Abstract
With the emergence of work-related musculoskeletal disorders and the associated high cost of injured workers, physical therapists are in a unique position to help employers manage these concerns through multidisciplinary injury prevention programs, education, ergonomics, on-site treatment, and return to work programs. The purpose of this paper, through a review of the literature, is to describe the effect that workplace injuries have on employees and the economic burden on employers. Furthermore, this paper will highlight the effectiveness a physical therapist can have in the occupational health setting as part of a multidisciplinary team on ergonomics, employee health, prevention of work-related musculoskeletal disorders, return to work programs, and on-site treatment interventions, such as therapeutic exercise and manual intervention. This review of the literature suggests that participation in ergonomics and on-site physical therapy treatment in the workplace (e.g., education, exercise, manual intervention) has a positive effect on decreasing work-related musculoskeletal disorders, decreasing costs associated with these injuries, increasing work productivity, and decreasing absenteeism and improving presenteeism amongst workers. It is important to ensure that payers, employers, and employees are aware of the crucial role physical therapists can play in occupational health. Physical therapists also need to advocate for their role in occupational health and offer expert care to workers in a nontraditional manner.
Keywords: Ergonomics, On-site physical therapy, Injury prevention, Work-related musculoskeletal disorders
INTRODUCTION
Musculoskeletal disorders (MSDs) are pathological injuries to the bones, ligaments, joints, muscles, nerves, and vascular system which can affect the overall function of the human body. Work-related MSDs (WMSDs) are injuries to the musculoskeletal system occurring in the workplace, due to the environment, caused by repetitive motions such as bending, crawling, twisting, lifting, pushing, and pulling. WMSDs have been classified by the World Health Organization in two categories: acute and chronic injuries. Acute injuries are those that have occurred recently and may require immediate care from a health care professional. Chronic injuries happen slowly over time and lead to lingering soreness and discomfort within the body; care from a health care professional is also indicated, depending on the nature and severity of the chronic injury, and whether or not it influences performance in the work place.
The economic burden of both MSDs and WMSDs is quite substantial. Liberty Mutual Insurance (2018) reported in their safety index for 2018 that 13.7 billion dollars were spent in 2017 on overexertion injuries in the workplace. The Bureau of Labor Statistics (2018) reported that in the private workplace industry there were approximately 2.9 million nonfatal injuries in the workplace in 2016. Thirty percent of those injuries were classified as sprains, strains, and tears resulting from overexertion injuries.
The next logical step to address these concerns is to focus on assigning a healthcare professional who specializes in workplace safety, ergonomics, and treatment of both MSDs and WMSDs. Physical therapists are in a distinct situation to help aide this growing epidemic. Physical therapists can prevent and treat musculoskeletal conditions within the population through education, ergonomics training, workplace safety modifications, exercise prescription and monitoring, and hands-on manual interventions (Bezner, 2015). Ergonomics is described as preparing the worker to be able to perform work tasks safely with the aim of reducing costs from employers, increasing productivity in the workplace, decreasing WMSDs, and decreasing overall absenteeism with workers (Pikaar, 2012). On-site physical therapy treatment including ergonomic education, training, and exercise, have been shown to be very cost effective, with employees spending significantly less money on health care costs when seeking treatment and advice on-site compared with offsite treatments (Cecil and Ross, 2017; Tompa et al., 2010).
The purpose of this paper is to describe the effect that workplace injuries have on employees and the economic burden on employers. This paper will highlight the effectiveness a physical therapist can have in the occupational health setting on ergonomics, employee health, preventions of MSDs and WMSDs, return to work programs, and on-site treatment interventions, such as therapeutic exercise prescription and manual intervention. With the prevalence of increased worksite injuries as well as the increased cost related to these injuries, it has been recommended that healthcare professionals need to move our healthcare system towards more proactive prevention and wellness and move away from the more traditional model of simply reactively treating injuries and illnesses (Cecil and Ross, 2017). Therefore, there would be benefit in having physical therapists play an expanded role in occupational health, by being a part of a multidisciplinary team and utilizing their unique clinical skill set to promote cost savings in the way of worksite injury prevention programs, education, ergonomics, on-site treatment, and return to work programs. The theoretical framework being used for this investigation is the knowledge translation theory. The knowledge translation theory allows researchers to take findings from the research and then apply these outcomes to clinical practice (Curran et al., 2011).
