, infected immunocompromised mice. Values are presented as mean ± standard deviation (n = 6). *P < 0.05; **P < 0.01; ***P < 0.001.
Discussion
The pathogenesis of MP infection is complex and involves adhesion damage; destruction of membrane fusion; nutrition depletion; and invasive, toxic, inflammatory, and immune damage. Immunological response appears to play an important role in aggravation of MPP. As a double-edged sword, the human immune system is usually able to protect the body against infections, but it also causes tissue damage. This study aimed to investigate the correlation between immune response and lung injury in MPP.
On the basis of the findings of many studies, it is believed that immunocompromised patients are more susceptible to pulmonary infections and experience a more severe disease course than the general population19. Surprisingly, we observed a greater incidence of MPP, especially severe MPP, among children receiving non-immunosuppressive treatment than among those receiving immunosuppressive treatment, which reminded us of the protective role of immunosuppression in MPP.
Although mycoplasmal pneumonia is usually self-limited and benign, in some cases, it may progress to clinical and radiological deterioration. As an increasing amount of research is being conducted on MP and many new and interesting discoveries are being made, many reports thus far have confirmed that aggravation of MPP might be due to host immune response rather than direct microbial damage. In our study, the severe MPP group exhibited a greater incidence of severe immune disorders than the mild MPP group. It was, therefore, hypothesized that immunosuppression could reduce lung injury after MP infection. In order to test this hypothesis, we successfully established MPP and immunosuppression models in mice.
The in vivo findings demonstrated that lung lesions were markedly inhibited in the immunosuppression model of MPP, which confirmed for us that host immune response mediates lung injury after MP infection. In a related study on sepsis20, it was verified that a low dose of cyclophosphamide could improve the survival duration in a murine model of sepsis, which supported the theory that appropriate immunosuppression can protect against severe immune reaction and improve the prognosis. As demonstrated in several studies, both cell-mediated and humoral immunological responses play an important role in the progression of MPP, especially with regard to imbalance in T cell populations11,21. However, few studies have evaluated the relationship between neutrophil-mediated hyperinflammation and MPP9,13.
Polymorphonuclear neutrophils are an important component of the immune defense system. It is well known that neutrophils play a vital role in eliminating pathogens through degranulation, autophagy, and neutrophil traps; these processes generate proteases, ROS, and reactive nitrogen species22, which can clear bacteria but also partially cause oxidant–antioxidant disorders. In a previous study on airway mycoplasma infection, Xu et al.23 suggested that PMNs could increase histamine production by upregulating enzyme transcription once antihistamine levels and histopathological scores were decreased and the pneumonia grade was changed.
In addition, Chen et al.16 had reported that, in MP infection, neutrophil accumulation might lead to hyperinflammation due to release of MPO, MMP-9, and NE. In our study, the results of MPO and oxidant–antioxidant enzyme activities demonstrated the existence of an oxidant–antioxidant imbalance in the body after MP infection; this phenomenon was more severe in immunocompetent mice than in immunocompromised mice, which indicated to us that neutrophils might participate in this pathogenic process by mediating oxidative stress. Further study is required to prove the changes and pathological role of neutrophils in lung injury after MPP.
In conclusion, we suppose that immunological response likely plays a vital role in the pathogenesis of MPP and that lung injury after MP infection—which might be caused by oxidant–antioxidant imbalance—could be reduced by immunosuppression.
Acknowledgements
This study was supported by grants from the Nanjing Medical Science and Technique Development Foundation, Nanjing, China (JQX15008); Jiangsu Youth Medical Talent Foundation, Nanjing, China (QNRC2016087); National Natural Science Foundation of China (81700035); Cooperative Research Project between Southeast University and Nanjing Medical University, Nanjing, China (2242018K3DN20); Foundation of Jiangsu Health and Family Planning Commission, Nanjing, China (ZKX18041) and Foundation of Nanjing Municipal Science and Technology Commission, Nanjing, China (201723003).
Author Contributions
Conceptualization, D.Z. and F.L. Data curation, S.S. and X.Z. Methodology and Investigation, S.S., X.Z., Y.Z. and H.T. Formal analysis and Writing – Original Draft Preparation, S.S. Writing – Review & Editing, S.S., X.Z., D.Z. and F.L.
Data Availability
The datasets used and analyzed during the present study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shuang Shi and Xiuqing Zhang contributed equally.
Contributor Information
Deyu Zhao, Email: zhaodeyu988@126.com.
Feng Liu, Email: axsliu@163.com.