LITERATURE REVIEW
This literature review will highlight the effectiveness a physical therapist can have as part of a multidisciplinary team in the occupational health setting on ergonomics, employee health, prevention of WMSDs, return to work programs, and on-site treatment interventions, such as therapeutic exercise and manual intervention. This review will be divided into two parts: (a) case reports and intervention studies and (b) literature reviews, systematic reviews, and meta-analyses for ergonomics and on-site physical therapy. Both areas of study were evaluated to determine the value of ergonomics training and on-site physical therapy in the workplace.
CASE REPORTS AND INTERVENTION STUDIES
This literature review will begin with an examination of research that has been focused on the care delivered when physical therapists act in the role of primary health professionals. Studies include interventions with the delivery of worksite ergonomics, worksite safety protocols, workplace physical therapy examinations, return to work programs, and physical therapy treatments.
A 29-year-old injured male worker with generalized cervical spine pain was the subject of a case study. The symptoms resulted from prolonged sessions sitting at his workstation computer. The patient was examined by a resident physical therapist on day 1 and again 6 weeks later after the patient was discharged following four 30-min treatment sessions. The physical therapist provided ergonomic training and education, manual therapy including joint and soft tissue mobilization for the cervical and thoracic spines, therapeutic exercises to address postural deficits, a workplace modification for the employee, and referral for an eye examination. At the patient’s 6-week visit, he was re-examined and reported less pain, increased range of motion, improved posture, and greater awareness of workplace safety and injury prevention tactics, and improved quality in work and activities of daily living (Chetty, 2010).
Two recent studies have examined the impact that on-site physical therapy and ergonomics has in the workplace. The first study investigated the effects of ergonomic interventions and strengthening exercises on acute musculoskeletal injuries amongst office workers. One hundred forty-two office workers aged 20–50 years old with neck, shoulder, and lower back pain were randomly assigned to one of four groups: an ergonomics group, an exercise group, a combined ergonomics and exercise group, and a control (no treatment) group. The exercise training group performed a series of stretching exercises that were designed to increase range and flexibility of motion of the back musculature as well as shoulders and neck joints, while the ergonomic group received some modification in the working place. More specifically, this included a “total workplace Occupational Safety and Health and ergonomic intervention” that involved modification of the chair height, work desk, sitting posture, and the distance and level between the eyes and the computer monitor. Patient outcome measures were assessed using the Cornell Musculoskeletal Disorders Questionnaire at baseline, 2, 4, and 6 months. The results of this study suggested that all of the groups showed a significant improvement in comparison with the control group (no treatment) and comparison with their baseline scores. Additionally, exercise modification was more effective in comparison with ergonomic modification after 4 months, suggesting that stretching exercises should be included in the treatment of office workers with neck, shoulder, and lower back pain, rather than solely relying on ergonomic modification for the treatment of WMSDs (Shariat et al., 2018). The second study investigated the effects of different ergonomic chairs on pain and muscle spasm in female office workers. A series of randomized, one subject design studies using A-B-A-C-A format over a 4-week period was used (n=2). Subjects completed the visual analog scale for pain levels and the Work Productivity and Activity Impairment questionnaire at baseline and at 4 weeks. Subjects were asked to complete high intensity office and computer work while either using either an intervention ergonomic chair or a less adjustable control ergonomic chair. The findings demonstrated that both intervention chairs reduced the frequency, intensity, and variability of pain and muscle spasm. One of the participants also showed an increase in productivity with both chairs. This implies that office chairs without adjustable armrests may be equivalent to more expensive fully adjustable chairs with respect to pain, muscle spasm and disability (Hoeben and Louw, 2014).
A series of ergonomic education studies were carried out including one conducted by Mani et al. (2016), which investigated the effects of ergonomic education sessions on awareness of risk factors of WMSDs among office workers. Researchers gave one educational session per week for 6 weeks and participants completed an ergonomics questionnaire and the Rapid Office Strain Assessment on postural assessment at baseline and 6 weeks. Results showed that 89% of the participants had a better understanding and awareness of WMSDs, improved posture and work behaviors. Another study involving ergonomic education used a single-blinded randomized control trial design to determine the effects of ergonomic training and education on posture and low back pain among nurses. One hundred twenty-four nurses with chronic low back pain were randomly assigned to either the experimental group or the control group. The experimental group participated in Back School once a week for 6 weeks; each 50-min session was divided into a 10-min ergonomics training exercise, and 20 min of muscle strengthening and stretching exercises prescribed by a physical therapist. The ergonomics training included education in body mechanics, posture, lifting techniques, biomechanical risk factors, and workstation assistance and redesign. The structure of muscle strengthening and stretching exercises were based on the Sachse–Janda–Lewit system: stretching muscles that are prone to shorthening and hypertonicity (e.g., pectoralis major, rectus femoris, the lower of the erector spinae, iliopsoas, upper trapezius) and strengthening muscles that are prone to weakening and hypotonicity (e.g., rhomboideus, abdominals, gluteus maximus and medius, lower and middle trapezius). The control group received a passive physical therapy intervention which consisted of heat and transcutaneous electrical nerve stimulation with no ergonomic training. Subjects completed a biomechanical postural assessment from a physical therapist and completed the visual analog scale for pain. This study showed a significant improvement in posture and decreased pain levels in nurses completing ergonomic training and education with physical therapist intervention versus nurses who received a passive physical therapy intervention at both the 6 month and 1-year follow-up. The authors recommended adopting the Back School program for the treatment of the healthcare workers with chronic low back problems as the treatment of choice and the standard when designing occupational healthcare policies and procedures (Jaromi et al., 2012). A study by Noh and Roh (2013) was done to assess posture among dental hygienists to identify potential musculoskeletal injuries occurring in the workplace. Three dental hygienists with at least 10 years’ experience had their posture videotaped and assessed during work by physical therapists. Physical therapists identified the shoulders, upper and lower back, and the waistline as areas for potential WMSDs. The researchers concluded that the development of therapeutic exercise programs that can be easily performed in the workplace and during activities of daily living would be crucial to prevent WMSDs among dental hygienists. Furthermore, the authors created a series of eight stretching and strengthening exercises to prevent injury in this population.
A recent study was conducted investigating the effects that different rehabilitation procedures and supportive conditions (e.g., influence at work, possibilities for development, degree of freedom at work, meaning of work, quality of leadership, social support, sense of community, and work satisfaction) have on work ability and the return to work process after a WMSD. The study consisted of 324 women in human services organizations who were out of work due to sickness or injury. Participants completed questionnaires on rehabilitations measures (e.g., manual therapy, stretching, and strengthening exercises), the Work Ability Index, working degree, and the Copenhagen Psychological Questionnaire at baseline, 6 months, and 12 months. The researchers concluded that participants worked harder and more often when employees had appropriate rehabilitation measures in place along with an on-site ergonomics program for successful return to work for employees. Furthermore, they recommended integrating workplace rehabilitation with supportive conditions at work in order to increase work ability and improve the return to work process for women on long-term sick leave (Ahlstrom et al., 2013).
Engberg et al. (2018) investigated the effect of health clinics providing physical therapy for teachers in a public school. A difference-in-difference approach was used and researchers looked at a public school’s student achievement growth, insurance claims, and health risk assessments for all active teachers during the academic years of 2007–2015. When compared with traditional, off-site treatment options for all medical and rehabilitation care, a worksite clinic decreased overall admissions to inpatient facilities, decreased overall healthcare costs, and showed lower rates of absenteeism in the population that was studied. Researchers determined that onsite healthcare clinics were important in reducing overall costs from insurances companies and significantly decreased work loss time (Engberg et al., 2018). Another study involving an academic institution was performed at the Emory Healthcare Center at Emory University in Atlanta, Georgia. The university invested in two contract orthopedic physical therapists who were trained in ergonomics to work on campus to treat employees experiencing musculoskeletal injuries as well as provide all staff with ergonomic interventions. The primary departments where injuries occurred were in Nursing, Facilities Management, and the Food and Nutrition Departments. University employees were discharged after a mean of five visits compared with the national average of 14 visits for a traditional outpatient physical therapist clinic course of care. The university saved $887,574 overall and 93% of all injured employees who sought treatment on campus returned to work full-time. A decrease in overall lifting injuries at the university was also noted (Norris, 2015).