References
- 1.Shimizu T, Kida Y, Kuwano K. Cytoadherence-Dependent Induction of Inflammatory Responses by Mycoplasma Pneumoniae. Immunology. 2011;133:51–61. doi: 10.1111/j.1365-2567.2011.03408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurata S, Taguchi H, Sasaki T, Fujioka Y, Kamiya S. Antimicrobial and Immunomodulatory Effect of Clarithromycin On Macrolide-Resistant Mycoplasma Pneumoniae. J Med Microbiol. 2010;59:693–701. doi: 10.1099/jmm.0.014191-0. [DOI] [PubMed] [Google Scholar]
- 3.Nilsson AC, Bjorkman P, Welinder-Olsson C, Widell A, Persson K. Clinical Severity of Mycoplasma Pneumoniae (MP) Infection is Associated with Bacterial Load in Oropharyngeal Secretions but Not with MP Genotype. BMC Infect Dis. 2010;10:39. doi: 10.1186/1471-2334-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, Liu J, Zhao S, Yang Y, Wu J. [Clinical Features and Treatment of Refractory Mycoplasma Pneumoniae Pneumonia Unresponded to Conventional Dose Methylprednisolone in Children] Zhonghua Er Ke Za Zhi. 2014;52:172–176. [PubMed] [Google Scholar]
- 5.Shan LS, et al. Effects of methylprednisolone or immunoglobulin when added to standard treatment with intravenous azithromycin for refractory Mycoplasma pneumoniae pneumonia in children. World J. Pediatr. 2017;14:321–327. doi: 10.1007/s12519-017-0014-9. [DOI] [PubMed] [Google Scholar]
- 6.Tamura A, et al. Methylprednisolone pulse therapy for refractory Mycoplasma pneumoniae pneumonia in children. J. Infect. 2008;57:223–228. doi: 10.1016/j.jinf.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Craig A, Mai J, Cai S, Jeyaseelan S. Neutrophil recruitment to the lungs during bacterial pneumonia. Infect. Immun. 2009;77:568–575. doi: 10.1128/IAI.00832-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foy HM, Ochs H, Davis SD, Kenny GE, Luce RR. Mycoplasma Pneumoniae Infections in Patients with Immunodeficiency Syndromes: Report of Four Cases. J Infect Dis. 1973;127:388–393. doi: 10.1093/infdis/127.4.388. [DOI] [PubMed] [Google Scholar]
- 9.Guo L, Liu F, Lu MP, Zheng Q, Chen ZM. Increased T cell activation in BALF from children with Mycoplasma pneumoniae pneumonia. Pediatr. Pulmonol. 2015;50:814–819. doi: 10.1002/ppul.23095. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Y, et al. The clinical characteristics and predictors of refractory Mycoplasma pneumoniae pneumonia in children. PLoS. One. 2016;11:e156465. doi: 10.1371/journal.pone.0156465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yan Y, Wei Y, Jiang W, Hao C. The clinical characteristics of corticosteroid-resistant refractory Mycoplasma Pneumoniae pneumonia in children. Sci. Rep. 2016;6:39929. doi: 10.1038/srep39929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai JF, et al. Critical Role of Macrophages and their Activation Via MyD88-NFkappaB Signaling in Lung Innate Immunity to Mycoplasma Pneumoniae. Plos One. 2010;5:e14417. doi: 10.1371/journal.pone.0014417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Z, et al. Role of the Mycoplasma pneumoniae/Interleukin-8/Neutrophil Axis in the Pathogenesis of Pneumonia. Plos One. 2016;11:e146377. doi: 10.1371/journal.pone.0146377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saraya T, et al. Novel Aspects On the Pathogenesis of Mycoplasma Pneumoniae Pneumonia and Therapeutic Implications. Front Microbiol. 2014;5:410. doi: 10.3389/fmicb.2014.00410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Subspecialty Group of Respiratory Diseases, The Society of Pediatrics, Chinese Medical Association; Editorial Board, Chinese Journal of Pediatrics.Guidelines for Management of Community Acquired Pneumonia in Children (The Revised Edition of 2013) (I). Zhonghua Er Ke Za Zhi. 51, 745–752 (2013). [PubMed]
- 16.Li S, et al. Global Secretome Characterization of A549 Human Alveolar Epithelial Carcinoma Cells During Mycoplasma Pneumoniae Infection. BMC Microbiol. 2014;14:27. doi: 10.1186/1471-2180-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hickman-Davis JM, Lindsey JR, Matalon S. Cyclophosphamide Decreases Nitrotyrosine Formation and Inhibits Nitric Oxide Production by Alveolar Macrophages in Mycoplasmosis. Infect Immun. 2001;69:6401–6410. doi: 10.1128/IAI.69.10.6401-6410.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yun L, Wu T, Li Q, Zhang M. Dietary Supplementation with Purified Wheat Germ Glycoprotein Improve Immunostimulatory Activity in Cyclophosphamide Induced Balb/c Mice. Int J Biol Macromol. 2018;118:1267–1275. doi: 10.1016/j.ijbiomac.2018.06.199. [DOI] [PubMed] [Google Scholar]
- 19.Sousa D, et al. Community-Acquired Pneumonia in Immunocompromised Older Patients: Incidence, Causative Organisms and Outcome. Clin Microbiol Infect. 2013;19:187–192. doi: 10.1111/j.1469-0691.2012.03765.x. [DOI] [PubMed] [Google Scholar]
- 20.Brown I, et al. Low-Dose Cyclophosphamide Improves Survival in a Murine Treatment Model of Sepsis. SHOCK. 2015;43:92–98. doi: 10.1097/SHK.0000000000000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo H, He Z, Li M, Wang T, Zhang L. Imbalance of Peripheral Blood Th17 and Treg Responses in Children with Refractory Mycoplasma Pneumoniae Pneumonia. J Infect Chemother. 2016;22:162–166. doi: 10.1016/j.jiac.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Camp JV, Jonsson CB. A Role for Neutrophils in Viral Respiratory Disease. Front Immunol. 2017;8:550. doi: 10.3389/fimmu.2017.00550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu X, et al. Neutrophil Histamine Contributes to Inflammation in Mycoplasma Pneumonia. J Exp Med. 2006;203:2907–2917. doi: 10.1084/jem.20061232. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the present study are available from the corresponding author on reasonable request.