ERGONOMICS AND ON-SITE PHYSICAL THERAPY IN LITERATURE REVIEWS, SYSTEMATIC REVIEWS, AND META-ANALYSES
There has been significant work done by researchers on the topic of ergonomics, on-site physical therapy, and reviews investigating the economic burden associated MSDs and WMSDs. All reviews included in this paper have a physical therapist as the primary health professional delivering ergonomic training and on-site treatment deliveries to employers.
Three literature reviews were conducted that looked at the effects that ergonomics and on-site physical therapy have in occupational health, as well as the role of the physical therapist in occupational health. First, a review by Kim et al. (2013) examined 36 scholarly journal articles to investigate how effective ergonomic interventions were when provided by physical therapists in the treatment of WMSDs. Included were literature reviews and studies with an inclusion criterion of ergonomic training and education as the intervention which was delivered by a physical therapist. Researchers found that ergonomic interventions were effective in treating WMSDs but much more rigorous studies need to be done to draw better conclusions as to the effect of ergonomic interventions for the treatment of WMSDs. Second, a literature review from Chetty (2013) was done to investigate the role in which a physical therapist plays in the field of occupational health. This author identified physical therapy playing a role in occupational health in the following ways: pre-employment screenings, ergonomic trainings, injury prevention methods, work hardening programs, on-site treatments of injured workers, and assisting human resources with case management duties. Third, a literature review on the role a physical therapist has in interventions to prevent workplace injuries and their role as return to work coordinators was also conducted. Researchers included 22 studies for this literature review. Researchers concluded that there are six domains for a physical therapist’s role in the workplace: ergonomic and workplace assessment, interviewing workers for clinical issues, social problem solving, mediation about health concerns in the workplace, and overall knowledge of medical and musculoskeletal conditions (Shaw et al., 2008).
Four systematic review were carried out looking at how ergonomic education, on-site physical therapy, and workstation adjustments impacted employees and employers alike. First, a review by Kennedy et al. (2010) was conducted to explore the role ergonomics training and workstation adjustments play on the prevention of upper extremity musculoskeletal injuries in the workforce. This systematic review consisted of 36 scholarly peer-reviewed articles focusing on interventions delivered by physical therapists. There was strong evidence that ergonomics training versus workstation adjustments only decreased upper extremity musculoskeletal injuries. Moderate evidence of effectiveness was shown for workstation adjustments in conjunction with ergonomics training to decrease upper extremity musculoskeletal injuries at work. A second systematic review examined how ergonomics training can counteract the economic burden employers experience from having injured employees and the associated negative costs. This review looked at 35 studies that had ergonomic interventions given by a physical therapist. The studies were divided into manufacturing/warehouse sector and administration/healthcare sector. There was strong evidence to show that ergonomics had a positive effect in the manufacturing/warehouse sector and moderate evidence in the administrative/healthcare sector. Researchers concluded that employing an ergonomics program also was cost effective (Tompa et al., 2010). A third systematic review specifically researching ergonomic interventions for musculoskeletal injuries in the workplace was conducted by Leyshon et al. (2010). This review synthesized the relevant literature and determined that eight articles were considered high quality. The purpose of this systematic review was to establish the level of evidence and the number of high-quality studies involving ergonomics as a baseline for future studies. Researchers concluded that the eight studies used in this review showed only insufficient to moderate levels of evidence. They concluded that more high-quality studies looking at the effect of ergonomics alone on musculoskeletal injuries in a work environment are needed. A third systematic review specifically researching ergonomic interventions for musculoskeletal injuries in the workplace was conducted by Leyshon et al. (2010). A fourth systematic review investigated whether there are effective workplace interventions that effectively manage chronic MSDs. The review included 12 studies that investigated effectiveness of a specific strengthening exercise program or interventions provided by health professionals at the workplace when compared with controls or interventions not at the workplace. Seven studies were classified as high quality and five studies were classified as acceptable. The authors concluded that workplace interventions such as high-intensity strengthening exercises and/or integrated health care can decrease pain and symptoms for employees who experience chronic MSDs. However, the authors noted that the current research in this area is limited (Skamagki et al., 2018).
A meta-analysis by Chen et al. (2018) was done to evaluate workplace treatments for employees with neck pain in an office setting. This review consisted of 27 articles which were all randomized control trials with on-site treatments provided to patients. Treatments consisted of strengthening, stretching, manual therapy techniques, and ergonomics training. There was moderate-quality evidence that neck/shoulder strengthening exercises and general fitness training programs were effective in reducing neck pain. Greater effects were observed with greater participation in exercise. Ergonomic interventions were supported by low-quality evidence. The authors concluded that workplace-based strengthening exercises and general fitness training were effective in reducing neck pain in office workers who were symptomatic.
CLINICAL IMPLICATIONS
As noted in this review, there are many options for the management of workers in the prevention and management of WMSDs, including education, ergonomic evaluations, and on-site treatment interventions (Fig. 1). One additional option is self-care of the worker, which may involve instructional pamphlets, manuals, and computer-based learning modules to prepare individuals to manage their health conditions or MSDs or change their lifestyle. Unfortunately, there is poor evidence to suggest that self-management programs are effective at decreasing pain and managing/preventing WMSDs (Skamagki et al., 2018). Therefore, other management options are necessary. This review suggests that physical therapists, as part of a multidisciplinary team, could be suitably equipped to manage WMSDs and help employees to remain healthy and injury-free at work.
Fig. 1.
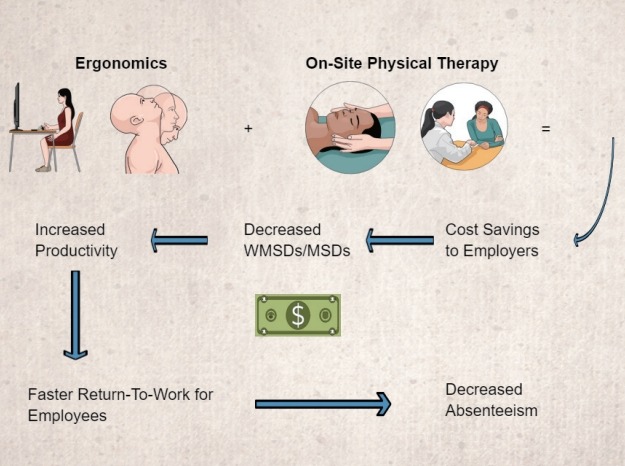
Graphic abstract depicting how participation in ergonomics and on-site physical therapy treatment in the workplace (e.g., education, exercise, manual intervention) has a positive effect on decreasing work-related musculoskeletal disorders (WMSDs), decreasing costs associated with these injuries, increasing work productivity, and decreasing absenteeism and improving presenteeism amongst workers.
While education and ergonomic intervention appear to have benefit in the prevention and management of WMSDs, the effectiveness of these interventions seems to be magnified when they are combined with stretching and strengthening exercises. With regard to stretching exercises, addressing those muscles that are prone to shortening and hypertonicity (e.g., pectoralis major, rectus femoris, the lower of the erector spinae, iliopsoas, and upper trapezius) is most indicated (Jaromi et al., 2012). Strengthening exercises are likely going to most effective when based on the principle of gradualism, especially in an individual with little experience in strengthening exercises. For a 6-week strengthening program, the following format may be used: isometric (1 to 2 weeks), isotonic concentric (3 to 4 weeks) exercises, and then isotonic eccentric (5 to 6 weeks) exercises, with strength exercises improving endurance first implemented (1 to 3 weeks, 3 to 5 sets of 25 to 30 repetitions), followed by maximal strength-improving exercises (4 to 6 weeks, 3 to 5 sets of 10 to 12 repetitions) (Jaromi et al., 2012). Many of the studies we examined utilized low-intensity strengthening; more research is necessary on the effects of high-intensity strengthening exercises, as well as cardiovascular endurance training, on the prevention and management of WMSDs. While the evidence in limited, we believe these interventions hold great promise for the prevention of WMSDs, as well as chronic conditions such as cardiovascular disease, diabetes, osteoporosis and cancer.
There appears to be strong evidence that on-site treatment options positively influence cost and treatment outcome (Fig. 1). One benefit to on-site care is that the physical therapist can easily visit the job site, gain a thorough understanding of the job requirements, and provide ergonomic modifications that are specific to an individual’s position. A second benefit is that the physical therapist, who now has expertise in that individual’s job, can be accessed directly by the worker and provide targeted intervention in the form of manual intervention and therapeutic exercise. A third benefit is that the evidence suggests that fewer treatments are necessary to achieve optimal outcomes with on-site care; additionally, the worker saves valuable time by not having to travel to and from off-site appointments.
In addition to having appropriate rehabilitation measures in place with an on-site ergonomics program, supportive work conditions at work increase work ability and improve the return to work process for individuals on long-term sick leave (Ahlstrom et al., 2013). Supportive work conditions include employees having a degree of freedom and meaning to their work, social support, a sense of community at their workplace, and job satisfaction. These are factors that would likely be driven by leadership in an organization; therefore, in addition to providing routine care, health care professionals should also discuss these supportive factors with leadership, in an effort to maximize outcome and facilitate timely return to work. In addition to a lack of supportive factors, fear-avoidance beliefs about work could also negatively influence outcome. Further research needs to evaluate fear-avoidance beliefs and how this influences prevention and return to work strategies, including specific rehabilitation strategies designed to manage individuals with these beliefs.
CONCLUSIONS
This paper highlighted the effectiveness a physical therapist can have in the occupational health setting on ergonomics, employee health, preventions of MSDs and WMSDs, return to work programs, and, such as therapeutic exercise prescription and manual intervention. Our review of the literature has shown an overwhelmingly positive effect that ergonomic training, workplace safety and education, on-site physical therapy treatments including exercise and manual therapy, and return to work programs were beneficial to employees and employers by decreasing injuries, increasing productivity, decreased absenteeism, and providing quicker return to work for injured workers. Due to the increasing incidence of MSDs and WMSDs, more research will be needed to help create more effective strategies, delivery systems, and interventions for worksite health promotion programs within sedentary occupations. Additional strategies include targeting specific groups determined by identifying risk factors and applying specific education and exercise interventions that are appropriate, as well as getting more companies to seek out ergonomics training and onsite treatment options from physical therapists. It is important to ensure that payers, employers and employees are awareness off the crucial role physical therapists can play in occupational health. Physical therapists also need to advocate for their role in occupational health and continue to offer expert care to workers in a nontraditional manner.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- Ahlstrom L, Hagberg M, Dellve L. Workplace rehabilitation and supportive conditions at work: a prospective study. J Occup Rehabil. 2013;23:248–260. doi: 10.1007/s10926-012-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezner JR. Promoting health and wellness: implications for physical therapist practice. Phys Ther. 2015;95:1433–1444. doi: 10.2522/ptj.20140271. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics . Employer related workplace injuries and illnesses – 2016 [Internet] Washington, DC: U.S. Bureau of Labor Statistics; c2018. [cited 2017 Nov 9]. Available from: https://www.bls.gov/news.release/archives/osh_11092017.pdf. [Google Scholar]
- Cecil R, Ross M. Effective worksite strategies and interventions to increase physical activity in sedentary workforce populations: the role of the physical therapists. Orthop Phys Ther Pract. 2017;29:56–62. [Google Scholar]
- Chen X, Coombes BK, Sjøgaard G, Jun D, O’Leary S, Johnston V. Workplace-based interventions for neck pain in office workers: systematic review and meta-analysis. Phys Ther. 2018;98:40–62. doi: 10.1093/ptj/pzx101. [DOI] [PubMed] [Google Scholar]
- Chetty L. Physiotherapy and ergonomics for a work-related musculoskeletal disorder. Int J Ther Rehabil. 2010;17:84–91. [Google Scholar]
- Chetty L. The role of physiotherapy in occupational health rehabilitation: a review of the literature. Indian J Physiother Occup Ther. 2013;7:118–122. [Google Scholar]
- Curran JA, Grimshaw JM, Hayden JA, Campbell B. Knowledge translation research: the science of moving research into policy and practice. J Contin Educ Health Prof. 2011;31:174–180. doi: 10.1002/chp.20124. [DOI] [PubMed] [Google Scholar]
- Engberg JB, Harris-Shapiro J, Hines D, McCarver P, Liu HH. The impact of worksite clinics on teacher health care utilization and cost, self-reported health status, and student academic achievement growth in a public school district. J Occup Environ Med. 2018;60:e397–405. doi: 10.1097/JOM.0000000000001373. [DOI] [PubMed] [Google Scholar]
- Hoeben C, Louw Q. Ergonomic chair intervention: effect on chronic upper quadrant dysfunction, disability and productivity in female computer workers. S Afr J Physiother. 2014;70:11–18. [Google Scholar]
- Jaromi M, Nemeth A, Kranicz J, Laczko T, Betlehem J. Treatment and ergonomics training of work-related lower back pain and body posture problems for nurses. J Clin Nurs. 2012;21:1776–1784. doi: 10.1111/j.1365-2702.2012.04089.x. [DOI] [PubMed] [Google Scholar]
- Kennedy CA, Amick BC, 3rd, Dennerlein JT, Brewer S, Catli S, Williams R, Serra C, Gerr F, Irvin E, Mahood Q, Franzblau A, Van Eerd D, Evanoff B, Rempel D. Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time. J Occup Rehabil. 2010;20:127–162. doi: 10.1007/s10926-009-9211-2. [DOI] [PubMed] [Google Scholar]
- Kim SE, Chun JC, Hong J. Ergonomics interventions as a treatment and preventative tool for work-related musculoskeletal disorders. Int J Caring Sci. 2013;6:339–348. [Google Scholar]
- Leyshon R, Chalova K, Gerson L, Savtchenko A, Zakrzewski R, Howie A, Shaw L. Ergonomic interventions for office workers with musculoskeletal disorders: a systematic review. Work. 2010;35:335–348. doi: 10.3233/WOR-2010-0994. [DOI] [PubMed] [Google Scholar]
- Liberty Mutual Insurance . Liberty mutual workplace safety index [Internet] Boston (MA): Liberty Mutual Insurance; c2018. [cited 2018 Nov 1]. Available from: https://business.libertymutualgroup.com/business-insurance/Documents/Services/Workplace%20Safety%20Index.pdf. [Google Scholar]
- Mani K, Provident I, Eckel E. Evidence-based ergonomics education: promoting risk factor awareness among office computer workers. Work. 2016;55:913–922. doi: 10.3233/WOR-162457. [DOI] [PubMed] [Google Scholar]
- Noh H, Roh H. Approach of industrial physical therapy to assessment of the musculoskeletal system and ergonomic risk factors of the dental hygienist. J Phys Ther Sci. 2013;25:821–826. doi: 10.1589/jpts.25.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris K. Expediting return to work full duty with successful onsite medical management. Procedia Manuf. 2015;3:152–157. [Google Scholar]
- Pikaar RN. Case studies--ergonomics in projects. Work. 2012;41(Suppl 1):5892–5898. doi: 10.3233/WOR-2012-0985-5892. [DOI] [PubMed] [Google Scholar]
- Shariat A, Cleland JA, Danaee M, Kargarfard M, Sangelaji B, Tamrin SBM. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: a randomized controlled trial. Braz J Phys Ther. 2018;22:144–153. doi: 10.1016/j.bjpt.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw W, Hong QN, Pransky G, Loisel P. A literature review describing the role of return-to-work coordinators in trial programs and interventions designed to prevent workplace disability. J Occup Rehabil. 2008;18:2–15. doi: 10.1007/s10926-007-9115-y. [DOI] [PubMed] [Google Scholar]
- Skamagki G, King A, Duncan M, Wåhlin C. A systematic review on workplace interventions to manage chronic musculoskeletal conditions. Physiother Res Int. 2018;23:e1738. doi: 10.1002/pri.1738. [DOI] [PubMed] [Google Scholar]
- Tompa E, Dolinschi R, de Oliveira C, Amick BC, 3rd, Irvin E. A systematic review of workplace ergonomic interventions with economic analyses. J Occup Rehabil. 2010;20:220–234. doi: 10.1007/s10926-009-9210-3. [DOI] [PubMed] [Google Scholar]


